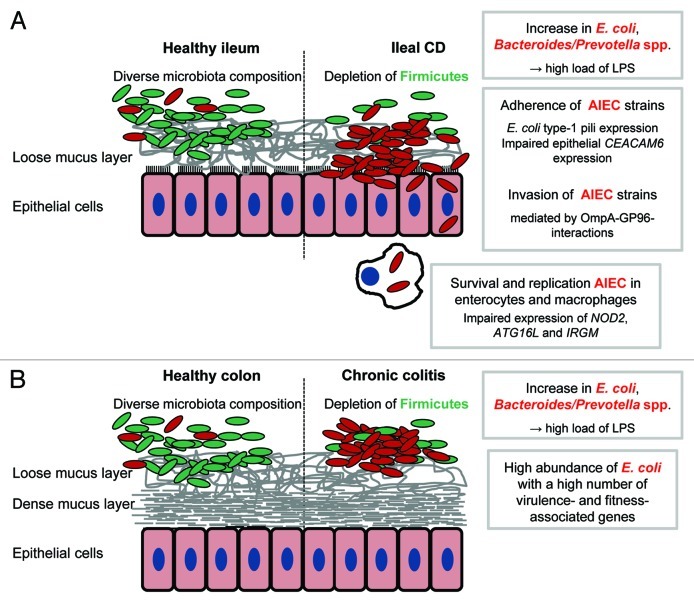
Figure 1. Pro-inflammatory effects of gut bacteria in IBD. Crohn’s disease and ulcerative colitis are characterized by a depletion of Firmicutes in conjunction with an increase of Gram negative bacteria, namely E. coli and Bacteroides/Prevotella spp The shift in microbiota composition is associated with high loads of bacterial antigens (mainly LPS). The recognition by the immune system of these antigens and the subsequent initiation of pro-inflammatory responses may be an important trigger of IBD. In a subset of patients with ileal CD, adherent-invasive E. coli (AIEC) strains are highly abundant and able to invade and to survive and replicate in host cells. An impaired bacterial clearance by the host may be responsible for disease development in patients with mutations in autophagy-associated genes (A). Direct interactions between bacterial and host cells may be less important in chronic colitis because the colonic mucosa is protected by a dense mucus layer. Increased concentrations of bacterial antigens resulting from a high abundance of Gram negative bacteria may drive colitis progression. The exact role in chronic colitis of E. coli strains with a high number of virulence- and fitness-associated genes remains to be identified (B).

An official website of the United States government
Here's how you know
Official websites use .gov
A
.gov website belongs to an official
government organization in the United States.
Secure .gov websites use HTTPS
A lock (
) or https:// means you've safely
connected to the .gov website. Share sensitive
information only on official, secure websites.