Abstract
Background
Adolescents have smoked less in recent years, but 11.7% of 12-to-17-year-olds were still smokers in 2011. The prevalence of smoking has also remained high among 18-to-25-year-olds (36.8%). An intervention program called “Students in the Hospital” was developed in which the health aspects of smoking and its individual and societal consequences were presented in an interactive informational event. In this study, we determine the efficacy of the program.
Methods
From September 2007 to July 2008, we performed an anonymous survey by questionnaire, with a quasi-experimental control-group design, two weeks before (t1) and six months after (t2) the intervention in a group of 760 participating school students in Berlin.
Results
40.8% of the participants were smokers, among whom 79% stated that they smoked water pipe. Significantly fewer students in the intervention group than in the control group began smoking in the six months after the intervention (p<0.001). The chance of remaining a non-smoker was four times as high in the intervention group (OR, 4.14; CI, 1.66–10.36). Girls benefited from the intervention more than boys (OR 2.56, CI 1.06–6.19). 16.1% of smokers in the intervention group and 17.6% in the control group gave up smoking (p>0.05).
Conclusion
A clear primary preventive effect of the program was demonstrated, although it apparently did not induce persons who were already smokers to quit.
Tobacco consumption is the leading cause of avoidable deaths worldwide (1). Smoking is still common in Germany, where it caused almost 107 000 deaths in 2007 (2). Although the proportion of adults who smoke has decreased in recent years, a study from 2009 showed that 26.1% of women and 33.9% of men were smokers (3). Most smokers have their first cigarettes in early adolescence (4) and are influenced by social factors (5). In a survey conducted by the Federal Centre for Health Education (Bundeszentrale für gesundheitliche Aufklärung, BZgA) in 2011, 11.7% of all adolescents (12 to 17 years) and 36.8% of all young adults (18 to 25 years) described themselves as cigarette smokers. Furthermore, the past few years have seen an increase in the use of water pipes (known as hookah, shisha, or hubble-bubble). In the 30 days leading up to the survey, 8.7% of adolescents and 11.2% of young adults had smoked water pipe at least once. Male respondents smoked water pipe more frequently than women (6). According to Maziak (7), water pipes pave the way to cigarette smoking and have similarly toxic effects.
A survey carried out in 2006 quantified nicotine dependency with the aid of the Fagerström test (8). It found that 50.8% of the 15– to 17-year-old smokers and 41.8% of those in the 18– to 24-year age group were dependent on nicotine. Laucht and Schmid (9) demonstrated an association between the number of cigarettes smoked and starting age in 15-year-olds. The younger they had been when they tried their first cigarette, the more likely they were still to smoke, the more cigarettes they smoked currently, and the higher their degree of dependence.
Early prevention of smoking is thus of crucial importance, and medical professionals in particular should consistently argue for abstinence from tobacco (10).
The Berlin Tumor Center (Tumorzentrum Berlin e.V.), in cooperation with the Berlin Senate Department for Education, Science, and Research, has developed a multimodal prevention program, “Students in the Hospital,” to educate adolescents about the health, individual, and societal aspects of smoking.
To establish the efficacy of this program, we set out to answer two questions:
Does the program help nonsmokers to remain abstinent?
Does the program encourage smokers to take steps to give up?
Method
Study design
A survey was carried out in the form of a prospective case–control study with quasi-experimental design. Participants in both study groups (intervention and control) were questioned 2 weeks before the intervention (t1) and 6 months thereafter (t2). For organizational reasons, randomization was not possible. To keep confounding factors to a minimum, the parallel class of an intervention class in a given grade was selected for the control group.
Participants and sample
Students aged 12 to 19 attending a secondary general, intermediate, grammar, or comprehensive school were eligible, as were apprentices aged 17 to 22 attending a part- or full-time vocational school. The teachers had been given a flyer with information about the project and could register their classes for the intervention program. Participation was voluntary and could be ended at any time without giving a reason. The program was approved by the ethics committee of Charité University Medicine, Berlin, Germany. At the end of recruitment the sample comprised 760 students from 32 school classes in Berlin.
Questionnaire
Besides demographic data (age, sex, type of school attended), the standardized questionnaire asked for information about current smoking status and smoking behavior. The questions branched for nonsmokers and smokers. The survey was approved by the Berlin Senate Department for Education, Science, and Research, and the data were anonymous (each participant generated his/her own personal password). The survey was conducted between September 2007 and July 2008.
Intervention
The school students in the intervention group attended an approximately 2-h-long interactive presentation of the health consequences of smoking at a Berlin lung hospital. This presentation was structured as follows:
In a two-way conversation, a physician informed the students about the reasons for smoking, the mechanisms, and the risks of smoking. Emphasis was placed on the health consequences of smoking, such as impairment of physical performance, cardiovascular disease, pulmonary disease, and nicotine addiction. Another important point was the role of advertising in tempting young people to smoke.
A patient suffering from a tobacco-related illness was introduced to the participants and had a conversation with them, moderated by the physician. A central topic of this program point was the consequences of the patient’s usually long-term smoking habit.
Two or three students from each school class had the opportunity to have their lung function measured by means of plethysmography. Alternatively their blood oxygen content could be determined by finger pulse oximetry.
In a concluding group discussion the results of lung function testing or oximetry were discussed and the students’ questions were answered.
A precondition for attendance of this hospital presentation on smoking was intensive preparation of the topic at school beforehand.
Statistical analyses
For comparison of the intervention and control group at the first timepoint (t1), we used Fisher’s exact test for binary data and the chi-square test for variables with more than two categories. Changes of smoking status within the groups were analyzed with the McNemar test and those between the groups with the chi-square test. We used backward stepwise binary logistic regression (adjusted for sex, age, type of school attended, and study group) to identify significant predictors of the smoking status 6 months after the intervention (t2). The significance level was set at α= 0.05. All analyses were performed using SPSS 16.0.
Results
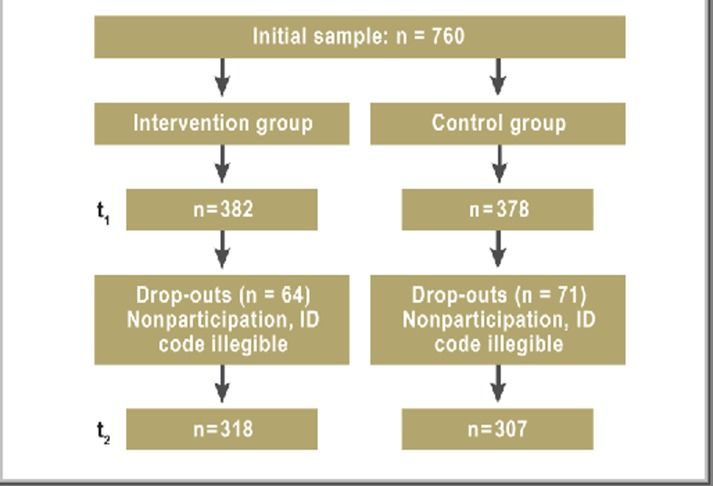
The questionnaire was completed by 760 school students at t1. Of these, 382 (50.3%) were in the intervention group and 378 (49.7%) in the control group. Six months after the intervention (t2), the questions were answered by 625 students (Figure 1), corresponding to a response rate of 82.2%. Analysis of those who dropped out showed no systematic bias with regard to study group or smoking status (p = 0.61).
Figure 1.
Flow diagram of the study participants
Data at baseline (t1)
Four hundred forty-four (58.4%) of the school students were female and 316 (41.6%) were male. Their mean age was 16 years, median 15 years. There were no clear differences with regard to comparability of the variables between the intervention group and the control group (Table 1). The two groups can thus be considered comparable.
Table 1. Characteristics of the school students in the intervention and control group at baseline (t1).
| Variable | Intervention group (n=382) | Control group (n=378) | p value | ||
| Age, mean (± SD) | 15.99 (3.17) | 15.91 (3.50) | 0.74 | ||
| Sex, % (n) | |||||
| Female | 57.3 (219) | 59.5 (225) | 0.56 | ||
| Male | 42.7 (163) | 40.5 (153) | |||
| School attended, % (n) | |||||
| Secondary general and intermediate school | 34.6 (140) | 37.6 (142) | 0.99 | ||
| Grammar school | 25.7 (95) | 24.9 (94) | |||
| Comprehensive school | 7.5 (28) | 7.1 (27) | |||
| Part-/full-time vocational school | 32.2 (119) | 30.4 (115) | |||
| Smoking status, % (n) | |||||
| Nonsmokers | 56.5 (216) | 61.9 (234) | 0.14 | ||
| Smokers | 43.5 (166) | 38.1 (144) | |||
| Smoking behavior of nonsmokers, % (n) | |||||
| Never smoked | 78.7 (170) | 82.8 (194) | 0.52 | ||
| Stopped less than 6 months beforehand | 7.9 (17) | 6.0 (14) | |||
| Stopped more than 6 months beforehand | 13.4 (29) | 11.2 (26) | |||
| Smoking behavior of smokers, % (n) | |||||
| Cigarettes | 51.0 (98) | 49.0 (94) | 0.29 | ||
| Daily | 65.3 (64) | 63.8 (60) | |||
| More than once per week | 9.2 (9) | 8.5 (8) | |||
| Once per week | 6.1 (6) | 7.5 (7) | 0.98 | ||
| Monthly | 19.4 (19) | 20.2 (19) | |||
| Water pipe | 56.3 (138) | 43.7 (107) | 0.07 | ||
| Daily | 0.0 (0) | 3.7 (4) | |||
| More than once per week | 7.3 (10) | 9.3 (10) | |||
| Once per week | 6.5 (9) | 9.3 (10) | 0.15 | ||
| Monthly | 61.6 (85) | 56.1 (60) | |||
| Yearly | 24.6 (34) | 21.5 (23) | |||
SD = standard deviation
Of the 760 students, 59.2% (n = 450) were nonsmokers. Of these, 80.9% (n = 364) had never smoked, 6.9% (n = 31) had stopped smoking less than 6 months previously, and 12.2% (n = 55) had given up more than 6 months beforehand. The proportion of smokers was 40.8% (n = 310). Of the students who smoked, 61.9% (n = 192) smoked cigarettes, 79% (n = 245) used a water pipe, and 41.0% (n = 127) did both.
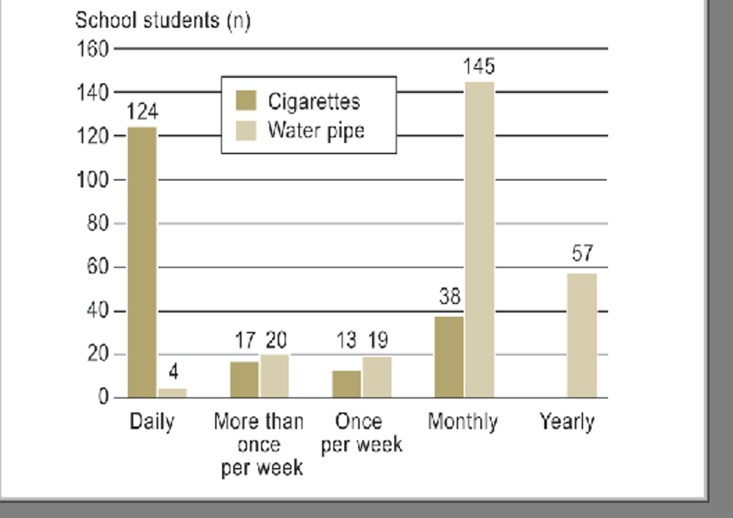
The smoking behavior of the cigarette and water pipe smokers is shown in Figure 2. The majority of cigarette smokers (n = 124) smoked daily, most frequently 6 to 10 cigarettes per day (data not shown). Most of the water pipe smokers (n = 145) smoked each month, most frequently once per month (data not shown). Male study participants smoked water pipe more often than their female counterparts (mean 2 versus 1.5 pipes per month).
Figure 2.
Smoking behavior of the cigarette smokers (n = 192) and water pipe smokers (n = 245)
NB: Annual cigarette consumption was not recorded
Follow-up at 6 months (t2)
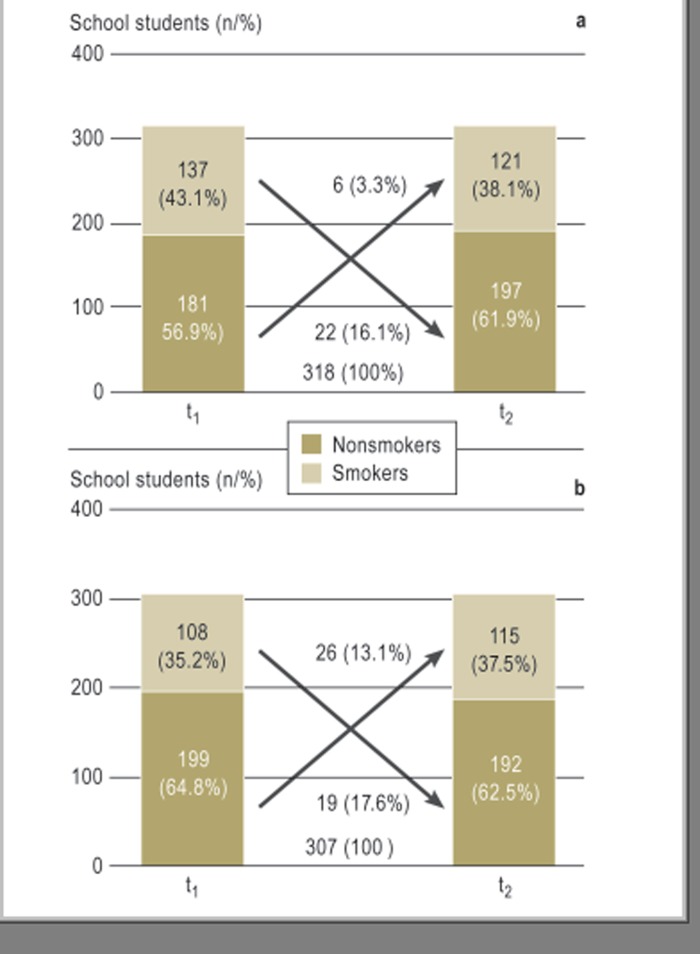
The following changes in the smoking status of the study participants were observed 6 months after the intervention (Figure 3). Altogether, 32 students had taken up smoking during the 6-month observation period: 6 (3.3%) in the intervention group, 26 (13.1%) in the control group (p < 0.001). The proportion of nonsmokers had increased by 5% in the intervention group but decreased by 2.3% in the control group. The “novice smokers” in both study groups behaved typically in that they smoked a very low number of cigarettes and/or water pipes.
Figure 3.
Change in smoking status in both study groups between baseline and the end of the observation period (a = intervention group, b = control group)
Altogether 41 students had given up smoking: 22 (16.1%) in the intervention group and 19 (17.6%) in the control group (p > 0.05).
Predictors of behavior change in nonsmokers and smokers
To enable prediction of abstinence on the part of nonsmokers and smokers (dependent variable), binary logistic regression analysis was carried out. This analysis was intended to establish whether a change in smoking status over the course of the observation period was dependent on study group, sex, age, or type of school. To this end, nonsmokers and smokers were analyzed separately at t1.
Nonsmokers—We determined how many nonsmokers at time t1 were still nonsmokers at t2 and how many had started smoking in the intervening period. Of the 380 nonsmokers at t1(not including the 70 drop-outs), 32 had started smoking by t2, while 348 were still abstinent.
The backward selection of the variables for the first and last step of regression is shown in Table 2. The variables “age” and “type of school” were eliminated by the procedure because they had no clear-cut influence on the predicted variable (p > 0.05).
Table 2. Summary of logistic regression analysis (major effects) for prediction of smoking abstinency by nonsmokers (n=380).
| Variable | OR | SE | 95 % CI | Nagelkerke’s R2 | |
| First step of regression | 0.15 | ||||
| Study group (ref.: control group) | 4.03 | 0.48 | 1.58–10.24 | ||
| Age | 1.18 | 0.12 | 0.92–1.50 | ||
| Sex (ref.: male) | 2.25 | 0.42 | 0.99–5.10 | ||
| Type of school (ref.: part-/full-time vocational school) | |||||
| Secondary general and intermediate school | 4.08 | 0.81 | 0.83–20.05 | ||
| Grammar school | 1.80 | 1.00 | 0.26–12.69 | ||
| Comprehensive school | 1.24 | 1.29 | 0.10–15.50 | ||
| Last step of regression | 0.10 | ||||
| Study group (ref.: control group) | 4.14 | 0.47 | 1.66–10.36 | ||
| Sex (ref.: male) | 2.26 | 0.39 | 1.05–4.88 | ||
OR=odds ratio; SE=standard error; CI=confidence interval; ref.=reference group
Compared with their counterparts in the control group, the nonsmokers in the intervention group had a fourfold likelihood of staying abstinent (odds ratio [OR] 4.14, standard error [SE] 0.47, 95% confidence interval [95% CI] 1.66–10.36). Female school students were twice as likely as male students (reference group) to stay abstinent (OR 2.26, SE 0.39, 95% CI 1.05–4.88).
We also investigated whether the intervention program affected female and male students differently. Table 3 shows the interaction effect between sex and membership of the intervention or control group. In the intervention group, females were approximately twice as likely as males to remain abstinent (OR 2.56, SE 0.45, 95% CI 1.06–6.19).
Table 3. Summary of logistic regression analysis (major and interaction effects) for prediction of smoking abstinency by nonsmokers (n=380).
| Variable | OR | SE | 95 % CI | Nagelkerke’s R2 |
| First step of regression | 0.10 | |||
| Study group (ref.: control group) | 3.01 | 0.69 | 0.78−11.70 | |
| Sex (ref.: male) | 1.47 | 0.83 | 0.29−7.47 | |
| Interaction | ||||
| Study group × sex | 1.75 | 0.95 | 0.27−11.13 | |
| Last step of regression | 0.10 | |||
| Study group (ref.: control group) | 2.54 | 0.56 | 0.85−7.53 | |
| Interaction | ||||
| Study group × sex | 2.56 | 0.45 | 1.06−6.19 |
OR=odds ratio; SE=standard error; CI=confidence interval; ref.=reference group
Smokers—We determined how many smokers at time t1 were still smokers at t2 and how many had stopped smoking in the intervening period. Of the 245 smokers at t1 (not including the 65 dropouts), 41 had given up smoking by t2 and 204 still smoked. The intervention showed no clear-cut effect compared with the control group (OR 0.85, SE 0.36, 95% CI 0.42–1.73).
Discussion
The smoking prevention program was demonstrated to have a primary preventive effect. Far fewer school students started smoking in the intervention group than in the control group: they were 4 times as likely to remain abstinent. Those who already smoked, however, were not persuaded to stop.
The overall proportion of smokers was 40.8%, higher than in other published studies. There were two reasons for this: first, we included both cigarette and water pipe smokers, whereas most surveys are restricted to cigarette smoking; second, the study was carried out in Berlin, where the proportion of smokers is 7.2% higher than in Germany overall (11). The high number of water pipe smokers indicates a change in the pattern of tobacco consumption. This is supported by the findings of Warren et al. (12), who investigated the smoking habits of half a million adolescents between 13 and 15 years of age in 95 countries. In the countries where the frequency of cigarette smoking had remained stable or decreased, other forms of tobacco consumption, particularly water pipe smoking, had increased.
To dissuade young people from taking up smoking, with all its negative effects on health, numerous school-based prevention programs have been developed and their efficacy tested in controlled studies. In Germany, the programs “Klasse 2000” and “Be smart—don’t start” have been offered for a number of years. The concept of the “Klasse 2000” program, aimed at children of grade-school age, is based on the promotion of life skills, including learning how to handle peer pressure with regard to smoking and recognize the danger of addiction. With an observation period of a year, the program showed a positive effect in children at the end of the 4th grade. The risk of starting to smoke was 3.7% lower in the intervention group than in the control group (13). “Be smart—don’t start” is aimed at children in grades 6 to 8 and comprises a competition with rewards for classes in which the students do not smoke for 6 months. Efficacy analysis showed smoking rates of 27.57% in the intervention group and 35.91% in the control group at the end of the observation period (OR 0.65, 95% CI 0.57–0.74, p < 0.001) (14).
A review by Thomas and Perera (15) embraced 94 randomized controlled trials in which the smoking behavior of children and adolescents ranging in age from 5 to 18 was studied over a period of at least 6 months.
The programs that were analyzed included not only information on smoking and approaches involving social influences and skills but also multimodal concepts. The latter combined elements of the existing school curriculum with initiatives at school and also outside, involving parents or communities in order to achieve changes in schools’ policies with regard to smoking. The most comprehensive of the studies covered by this review, the 15-year Hutchinson Smoking Prevention Project (16), focusing mainly on social influences, demonstrated no long-term effect on smoking prevalence. Summing up, Thomas and Perera (15) opine that a combination of multimodal concepts and communal initiatives could boost the efficacy of school-based interventions and state that further research is required.
The intervention program described in this article combines components embedded in the school curriculum with medical elements presented in a clinical context. A preventive effect was demonstrated for nonsmoking students. The findings of other studies are similar. Two years after a program of four 90-minute antismoking lessons given by physicians in German schools, significantly fewer students in the intervention group than in the control group had started smoking (17). In the USA, a prevention program was offered to 13– to 17-year-old patients in pediatric primary care clinics. At the end of a 6-month observation period, nonsmoking members of the intervention group were twice as likely (OR 2.15) still not to have taken up smoking than their counterparts in the control group (18).
The behavior of students who smoked, however, was not changed by our program. This result is not surprising. Almost two thirds of the cigarette smokers were smoking daily at baseline, most of them six to ten cigarettes each day; approximately 25% were smoking one to five cigarettes per day. Smoking two cigarettes on one day each week can, however, be enough to cause nicotine dependence (19). Thus all of the cigarette smokers in our survey were in danger of addiction. If adolescents who smoke are to be persuaded to give up, they must be offered programs tailored to their age group. Sussman and Sun (20) reviewed the results of 64 controlled studies on the efficacy of tobacco withdrawal programs for adolescents and concluded that to be effective, a program must comprise a minimum of five sessions and must be embedded in a school-based concept. This makes it clear that the intervention program presented here is purely preventive in nature with no potential to assist withdrawal.
Limitations
For organizational reasons, no randomization was possible. A result approximating random distribution was achieved, however, by matching parallel classes from the same grade in the same school as intervention and control group. This was reflected by the fact that the characteristics of the members of the intervention group and the control group were not significantly different at baseline (t1). Nevertheless, cluster effects cannot be excluded. The population of smokers is inhomogeneous because of the different patterns of consumption displayed by cigarette smokers and water pipe smokers. The low frequency of water pipe smoking (82% reported smoking only monthly or yearly) should be taken into account when interpreting the findings that relate to smokers. The observation period was only 6 months. It remains to be determined whether there might be a longer-term preventive effect.
Conclusion
The intervention program “Students in the Hospital” proved to have a primary preventive effect. It should ideally be offered before the students have started to smoke. Apart from cigarettes, water pipe smoking entails a considerable health risk of which many adolescents are unaware. This should be borne in mind when planning smoking prevention measures.
Key Messages.
The prevalence of water pipe smoking was very high in our sample of school students (32.2%).
Only 3.3% of students who had taken part in the intervention program started to smoke during the observation period. The corresponding figure in the control group was 13.1% (p<0.001).
In the intervention group, female students were twice as likely to remain abstinent as males.
Students who had already taken up smoking did not profit from the program.
Preventive measures aimed at adolescents should be administered before they have started smoking.
Acknowledgments
Translated from the original German by David Roseveare.
The authors would like to thank Prof. W. Pankow und Drs. C. Grah, B. Schmidt, T. Carstensen, C. Gogoll, M. Schönrock, and H. Badakhshi for implementing the intervention program in their institutions.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
References
- 1.World Health Organization. WHO report on the global tobacco epidemic. http://whqlibdoc.who.int/publications/2011/9789240687813_eng.pdf. 2011 (last accessed on 17.08.2012) [Google Scholar]
- 2.Mons U. Tabakattributable Mortalität in Deutschland und in den deutschen Bundesländern - Berechnungen mit Daten des Mikrozensus und der Todesursachenstatistik. Gesundheitswesen. 2011;73:238–246. doi: 10.1055/s-0030-1252039. [DOI] [PubMed] [Google Scholar]
- 3.Lampert T Robert Koch-Institut Berlin (eds.) Rauchen - Aktuelle Entwicklungen bei Erwachsenen GBE kompakt 2(4) www.rki.de/DE/Content/Gesundheitsmonitoring/Gesundheitsberichterstattung/GBEDownloadsK/2011_4_Rauchen.pdf?__blob=publicationFile. 2011 (last accessed on 23.08.12) [Google Scholar]
- 4.Haustein K-O, Groneberg D. Berlin, Heidelberg: Springer; 2009. Tobacco or Health? Physiological and Social Damages Caused by Tobacco Smoking. [Google Scholar]
- 5.Lampert T. Smoking, physical inactivity, and obesity: associations with social status. Dtsch Arztebl Int. 2010;107(1-2):1–7. doi: 10.3238/arztebl.2010.0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bundeszentrale für gesundheitliche Aufklärung (BZgA) Teilband Rauchen. [Bericht]. Köln: BZgA; 2012. Die Drogenaffinität Jugendlicher in der Bundesrepublik Deutschland 2011. [Google Scholar]
- 7.Maziak W. The global epidemic of waterpipe smoking. Addict Behav. 2011;36:1–5. doi: 10.1016/j.addbeh.2010.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kraus L, Rösner S, Baumeister SE, Pabst A, Steiner S. www.berlin-suchtpraevention.de/upload/material/Suchtsurvey_2006_Berlin.pdf. München: IFT-Bericht Band 167; 2008. Epidemiologischer Suchtsurvey 2006 Repräsentativerhebung zum Gebrauch und Missbrauch psychoaktiver Substanzen bei Jugendlichen und Erwachsenen in Berlin. [last accessed: 23.08.2012] [Google Scholar]
- 9.Laucht M, Schmid B. Früher Einstieg in den Alkohol- und Tabakkonsum - Indikator für eine erhöhte Suchtgefährdung? Z Kinder Jugendpsychiatr Psychother. 2007;35:137–143. doi: 10.1024/1422-4917.35.2.137. [DOI] [PubMed] [Google Scholar]
- 10.Batra A. Treatment of tobacco dependence. Dtsch Arztebl Int. 2011;108(33):555–564. doi: 10.3238/arztebl.2011.0555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Deppermann KM. Epidemiologie des Lungenkarzinoms. Internist (Berl.) 2011;52:125–129. doi: 10.1007/s00108-010-2695-1. [DOI] [PubMed] [Google Scholar]
- 12.Warren CW, Lea V, Lee J, Jones NR, Asma S, McKenna M. Change in tobacco use among 13-15 year olds between 1999 und 2008: findings from the Global Youth Tobacco Survey. Glob Health Promot. 2009;16:38–90. doi: 10.1177/1757975909342192. [DOI] [PubMed] [Google Scholar]
- 13.Maruska K, Isensee B, Hanewinkel R. Universelle Prävention des Substanzkonsums: Effekte des Grundschulprogramms Klasse2000. Sucht. 2011;57:301–312. [Google Scholar]
- 14.Hanewinkel R. „Be Smart - don’t start“. Ergebnisse des Nichtraucherwettbewerbs in Deutschland 1997-2007. Gesundheitswesen. 2007;69:38–44. doi: 10.1055/s-2007-970057. [DOI] [PubMed] [Google Scholar]
- 15.Thomas R, Perera R. School-based programmes for preventing smoking. Cochrane Database Syst Rev. 2006 doi: 10.1002/14651858.CD001293.pub2. 3CD001293. [DOI] [PubMed] [Google Scholar]
- 16.Peterson AV, Jr, Kealey KA, Mann SL, Marek PM, Sarason IG. Hutchinson Smoking Prevention Project: long-term randomized trial in school-based tobacco use prevention - results on smoking. J Natl Cancer Inst. 2000;92:1979–1791. doi: 10.1093/jnci/92.24.1979. [DOI] [PubMed] [Google Scholar]
- 17.Scholz M, Kaltenbach M. Förderung des Nichtraucherverhaltens bei 13-jährigen Schülerinnen und Schülern von Realschule und Gymnasium. Gesundheitswesen. 2000;62:78–85. doi: 10.1055/s-2000-10412. [DOI] [PubMed] [Google Scholar]
- 18.Pbert L, Flint AJ, Fletcher KE, Young MH, Druker S, DiFranza JR. Effect of a pediatric practice-based smoking prevention and cessation intervention for adolescents: a randomized, controlled trial. Pediatrics. 2008;121:738–747. doi: 10.1542/peds.2007-1029. [DOI] [PubMed] [Google Scholar]
- 19.DiFranza JR, Savageau JA, Rigotti NA, et al. Development of symptoms of tobacco dependence in youths: 30 month follow up data from the DANDY study. Tob Control. 2002;11:228–235. doi: 10.1136/tc.11.3.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sussman S, Sun P. Youth tobacco use cessation: 2008 update. Tob Induc Dis. 2009;5 doi: 10.1186/1617-9625-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]