Abstract
In addition to being a major cause of mortality in South Asia, childhood diarrhea creates economic burden for affected households. We used survey data from sites in Bangladesh, India, and Pakistan to estimate the costs borne by households due to childhood diarrhea, including direct medical costs, direct nonmedical costs, and productivity losses. Mean cost per episode was $1.82 in Bangladesh, $3.33 in India, and $6.47 in Pakistan. The majority of costs for households were associated with direct medical costs from treatment. Mean costs understate the distribution of costs, with 10% of cases exceeding $6.61, $8.07, and $10.11 in Bangladesh, India, and Pakistan, respectively. In all countries there was a trend toward lower costs among poorer households and in India and Pakistan there were lower costs for episodes among girls. For both poor children and girls this may reflect rationing of care, which may result in increased risks of mortality.
Diarrhea is a leading cause of child mortality in south Asia and globally, especially in low-income settings [1]. In addition to the health burden from mortality, diarrhea can have an important economic impact on the households of affected children and society as a whole. The economic costs to the healthcare system and governments can help offset the costs of interventions to reduce diarrheal morbidity and mortality, and there have been growing efforts to estimate these costs [2–8]. In addition, households themselves can bear a substantial economic burden due to the costs of treatment, other out-of-pocket expenses like transportation, and lost time from work. However, there is little empirical evidence of the magnitude of these costs to households.
Household economic costs of diarrhea episodes can have both an economic and a health impact [9–11]. First, they can reduce household resources for other activities, including productive investments, education, and food. Second, they can influence whether households seek care and how much they seek; that is, households—especially poor households—may avoid treatment due to the high cost, potentially exposing their children to higher risks of mortality. Given the high frequency of diarrhea among children in low-income settings, households are repeatedly balancing these health risks and economic costs.
This balance between household costs and health risks also interacts with important policy debates on user fees for treatment. Globally there has been a push to increase user fees for basic health services as a way to increase the financial sustainability of government-supported health systems. However, shifting costs of basic health services may result in households delaying or forgoing treatment [11, 12]. For example, Stanton and Clemens argued that instituting user fees in government health clinics in Bangladesh could have detrimental health impacts, via reductions in utilization, on some of the most medically vulnerable groups that utilize this system, namely, women, children, and the poor [13]. For health conditions like childhood diarrhea for which there are effective, low-cost solutions [14, 15], this may have adverse consequences [16–19].
We explore these issues within the context of 3 South Asian nations: Bangladesh, India, and Pakistan. We had 3 related objectives: (1) to estimate and characterize household costs associated with childhood diarrhea episodes by type and setting, (2) to explore how child and household characteristics alter cost patterns, and (3) explore how high costs can serve as a barrier to care or contribute to impoverishment of the household.
METHODS
This study uses data from the Global Enteric Multicenter Study (GEMS) of acute moderate-and-severe diarrhea in 3 Asian countries—Bangladesh, India, and Pakistan. Specifically, data come from the Healthcare Utilization and Attitudes Survey (HUAS). All 3 countries were chosen because of their relatively high rates of child mortality. Data were collected using a standardized interview from an age-stratified random sample of approximately 1000 households containing a child 0–59 months of age within each study area (described in [20]). Analyses were weighted based on the probability of selection. Each site aimed to enroll 400 infants 0–11 months of age, 370 children 12–23 months of age, and 370 children 24–59 months of age. For children aged 0–59 months who experienced a diarrheal episode in the previous 14 days, additional retrospective data were collected on household expenditures for medical care, other direct costs such as transportation, and time lost from paid work (indirect costs).
Sample sizes varied among countries. The initial household sampling was expected to be large enough to identify approximately 200 children with diarrhea in the previous 14 days and 150 children with household costs associated with the episodes. Based on World Health Organization methods for estimating diarrheal costs [15], this was expected to be sufficient to produce estimates of means with a confidence interval of +10% of the true mean with 80% power. The observed power in each country varies based on the variance in costs within each and the actual number of episodes. Sample sizes were not powered for secondary analyses to detect differences between subgroups. Sample sizes for each of the countries and subpopulations are provided in Table 1.
Table 1.
Study Population Characteristics and Subsamples
| Bangladesh |
India |
Pakistan |
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Children With Diarrhea | Children With Any Costs | Children With Direct Medical Costs | Children With Diarrhea | Children With Any Costs | Children With Direct Medical Costs | Children With Diarrhea | Children With Any Costs | Children With Direct Medical Costs | ||||||||||
| Sex | ||||||||||||||||||
| Male | 52 | (55) | 44 | (54) | 44 | (54) | 44 | (48) | 30 | (48) | 29 | (49) | 178 | (51) | 120 | (53) | 109 | (52) |
| Female | 43 | (45) | 37 | (46) | 37 | (46) | 48 | (52) | 32 | (52) | 30 | (51) | 171 | (49) | 107 | (47) | 100 | (48) |
| Education | ||||||||||||||||||
| None to primary | 31 | (33) | 25 | (31) | 25 | (31) | 36 | (39) | 22 | (36) | 20 | (34) | 211 | (61) | 139 | (61) | 128 | (61) |
| Finished primary | 50 | (53) | 43 | (53) | 43 | (53) | 41 | (45) | 32 | (52) | 31 | (53) | 34 | (10) | 26 | (12) | 26 | (12) |
| Some secondary | 14 | (15) | 13 | (16) | 13 | (16) | 14 | (15) | 7 | (11) | 7 | (12) | 20 | (6) | 12 | (5) | 12 | (6) |
| Religious only | … | … | … | … | … | … | 1 | (1) | 1 | (2) | 1 | (2) | 84 | (24) | 50 | (22) | 43 | (21) |
| Age | ||||||||||||||||||
| 0–11 mo | 36 | (38) | 32 | (40) | 32 | (40) | 42 | (46) | 31 | (50) | 30 | (51) | 154 | (44) | 107 | (47) | 98 | (47) |
| 12–23 mo | 39 | (41) | 32 | (40) | 32 | (40) | 26 | (28) | 17 | (27) | 17 | (29) | 117 | (34) | 71 | (31) | 65 | (31) |
| 24–59 mo | 20 | (21) | 17 | (21) | 17 | (21) | 24 | (26) | 14 | (23) | 12 | (20) | 78 | (22) | 49 | (22) | 46 | (22) |
| Severity | ||||||||||||||||||
| Mild | 22 | (23) | 18 | (22) | 18 | (22) | 26 | (28) | 13 | (21) | 13 | (22) | 55 | (16) | 31 | (14) | 27 | (13) |
| Moderate/severe | 73 | (77) | 63 | (78) | 63 | (78) | 66 | (72) | 49 | (79) | 46 | (78) | 294 | (84) | 196 | (86) | 182 | (87) |
| Duration | ||||||||||||||||||
| 1–3 d | 39 | (53) | 32 | (51) | 32 | (51) | 70 | (83) | 46 | (79) | 44 | (80) | 87 | (43) | 60 | (40) | 58 | (41) |
| 4–7 d | 25 | (34) | 23 | (37) | 23 | (37) | 10 | (12) | 8 | (14) | 8 | (15) | 86 | (43) | 67 | (45) | 63 | (45) |
| 8–14 d | 8 | (11) | 7 | (11) | 7 | (11) | 3 | (4) | 3 | (5) | 2 | (4) | 15 | (8) | 13 | (9) | 10 | (7) |
| ≥15 days | 1 | (1) | 1 | (2) | … | … | 1 | (1) | 1 | (2) | 1 | (2) | 13 | (7) | 9 | (6) | 9 | (6) |
All data are presented as no. (%).
We examined direct medical costs, direct nonmedical costs, indirect medical costs, and total costs per child for utilizing healthcare services to treat a given case of diarrhea, all of which are converted to US dollars. Direct medical costs were defined as either informal or formal expenditures, with the former representing care provided by a local healer or pharmacists and the latter combining both outpatient and inpatient care. Outpatient and inpatient facilities at each site are described in more detail in Levine et al [20], but outpatient facilities were primarily health centers and private doctors' offices, while inpatient facilities were primarily public district hospitals. Direct nonmedical costs were broken down by transportation and other costs, whereas indirect medical costs were either time costs or other costs. For both medical and total costs, some cases incur no costs and the remainder of episodes typically produced a right-skewed distribution. Descriptive statistics (means and standard errors) for costs are provided for all cases, those incurring medical or other costs, and the proportion incurring costs (Table 1). All costs were collected in local currencies, converted to US dollars, and then adjusted to 2011 as the reference year.
We also examined how child, household, and episode characteristics were associated with the costs incurred by households. This was analyzed separately for direct medical costs and total costs. Analysis of variance was used to assess the effect of household economic status, maternal education, child sex, age, duration of illness, and illness severity. Multivariate analysis was considered but not presented due to the limited sample size. This analysis was conducted separately for all episodes and those incurring medical or any costs. Logistic regression was used estimate the effect of these variables on the likelihood of costs being incurred by the household. Household economic status is based on an asset index calculated using principal components analysis using the full household sample for each country [21]. Maternal education was broken down into 4 categories: no formal or some primary education, completed primary education, some secondary, and religious education only. Due to the limited sample size and power, we considered P < .05 as statistically significant and P values between .05 and .20 as marginally significant.
Given the empirical evidence citing costs as a significant factor driving healthcare behavior and utilization, we examine the potential impact of costs on household impoverishment and avoidance of care owing to the economic costs. This is done by examining respondents' self-reported reasons for not seeking care and strategies for paying for the costs. In addition, we examine the distribution of costs to households and the possibility of large expenditures.
RESULTS
Expenditures by Type and Category
Among all diarrhea episodes, household costs ranged from $1.82 in Bangladesh to $6.47 per episode in India (Table 2). Among cases with nonzero costs, it was slightly higher, ranging from $2.13 in Bangladesh to $6.83 in Pakistan. In all 3 countries, direct medical costs exceeded direct nonmedical and indirect costs, accounting for 52% of costs per episode in Bangladesh, 51% in Pakistan, and 62% in India. Of these direct medical costs to households, in India and Pakistan, care in formal settings accounted for the majority (87% and 75%, respectively). In Bangladesh, formal costs were less than informal. In all 3 settings, the cost of medications far exceeded visits and diagnostic tests, accounting for 75% of the direct medical cost in India, 76% in Pakistan, and 81% in Bangladesh. Indirect costs from lost earnings amounted 30% of the household cost in India, 61% in Pakistan, and 35% in Bangladesh.
Table 2.
Household Costs Associated With Diarrheal Illness by Type and Setting (2011 US$) in Bangladesh, India, and Pakistan
| Bangladesh |
India |
Pakistan |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All Seeking Care | Std. Error | Incurring Any Treatment Cost | Std. Error | All Seeking Care | Std. Error | Incurring Any Treatment Cost | Std. Error | All Seeking Care | Std. Error | Incurring Any Treatment Cost | Std. Error | |
| Cost by type | n = 95 | n = 81 | n = 92 | n = 62 | n = 349 | n = 232 | ||||||
| Direct medical | 0.94 | 0.16 | 1.09 | 0.18 | 2.08 | 0.39 | 3.31 | 0.57 | 2.30 | 0.53 | 3.51 | 0.80 |
| Direct nonmedical | 0.25 | 0.07 | 0.29 | 0.08 | 0.25 | 0.07 | 0.40 | 0.11 | 0.25 | 0.07 | 0.37 | 0.11 |
| Total direct | 1.19 | 0.20 | 1.39 | 0.23 | 2.33 | 0.44 | 3.71 | 0.64 | 2.54 | 0.54 | 3.89 | 0.81 |
| Indirect cost | 0.63 | 0.22 | 0.74 | 0.26 | 1.00 | 0.25 | 1.60 | 0.36 | 3.93 | 2.07 | 2.94 | 0.77 |
| Total | 1.82 | 0.34 | 2.13 | 0.39 | 3.33 | 0.60 | 5.31 | 0.84 | 6.47 | 2.16 | 6.83 | 1.15 |
| Direct medical cost by setting | ||||||||||||
| Informal (healer, pharmacist) | 0.50 | 0.08 | 0.58 | 0.09 | 0.28 | 0.12 | 0.44 | 0.18 | 0.58 | 0.13 | 0.89 | 0.20 |
| Formal (hospital, clinic, office, etc) | 0.44 | 0.15 | 0.51 | 0.17 | 1.80 | 0.39 | 2.87 | 0.60 | 1.72 | 0.51 | 2.63 | 0.78 |
| Direct medical cost by purpose | ||||||||||||
| Consultation | 0.05 | 0.01 | 0.05 | 0.02 | 0.55 | 0.11 | 0.87 | 0.17 | 0.55 | 0.18 | 0.85 | 0.27 |
| Medication | 0.76 | 0.10 | 0.89 | 0.11 | 1.56 | 0.30 | 2.47 | 0.43 | 1.75 | 0.50 | 2.68 | 0.76 |
| Diagnostic tests | 0.12 | 0.09 | 0.14 | 0.11 | 0.05 | 0.03 | 0.07 | 0.05 | 0.02 | 0.01 | 0.03 | 0.02 |
In addition to mean costs, we examined the range and distribution of costs within each setting. Figure 1 shows the distribution of costs by wealth quintile. For each group, the box represents the 25th and 75th percentile and the bars show the 5th and 95th percentile. In Bangladesh, 25% of episodes (or all cases and all wealth quintiles) had total household costs in excess of $1.94, 10% exceeded $6.61, and 5% were greater than $10.44. In India the range was higher: 25% greater than $5.88, 10% greater than $8.07, and 5% greater than $12.22. Household costs were similar in Pakistan with 25% greater than $4.15, 10% greater than $10.11, and 5% greater than $18.29.
Figure 1.
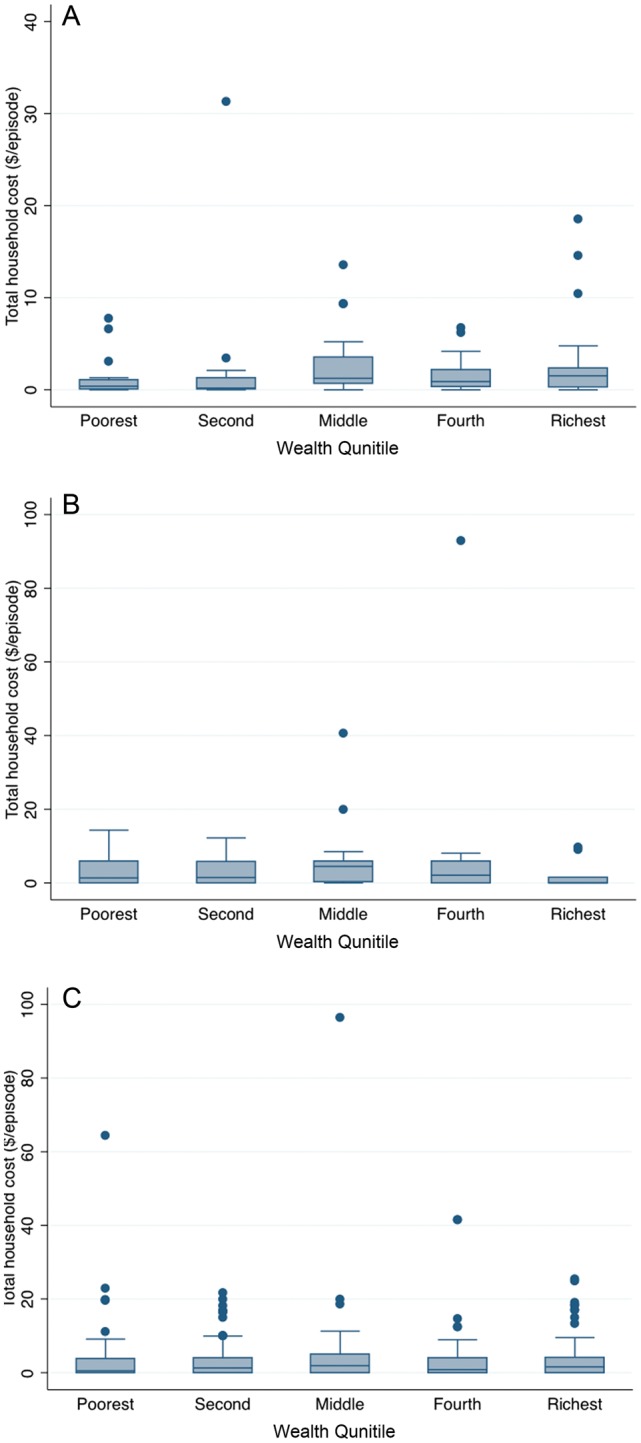
Distribution of total household diarrhea costs by wealth quintile ($ per episode) in (A) Bangladesh, (B) India, and (C) Pakistan.
Determinants of Costs
We examined the association between wealth, sex, education, age, severity, and duration and household direct medical costs and total costs (Tables 3 and 4). Both direct and total costs tend to be lower for children in the lowest wealth quintile in all 3 countries; however, with only marginal statistical significance. In Bangladesh, there is a trend toward increasing medical and total costs with wealth. In India, both types of costs take the form of an inverted U-shape, with costs increasing for the middle and fourth quintiles and then declining again for the richest. For Pakistan they are relatively consistent across wealth groups.
Table 3.
Household Direct Medical Costs for Childhood Diarrhea by Socioeconomic, Demographic, and Illness Characteristic in Bangladesh, India, and Pakistan
| Bangladesh |
India |
Pakistan |
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean Cost for All Episodes |
Proportion With Costs |
Mean Cost for Episodes With Costs |
Mean Cost for All Episodes |
Proportion With Costs |
Mean Cost for Episodes With Costs |
Mean Cost for All Episodes |
Proportion With Costs |
Mean Cost for Episodes With Costs |
||||||||||
| $ | ANOVA | P Value | $ | ANOVA | $ | ANOVA | P Value | $ | ANOVA | $ | ANOVA | P Value | $ | ANOVA | ||||
| Wealth quintile | ||||||||||||||||||
| Poorest | 1.00 | 0.61 | 1.65 | 0.99 | 0.40 | 2.47 | 1.35 | 0.53 | 2.55 | |||||||||
| Second | 0.53 | P = .41 | 0.93 | .02 | 0.57 | P = .41 | 1.92 | P = .56 | 0.72 | .13 | 2.89 | P = .60 | 1.47 | P = .08 | 0.68 | .11 | 2.24 | P = .12 |
| Middle | 1.19 | 0.96 | .02 | 1.24 | 3.48 | 0.81 | .02 | 4.85 | 2.81 | 0.65 | .26 | 4.24 | ||||||
| Fourth | 1.08 | 0.89 | .06 | 1.21 | 2.64 | 0.59 | .29 | 4.67 | 0.88 | 0.53 | 1 | 1.71 | ||||||
| Richest | 1.12 | 0.88 | .08 | 1.27 | 1.16 | 0.36 | .84 | 3.26 | 2.95 | 0.57 | .75 | 5.41 | ||||||
| Sex | ||||||||||||||||||
| Male | 0.71 | 0.86 | 0.82 | 2.13 | 0.54 | 4.20 | 2.1 | 0.61 | 3.61 | |||||||||
| Female | 1.30 | P = .13 | 0.85 | .92 | 1.53 | P = .13 | 2.03 | P = .46 | 0.60 | .67 | 3.54 | P = .50 | 1.53 | P = .44 | 0.58 | .64 | 2.65 | P = .36 |
| Education | ||||||||||||||||||
| None to primary | 0.66 | 0.83 | 0.8 | 1.20 | 0.50 | 2.64 | 1.32 | 0.6 | 2.2 | |||||||||
| Finished primary | 1.04 | P = .20 | 0.84 | .87 | 1.23 | P = .29 | 3.20 | P = .16 | 0.70 | .17 | 4.74 | P = .49 | 2.44 | P = .08 | 0.72 | .31 | 3.53 | P = .01 |
| Some secondary | 1.18 | 0.95 | .22 | 1.24 | 1.61 | 0.41 | .63 | 3.92 | 3.71 | 0.62 | .86 | 5.98 | ||||||
| Religious only | … | … | … | 3.54 | 1.00 | 3.54 | 2.58 | 0.53 | .37 | 5.33 | ||||||||
| Age | ||||||||||||||||||
| 0–11 mo | 1.01 | 0.9 | 1.13 | 4.80 | 0.71 | 6.97 | 2.77 | 0.64 | 4.36 | |||||||||
| 12–23 mo | 1.14 | P = .69 | 0.82 | .32 | 1.39 | P = .56 | 1.51 | P = .09 | 0.65 | .61 | 2.80 | P = .22 | 1.51 | P = .10 | 0.56 | .2 | 2.72 | P = .22 |
| 24–35 mo | 0.77 | 0.85 | .6 | 0.9 | 1.40 | 0.50 | .08 | 2.82 | 1.49 | 0.59 | .49 | 2.64 | ||||||
| Severity | ||||||||||||||||||
| Mild | 0.53 | 0.88 | 0.61 | 1.20 | 0.41 | 3.07 | 1.34 | 0.44 | 2.89 | |||||||||
| Moderate/severe | 1.07 | P = .07 | 0.85 | .68 | 1.27 | P = .08 | 2.33 | P = .25 | 0.62 | .16 | 3.97 | P = .50 | 1.89 | P = .53 | 0.62 | .04 | 3.17 | P = .74 |
| Duration | ||||||||||||||||||
| 1–3 d | 0.70 | 0.85 | 0.83 | 1.54 | 0.57 | 2.86 | 2.27 | 0.71 | 3.31 | |||||||||
| 4–7 d | 1.13 | P = .27 | 0.9 | .59 | 1.25 | P = .41 | 3.27 | P < .001 | 0.86 | .09 | 4.03 | P < .001 | 1.87 | P < .001 | 0.74 | .71 | 2.66 | P < .001 |
| 8–14 d | 0.78 | 0.92 | .56 | 0.85 | 11.64 | 0.26 | .31 | 44.01 | 1.42 | 0.5 | .19 | 2.82 | ||||||
| ≥15 days | 2.34 | 1 | 2.34 | 6.53 | 1.00 | 6.53 | 8 | 0.64 | .67 | 12.58 | ||||||||
Table 4.
Household Total Costs for Childhood Diarrhea by Socioeconomic, Demographic, and Illness Characteristic in Bangladesh, India, and Pakistan
| Bangladesh |
India |
Pakistan |
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean Cost for All Episodes |
Proportion With Costs |
Mean Cost for Episodes With Costs |
Mean Cost for All Episodes |
Proportion With Costs |
Mean Cost for Episodes With Costs |
Mean Cost for All Episodes |
Proportion With Costs |
Mean Cost for Episodes With Costs |
||||||||||
| $ | ANOVA | P Value | $ | ANOVA | $ | ANOVA | P Value | $ | ANOVA | $ | ANOVA | P Value | $ | ANOVA | ||||
| Wealth quintile | ||||||||||||||||||
| Poorest | 1.36 | 0.61 | 2.24 | 2.38 | 0.50 | 4.73 | 4.08 | 0.53 | 7.71 | |||||||||
| Second | 1.22 | P = .64 | 0.93 | .02 | 1.31 | P = .73 | 3.65 | P = .74 | 0.72 | .30 | 5.10 | P = .83 | 3.40 | P = .86 | 0.78 | .01 | 4.36 | P = .77 |
| Middle | 2.39 | 0.96 | .02 | 2.49 | 5.07 | 0.81 | .07 | 6.25 | 3.94 | 0.69 | .14 | 5.71 | ||||||
| Fourth | 1.89 | 0.89 | .06 | 2.11 | 3.63 | 0.66 | .36 | 5.46 | 4.35 | 0.64 | .28 | 6.72 | ||||||
| Richest | 2.68 | 0.88 | .08 | 3.04 | 1.38 | 0.36 | .52 | 3.87 | 4.19 | 0.56 | .81 | 7.39 | ||||||
| Sex | ||||||||||||||||||
| Male | 1.51 | 0.86 | 1.76 | 3.17 | 0.60 | 5.30 | 4.42 | 0.66 | 6.73 | |||||||||
| Female | 2.31 | P = .87 | 0.85 | .92 | 2.72 | P = .84 | 3.47 | P = .57 | 0.65 | .67 | 5.32 | P = .58 | 3.50 | P = .16 | 0.62 | .60 | 5.56 | P = .22 |
| Education | ||||||||||||||||||
| None to primary | 1.71 | 0.83 | 2.07 | 2.49 | 0.56 | 4.47 | 3.79 | 0.65 | 5.79 | |||||||||
| Finished primary | 1.44 | P = .17 | 0.84 | .87 | 1.70 | P = .20 | 4.69 | P = .23 | 0.76 | .15 | 6.18 | P = .51 | 4.91 | P = .54 | 0.72 | .57 | 6.76 | P = .48 |
| Some secondary | 3.26 | 0.95 | .22 | 3.42 | 1.72 | 0.41 | .42 | 4.17 | 4.81 | 0.62 | .78 | 7.75 | ||||||
| Religious only | 5.25 | 1.00 | 5.25 | 3.97 | 0.58 | .36 | 6.73 | |||||||||||
| Age | ||||||||||||||||||
| 0–11 mo | 2.74 | 0.90 | 3.04 | 6.98 | 0.74 | 9.47 | 4.30 | 0.70 | 6.14 | |||||||||
| 12–23 mo | 2.09 | P = .37 | 0.82 | .32 | 2.55 | P = .42 | 2.56 | P = .14 | 0.65 | .47 | 3.92 | P = .24 | 2.91 | P = .33 | 0.61 | .14 | 4.68 | P = .43 |
| 24–35 mo | 1.14 | 0.85 | .60 | 1.34 | 2.42 | 0.58 | .20 | 4.16 | 4.33 | 0.63 | .31 | 6.90 | ||||||
| Severity | ||||||||||||||||||
| Mild | 1.06 | 0.88 | 1.20 | 1.67 | 0.41 | 4.06 | 1.86 | 0.49 | 3.57 | |||||||||
| Moderate/severe | 2.08 | P = .27 | 0.85 | .68 | 2.45 | P = .31 | 3.81 | P = .20 | 0.69 | .06 | 5.52 | P = .47 | 4.29 | P = .14 | 0.66 | .05 | 6.46 | P = .23 |
| Duration | ||||||||||||||||||
| 1–3 d | 1.60 | 0.85 | 1.89 | 2.49 | 0.60 | 4.12 | 4.92 | 0.72 | 6.82 | |||||||||
| 4–7 d | 2.19 | P = .63 | 0.90 | .59 | 2.43 | P = .70 | 4.29 | P < .001 | 0.86 | .13 | 4.98 | P < .001 | 3.44 | P < .001 | 0.78 | .43 | 4.41 | P < .001 |
| 8–14 d | 0.83 | 0.92 | .56 | 0.90 | 19.04 | 1.00 | 19.04 | 3.94 | 0.66 | .73 | 5.97 | |||||||
| ≥15 days | 3.06 | 1.00 | 3.06 | 8.48 | 1.00 | 8.48 | 17.87 | 0.78 | .62 | 21.69 | ||||||||
In Bangladesh, medical costs were higher for girls than for boys, but there are no apparent differences for total costs. All 3 countries show a trend to higher costs with higher levels of education, especially for household direct medical costs.
In India and Pakistan there is a trend toward lower direct medical costs for older children (45%–65% less), and to a lesser extent for total household costs. There is a trend for greater cost for moderate-to-severe diarrhea (45%–50% greater) in Bangladesh and India, compared to mild, but this was less marked for Pakistan. There is also a trend toward higher costs with greater duration, but the pattern is inconsistent.
Costs as a Barrier
Table 5 shows the results for questions relating to why parents did not seek care of diarrhea or why they did not seek hospital attention when it was recommended. In all 3 countries, the primary reason for not seeking care was a perception that no care was needed, with 31%, 73%, and 95% of parents reporting this in Pakistan, Bangladesh, and India respectively. Among the remainder who thought that care was needed, the main causes related directly (eg, transportation, treatment) or indirectly (eg, no time off work, lack of transportation, and distance) to costs. Among those who were recommended to take their child to the hospital and did not, no perceived need was the primary reason in Bangladesh (43%) and costs were the primary reason in Pakistan (53%).
Table 5.
Reasons for Not Seeking Treatment and Sources of Household Costs for Diarrhea Episodes in Bangladesh, India, and Pakistan
| Question | Pakistan (n = 68) | Bangladesh (n = 11) | India (n = 20) |
|---|---|---|---|
| Why did households not seek care for their child? | |||
| No need for care | 30.9% | 72.7% | 95.0% |
| Distance too far | 4.4% | 9.1% | 0.0% |
| Lack of transportation | 1.5% | 0.0% | 0.0% |
| No time off work | 11.8% | 18.2% | 5.0% |
| Local situation (political) | 2.9% | 0.0% | 0.0% |
| Transportation costs | 5.9% | 0.0% | 0.0% |
| Treatment costs | 27.9% | 18.2% | 5.0% |
| Leaving other children at home | 5.9% | 0.0% | 5.0% |
| Unhappy with clinical services | 11.8% | 0.0% | 0.0% |
| Prefer traditional medicine | 5.8% | 0.0% | 0.0% |
| Cultural differences | 0.0% | 0.0% | 0.0% |
| Other | 19.1% | 0.0% | 0.0% |
| Why did the household not seek hospital care when advised? | Pakistan (n = 19) | Bangladesh (n = 14) | |
| Hospital too far | 0.0% | 14.3% | |
| No transportation | 0.0% | 0.0% | |
| Travel costs too high | 5.3% | 7.1% | |
| No time off work | 0.0% | 7.1% | |
| Local situation | 0.0% | 0.0% | |
| Treatment costs | 47.4% | 21.4% | |
| Needs of other children at home | 21.1% | 0.0% | |
| Child not sick enough | 0.0% | 42.9% | |
| Unhappy with clinical services | 15.8% | 0.0% | |
| Other | 10.5% | 7.1% | |
| Where did the money come from? | Pakistan (n = 281) | Bangladesh (n = 81) | India (n = 62) |
| Fewer meals | 12.5% | 1.2% | 19.4% |
| Cutting other expenses | 13.9% | 1.2% | 21.0% |
| Savings | 47.7% | 80.3% | 48.4% |
| Borrowing | 29.2% | 9.9% | 21.0% |
| Selling assets | 3.2% | 4.9% | 3.2% |
| Donations | 1.4% | 0.0% | 0.0% |
| Relative or friend | 3.9% | 2.5% | 1.6% |
| Other | 7.8% | 4.9% | 1.6% |
The main source of funding for household costs for diarrhea episodes was savings in all 3 countries, with 48% in Pakistan, 48% in India, 80% in Bangladesh reporting this. The other common sources were borrowing and cutting expenses.
DISCUSSION
What Are the Costs of Diarrhea to Households?
Few studies measure the financial cost of a diarrheal illness borne by the family and the healthcare system, yet this information becomes critical when decision makers must set priorities for designing and implementing public health interventions to prevent and treat these illnesses. The HUAS provided an opportunity to assess the direct costs and productivity losses associated with a diarrheal illness during the first 5 years of life in a random sample of children living in resource-poor settings in South Asia. These analyses, undertaken in preparation for the GEMS case/control study that will provide prospective, pathogen-specific data on the costs of moderate-to-severe medically attended diarrheal illnesses in the same population, demonstrate in 3 Asian sites that financial costs represent an important component of the diarrheal disease burden.
The 3 countries provide different patterns of household costs from diarrhea. Both direct medical and total costs are lower in Bangladesh than in India and Pakistan (approximately 50%). Interestingly, the proportion of episodes that incur some costs is higher in Bangladesh, suggesting that households are more likely to seek care, and when they do the amount they spend is less. Among episodes that incur some costs, the total cost is less in Bangladesh compared with India or Pakistan.
This difference is almost completely accounted for by the difference in direct medical costs, with little difference in other direct costs or indirect costs. This is also reflected in where care is sought. In Bangladesh approximately half of the household direct medical cost is for care in informal settings, while in India and Pakistan 87% and 75% of costs are in the formal sector. This may reflect higher utilization of low-cost oral rehydration from pharmacies and other outlets. While the lower level of costs in Bangladesh may reflect a lower income level for the setting, it is also likely to be influenced by the healthcare system and high awareness of early treatment of diarrhea with oral rehydration therapy.
Average household costs provide only one aspect of the economic burden. Given the high frequency of diarrhea among young children in low-income settings, there is a possibility that a low-probability but high-cost episode might occur, creating a financial strain for the household. Based on the results presented here, for each diarrhea episode a household faces, there is a 1 in 10 chance of a total cost greater than $6.61 in Bangladesh, $8.07 in India, and $10.11 in Pakistan. In countries where many households live on less than $1 per day, this represents a substantial risk.
In all 3 countries there is some evidence of lower costs for children in households with lower economic or educational levels. This is consistent with poorer households being more likely to ration or delay care due to high costs. This brings with it the risk that delayed treatment will result in more severe outcomes. Although we are not able to address this directly in this study, it should be addressed empirically in subsequent analyses.
Costs by sex differed between countries, with high costs for girls in Bangladesh and higher costs for boys in Pakistan, and little difference in India. This was true for direct medical and total costs. This deserves additional exploration given the evidence in the literature that household expenditures for healthcare, food, and education often favor boys over girls. [22–25]. In making decisions about whether and when to invest in treatment, households may be willing to take greater risks with girls. It is important to note that household costs for girls are not lower in Bangladesh, the where overall household economic burden is less and there may be less need to ration care.
Cross-Country Comparisons
The present study in combination with our related study on household costs for diarrhea treatment in African settings provides helps identify similarities and differences among countries and regions [26]. Across the 6 countries, mean total household costs fell within a fairly wide range, from $1.82 in Bangladesh to $6.47 in Pakistan. In general, costs were higher in higher income settings, reflecting available household resources and the cost of services. However, mean out-of-pocket costs also appear to reflect health system characteristics, in particular the level of subsidy for direct medical costs. In most countries, costs tended to be lower among low-income households, potentially reflecting rationing of care; however, others exhibited an inverted U-shape with the highest costs in the middle-income levels. As described above, 3 of the 6 countries demonstrated lower costs for girls; however, this was not present in others. A number of factors may affect whether there are observed differences between boys and girls. Household income and the absolute level of costs borne by households may affect the need to ration care.
Limitations
The current work suffers from several important limitations. First, the study sample size was designed to provide estimates of overall costs within a margin of error. This is particularly true for India and Bangladesh. It was not powered to examine the determinants of costs and as a result some differences in means among subgroups are often not statistically significant. Additional work with larger samples would help address this. Second, with one-time cross-sectional data we are not able to directly examine the long-term health or economic consequences of the costs incurred by household for individual events or repeated episodes. Lastly, the cross-sectional nature of the study makes it difficult to assess whether low costs for specific subgroups are the result of reduced severity, cheaper services, or rationing of care. Additional work must also be conducted to better understand how the complex interaction between direct medical, direct nonmedical, and indirect costs impact households' demand for and decisions to seek informal or formal care.
CONCLUSIONS
While the absolute value of household economic costs are relatively low for each childhood diarrhea episode, their cumulative impact is likely to be great. Given the frequency of diarrheal episodes among children in low-income settings, these small amounts per case would translate into billions of dollars globally, borne by the families themselves. The small average costs also hide the repeated possibility that an episode will require more extensive and expensive care, resulting in indebtedness or selling of productive assets. Our results also suggest that the household economic burden may result in some households choosing to reduce or delay direct medical expense, especially poor households or for girls. This suggests that these costs and other barriers to care may create or accentuate disparities in adverse outcomes including mortality.
Notes
Financial support. This work was supported by the Bill & Melinda Gates Foundation (grant number 38874).
Supplement sponsorship. This article was published as part of the supplement entitled “The Global Enteric Multicenter Study (GEMS),” sponsored by the Bill & Melinda Gates Foundation.
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Black RE, Cousens S, Johnson HL, et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet. 2010;375:1969–87. doi: 10.1016/S0140-6736(10)60549-1. [DOI] [PubMed] [Google Scholar]
- 2.Atherly DE, Lewis KD, Tate J, Parashar UD, Rheingans RD. Projected health and economic impact of rotavirus vaccination in GAVI—eligible countries: 2011–2030. Vaccine. 2012;30(suppl 1):A7–14. doi: 10.1016/j.vaccine.2011.12.096. [DOI] [PubMed] [Google Scholar]
- 3.Chai PF, Lee WS. Out-of-pocket costs associated with rotavirus gastroenteritis requiring hospitalization in Malaysia. Vaccine. 2009;27(suppl 5):F112–5. doi: 10.1016/j.vaccine.2009.08.069. [DOI] [PubMed] [Google Scholar]
- 4.Fischer TK, Anh DD, Antil L, et al. Health care costs of diarrheal disease and estimates of the cost-effectiveness of rotavirus vaccination in Vietnam. J Infect Dis. 2005;192:1720–6. doi: 10.1086/497339. [DOI] [PubMed] [Google Scholar]
- 5.Forsberg BC, Sullesta E, Pieche S, Lambo N. Costs of diarrhoeal diseases and the savings from a control programme in Cebu, Philippines. Bull World Health Organ. 1993;71:579–86. [PMC free article] [PubMed] [Google Scholar]
- 6.Jeuland M, Whittington D. Cost–benefit comparisons of investments in improved water supply and cholera vaccination programs. Vaccine. 2009;27:3109–20. doi: 10.1016/j.vaccine.2009.02.104. [DOI] [PubMed] [Google Scholar]
- 7.Podewils LJ, Antil L, Hummelman E, Bresee J, Parashar UD, Rheingans R. Projected cost-effectiveness of rotavirus vaccination for children in Asia. J Infect Dis. 2005;192(suppl 1):S133–45. doi: 10.1086/431513. [DOI] [PubMed] [Google Scholar]
- 8.Rheingans R, Atherly D, Anderson J. Distributional impact of rotavirus vaccination in 25 GAVI countries: estimating disparities in benefits and cost-effectiveness. Vaccine. 2012;30(suppl 1):A15–23. doi: 10.1016/j.vaccine.2012.01.018. [DOI] [PubMed] [Google Scholar]
- 9.Andersen RM, Davidson PL. Improving access to care in America: individual and contextual indicators. In: Andersen RM, Rice TH, Kominski GE, editors. Changing the US health care systems: key issues in health services policy and management. San Francisco: Jossey-Bass; 2001. pp. 3–30. [Google Scholar]
- 10.Chola L, Robberstad B. Estimating average inpatient and outpatient costs and childhood pneumonia and diarrhoea treatment costs in an urban health centre in Zambia. Cost effectiveness and resource allocation: C/E. 2009;7:16. doi: 10.1186/1478-7547-7-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gelberg L, Andersen RM, Leake BD. The behavioral model for vulnerable populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34:1273–302. [PMC free article] [PubMed] [Google Scholar]
- 12.Banerjee A, Deaton A, Duflo E. Health, health care, and economic development: wealth, health, and health services in rural Rajasthan. Am Econ Rev. 2004;94:236–30. doi: 10.1257/0002828041301902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stanton B, Clemens J. User fees for health care in developing countries: a case study of Bangladesh. Soc Sci Med. 1989;29:1199–205. doi: 10.1016/0277-9536(89)90363-8. [DOI] [PubMed] [Google Scholar]
- 14.Robberstad B, Strand T, Black R, Sommerfelt H. Cost-effectiveness of zinc as adjunct therapy for acute childhood diarrhoea in developing countries. Bull World Health Organ. 2004;82:523–31. [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization. Geneva, Switzerland: WHO; 2005. Guidelines for estimating the economic burden of diarrheal disease with focus on assessing the costs of rotavirus diarrhea. [Google Scholar]
- 16.Mwabu G, Mwanzia J, Liambila W. User charges in government health facilities in Kenya: effect on attendance and revenue. Health Policy Plan. 1995;10:164–70. doi: 10.1093/heapol/10.2.164. [DOI] [PubMed] [Google Scholar]
- 17.Nyman JA. Is ‘moral hazard’ inefficient? The polity implications of a new theory. Health Aff. 2004;23:194–9. doi: 10.1377/hlthaff.23.5.194. [DOI] [PubMed] [Google Scholar]
- 18.Patil AV, Somasundaram KV, Goyal RC. Current health scenario in rural India. Aust J Rural Health. 2002;10:129–35. doi: 10.1046/j.1440-1584.2002.00458.x. [DOI] [PubMed] [Google Scholar]
- 19.Rao NS. Delivery of health services in the public sector. Financing and delivery of health care services in India. New Delhi: Ministry of Health and Family Welfare; 2005. pp. 43–59. In: National Commission on Macroeconomics and Health Background Papers. [Google Scholar]
- 20.Levine MM. Etiology of diarrhoeal and enteric diseases in developing countries: the Global Enteric Multicenter Study (GEMS) project. Bamako, Mali: WHO; 2009. Global Vaccine Research Forum. [Google Scholar]
- 21.O'Donnell O, van Doorslaer E, Wagstaff A, Lindelow M. Measurement of living standards. Analyzing health equity using household survey data: a guide to techniques and their implementation. Washington, DC: World Bank; 2008. pp. 69–82. [Google Scholar]
- 22.Nguyen H, Knowles J. Demand for voluntary health insurance in developing countries: the case of Vietnam's school-age children and adolescent student health insurance program. Soc Sci Med. 2010;71:2074–82. doi: 10.1016/j.socscimed.2010.09.033. [DOI] [PubMed] [Google Scholar]
- 23.Nuruddin R, Hadden WC, Petersen MR, Lim MK. Does child gender determine household decision for health care in rural Thatta, Pakistan? J Public Health (Oxf) 2009;31:389–97. doi: 10.1093/pubmed/fdp038. [DOI] [PubMed] [Google Scholar]
- 24.Pandey A, Sengupta PG, Mondal SK, et al. Gender differences in healthcare-seeking during common illnesses in a rural community of West Bengal, India. J Health Popul Nutr. 2002;20:306–11. [PubMed] [Google Scholar]
- 25.Pokhrel S, Snow R, Dong H, Hidayat B, Flessa S, Sauerborn R. Gender role and child health care utilization in Nepal. Health Policy. 2005;74:100–9. doi: 10.1016/j.healthpol.2004.12.013. [DOI] [PubMed] [Google Scholar]
- 26.Rheingans R, Kukla M, Adegbola R, et al. Exploring household economic impacts of childhood diarrheal illnesses in three African settings. Clin Infect Dis. 2012;55:S317–26. doi: 10.1093/cid/cis763. [DOI] [PMC free article] [PubMed] [Google Scholar]


