Abstract
Neurolymphomatosis (NL) is an extremely rare manifestation. Involvement of the cranial and peripheral nerves is an unusual manifestation of NL which is occasionally difficult to diagnose using conventional imaging modalities. A 45-year-old female in complete remission from primary breast lymphoma presented with multiple neurological symptoms. 18F-FDG PET/CT revealed multiple nodular hypermetabolic lesions along the cranial and peripheral nerves, which corresponded to the patient’s neurological symptoms. These findings suggest that 18F-FDG PET/CT successfully detects the infiltration of cranial and peripheral nerves by lymphoma.
Keywords: primary breast lymphoma, neurolymphomatosis, cranial nerves, peripheral nerves, fluorine-18-fluorodeoxyglucose positron emission tomography/computed tomography
Introduction
Primary breast lymphoma (PBL) is a rare condition which affects less than 1% of patients with non-Hodgkin’s lymphoma (NHL) and constitutes less than 2% of all extranodal NHLs (1). Neurolymphomatosis (NL) is a rare manifestation characterized by the infiltration of peripheral nerves, nerve roots, nervous plexuses or cranial nerves by malignant lymphocytes (2). Involvement of the cranial and peripheral nerves is an unusual manifestation of NL which is occasionally difficult to diagnose using conventional imaging modalities. 18F-FDG PET/CT is being increasingly used for the diagnosis and staging of NHL and it also appears to be a highly sensitive diagnostic method for facilitating the identification of NL (2). The present case report describes a patient in complete remission of PBL who demonstrated increasing uptake of 18F-FDG in the cranial and peripheral nerves, suggestive of NL. Informed consent was obtained from the patient prior to the study.
Case report
A 45-year-old female was admitted complaining of headache, impaired hearing on the right side, bilateral facial hypesthesia, decreased vision, diplopia, lumbodorsal pain and weakness in both inferior extremities. The patient had been diagnosed with stage IIb non-Hodgkin’s lymphoma in her left breast two years previously, which was identified as a CD20-positive diffuse large B cell phenotype following lumpectomy. A total of 8 cycles of R-CHOP chemotherapy led to complete remission. However, following 16 months, the patient developed multiple neurological symptoms. Cerebrospinal fluid (CSF) analysis revealed increased protein (325 mg/dl) and the cytology was positive for malignant lymphocytes. CSF tests for tuberculosis, viruses and fungi were negative.
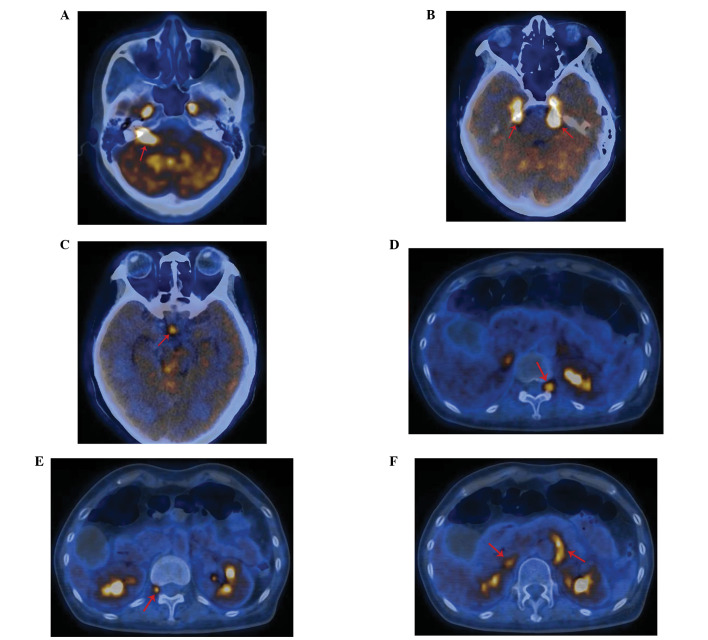
Whole body 18F-FDG PET/CT was performed to assess the extent of relapse. The patient fasted for at least 6 h prior to undergoing scanning and the fasting blood sugar level was <6.1 mmol/l. To prevent muscular radiotracer uptake, the patient was instructed to sit without speaking and avoid strenuous activity prior to the examination and following injection of the radioisotope. A standard dose of 18F-FDG 0.1 mCi/kg was intravenously injected 60 min prior to scanning. The data were acquired with a combined PET/CT in-line system (GE Discovery STE 16) with the following parameters: section thickness 3.75 mm, pitch 1.0 and FOV 70 cm. 18F-FDG PET/CT revealed multiple nodular or linear hypermetabolic lesions along the right acoustic nerve [maximum standardized uptake value (SUVmax), 7.98; Fig. 1A], bilateral trigeminal nerves (SUVmax, 8.91, 10.25; Fig. 1B), the optic chiasm (SUVmax, 4.73; Fig. 1C), the left nerve root of T11/12 (SUVmax, 4.79; Fig. 1D), the right nerve root of T12/L1 (SUVmax, 4.52; Fig. 1E) and the right adrenal gland (SUVmax, 4.05; Fig. 1F), while CT imaging revealed that the right adrenal gland and optic chiasm were normal. 18F-FDG PET/CT also revealed increased FDG uptake in the left retroperitoneal space (SUVmax, 5.48; Fig. 1F) where CT identified a strip-like soft tissue lesion between the left adrenal gland and abdominal aorta. Although a nerve biopsy was not performed, relapse of lymphoma and NL were diagnosed by 18F-FDG PET/CT and positive CSF cytology. The symptoms were markedly relieved following two cycles of R-CHOP chemotherapy.
Figure 1.
18F-FDG PET/CT images showing linear or nodular hypermetabolic lesions (red arrow) involving multiple cranial and peripheral nerves, corresponding to the patient’s complex neurological symptoms, including impaired hearing in the right side, bilateral facial hypesthesia, decreased vision, diplopia, lumbodorsal pain and weakness in both inferior extremities. 18F-FDG PET/CT showing increased 18F-FDG uptake along (A) the right acoustic nerve, (B) the bilateral trigeminal nerves and Meckel’s caves, (C) in the optic chiasm. 18F-FDG PET/CT showing increased 18F-FDG uptake in (D) the left nerve root of T11/12, (E) the right nerve root of T12/L1, (F) a strip-like soft tissue lesion between the left adrenal gland and abdominal aorta.
Discussion
PBL is used to define malignant lymphoma primarily occurring in the breast in the absence of previously detected lymphoma localizations. The most common type of PBL is the diffuse large B cell type. In this case, the patient, without a notable medical history, presented with a rapidly growing mass in the left breast. A systemic examination revealed no extramammary lymphoma and a lumpectomy was performed. Histopathological and immunohistochemical findings confirmed a diffuse large B cell type lymphoma.
NHL may involve the nervous system at every level, including the peripheral nerves, spinal nerve roots, spinal cord, meninges and brain. NL is a rare manifestation of malignant lymphoma in which the malignant lymphocytes infiltrate the peripheral nervous systems. NL is usually disclosed in proximal sites, including roots, spinal ganglia, nervous plexuses and proximal trunks (3). The involvement of the cranial and peripheral nerves in patients with PBL has rarely been documented. A study of 84 consecutive patients with PBL treated in 20 institutions identified that 12 patients suffered from a relapse in the central nervous system, but no patients presented with relapse in the peripheral nerves (4). In the present case, the chief complaints included multiple neurological symptoms, which were consistent with certain pathological changes in the nervous system. Further examinations were performed to assess the involvement of the nervous system and the extent of relapse.
Diagnosis of NL is often difficult and depends on the histopathological identification of infiltrating malignant lymphocytes in the affected nerves. However, nerve biopsy may yield false negative results despite the widespread lymphomatous infiltration of peripheral nerves (5). CSF cytological examination may lead to a false diagnosis since only a minority of NL cases reported present with positive CSF cytology at the initial diagnosis. Alternatively, imaging studies are of great value in diagnosing NL prior to histopathological confirmation. In the past, the imaging evaluation and follow-up of lymphoma patients was based solely on the findings from contrast-enhanced CT. However, contrast-enhanced CT has limited sensitivity in detecting lymphomatous involvement of normal-sized lymph nodes, bone marrow, spleen and extranodal tissues (6). Magnetic resonance imaging (MRI) is the most commonly used modality in the diagnosis and therapy of patients with lymphomatous infiltration of nerves. A retrospective study by Grisariu et al (2) of 50 patients with NL revealed that 18F-FDG PET/CT and MRI was positive in 84 and 77% of patients, respectively. While MRI typically shows the enlargement and enhancement of affected nerves, it does not always provide optimal visualization of lymphomatous involvement of peripheral nerves. In such cases, 18F-FDG PET/CT provides additional information that aids the correct identification of recurrence or exclusion of other diseases (7). In a previous systematic review, the overall sensitivity and specificity of 18F-FDG PET/CT for the initial staging of NHL and Hodgkin’s disease were 97 and 100%, respectively (8). A case report of NL on 18F-FDG PET/CT and MRI findings demonstrated that 18F-FDG PET/CT detected peripheral nerve infiltration by malignant lymphoma earlier than MRI (9). A study by Bronstein et al (10) indicated that 18F-FDG PET/CT is useful in diagnosing the malignant involvement of the peripheral nerves, particularly when findings from anatomical imaging (MRI or CT) are negative. The advanced technique of 18F-FDG PET/CT provides improved anatomical details of less commonly involved peripheral nerves, particularly in cases with NL. However, similar to MRI, 18F-FDG PET/CT also has diagnostic limitations. 18F-FDG uptake is highly sensitive for tumors but is not specific and may also be observed in any process where the rate of glycolysis is increased, including infection or neoplastic diseases. According to Hong et al (9) and Bronstein et al (10), the diagnosis of NHL required integrated clinical information from 18F-FDG PET/CT as well as CSF cytological examination.
In the present case, CT imaging revealed the enlargement of multiple cranial and peripheral nerves, while PET imaging revealed increased 18F-FDG uptake along these nerves. Subsequently, positive CSF cytology also aided the diagnosis of NL. The diagnosis was confirmed following careful integration of all the relevant clinical findings from 18F-FDG PET/CT and CSF cytological examination. The symptoms, including headache and lumbodorsal pain, were markedly relieved following two cycles of R-CHOP chemotherapy.
In cases of known treated malignancy involving the peripheral nerves, follow-up by 18F-FDG PET/CT has the advantage of high sensitivity in detecting local recurrence. Therefore, it is recommended that 18F-FDG PET/CT should be performed to evaluate the possibility of NL in patients with a history of lymphoma presenting with neurological symptoms.
References
- 1.Mason HS, Johari V, March DE, Crisi GM. Primary breast lymphoma: radiologic and pathologic findings. Breast J. 2005;11:495–496. doi: 10.1111/j.1075-122X.2005.00167.x. [DOI] [PubMed] [Google Scholar]
- 2.Grisariu S, Avni B, Batchelor TT, et al. Neurolymphomatosis: an International Primary CNS Lymphoma Collaborative Group report. Blood. 2010;115:5005–5011. doi: 10.1182/blood-2009-12-258210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kahraman S, Sabuncuoglu H, Gunhan O, Gurses MA, Sirin S. A rare reason of foot drop caused by primary diffuse large b-cell lymphoma of the sciatic nerve: case report. Acta Neurochir (Wien) 2010;152:125–128. doi: 10.1007/s00701-009-0339-9. [DOI] [PubMed] [Google Scholar]
- 4.Stefoni V, Broccoli A, Pellegrini C, Derenzini E, Fina M, Zinzani PL. CNS recurrence of primary mediastinal large b-cell lymphoma after complete remission. J Neurooncol. 2009;95:135–139. doi: 10.1007/s11060-009-9898-0. [DOI] [PubMed] [Google Scholar]
- 5.van den Bent MJ, de Bruin HG, Bos GM, Brutel de la Rivière G, Sillevis Smitt PA. Negative sural nerve biopsy in neurolymphomatosis. J Neurol. 1999;246:1159–1163. doi: 10.1007/s004150050535. [DOI] [PubMed] [Google Scholar]
- 6.Paes FM, Kalkanis DG, Sideras PA, Serafini AN. FDG PET/CT of extranodal involvement in non-Hodgkin lymphoma and Hodgkin disease. Radiographics. 2010;30:269–291. doi: 10.1148/rg.301095088. [DOI] [PubMed] [Google Scholar]
- 7.Palmedo H, Urbach H, Bender H, et al. FDG-PET in immunocompetent patients with primary central nervous system lymphoma: correlation with MRI and clinical follow-up. Eur J Nucl Med Mol Imaging. 2006;33:164–168. doi: 10.1007/s00259-005-1917-6. [DOI] [PubMed] [Google Scholar]
- 8.Even-Sapir E, Lievshitz G, Perry C, Herishanu Y, Lerman H, Metser U. Fluorine-18 fluorodeoxyglucose PET/CT patterns of extranodal involvement in patients with Non-Hodgkin lymphoma and Hodgkin’s disease. Radiol Clin North Am. 2007;45:697–709. vii. doi: 10.1016/j.rcl.2007.05.009. [DOI] [PubMed] [Google Scholar]
- 9.Hong CM, Lee S-W, Lee HJ, et al. Neurolymphomatosis on F-18 FDG PET/CT and MRI findings: A case report. Nucl Med Mol Imaging. 2011;45:76–78. doi: 10.1007/s13139-010-0070-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bronstein Y, Tummala S, Rohren E. F-18 FDG PET/CT for detection of malignant involvement of peripheral nerves: case series and literature review. Clin Nucl Med. 2011;36:96–100. doi: 10.1097/RLU.0b013e318203bb0e. [DOI] [PubMed] [Google Scholar]