Abstract
Most of the extant literature on borderline personality disorder has focused on the course, consequences, and correlates of this disorder among adults. However, little is known about childhood borderline personality (BP) features, or the factors associated with the emergence of BP pathology in childhood. A greater understanding of childhood BP features and associated risk factors has important implications for the development of primary and secondary prevention programs. The goal of the present study was to examine the interrelationships among two BP-relevant traits (affective dysfunction and impulsivity), a BP-relevant environmental stressor (emotional abuse), and BP features in a sample of 225 children aged 11 to 14 years. Results provide support for the role of both trait vulnerabilities and environmental stressors in childhood BP features. Further, findings highlight the moderating role of affective dysfunction in the relationship between emotional abuse and childhood BP features.
Borderline personality disorder (BPD) is a serious mental health problem with great public health significance. Although BPD is found at rates of 1% to 2% in the general population (Lenzenweger, Lane, Loranger, & Kessler, 2007; Skodol et al., 2002), individuals with BPD represent approximately 15% of clinical populations (Skodol et al., 2002; Widiger & Weissman, 1991) and are major consumers of health care resources (Skodol et al., 2005; Zanarini, Frankenburg, Khera, & Bleichmar, 2001). Further, BPD is associated with severe functional impairment, high rates of co-occurring psychiatric disorders, and elevated risk for completed suicide (see Skodol et al., 2002, 2005; Work Group on Borderline Personality Disorder, 2001).
Although research has been conducted on the prognosis, course, consequences, and correlates of BPD, little is known about the emergence and early manifestations of this disorder (Crick, Murray-Close, & Woods, 2005; Paris, 2005). However, given evidence that personality develops from an early age (Caspi, Roberts, & Shiner, 2005; Hartup & van Lieshout, 1995), it is unlikely that personality disorders develop suddenly in adulthood. Furthermore, findings that adults with BPD report having experienced many borderline personality (BP) symptoms in childhood (Reich & Zanarini, 2001; Shiner, 2005; Zanarini et al., 2006) suggest that early manifestations of BP pathology can likely be observed in childhood. Not only would research on the early manifestations of BP pathology have important implications for the development of secondary prevention programs, studies examining the risk factors associated with childhood BP features may facilitate the identification of children at risk for the later development of BPD or other personality disorders (e.g., antisocial personality disorder; see Beauchaine, Klein, Crowell, Derbidge, & Gatzke-Kopp, 2009), as well as frequently co-occurring Axis I disorders (such as substance use disorders; see Cohen, Chen, Crawford, Brook, & Gordon, 2007). Additionally, such investigations may provide a better understanding of the pathogenesis of both personality disorders in general and BPD specifically. The current study represents the first investigation of the interrelations among BPD-relevant trait vulnerabilities, the experience of emotional abuse, and BP features in a community sample of children.
Importance of Borderline Personality Symptoms in Childhood
Most research on the factors associated with childhood BP pathology has used modified criteria corresponding to adult BPD diagnostic criteria to diagnose BPD in children (Goldman, D’Angelo, DeMaso, & Mezzacappa, 1992; Greenman, Gunderson, Cane, & Saltzman, 1986; Guzder, Paris, Zelkowitz, & Feldman, 1999; Guzder, Paris, Zelkowitz, & Marchessault, 1996; Paris, Zelkowitz, Guzder, Joseph, & Feldman, 1999). Despite providing evidence that the environmental and neuropsychological factors associated with a BPD diagnosis in childhood are the same as those associated with BPD in adults (Goldman et al., 1992; Guzder et al., 1996, 1999; Paris et al., 1999; Zelkowitz, Paris, Guzder, & Feldman, 2001), the practice of diagnosing BPD in childhood has been criticized for assuming a stability in functioning and developmental trajectory that likely vary (Coolidge, 2005; Crick et al., 2005). Instead, developmental researchers emphasize the importance of assessing childhood BP pathology dimensionally (vs. categorically) and within a developmental psychopathology framework. Such an approach allows for an examination of the full range of BP features and dose-response relationships, and does not assume the presence of pathology (as problem behavior is conceptualized as falling on a continuum ranging from none to severe). Further, a developmental psychopathology perspective suggests the importance of examining the ways in which various biological, psychological, and social-contextual factors interact to predict normal and abnormal development across the life course (Cicchetti & Toth, 2009), emphasizing the likelihood of varying pathways to both adaptive and maladaptive outcomes. As such, the same constellation of symptoms and behaviors in childhood may lead to a variety of outcomes (i.e., multifinality; Cicchetti & Rogosch, 1996, 2002), and one outcome may emerge as a result of different risk factors or developmental processes (i.e., equifinality; Cicchetti & Rogosch, 1996, 2002).
As applied here, a developmental psychopathology approach suggests that childhood BP features may have many different trajectories, and should not be considered indicative of an enduring disorder (as these features will not necessarily evolve on one course to the development of BPD in adulthood). Rather, consistent with the concept of multifinality, children who display early signs of BP pathology are expected to take different pathways depending on the risk and protective factors they encounter (Cicchetti & Lynch, 1993). Thus, although the presence of BP features in childhood may, for some children, be indicative of risk for the later development of BPD (as it is likely that this disorder has its origins earlier in development), they may also lead to a variety of multifinal outcomes, ranging from the development of other personality disorders (e.g., antisocial personality disorder) or Axis I disorders in adolescence and adulthood to more adaptive outcomes reflecting the absence of any enduring pathology. Of course, it is also important to note that the presence of BP features in childhood likely represent only one pathway through which BPD may develop, with other difficulties in childhood also potentially leading to BPD in adulthood. Nonetheless, given evidence of a connection between childhood and adulthood forms of other disorders (see Rutter, 1996), examining the presence of childhood BP features is a useful first step in examining the emergence of BP pathology earlier in the lifespan. In particular, research on the factors associated with childhood BP features may provide important information regarding the development of BP and related pathologies, paving the way for prevention and intervention efforts (Rogosch & Cicchetti, 2005).
Risk Factors for BP Pathology
Consistent with a developmental psychopathology approach, risk factors can be conceptualized as occurring within multiple domains of influence, including individual difference characteristics, family characteristics, and environmental characteristics (Bronfenbrenner, 1979; Cicchetti, 2008; Cicchetti & Lynch, 1993). With regard to BPD, extant theoretical models suggest that BPD results from the interaction of trait vulnerabilities and environmental stressors (Beauchaine et al., 2009; Crowell, Beauchaine, & Linehan, 2009; Linehan, 1993; Zanarini & Frankenburg, 1997).
The most commonly reported environmental stressor that has been shown to increase risk for BPD is childhood maltreatment, including experiences of abuse and neglect (Zanarini, 2000). Indeed, not only does childhood maltreatment represent a risk factor for BP pathology in childhood (Goldman et al., 1992; Guzder et al., 1996, 1999; Zelkowitz et al., 2001) and adolescence (Westen, Ludolph, Misle, Ruffins, & Block, 1990), adult BPD patients report higher rates of childhood abuse and neglect than individuals with other personality disorders (Battle et al., 2004; Zanarini, Gunderson, Marino, Schwartz, & Frankenburg, 1990) and Axis I disorders (Ogata et al., 1990). As for the particular forms of maltreatment associated with BPD, although sexual abuse was once thought to be the most relevant environmental risk factor for BPD (Zanarini et al., 1997), recent research suggests that emotional abuse (i.e., verbal assaults on a child’s sense of self, worth, well-being, or safety) may be the form of maltreatment most relevant to BPD. For example, studies examining the associations between various forms of maltreatment and BPD in adults have found that emotional abuse (as assessed with the Childhood Trauma Questionnaire; see Measures below) is the only form of maltreatment to demonstrate a unique association with BPD above and beyond other forms of abuse and neglect (including sexual and physical abuse and emotional and physical neglect; Bornovalova, Gratz, Delany-Brumsey, Paulson, & Lejuez, 2006; Gratz, Tull, Baruch, Bornovalova, & Lejuez, 2008). Likewise, in their longitudinal Children in the Community study, Johnson and colleagues (2001) found that childhood experiences of verbal abuse (defined as episodes of screaming at the child combined with threats of physical violence for misbehavior and/or statements of not loving or wanting the child or intentions to send the child away) prospectively predicted elevated BP symptoms in adolescence and young adulthood, as well as increased risk for BPD per se, even after controlling for a wide range of relevant factors, including physical and sexual abuse and neglect. Moreover, Linehan’s (1993) emphasis on the etiologic role of invalidation (i.e., the punishment, denial, trivialization, or ridicule of expressions of private experiences) in BPD provides theoretical support for the relevance of emotional abuse in particular (which arguably may be more closely related to invalidation than other forms of abuse).
Emotional abuse alone is not sufficient to account for the development of BP pathology, however. Instead, consistent with a developmental psychopathology framework, maltreatment is thought to lead to BPD only in the context of underlying trait vulnerabilities (Paris, 2000). In particular, the higher-order traits of affective dysfunction and disinhibition have been identified as “core” personality traits underlying BPD (Linehan, 1993; Livesley, Jang, & Vernon, 1998; Nigg, Silk, Stavro, & Miller, 2005; Siever & Davis, 1991; Skodol et al., 2002). Although these traits are not considered to be specific to BPD, researchers in this area have long suggested that it is the interaction of these traits with each other, as well as relevant environmental stressors (such as maltreatment), that likely distinguishes BPD from other disorders (Paris, 2005; Siever & Davis, 1991; Trull, 2001). More recently, theories of BPD grounded in a developmental psychopathology perspective (e.g., Crowell et al., 2009) have highlighted the potential independent contributions of impulsivity and affective dysfunction to the development of BPD, suggesting that each may represent one pathway to the development of this disorder (consistent with the principle of equifinality).
The affective dysfunction thought to be relevant to BPD encompasses several lower-order emotion-related traits, including anxiousness and affective lability (i.e., the tendency to experience extreme fluctuations in affective states; Livesley et al., 1998); emotional intensity (i.e., the tendency to experience emotions strongly), reactivity (i.e., the tendency to be easily distressed by discrete emotional events), and sensitivity (i.e., the tendency to react quickly to stimuli; Linehan, 1993); and affective instability (i.e., marked, reactive shifts in mood; Siever & Davis, 1991; Skodol et al., 2002), all of which have been found to be associated with BP pathology. Specifically, research indicates that adult patients with BPD: (a) report heightened affective instability (Bornovalova et al., 2006; Henry et al., 2001; Koenigsberg et al., 2002) and emotional intensity/reactivity (Gratz, Rosenthal, Tull, Lejuez, & Gunderson, 2010; Henry et al., 2001; Koenigsberg et al., 2002); (b) evidence heightened sensitivity to emotional stimuli (Donegan et al., 2003; Herpertz et al., 2001) and emotion-specific reactivity (Gratz et al., 2010); and (c) exhibit elevated symptoms of anxiety (Snyder & Pitts, 1988). Further, affective dysfunction (in the form of emotional sensitivity alone, as well as the combination of several relevant lower-order traits, including emotional sensitivity, intensity, reactivity, and lability) has been shown to be associated with BP features in childhood (Crick et al., 2005; Gratz et al., 2009).
Research likewise provides evidence for a relationship between disinhibition and BPD. Specifically, behavioral dyscontrol or impulsiveness (in the form of deliberate self-harm, suicidal behaviors, substance use, and risky sexual behavior, among others) is one of the central defining features of BPD (Paris, 2005; Skodol et al., 2002), and is thought to stem from one of several lower-order disinhibition-related traits, including impulsivity, sensation seeking, risk-taking, and novelty seeking (Verheul, 2006). In particular, although research provides some evidence for an association between each of these lower-order personality traits and BP pathology in adulthood (e.g., Bornovalova et al., 2006; Kilpatrick et al., 2007; Pukrop, 2002; Reist, Haier, DeMet, & Chicz-DeMet, 1990), the lower-order trait that has received the most attention from researchers is impulsivity (defined here as the tendency to respond quickly and without forethought or consideration of the consequences of one’s behaviors; see Eysenck, 1993). This particular trait is considered to be the most relevant dimension of disinhibition to BPD (Beauchaine et al., 2009; Links, Heslegrave, & van Reekum, 1999; Siever & Davis, 1991; Zanarini, 1993), and has been found to be associated with BP pathology in both adulthood (Bornovalova et al., 2006; Henry et al., 2001; Hochhausen, Lorenz, & Newman, 2002) and childhood (Paris et al., 1999). Further, recent theoretical work has highlighted the relevance of impulsivity to the emergence of BP pathology in childhood as well (Beauchaine et al., 2009; Crowell et al., 2009).
Despite the complexity of the theorized interrelationships of these traits and environmental stressors in the development of BP pathology, no studies have examined the ways in which affective dysfunction and impulsivity interact to predict BP features, nor have studies examined the interaction of these traits with aspects of childhood maltreatment. However, a recent study examining the interrelations among the BPD-relevant traits of affective dysfunction and sensation seeking and BP symptoms within a community sample of children found a significant interaction between affective dysfunction and sensation seeking on childhood BP symptoms (with sensation seeking related to BP symptoms only among children with at least average levels of trait affective dysfunction; Gratz et al., 2009). These findings provide support for the hypothesized interaction of core personality traits in the risk for BP pathology, and highlight the importance of further examining the ways in which BP-relevant personality traits interact to predict childhood BP features. Furthermore, given the emphasis on the interaction of trait vulnerabilities and environmental stressors within theories of the pathogenesis of BPD (Beauchaine et al., 2009; Crowell et al., 2009; Linehan, 1993; Zanarini & Frankenburg, 1997), as well as many forms of psychopathology in children (see Cicchetti & Cohen, 2006), research examining the complex interrelationships of traits and environmental stressors is needed.
The Current Study
Thus, the goal of the present study was to examine the interrelations among two BP-relevant personality traits (affective dysfunction and impulsivity), a BP-relevant environmental stressor (emotional abuse), and childhood BP features in a sample of 225 children aged 11 to 14 years. Consistent with previous research and extant theoretical literature, we hypothesized that both the trait vulnerabilities (and their interaction) and emotional abuse would be associated with childhood BP features. Further, consistent with a developmental psychopathology framework, we hypothesized that the trait vulnerabilities of interest would moderate the association between emotional abuse and childhood BP features (with emotional abuse predicting BP features only in the context of an underlying trait vulnerability).
Method
Participants
This study employed data from a sample of 277 participant dyads (children aged 9 to 13 at initial enrollment and their parents/legal guardians) participating in a larger prospective study of behavioral, environmental, and genetic mechanisms of risk for HIV-related risk behaviors in youth. Participants were a convenience sample of children and their caregivers recruited through media outreach in the greater Washington, D.C., metropolitan area, as well as study advertisements distributed to area schools, libraries, and Boys and Girls Clubs. Recruitment lasted approximately 2 years and was open to all youth in the 5th and 6th grades who were proficient in English; no other exclusion criteria were used.
Participant dyads included in the present analyses are youth and their mothers who completed both the baseline and first annual follow-up assessments (Waves 1 and 2). However, this study examines only Wave 2 data, as the measures of BP features and emotional abuse were added partway through Wave 1, and the measure of impulsivity was not added until Wave 2. Participants were excluded from the present analyses if they did not complete the second wave of data collection (n = 33), were accompanied by a caregiver other than their mother (n = 10), or were missing data on the primary dependent or independent variables of interest (n = 9). Participants lost to attrition included those who had moved from the area, could not be located, or did not respond to phone or letter inquiries. Excluded participants did not differ significantly on gender, age, or ethnicity (ps >.10).
The resultant sample of 225 youth ranged in age from 11 to 14 (M = 12.15, SD = 0.82) and 45% (n = 101) were female. With regard to the children’s racial/ethnic background, 50% were White, 33% were Black/African-American, 3% were Latino, 1% were Asian, and 13% were of another or unidentified racial/ethnic background. With regard to the parents’ highest level of education attained, 8% of the mothers and 15% of the fathers had completed high school or received a GED, 27% of the mothers and 23% of the fathers had attended at least some college or technical school, 30% of the mothers and 20% of the fathers had graduated college, and 31% of the mothers and 32% of the fathers had received an advanced degree. Median family income was $93,000 per year (mean = $96,873 ± $54,574).
Measures
Due to concerns regarding participant burden related to the addition of supplementary measures to an already lengthy assessment battery, it was not possible to include both caregiver- and child-report measures of the key constructs of interest; thus, assessments of the constructs of interest were generally limited to only one measure each (i.e., either child- or caregiver-report).
Caregiver-Report Measures
The Coolidge Personality and Neuropsychological Inventory for Children (CPNI; Coolidge, 2005) is a 200-item, caregiver-as-respondent measure of DSM-IV Axis I and II pathology and related difficulties among children and adolescents. Caregivers are asked to rate the extent to which each item accurately describes their child on a 4-point Likert-type scale (ranging from 1 = “This is strongly false for my child; My child is not at all like this” to 4 = “This is strongly true for my child; I would say this describes my child very well”). The CPNI was normed on a sample of 780 ethnically diverse children ranging in age from 5 to 17 (Coolidge, 2005), and its psychometric properties are well-established (Coolidge, Segal, Stewart, & Ellett, 2000; Coolidge & Thede, 2000; Coolidge, Thede, & Jang, 2001; Coolidge, Thede, Stewart, & Segal, 2002). This study utilized the subscales assessing BP features and the trait of affective dysfunction.
The BP subscale includes 9 items adapted from the DSM-IV criteria for adult BPD to be age-appropriate for children (Coolidge, 2005). To ensure that developmentally appropriate behaviors are not erroneously considered indicative of the emergence of BP pathology, the CPNI requires that parents compare their child’s behavior to the behavior of other children of the same age. Further, parents are instructed to endorse only those behaviors that have been typical of their child over an extended period of time (i.e., for several months). Example items include, “My child tries very hard to avoid being alone or feeling abandoned,” “My child has threatened or tried to commit suicide or has hurt himself/herself on purpose,” and “My child makes friends quickly but soon after seems to hate them.” Consistent with the conceptualization of childhood BP features used in this study, the CPNI takes a dimensional approach to the assessment of BP features among children.
The BP subscale has been found to have good test-retest reliability across a 4- to 6-week period (r = .67; Coolidge et al., 2002), as well as good construct and concurrent validity (see Coolidge et al., 2000). Specifically, in support of the construct validity of the BP subscale, children with elevated levels of BP features have been found to exhibit co-occurring difficulties commonly found among adults with BPD, including executive functioning deficits (Coolidge et al., 2000), impulsiveness (Kristensen & Torgersen, 2007), social anxiety (Kristensen & Torgersen), and ADHD (Coolidge et al., 2000). Further, in line with evidence that BPD is partially heritable among adults (e.g., Livesley et al., 1998; Torgersen, 2000; Torgersen et al., 2008), with studies finding heritability estimates as high as .69 for subthreshold BPD and .80 for definite BPD (see Torgersen et al., 2000), Coolidge et al. (2001) found that elevated BP features as assessed by the CPNI had a heritability of .76 among 112 child twin pairs averaging 9 years of age. For the present study, items were summed to create a total BP features score (with possible scores ranging from 9 to 36). Internal consistency in this sample was adequate (α = .77).
The affective dysfunction subscale of the CPNI assesses several lower-order emotion-related traits found to be particularly relevant to BPD in adults, including emotional lability, sensitivity, intensity, and reactivity. Although the original subscale consists of 10 items, one of these items overlaps with an item on the BP subscale (i.e., the item used to assess the emotional lability criterion of BPD, “My child’s moods change quickly.”). Therefore, this item was excluded from the affective dysfunction subscale, which was created by summing scores on the remaining 9 items (none of which overlapped with the BPsubscale). Sample items include “My child’s emotions seem to shift rapidly and seem to be shallow” and “My child is too touchy or easily annoyed.” The affective dysfunction subscale has been found to be have good test-retest reliability over a 4–6 week period (r = .86; Coolidge et al., 2002), and to be positively associated with childhood BP symptoms (Gratz et al., 2009). Scores on the affective dysfunction items were summed to create an overall subscale score ranging from 9 to 36, with higher scores indicating greater affective dysfunction. Internal consistency in the current sample was good (α = .84).
The Oppositional Defiant Disorder and Conduct Disorder Subscales of the Disruptive Behavior Disorders Rating Scale (DBD; Pelham, Gnagy, Greenslade, & Milich, 1992) were used to assess for DSM-IV diagnoses of oppositional-defiant disorder (ODD) and conduct disorder (CD). Caregivers are asked to rate the extent to which each DSM-IV criterion accurately describes their child on a 4-point Likert-type scale ranging from “not at all” to “very much”, with those criteria endorsed as “pretty much” or “very much” considered to be present (see Pelham et al., 1992; Pillow, Pelham, Hoza, Molina, & Stultz, 1998). Consistent with past research using this measure (see Antrop, Roeyers, Oosterlaan, & Van Oost, 2002; Oosterlaan, Scheres, & Sergeant, 2005; Pelham et al., 1992; Wright, Waschbusch, & Frankland, 2007; Wymbs & Pelham, 2010), dichotomous variables reflecting the presence versus absence of ODD and CD were created, with four or more symptoms needed to meet criteria for ODD, and three or more symptoms needed to meet criteria for CD. The factor structure of the DBD has been supported through exploratory factor analyses (Pelham et al., 1992), and support for its construct validity has been provided by findings of significant associations between the ODD and CD subscales and both (a) ODD and CD diagnoses from well-established caregiver-report structured clinical interviews (e.g., Wright et al., 2007), and (b) teacher-report ratings of externalizing psychopathology (Oosterlaan et al., 2005). The ODD and CD subscales were included in this study as potential covariates to examine whether affective dysfunction, impulsivity, and emotional abuse are associated with childhood BP features above and beyond externalizing psychopathology (thereby enabling a more conservative test of the study’s hypotheses). Internal consistency of these scales within this sample was good (αs > .83).
Child-Report Measures
The Eysenck Impulsivity Subscale(EIS) of the Eysenck Impulsiveness Scale (Eysenck, Pearson, Easting, & Allsopp, 1985) is a 19-item, forced choice (yes vs. no) measure of impulsivity, defined as the tendency to respond quickly and without forethought or consideration of the consequences of one’s behaviors (Eysenck, 1993). This measure has been examined within numerous samples, including ethnically diverse youth (Aklin, Lejuez, Zvolensky, Kahler, & Gwadz, 2005; Lejuez et al., 2007), and has been found to have good internal consistency (α = .84) among both female and male participants (Eysenck et al., 1985). Providing support for the predictive validity of the EIS, scores on this measure have been found to be significantly associated with a laboratory-based assessment of risk-taking behavior (Lejuez et al., 2007), as well as self-reported substance use, delinquency, and fighting (Aklin et al., 2005) within ethnically diverse adolescent samples. Items were summed to create an overall impulsivity score ranging from 0 to 19. Internal consistency in the current sample was adequate (α = .77).
The Emotional Abuse Subscaleof the Childhood Trauma Questionnaire–Short Form (CTQ; Bernstein et al., 2003) is a 5-item self-report measure of emotional abuse, defined as “verbal assaults on a child’s sense of worth or well-being or any humiliating or demeaning behavior directed toward a child by an adult” (see Bernstein, Ahluvalia, Pogge, & Handelsman, 1997; Bernstein et al., 2003). The CTQ has been validated within a variety of samples, including ethnically diverse adolescent psychiatric inpatients aged 12 to 17 (Bernstein et al., 1997; Bernstein et al., 2003). Scores on the emotional abuse subscale of the CTQ have been found to have good internal consistency (α = .95) and to be significantly correlated with therapists’ independent ratings of emotional abuse among a large sample of adolescent inpatients (Bernstein et al., 1997, 2003). Further, scores on this subscale have been found to predict changes in adolescents’ depressive symptoms over the course of a year (Gibb & Abela, 2008), to be significantly associated with externalizing behaviors among adolescent inpatients (Buckle, Lancaster, Powell, & Higgins, 2005), and to be uniquely associated with both negative affect and externalizing symptoms among a large community-based sample of urban adolescents (Arata, Langhinrichsen-Rohling, Bowers, & O’Brien, 2007). Items were summed to create an overall emotional abuse score ranging from 5 to 25. Internal consistency of this subscale in the current sample was good (α = .84).
The Revised Child Anxiety and Depression Scale(RCADS; Chorpita, Yim, Moffitt, Umemoto, & Francis, 2000) was used to assess symptoms of anxiety disorders and major depression. Participants are asked to rate the frequency with which they have experienced each item on a 4-point Likert-type scale (0 = never; 3 = always). The RCADS has demonstrated convergent validity with other well-established measures of childhood anxiety and depression within both nonclinical (Chorpita et al., 2000) and clinical (Chorpita, Moffitt, & Gray, 2005) samples. Items on the major depression subscale were summed to create a total score of depression symptom severity, and items on the anxiety disorder subscales were summed to create a total score of anxiety symptom severity. The RCADS subscales were included in this study as potential covariates to examine whether affective dysfunction, impulsivity, and emotional abuse are associated with childhood BP features above and beyond internalizing psychopathology. Internal consistency of these scales within this sample was good (αs > .82).
A shortened version of the Centers for Disease Control and Prevention Youth Risk Behavior Surveillance System(CDC, 2001) was used to assess delinquent behaviors (a form of externalizing psychopathology; see MacPherson et al., 2010). Children were asked to indicate the past year frequency of seven different delinquent behaviors, including fighting, gambling, stealing, and carrying a weapon. Consistent with past research, items were summed to create a total delinquency score (Lejuez, Aklin, Zvolensky, & Pedulla, 2003; see also Feinberg, Greenberg, Osgood, Sartorius, & Bontempo, 2007), with possible scores ranging from 0 to 35. This measure was included as a potential covariate to examine whether the traits and stressor of interest are associated with childhood BP features above and beyond externalizing psychopathology.
Procedure
All procedures were reviewed and approved by the University of Maryland Institutional Review Board (IRB). Study advertisements instructed interested caregivers to call the university for further details about the study. Upon calling, caregivers were informed that the purpose of the study was to examine youth risk-taking behaviors. Eligible participants were scheduled for an assessment session at the University of Maryland campus accessible by public transportation.
Upon arrival at the baseline assessment session, a more detailed description of the study procedures was provided and the caregivers and children signed informed consent/assent forms, respectively. The child and caregiver were then accompanied to separate rooms to complete the assessments. Standardized instructions for completing the measures were provided to each member of the dyad separately, and participants were encouraged to ask the researchers questions. Once the participants had completed the assessments, they were debriefed and provided with their reimbursement (i.e., children were able to choose their prize, and parents were provided with $25 for their time). These procedures were repeated at all assessment points.
Results
Variable Transformations and Calculations
Skewness and kurtosis of all variables were within the acceptable range of normality (i.e., skewness < 3 and kurtosis < 10; see Kline, 1998). Therefore, variable transformations were not required. However, before creating the interaction terms, the affective dysfunction, impulsivity, and emotional abuse variables were centered (i.e., put in deviation score form), so that the mean of each variable was 0 (see Aiken & West, 1991). These standardized scores were then used to create the interaction terms, with those scores on the variables making up each interaction term multiplied together.
Identification of Covariates
Preliminary analyses were conducted to explore the impact of demographic factors (including age, ethnic/racial background, gender, and family income) and measures of internalizing and externalizing psychopathology (including depression and anxiety symptoms, delinquent behaviors, and externalizing disorders) on the dependent variable, in order to identify potential covariates for later analyses (see Tabachnick & Fidell, 1996). Although childhood BP features were not significantly associated with any of the demographic variables (rs ≤ .09; ps > .10), they were significantly associated with the measures of depression and anxiety symptom severity (rs> .20; ps < .01), delinquent behaviors (r = .14; p < .05), and externalizing disorders (rs> .40; ps < .01). Thus, all of these measures of internalizing and externalizing psychopathology were included as covariates in subsequent analyses.
Preliminary Analyses
Table 1 presents descriptive data on the internalizing and externalizing disorders of participants, as well as each of the BP features assessed in the CPNI. Table 2 presents descriptive data on the primary variables of interest, as well as the correlations between these variables. Of note, although the average level of emotional abuse reported by the participants in this sample was in the minimal range (consistent with past studies of emotional abuse in community samples of youth this age; see Gibb & Abela, 2008), 9.3% of the children in this sample reported a history of moderate-severe emotional abuse. As predicted, results of the correlational analyses indicate that childhood BP features were significantly associated with the traits of affective dysfunction and impulsivity, as well as emotional abuse.
Table 1.
Descriptive Data for Internalizing and Externalizing Disorders, as well as Borderline Personality Features (N = 225)
| Mean | SD | % Meeting Clinical Threshold | |
|---|---|---|---|
| Internalizing Disorders | |||
| Major depressive disorder | 6.13 | 4.32 | 8.6 |
| Separation anxiety disorder | 2.76 | 2.92 | 11.3 |
| Social phobia | 8.31 | 4.30 | 1.8 |
| Obsessive compulsive disorder | 3.36 | 2.99 | 1.8 |
| Panic disorder | 2.89 | 3.15 | 6.5 |
| Generalized anxiety disorder | 4.93 | 3.06 | 3.8 |
| Total anxiety symptoms | 22.25 | 13.34 | |
| Externalizing Disorders | |||
| Oppositional defiant disorder | 0.60 | 1.32 | 4.9 |
| Conduct disorder | 0.25 | 0.91 | 3.6 |
| Borderline Personality Features | |||
| Inappropriate anger | 1.67 | 0.83 | |
| Affective instability | 2.40 | 0.91 | |
| Emptiness/boredom | 2.28 | 0.95 | |
| Identity problems | 1.52 | 0.78 | |
| Transient paranoia or dissociation | 1.28 | 0.63 | |
| Efforts to avoid abandonment | 1.90 | 0.95 | |
| Self-harm/suicidality | 1.06 | 0.28 | |
| Impulsive actions | 1.62 | 0.85 | |
| Unstable relationships | 1.32 | 0.56 | |
Table 2.
Descriptive Data for and Correlations between Primary Variables of Interest (N = 225)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | Mean | SD | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. BP features | --- | 15.05 | 4.14 | |||||||
| 2. Affective Dysfunction | .72** | --- | 14.91 | 4.43 | ||||||
| 3. Impulsivity | .26** | .15* | --- | 8.05 | 4.02 | |||||
| 4. Emotional Abuse | .27** | .08 | .26** | --- | 7.56 | 3.53 | ||||
| 5. Depression | .20** | .11 | .34** | .59** | --- | 6.13 | 4.32 | |||
| 6. Anxiety | .23** | .10 | .33** | .52** | .77** | --- | 22.25 | 13.34 | ||
| 7. ODD | .41** | .48** | .15* | .17* | .06 | .02 | --- | 0.60 | 1.32 | |
| 8. CD | .42** | .36** | .11 | .20** | .05 | .12 | .51** | --- | 0.25 | 0.91 |
| 9. Delinquency | .14* | .13* | .32** | .27** | .16* | .15* | .22** | .07 | 2.47 | 2.75 |
Note. BP = borderline personality.
p < .05.
p < .01.
Primary Analyses
A hierarchical multiple regression analysis was conducted to examine if (a) the personality traits of interest (and/or their interaction) significantly predict childhood BP features, (b) emotional abuse accounts for unique variance in childhood BP features above and beyond the personality traits of interest, and (c) the interaction of emotional abuse and the traits of interest accounts for additional variance in childhood BP features (above and beyond the main effects of the traits and stressor). Childhood BP features served as the dependent variable, with the covariates of depression symptom severity, anxiety symptom severity, delinquent behaviors, ODD, and CD entered in the first step of the equation, the traits of affective dysfunction and impulsivity entered in the second step of the equation, the interaction of affective dysfunction and impulsivity entered in the third step of the equation, the environmental stressor of emotional abuse entered in the fourth step of the equation, the interactions of emotional abuse with both affective dysfunction and impulsivity entered in the fifth step of the equation, and the three-way interaction of emotional abuse, affective dysfunction, and impulsivity entered in the final step of the equation.
The overall model was significant, accounting for 59% of the variance in childhood borderline personality symptoms, F(12, 212) = 28.05, p < .001 (see Table 3). As predicted, the two personality traits significantly predicted childhood BP features (above and beyond the covariates; FΔ[2, 217] = 80.76, p < .001). Further, both affective dysfunction and impulsivity accounted for a significant amount of unique variance in childhood BP features (βs = .63 and .11, respectively; ps < .05). However, contrary to predictions, the interaction of affective dysfunction and impulsivity did not account for a significant amount of additional variance in BP features above and beyond the main effects of these traits, FΔ (1, 216) = .03, p > .10.
Table 3.
Hierarchical Regression Analysis Exploring the Roles of Affective Dysfunction, Impulsivity, Emotional Abuse, and their Interactions in Childhood Borderline Personality Symptoms, Controlling for Internalizing and Externalizing Psychopathology (N = 225)
| Predictors | β | R2 (Adj. R2) | ΔR2 | F |
|---|---|---|---|---|
| Step 1 | .27 (.25) | .27*** | 15.77** | |
| Depression symptom severity | .06 | |||
| Anxiety symptom severity | .15 | |||
| Delinquent behaviors | .03 | |||
| Oppositional defiant disorder | .26*** | |||
| Conduct disorder | .26*** | |||
| Step 2 | .58 (.57) | .31*** | 42.55*** | |
| Affective dysfunction | .63*** | |||
| Impulsivity | .11* | |||
| Step 3 | .58 (.56) | .00 | 37.07*** | |
| Affective dysfunction × Impulsivity | .01 | |||
| Step 4 | .60 (.58) | .02** | 35.09*** | |
| Emotional abuse | .17** | |||
| Step 5 | .61 (.59) | .01* | 30.09*** | |
| Emotional abuse × Affective dysfunction | .13** | |||
| Emotional abuse × Impulsivity | −.00 | |||
| Step 6 | .61 (.59) | .01 | 28.05*** | |
| Emotional abuse × Affective dysfunction × Impulsivity | −.12 |
p < .05.
p < .01.
p< .001.
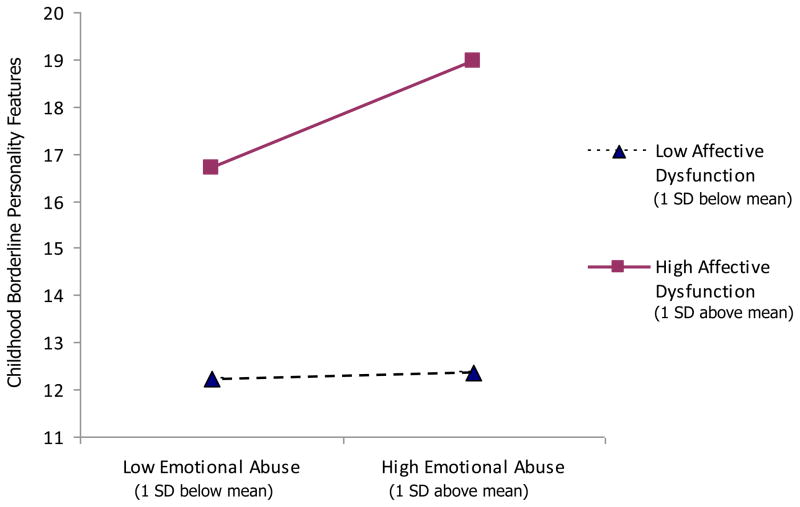
As for the role of the environmental stressor of interest in childhood BP features, emotional abuse accounted for a significant amount of unique variance in BP features above and beyond the personality traits, FΔ (1, 215) = 8.69, p < .01. Further, consistent with hypotheses, the step including the two-way interactions of emotional abuse with both affective dysfunction and impulsivity accounted for a significant amount of additional variance in BP features above and beyond the main effects of these factors, FΔ (2, 213) = 3.67, p < .05. However, only the interaction between emotional abuse and affective dysfunction accounted for a significant amount of unique variance in childhood BP features (above and beyond the covariates and main effects of these risk factors; see Figure 1); the interaction of emotional abuse and impulsivity was not significant (β = −.00, p > .10).1 Finally, the three-way interaction of emotional abuse, affective dysfunction, and impulsivity did not account for a significant amount of additional variance in BP features above and beyond the main effects and two-way interactions of these factors, FΔ (1, 212) = 2.80, p > .05.
Figure 1.
Interactive effect of affective dysfunction and emotional abuse on childhood borderline personality features (N = 225).
The significant interaction was explored following methods outlined by Aiken and West (1991). First, the regression lines were plotted at high (one SD above the mean) and low (one SD below the mean) levels of affective dysfunction and emotional abuse, and then follow-up tests were conducted to examine whether the slopes of the regression lines differed significantly from zero. These tests revealed that the relationship between emotional abuse and BP features increased in magnitude as affective dysfunction moved from low (b = .07, t = .21, ns) to high (b = 1.13, t= 3.68, p < .001; see Figure 1).
Discussion
Despite the growing body of research examining the prognosis, course, consequences, and correlates of BPD in adults, little is known about the emergence of BP pathology in youth, or the factors associated with childhood BP features (Crick et al., 2005; Paris, 2005). Thus, the goal of the present study was to examine the interrelations among two BPD-relevant personality traits (i.e., affective dysfunction and impulsivity), emotional abuse (an environmental stressor previously found to be strongly associated with BPD), and childhood BP features in a community sample of youth aged 11 to 14.
Consistent with a developmental psychopathology perspective, the current investigation examined multiple domains of influence in concert. In particular, drawing upon extant theoretical models of the pathogenesis of BPD (Crowell et al., 2009; Linehan, 1993; Zanarini & Frankenburg, 1997), this study examined the interaction of trait vulnerabilities and childhood maltreatment (in the form of emotional abuse) in childhood BP features. As hypothesized, both affective dysfunction and impulsivity were uniquely associated with childhood BP features, consistent with extant theoretical and empirical literature suggesting the relevance of these vulnerabilities in particular to BPD (Siever & Davis, 1991). However, findings provided no support for the hypothesized interaction of affective dysfunction and impulsivity in childhood BP features. Although these findings are contrary to extensive theoretical literature emphasizing the interaction of these traits in the development of BPD (Paris, 2005; Siever & Davis; Trull, 2001), they are consistent with more recent developmental models of the pathogenesis of BPD (e.g., Crowell et al., 2009), which highlight the independent contributions of affective dysfunction and impulsivity to the development of BP pathology among youth. Specifically, and consistent with the principle of equifinality, our findings suggest that affective dysfunction and impulsivity may independently predict childhood BP features.
Consistent with past research on BPD in adults (Bornovalova et al., 2006; Gratz et al., 2008), findings provided support for the role of emotional abuse in childhood BP features, with this environmental stressor accounting for unique variance in childhood BP features even after controlling for the trait vulnerabilities and internalizing and externalizing psychopathology. Moreover, consistent with extant theoretical models of the development of BPD (e.g., Linehan, 1993; Zanarini & Frankenburg, 1997), results provided support for the hypothesized interaction of trait vulnerabilities and emotional abuse in childhood BP features. Specifically, findings revealed that affective dysfunction moderated the relationship between emotional abuse and childhood BP features, with emotional abuse associated with BP features only among children with high (vs. low) levels of affective dysfunction. This finding is consistent with theoretical literature suggesting that childhood maltreatment leads to BP pathology only in the context of an underlying trait vulnerability (Paris, 2000). Although findings suggest that the trait of affective dysfunction in particular moderates the effects of emotional abuse on BP features in childhood, the absence of a significant interaction between impulsivity and emotional abuse may be due to the shared-method variance between the measures of affective dysfunction and BP features used in this study (the precise impact of which cannot be determined). Nonetheless, it is important to note that theoretical literature does provide some support for expecting that this particular vulnerability would moderate the association between this specific form of maltreatment and BP pathology (Linehan, 1993; Zanarini & Frankenburg, 2007), whereas impulsivity may moderate the association between other forms of maltreatment (e.g., physical abuse; Shields & Cicchetti, 1998; Westen et al., 1990) and BP pathology. Clearly, further research is needed to explore the precise interactions within and across individual and environmental risk factors associated with BP features in childhood.
Although interesting, findings must be considered in light of limitations present. First, this study used correlational data and a cross-sectional design to examine questions pertaining to the development of BP features in childhood. As such, it is possible that the direction or temporal order of these relationships differs from our predictions. Prospective, longitudinal studies are needed to address these limitations and more fully examine these relationships. Further, our exclusive focus on emotional abuse provides no way of assessing the unique association between this form of maltreatment and childhood BP features. Although past research has provided support for the unique role of emotional abuse in particular to BP pathology in adolescence and adulthood (Gratz et al., 2008; Johnson et al., 2001), future studies are needed to examine the extent to which experiences of emotional abuse are uniquely associated with BP features in childhood.
An additional limitation is the use of only self- and caregiver-report measures. Given limitations associated with the exclusive use of self-report measures, future studies would benefit from a more expanded use of behavioral, biological, and/or psychophysiological measures of the key constructs examined here. Moreover, the self-report nature of our measure of emotional abuse provides no way to substantiate the actual occurrence of this abuse and introduces the possibility of self-report bias. Likewise, the format and brevity of this measure prohibits examination of certain facets of emotional abuse that may be particularly relevant to BP features, such as the severity and duration of the abuse and the relationship of the child to the perpetrator. However, it is important to note that our measure of emotional abuse does provide an assessment of the frequency of the abuse (a dimension of abuse found to be associated with greater difficulties; see Jasinski, Williams, & Siegel, 2000), and has been found to be significantly correlated with therapists’ independent ratings of emotional abuse among adolescent inpatients (Bernstein et al., 2003). Nonetheless, future studies of the relation between emotional abuse and BP features among children would benefit from a more comprehensive and objective assessment of emotional abuse, including the independent verification of abuse history.
Furthermore, due to the preliminary nature of this particular research question, as well as concerns regarding participant burden (as most of the measures of interest here were added to an already lengthy assessment battery of the mechanisms underlying HIV-related risk behaviors partway through data collection), it was not possible to include comprehensive assessments of all of the constructs of interest; thus, most were assessed through either caregiver-report or child-report only. The exclusive reliance on caregiver reports of children’s affective dysfunction and BP features may have limited our ability to obtain a complete picture of these phenomena. It is possible that some caregivers may not have had access to the personal experiences of their children, thereby limiting their ability to accurately report on certain aspects of key constructs, particularly less publicly observable phenomena such as fears of abandonment or behaviors that are often kept hidden from others (e.g., self-harm). Indeed, given evidence that many adults with BPD report a history of self-harm in childhood or adolescence (Zanarini et al., 2006), the absence of a comprehensive assessment of this behavior (and possible underestimation of the full extent of this behavior among the youth in this study) is a particular concern, and has implications for the validity of our BP assessment. Nonetheless, it is important to note that the rate of self-harm/suicidal behaviors reported by the caregivers in this sample (i.e., 5.3%) is well within the range reported by youth themselves, as past-year rates of self-reported self-harm and suicidal behaviors among children in this age range vary from 2.5% to 12.5% (Jacobson & Gould, 2007) and tend to fall between 4% to 7% (De Leo & Heller, 2004; Hilt, Nock, Lloyd-Richardson, & Prinstein, 2008; Madge et al., 2008; Patton et al., 2007; Ystgaard, Reinholdt, Husby, & Mehlum, 2003). Thus, there is some evidence to suggest that the mothers in this study may have been at least somewhat aware of their children’s self-harm and suicidal behaviors.
Further, providing support for our use of a caregiver-report measure of childhood BP features specifically, researchers have raised concerns about the validity of self-report measures of personality pathology (one feature of which may be limited awareness of one’s behaviors and their effects on others), particularly among youth (Westen & Chang, 2000), suggesting the importance of incorporating other-report measures of personality disorder features into studies of personality pathology (Oltmanns & Turkheimer, 2006; for a discussion of this issue, see Beauchaine et al., 2009). Likewise, researchers have suggested that caregivers are better informants than youth themselves on issues where normative comparisons are needed (see Cohen & Crawford, 2005), as in the case of the assessment of BP features here (which requires caregivers to compare their child’s behavior to that of other children, so as not to pathologize developmentally appropriate behaviors; Coolidge, 2005). Nonetheless, future research would benefit from more comprehensive assessments of BP features, including child-report measures of both BP features and behaviors that may be considered developmental precursors of BPD, such as self-harm (see Beauchaine et al.; Crowell, Beauchaine, & Lenzenweger, 2008).
Additionally, given that most of the constructs of interest were assessed through either caregiver-report or child-report only, it is important to note that method variance (i.e., caregiver- vs. child-report measures) may explain the differential strength of the relationships between affective dysfunction and BP features on the one hand (both of which were assessed with caregiver-report measures) and impulsivity and BP features on the other (the former of which was assessed through a child-report measure), as well as the failure to find a significant interaction between affective dysfunction and impulsivity in the prediction of caregiver-reported BP features. In the absence of both caregiver- and child-report measures of the same constructs, there is no way to determine the extent to which method variance or reporter bias influenced our findings. However, in light of this design, findings of a unique association between both trait impulsivity and emotional abuse (assessed via child-report measures) and BP features (assessed via a caregiver-report measure) are particularly notable, as they cannot be accounted for by shared method variance and, thus, arguably represent a more conservative test of these associations. Nonetheless, it will be important for future studies to combine caregiver-report measures with child self-report measures of key constructs. Such an approach will facilitate the systematic assessment of discrepancies in how caregivers and children perceive the measured traits, environmental stressors, and childhood BP features, and will clarify the strength of the interrelationships between these constructs.
Limitations with regard to the generalizability of the results also warrant mention. Although our use of an ethnically diverse mixed-gender sample increases the generalizability of our findings, our sample was relatively well-educated and financially secure. Thus, findings cannot be assumed to generalize to lower SES samples and require replication within a more socioeconomically diverse community sample. However, it is important to note that past research has not found evidence of a significant association between SES indices (e.g., income and education) and BP pathology in children or adults (Bornovalova et al., 2008; Gratz, Rosenthal, Tull, Lejuez, & Gunderson, 2006; Gratz et al., 2009), and levels of childhood BP features were not significantly associated with family income in the present sample.
Additionally, it should be noted that although we found evidence for unique associations between impulsivity, affective dysfunction, emotional abuse, and BP features, as well as the interactive effect of affective dysfunction and emotional abuse on BP features, we did not examine whether these factors distinguish BP features from other forms of psychopathology. Although findings of a significant relationship between the factors of interest here and BP features when controlling for anxiety and depression symptom severity, delinquent behaviors, and externalizing disorders provide evidence for a unique relationship between these putative risk factors and childhood BP features above and beyond general internalizing and externalizing psychopathology, future studies should examine the specificity of the model examined here to childhood BP features.
Further, future research should examine the relationships between childhood BP features and other trait vulnerabilities thought to be relevant to BPD, such as cognitive dysfunction. Indeed, although impulsivity and affective dysfunction (and their interaction) have been suggested to be particularly relevant to the development of BPD (Crowell et al., 2009; Siever & Davis, 1991; Trull, 2001), preliminary evidence provides support for the role of cognitive dysfunction in the pathogenesis of BPD as well (Judd, 2005; Livesley et al., 1998). Likewise, future studies should examine the role of other forms of maltreatment (such as neglect and sexual abuse), as well as other environmental risk factors in general (such as disruptions in attachment), in childhood BP features. In particular, studies should examine the extent to which various environmental risk (and protective) factors interact with BP-relevant personality traits to predict both childhood BP features and the varying adaptive and maladaptive trajectories of these features. Finally, it will be important for future research to continue to explore the influence of pertinent demographic factors on the nature, extent, and correlates of childhood BP features. Although findings from this study provided no evidence of an association between childhood BP features and a variety of potentially relevant demographic factors (including gender, age, family income, and ethnic/racial background), future research should examine the extent to which relevant demographic factors interact with one another to influence levels of BP features in childhood (see Crick et al., 2005, for preliminary findings to this effect).
Despite limitations, the present study provides further support for the applicability of extant models of the pathogenesis of BPD in adults to BP features in childhood, contributing to the burgeoning literature on the pathogenesis of BP pathology. This study represents the first empirical investigation of the interactive effect of trait vulnerabilities and environmental stressors on BP features in childhood, an interaction that is thought to be critical to the development of personality disorders in general, as well as BP pathology specifically. Findings provide support for the hypothesized moderating role of personality traits in the association between environmental stressors and BP features in childhood, suggesting that emotional abuse is associated with childhood BP features only among youth with high (vs. low) levels of affective dysfunction. In addition to furthering our understanding of the complex interrelationships of personality traits and environmental stressors in the development of BP pathology in general, the results of this study may assist in the identification of children at risk for the later development of personality disorders (including BPD), as well as co-occurring Axis I disorders. Thus, these findings have important implications for the development of secondary prevention programs, suggesting the utility of teaching vulnerable youth skills for effectively managing their emotions and behaviors (including strategies for regulating their emotions and controlling impulsive behaviors).
Acknowledgments
This research was supported by National Institute on Drug Abuse Grant R01 DA18647, awarded to C. W. Lejuez.
Footnotes
In order to examine further the moderating roles of affective dysfunction and impulsivity in the association between emotional abuse and childhood BP features, separate analyses were conducted to examine the interaction between emotional abuse and each of the personality traits of interest. Findings of these analyses were the same as those obtained in the full model including both interactions together. Specifically, whereas the interaction between emotional abuse and affective dysfunction accounted for a significant amount of unique variance in childhood BP features (above and beyond the main effects of these factors; FΔ[1, 219] = 6.37, β= .11, ps < .05), the interaction of emotional abuse and impulsivity was not significant, FΔ (1, 219) = 0.44, β = .05, ps > .10.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Kim L. Gratz, University of Mississippi Medical Center
Robert D. Latzman, University of Mississippi Medical Center
Matthew T. Tull, University of Mississippi Medical Center
Elizabeth K. Reynolds, Center for Addictions, Personality, and Emotion Research and the University of Maryland
C. W. Lejuez, Center for Addictions, Personality, and Emotion Research and the University of Maryland
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA: Sage Publishing; 1991. [Google Scholar]
- Aklin WM, Lejuez CW, Zvolensky MJ, Kahler CW, Gwadz M. Evaluation of behavioral measures of risk taking propensity with inner city adolescents. Behaviour Research and Therapy. 2005;43:215–228. doi: 10.1016/j.brat.2003.12.007. [DOI] [PubMed] [Google Scholar]
- Antrop I, Roeyers H, Oosterlaan J, Van Oost P. Agreement between parent and teacher ratings of disruptive behavior disorders in children with clinically diagnosed ADHD. Journal of Psychopathology and Behavioral Assessment. 2002;24:67–73. [Google Scholar]
- Arata CM, Langhinrichsen-Rohling J, Bowers D, O’Brien NO. Differential correlates of multi-type maltreatment among urban youth. Child Abuse & Neglect. 2007;31:393–415. doi: 10.1016/j.chiabu.2006.09.006. [DOI] [PubMed] [Google Scholar]
- Battle CL, Shea MT, Johnson DM, Yen S, Zlotnick C, Zanarini MC, Morey L. Childhood maltreatment associated with adult personality disorders: Findings from the collaborative longitudinal personality disorders study. Journal of Personality Disorders. 2004;18:193–211. doi: 10.1521/pedi.18.2.193.32777. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, Klein DN, Crowell SE, Derbidge CM, Gatzke-Kopp LM. Multifinality in the development of personality disorders: A Biology × Sex × Environment model of antisocial and borderline traits. Development and Psychopathology. 2009;21:735–770. doi: 10.1017/S0954579409000418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein DP, Ahluvalia T, Pogge D, Handelsman L. Validity of the Childhood Trauma Questionnaire in an adolescent psychiatric population. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:340–348. doi: 10.1097/00004583-199703000-00012. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, Zule W. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect. 2003;27:169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Bornovalova MA, Gratz KL, Daughters SB, Nick B, Delany-Brumsey A, Lynch TR, Lejuez CW. A multimodal assessment of the relationship between emotion dysregulation and borderline personality disorder among inner-city substance users in residential treatment. Journal of Psychiatric Research. 2008;42:717–726. doi: 10.1016/j.jpsychires.2007.07.014. [DOI] [PubMed] [Google Scholar]
- Bornovalova MA, Gratz KL, Delany-Brumsey A, Paulson A, Lejuez CW. Temperamental and environmental risk factors for borderline personality disorder among inner-city substance users in residential treatment. Journal of Personality Disorders. 2006;20:218–231. doi: 10.1521/pedi.2006.20.3.218. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. Contexts of child rearing: Problems and prospects. American Psychologist. 1979;34:844–850. [Google Scholar]
- Buckle SK, Lancaster S, Powell MB, Higgins DJ. The relationship between child sexual abuse and academic achievement in a sample of adolescent psychiatric inpatients. Child Abuse and Neglect. 2005;29:1031–1047. doi: 10.1016/j.chiabu.2004.12.013. [DOI] [PubMed] [Google Scholar]
- Caspi A, Roberts BW, Shiner RL. Personality development: Stability and change. Annual Review of Psychology. 2005;56:453–484. doi: 10.1146/annurev.psych.55.090902.141913. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control (CDC) Youth risk behavior surveillance system. Atlanta: Author; 2001. [Google Scholar]
- Chorpita BF, Moffitt CE, Gray J. Psychometric properties of the Revised Child Anxiety and Depression Scale in a clinical sample. Behaviour Research and Therapy. 2005;43:309–322. doi: 10.1016/j.brat.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Yim L, Moffitt C, Umemoto LA, Francis SE. Assessment of symptoms of DSM-IV anxiety and depression in children: A revised child anxiety and depression scale. Behaviour Research and Therapy. 2000;38:835–855. doi: 10.1016/s0005-7967(99)00130-8. [DOI] [PubMed] [Google Scholar]
- Cicchetti D. A multiple-levels-of-analysis perspective on research in developmental psychopathology. In: Beauchaine TP, Hinshaw SP, editors. Child psychopathology. Hoboken, NJ: Wiley; 2008. pp. 27–57. [Google Scholar]
- Cicchetti D, Cohen D. Developmental psychopathology: Risk, disorder, and adaptation. 2. Vol. 3. New York: Wiley; 2006. [Google Scholar]
- Cicchetti D, Lynch M. Toward an ecological/transactional model of community violence and child maltreatment: Consequences for children’s development. Psychiatry. 1993;53:96–118. doi: 10.1080/00332747.1993.11024624. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA. Equifinality and multifinality in developmental psychopathology. Development and Psychopathology. 1996;8:597–600. [Google Scholar]
- Cicchetti D, Rogosch FA. A developmental psychopathology perspective on adolescence. Journal of Consulting and Clinical Psychology. 2002;70:6–20. doi: 10.1037//0022-006x.70.1.6. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Toth SL. The past achievements and future promises of developmental psychopathology: The coming of age of a discipline. The Journal of Child and Adolescent Psychiatry. 2009;50:16–25. doi: 10.1111/j.1469-7610.2008.01979.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen P, Chen H, Crawford TN, Brook JS, Gordon K. Personality disorders in early adolescence and the development of later substance use disorders in the general population. Drug and Alcohol Dependence. 2007;88:S71–S84. doi: 10.1016/j.drugalcdep.2006.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen P, Crawford TN. Developmental issues. In: Oldham JM, Skodol AE, Bender DS, editors. The textbook of personality disorders. Washington, DC: American Psychiatric Publishing; 2005. pp. 171–185. [Google Scholar]
- Coolidge FL. Coolidge Personality and Neuropsychological Inventory for Children Manual: CPNI. Colorado Springs: Author; 2005. [Google Scholar]
- Coolidge FL, Segal DL, Stewart SE, Ellett JA. Neuropsychological dysfunction in children with borderline personality disorder features: A preliminary investigation. Journal of Research in Personality. 2000;34:554–561. [Google Scholar]
- Coolidge FL, Thede LL. Heritability and the comorbidity of ADHD with behavioral disorders and executive function deficits: A preliminary investigation. Developmental Neuropsychology. 2000;17:273–287. doi: 10.1207/S15326942DN1703_1. [DOI] [PubMed] [Google Scholar]
- Coolidge FL, Thede LL, Jang KL. Heritability of childhood personality disorders: A preliminary study. Journal of Personality Disorders. 2001;15:33–40. doi: 10.1521/pedi.15.1.33.18645. [DOI] [PubMed] [Google Scholar]
- Coolidge FL, Thede LL, Stewart SE, Segal DL. The Coolidge Personality and Neuropsychological Inventory for Children (CPNI): Preliminary psychometric characteristics. Behavior Modification. 2002;26:550–566. doi: 10.1177/0145445502026004007. [DOI] [PubMed] [Google Scholar]
- Crick NR, Murray-Close D, Woods K. Borderline personality features in childhood: A short-term longitudinal study. Development and Psychopathology. 2005;17:1051–1070. [PubMed] [Google Scholar]
- Crowell SE, Beauchaine TP, Lenzenwger MF. The development of borderline personality disorder and self-injurious behavior. In: Beauchaine TP, Hinshaw SP, editors. Child and adolescent psychopathology. Hoboken, NJ: Wiley; 2008. pp. 510–539. [Google Scholar]
- Crowell SE, Beauchaine TP, Linehan M. The development of borderline personality: Extending Linehan’s model. Psychological Bulletin. 2009;135:495–510. doi: 10.1037/a0015616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Leo D, Heller TS. Who are the kids who self-harm? An Australian self-report school survey. The Medical Journal of Australia. 2004;181:140–144. doi: 10.5694/j.1326-5377.2004.tb06204.x. [DOI] [PubMed] [Google Scholar]
- Donegan NH, Sanislow CA, Blumberg HP, Fulbright RK, Lacadie C, Skudlarski P, Wexler BE. Amygdala hyperreactivity in borderline personality disorder: Implications for emotional dysregulation. Biological Psychiatry. 2003;54:1284–1293. doi: 10.1016/s0006-3223(03)00636-x. [DOI] [PubMed] [Google Scholar]
- Eysenck SBG. The I7: Development of a measure of impulsivity and its relationship to the superfactors of personality. In: McCown WG, Johnson JL, Shure MB, editors. The impulsive client: Theory, research, and treatment. Washington, DC: American Psychological Association; 1993. pp. 141–149. [Google Scholar]
- Eysenck SBG, Pearson PR, Easting G, Allsopp JF. Age norms for impulsiveness, venturesomeness, and empathy in adults. Personality and Individual Differences. 1985;6:613–619. [Google Scholar]
- Feinberg ME, Greenberg MT, Osgood DW, Sartorius J, Bontempo D. Effects of the communities that care model in Pennsylvania on youth risk and problem behaviors. Preventative Science. 2007;8:261–270. doi: 10.1007/s11121-007-0073-6. [DOI] [PubMed] [Google Scholar]
- Gibb BE, Abela JRZ. Emotional abuse, verbal victimization, and the development of children’s negative inferential styles and depressive symptoms. Cognitive Therapy and Research. 2008;32:161–176. [Google Scholar]
- Goldman SJ, D’Angelo EJ, DeMaso DR, Mezzacappa E. Physical and sexual abuse histories among childrenwith borderline personality disorder. American Journal of Psychiatry. 1992;149:1723–1726. doi: 10.1176/ajp.149.12.1723. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Rosenthal MZ, Tull MT, Lejuez CW, Gunderson JG. An experimental investigation of emotion dysregulation in borderline personality disorder. Journal of Abnormal Psychology. 2006;115:850–855. doi: 10.1037/0021-843X.115.4.850. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Rosenthal MZ, Tull MT, Lejuez CW, Gunderson JG. An experimental investigation of emotional reactivity and delayed emotional recovery in borderline personality disorder: The role of shame. Comprehensive Psychiatry. 2010;51:275–285. doi: 10.1016/j.comppsych.2009.08.005. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Tull MT, Baruch DE, Bornovalova MA, Lejuez CW. Factors associated with co-occurring borderline personality disorder among inner-city substance users: The roles of childhood maltreatment, negative affect intensity/reactivity, and emotion dysregulation. Comprehensive Psychiatry. 2008;49:603–615. doi: 10.1016/j.comppsych.2008.04.005. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Tull MT, Reynolds EK, Bagge C, Latzman RD, Daughters SB, Lejuez CW. Extending extant models of the pathogenesis of borderline personality disorder to childhood borderline personality symptoms: The roles of affective dysfunction, disinhibition, and self- and emotion-regulation deficits. Development and Psychopathology. 2009;21:1263–1291. doi: 10.1017/S0954579409990150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenman DA, Gunderson JG, Cane M, Saltzman PR. An examination of the borderline diagnosis in children. American Journal of Psychiatry. 1986;143:998–1003. doi: 10.1176/ajp.143.8.998. [DOI] [PubMed] [Google Scholar]
- Guzder J, Paris J, Zelkowitz P, Feldman R. Psychological risk factors for borderline pathology in school-age children. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:206–212. doi: 10.1097/00004583-199902000-00021. [DOI] [PubMed] [Google Scholar]
- Guzder J, Paris J, Zelkowitz P, Marchessault K. Risk factors for borderline psychology in children. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:26–33. doi: 10.1097/00004583-199601000-00009. [DOI] [PubMed] [Google Scholar]
- Hartup WW, van Lieshout CF. Personality development in social context. Annual Review of Psychology. 1995;46:655–687. doi: 10.1146/annurev.ps.46.020195.003255. [DOI] [PubMed] [Google Scholar]
- Henry C, Mitropoulou V, New AS, Koenigsberg HW, Silverman J, Siever LJ. Affective instability and impulsivity in borderline personality and bipolar II disorders: Similarities and differences. Journal of Psychiatric Research. 2001;35:307–312. doi: 10.1016/s0022-3956(01)00038-3. [DOI] [PubMed] [Google Scholar]
- Herpertz SC, Dietrich TM, Wenning B, Krings T, Erberich SG, Willmes K, Sass H. Evidence of abnormal amygdala functioning in borderline personality disorder: A functional MRI study. Biological Psychiatry. 2001;50:292–298. doi: 10.1016/s0006-3223(01)01075-7. [DOI] [PubMed] [Google Scholar]
- Hilt LM, Nock MK, Lloyd-Richardson EE, Prinstein MJ. Longitundinal study of nonsuicidal self-injury among young adolescents. Journal of Early Adolescence. 2008;28:455–469. [Google Scholar]
- Hochhausen NM, Lorenz AR, Newman JP. Specifying the impulsivity of female inmates with borderline personality disorder. Journal of Abnormal Psychology. 2002;111:495–501. [PubMed] [Google Scholar]
- Jacobson CM, Gould M. The epidemiology and phenomenology of non-suicidal self-injurious behavior among adolescents: A critical review of the literature. Archives of Suicide Research. 2007;11:129–147. doi: 10.1080/13811110701247602. [DOI] [PubMed] [Google Scholar]
- Jasinski JL, Williams LM, Siegel J. Childhood physical and sexual abuse as risk factors for heavy drinking among African-American women: A prospective study. Child Abuse and Neglect. 2000;24:1061–1071. doi: 10.1016/s0145-2134(00)00158-7. [DOI] [PubMed] [Google Scholar]
- Johnson JK, Cohen P, Smailes EM, Skodol AE, Brown J, Oldham JN. Childhood verbal abuse and risk for personality disorders during adolescence and early adulthood. Comprehensive Psychiatry. 2001;42:16–23. doi: 10.1053/comp.2001.19755. [DOI] [PubMed] [Google Scholar]
- Judd PH. Neurocognitive impairment as a moderator in the development of borderline personality disorder. Development and Psychopathology. 2005;17:1173–1196. doi: 10.1017/s0954579405050558. [DOI] [PubMed] [Google Scholar]
- Kilpatrick T, Joyce E, Milton J, Duggan C, Tyrer P, Rogers RD. Altered emotional decision-making in prisoners with borderline personality disorder. Journal of Personality Disorders. 2007;21:243–261. doi: 10.1521/pedi.2007.21.3.243. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and practices of structural equation modeling. New York: Guilford Press; 1998. [Google Scholar]
- Koenigsberg HW, Harvey PD, Mitropoulou V, Schmeidler J, New AS, Goodman M, et al. Characterizing affective instability in borderline personality disorder. American Journal of Psychiatry. 2002;159:784–788. doi: 10.1176/appi.ajp.159.5.784. [DOI] [PubMed] [Google Scholar]
- Kristensen H, Torgersen S. The association between avoidant personality traits and motor impairment in a population-based sample of 11–12 year-old children. Journal of Personality Disorders. 2007;21:87–97. doi: 10.1521/pedi.2007.21.1.87. [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Aklin W, Daughters S, Zvolensky MJ, Kahler CW, Gwadz M. Reliability and validity of the youth version of the Balloon Analogue Risk Task (BART-Y) in the assessment of risk-taking behavior among inner-city adolescents. Journal of Clinical Child and Adolescent Psychology. 2007;36:106–111. doi: 10.1080/15374410709336573. [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Aklin WM, Zvolensky MJ, Pedulla CM. Evaluation of the Balloon Analogue Risk Task (BART) as a predictor of adolescent real-world risk-taking behaviors. Journal of Adolescence. 2003;26:475–479. doi: 10.1016/s0140-1971(03)00036-8. [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF, Lane MC, Loranger AW, Kessler RC. DSM-IV personality disorders in the National Comorbidity Survey Replication. Biological Psychiatry. 2007;62:553–564. doi: 10.1016/j.biopsych.2006.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. New York: Guilford Press; 1993. [Google Scholar]
- Links PS, Heslegrave R, van Reekum R. Impulsivity: Core aspect of borderline personality disorder. Journal of Personality Disorders. 1999;13:1–9. doi: 10.1521/pedi.1999.13.1.1. [DOI] [PubMed] [Google Scholar]
- Livesley WJ, Jang KL, Vernon PA. Phenotypic and genetic structure of traits delineating personality disorder. Archives of General Psychiatry. 1998;55:941–948. doi: 10.1001/archpsyc.55.10.941. [DOI] [PubMed] [Google Scholar]
- MacPherson L, Reynolds EK, Daughters SB, Wang F, Cassidy J, Mayes LC, Lejuez’ CW. Positive and Negative Reinforcement Underlying Risk Behavior in Early Adolescents. Prevention Science. 2010;11:331–342. doi: 10.1007/s11121-010-0172-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madge N, Hewitt A, Hawton K, Jan de Wilde E, Corcoran P, et al. Deliberate self harm within an international community sample of young people: Comparative findings from the Child & Adolescent Self-harm in Europe (CASE) study. Journal of Child Psychology and Psychiatry. 2008;49:667–677. doi: 10.1111/j.1469-7610.2008.01879.x. [DOI] [PubMed] [Google Scholar]
- Nigg JT, Silk KR, Stavro G, Miller T. Disinhibition and borderline personality disorder. Development and Psychopathology. 2005;17:1129–1149. doi: 10.1017/s0954579405050534. [DOI] [PubMed] [Google Scholar]
- Ogata SN, Silk KR, Goodrich S, Lohr NE, Westen D, Hill EM. Childhood sexual and physical abuse in adult patients with borderline personality disorder. American Journal of Psychiatry. 1990;147:1008–1013. doi: 10.1176/ajp.147.8.1008. [DOI] [PubMed] [Google Scholar]
- Oltmanns TF, Turkheimer E. Perceptions of self and others regarding pathological personality traits. In: Krueger RF, Tackett J, editors. Personality and psychopathology: Building bridges. New York: Guilford Press; 2006. pp. 71–111. [Google Scholar]
- Oosterlaan J, Scheres A, Sergeant JA. Which executive functioning deficits are associated with AD/HD, ODD/CD, and comorbid AD/HD+ODD/CD. Journal of Abnormal Child Psychology. 2005;33:69–85. doi: 10.1007/s10802-005-0935-y. [DOI] [PubMed] [Google Scholar]
- Paris J. Childhood precursors of borderline personality disorder. Psychiatric Clinics of North America. 2000;23:77–88. doi: 10.1016/s0193-953x(05)70144-1. [DOI] [PubMed] [Google Scholar]
- Paris J. The development of impulsivity and suicidality in borderline personality disorder. Development and Psychopathology. 2005;17:1091–1104. doi: 10.1017/s0954579405050510. [DOI] [PubMed] [Google Scholar]
- Paris J, Zelkowitz P, Guzder J, Joseph S, Feldman R. Neuropsychological factors associated with borderline pathology in children. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:770–774. [PubMed] [Google Scholar]
- Patton GC, Hemphill SA, Beyers JM, Bond L, Toumbourou JW, McMorris BJ, Catalano RF. Pubertal stage and deliberate self-harm in adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:508–514. doi: 10.1097/chi.0b013e31803065c7. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Gnagy EM, Greenslade KE, Milich R. Teacher ratings of DSM-III-R symptoms of the disruptive behavior disorders. Journal of American Academy of Child & Adolescent Psychiatry. 1992;31:210–218. doi: 10.1097/00004583-199203000-00006. [DOI] [PubMed] [Google Scholar]
- Pillow DR, Pelham WE, Hoza B, Molina BSG, Stultz CH. Confirmatory factor analysis examining attention deficit hyperactivity disorder symptoms and other childhood disruptive behaviors. Journal of Abnormal Child Psychology. 1998;26:293–309. doi: 10.1023/a:1022658618368. [DOI] [PubMed] [Google Scholar]
- Pukrop R. Dimensional personality profiles of borderline personality disorder in comparison with other personality disorders and healthy controls. Journal of Personality Disorders. 2002;16:135–147. doi: 10.1521/pedi.16.2.135.22550. [DOI] [PubMed] [Google Scholar]
- Reich DB, Zanarini MC. Developmental aspects of borderline personality disorder. Harvard Review of Psychiatry. 2001;9:294–301. doi: 10.1080/10673220127909. [DOI] [PubMed] [Google Scholar]
- Reist C, Haier RJ, DeMet E, Chicz-DeMet A. Platelet MAO activity in personality disorders and normal controls. Psychiatry Research. 1990;33:221–227. doi: 10.1016/0165-1781(90)90039-8. [DOI] [PubMed] [Google Scholar]
- Rogosch FA, Cicchetti D. Child maltreatment, attention networks, and potential precursors to borderline personality disorder. Development and Psychopathology. 2005;17:1071–1089. doi: 10.1017/s0954579405050509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter M. Connections between child and adult psychopathology. European Child and Adolescent Psychiatry. 1996;5(Suppl 1):4–7. doi: 10.1007/BF00538535. [DOI] [PubMed] [Google Scholar]
- Shields AM, Cicchetti D. Reactive aggression among maltreated children: The contributions of attention and emotion dysregulation. Journal of Clinical Child Psychology. 1998;27:381–395. doi: 10.1207/s15374424jccp2704_2. [DOI] [PubMed] [Google Scholar]
- Shiner RL. A developmental perspective on personality disorders: Lessons from research on normal personality development in childhood and adolescence. Journal of Personality Disorders. 2005;19:202–210. doi: 10.1521/pedi.19.2.202.62630. [DOI] [PubMed] [Google Scholar]
- Siever LJ, Davis KL. A psychobiological perspective on the personality disorders. American Journal of Psychiatry. 1991;148:1647–1658. doi: 10.1176/ajp.148.12.1647. [DOI] [PubMed] [Google Scholar]
- Skodol AE, Gunderson JG, Pfohl B, Widiger TA, Livesley WJ, Siever LJ. The borderline diagnosis I: Psychopathology, comorbidity, and personality structure. Biological Psychiatry. 2002;51:936–950. doi: 10.1016/s0006-3223(02)01324-0. [DOI] [PubMed] [Google Scholar]
- Skodol AE, Gunderson JG, Shea MT, McGlashan TH, Morey LC, Sanislow CA, et al. The Collaborative Longitudinal Personality Disorders Study (CLPS): Overview and implications. Journal of Personality Disorders. 2005;19:487–504. doi: 10.1521/pedi.2005.19.5.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder S, Pitts WM. Characterizing anxiety in the DSM-III borderline personality disorder. Journal of Personality Disorders. 1988;2:93–101. [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. New York, NY: Harper Collins College Publishers; 1996. [Google Scholar]
- Torgersen S. Genetics of patients with borderline personality disorder. Psychiatric Clinics of North America. 2000;23:1–9. doi: 10.1016/s0193-953x(05)70139-8. [DOI] [PubMed] [Google Scholar]
- Torgersen S, Czajkowski N, Jacobson K, Reichborn-Kjennerud T, Røysamb E, Neale MC, Reichborn-Kjennerud T. Dimensional representations of DSM-IV cluster B personality disorders in a population-based sample of Norwegian twins: A multivariate study. Psychological Medicine. 2008;38:1–9. doi: 10.1017/S0033291708002924. [DOI] [PubMed] [Google Scholar]
- Torgersen S, Lygren S, Oien PA, Skre I, Onstad S, Edvardsen J, Kringler E. A twin study of personality disorders. Comprehensive Psychiatry. 2000;41:416–425. doi: 10.1053/comp.2000.16560. [DOI] [PubMed] [Google Scholar]
- Trull TJ. Structural relations between borderline personality disorder features and putative etiological correlates. Journal of Abnormal Psychology. 2001;110:471–481. doi: 10.1037//0021-843x.110.3.471. [DOI] [PubMed] [Google Scholar]
- Verheul R. Impulsivity in the diagnosis of borderline personality disorder. Position paper presented at the Phenotype Conference of the Borderline Personality Disorder Research Foundation; New York, NY. 2006. [Google Scholar]
- Westen D, Chang C. Personality pathology in adolescence: A review. Adolescent Psychiatry. 2000;25:61–100. [Google Scholar]
- Westen D, Ludolph P, Misle B, Ruffins S, Block J. Physical and sexual abuse in adolescent girls with borderline personality disorder. American Journal of Orthopsychiatry. 1990;60:55–66. doi: 10.1037/h0079175. [DOI] [PubMed] [Google Scholar]
- Widiger TA, Weissman MM. Epidemiology of borderline personality disorder. Hospital and Community Psychiatry. 1991;42:1015–1021. doi: 10.1176/ps.42.10.1015. [DOI] [PubMed] [Google Scholar]
- Work Group on Borderline Personality Disorder. Practice guideline for the treatment of patients with borderline personality disorder. American Journal of Psychiatry. 2001;158:1–52. [PubMed] [Google Scholar]
- Wright KD, Waschbusch DA, Frankland BW. Combining data from parent ratings and parent interview when assessing ADHD. Journal of Psychopathology and Behavioral Assessment. 2007;29:141–148. [Google Scholar]
- Wymbs BT, Pelham WE. Child effects on communication between parents of youth with and without attention deficit/hyperactivity disorder. Journal of Abnormal Psychology. 2010;119:366–375. doi: 10.1037/a0019034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ystgaard M, Reinholdt N, Husby J, Mehlum J. Deliberate self harm in adolescents. Norwegian Medical Journal. 2003;123:2241–2245. [PubMed] [Google Scholar]
- Zanarini MC. Borderline personality disorder as an impulse spectrum disorder. In: Paris J, editor. Borderline personality disorder: Etiology and treatment. Washington, DC: American Psychiatric Publishing; 1993. pp. 67–86. [Google Scholar]
- Zanarini MC. Childhood experiences associated with the development of borderline personality disorder. Psychiatric Clinics of North America. 2000;23:89–101. doi: 10.1016/s0193-953x(05)70145-3. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR. Pathways to the development of borderline personality disorder. Journal of Personality Disorders. 1997;11:93–104. doi: 10.1521/pedi.1997.11.1.93. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Khera GS, Bleichmar J. Treatment histories of borderline inpatients. Comprehensive Psychiatry. 2001;42:144–150. doi: 10.1053/comp.2001.19749. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Ridolfi ME, Jager-Hyman S, Hennen J, Gunderson JG. Reported childhood onset of self-mutilation among borderline patients. Journal of Personality Disorders. 2006;20:9–15. doi: 10.1521/pedi.2006.20.1.9. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Gunderson JG, Marino MF, Schwartz EO, Frankenburg FR. Psychiatric disorders in the families of borderline outpatients. In: Links PS, editor. Family environment and borderline personality disorder. Progress in psychiatry series. Washington, DC: American Psychiatric Association; 1990. pp. 69–84. [Google Scholar]
- Zanarini MC, Williams AA, Lewis RE, Reich RB, Soledad C, Vera MA, Frankenburg FR. Reported pathological childhood experiences associated with the development of borderline personality disorder. American Journal of Psychiatry. 1997;154:1101–1106. doi: 10.1176/ajp.154.8.1101. [DOI] [PubMed] [Google Scholar]
- Zelkowitz P, Paris J, Guzder J, Feldman R. Diathesis and stressors in borderline pathology of childhood: The role of neuropsychological risk and trauma. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:100–105. doi: 10.1097/00004583-200101000-00022. [DOI] [PubMed] [Google Scholar]