Abstract
Background
To report the results of an arthroscopic percutaneous repair technique for partial-thickness tears of the anterosuperior cuff combined with a biceps lesion.
Methods
The inclusion criteria were evidence of the upper subscapularis tendon tear and an articular side partial-thickness tear of the supraspinatus tendon, degeneration of the biceps long head or degenerative superior labrum anterior-posterior, above lesions treated by arthroscopic percutaneous repair, and follow-up duration > 24 months after the operation. American Shoulder and Elbow Surgeons (ASES) score, constant score, the pain level on a visual analogue scale, ranges of motion and strength were assessed.
Results
The mean (± standard deviation) age of the 20 enrolled patients was 56.0 ± 7.7 years. The forward flexion strength increased from 26.3 ± 6.7 Nm preoperatively to 38.9 ± 5.1 Nm at final follow-up. External and internal rotation strength was also significantly increased (14.2 ± 1.7 to 19.1 ± 3.03 Nm, 12.3 ± 3.2 to 18.1 ± 2.8 Nm, respectively). Significant improvement was observed in ASES and constant scores at 3 months, 1 year and the time of final follow-up when compared with preoperative scores (p < 0.001). The mean subjective shoulder value was 86% (range, 78% to 97%).
Conclusions
The implementation of complete rotator cuff repair with concomitant tenodesis of the biceps long head using arthroscopic percutaneous repair achieved full recovery of normal rotator cuff function, maximum therapeutic efficacy, and patient satisfaction.
Keywords: Subscapularis tendon, Partial tear, Arthroscopic repair, Biceps tenodesis
The upper edge of subscapularis tendon tear and partial thickness supraspinatus tear with an associated bicep lesion is now recognized as a common cause of a shoulder pain. Although there has been some debate, it is considered a preceding pathology in full thickness anterosuperior rotator cuff tear.1,2) Since the first description of subscapularis tendon tear by Smith, many researchers have described methods to diagnose and treat isolated subscapularis tendon.3-9) The subscapularis tear can be caused by trauma, degenerative change and anterosuperior impingement. With anatomical proximity, the subscapular tendon tear is frequently found in combination with biceps long head lesion and partial tear of supraspinatus tendon, which has been called "anterosuperior" cuff tear.3,10,11)
Prevalence of anterosuperior cuff tear associated with biceps lesions has gradually increased with an increasing number of arthroscopic procedures and growing concern regarding the importance of anterosuperior cuff lesion, which is accounting for 9.3% to 23.9% of all rotator cuff tear.12)
Although several studies have documented high success rates following the arthroscopic treatment of anterosuperior cuff tear, less favorable and predictable results were found in the treatment of anterosuperior cuff tears compared with isolated subscapularis tendon tear or posterosuperior cuff tear because of delayed diagnosis and usual involvement of biceps lesion. Therefore, early surgical repair of anterosuperior cuff combined with a biceps lesion before it progresses to a complete full thickness tear is of paramount importance. However, determining the most appropriate treatment for a patient with an early phase of anterosuperior combined lesions can be uncertain since the natural history of these lesions has not been described. Although nonsurgical treatment of these lesions may be suitable for elderly patients with limited functional goals below shoulder level, meticulous surgical repair is more reasonable in preventing the tear propagation over time and gaining maximal postoperative function.
Many techniques have been described for partial tear of rotator cuff and biceps long head lesions independently. Although many of these procedures are effective and are currently in use, the percutaneous intra-articular transtendon (PITT) technique13-16) might be most efficient for a combined lesion because of its simplicity. This method, which is performed using simple instruments and a minimal number of portals, can diminish operation time and enables the surgeon to successfully complete repair with little effort. In this report, we describe the results of an arthroscopic percutaneous repair technique for partial-thickness tears of the anterosuperior cuff combined with a biceps lesion.
METHODS
Selection of Patients
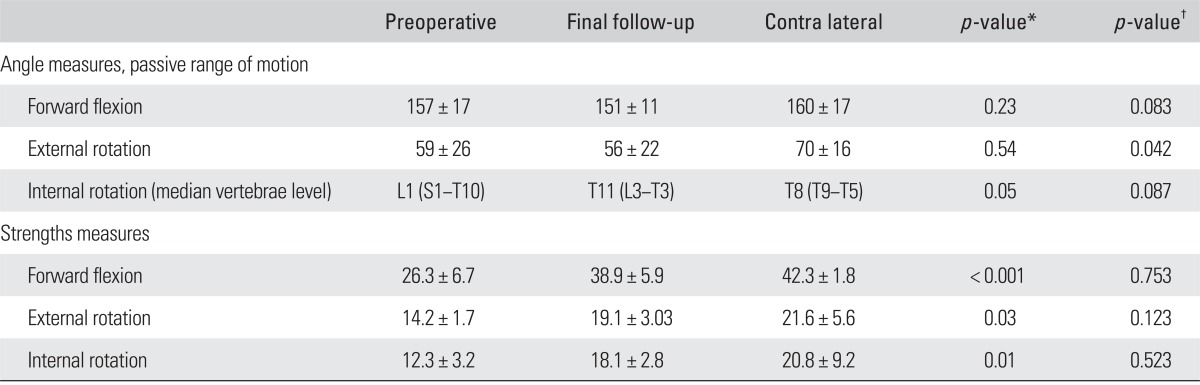
For this retrospective review of data collected prospectively from September 2007 to March 2009, we selected patients who met the following criteria: 1) evidence of upper 1/3 part tear of the subscapularis tendon, 2) evidence of an articular side partial-thickness tear more than 25% of the supraspinatus tendon (Ellman grade AII and AIII), 3) degeneration of the biceps long head or degenerative superior labrum anterior-posterior (SLAP), 4) above lesions treated by arthroscopic percutaneous repair, using a suture anchor and a spinal needle, 5) the duration of follow-up was more than twenty-four months after the operation. We excluded patients who had a stiff shoulder, a more than complete superior 2/3 tear of the subscapularis tendon (Laffose classification III, IV, and V) which might need major procedure in subcoracoid space and/or full thickness tears of supraspinatus tendon, those who had undergone revision surgery, or those with rheumatoid arthritis, or an infection, or previous surgery of the same shoulder. Initially 32 patients met our inclusion criteria on clinical examination and magnetic resonance imaging (MRI) (Fig. 1). At the time of presentation, operative options, depending on the structural alterations of the rotator cuff and biceps long head, were discussed with the patients. However, 12 of 32 patients who had met our inclusion criteria preoperatively were excluded after arthroscopic procedure. Unlike the finding on clinical examination and MRI, 7 patients had a healthy biceps tendon and 4 patients just had a partial tear of supraspinatus tendon less than 25% of entire thickness, which were able to treat with arthroscopic debridement. One patient had a complete superior 2/3 subscapularis tendon tear, which used to require subacromial procedure for proper coverage of subscapular footprint by use of at least two anchors. Thus, 20 patients were finally included in this study. Twelve patients were men, and the mean patient age was 56.0 ± 7.7 years. Twelve patients had symptoms in the dominant shoulder. The average period of symptoms before the operation was 12.8 weeks (range, 6 to 32 weeks). The Institutional Review Board of our center approved the study.
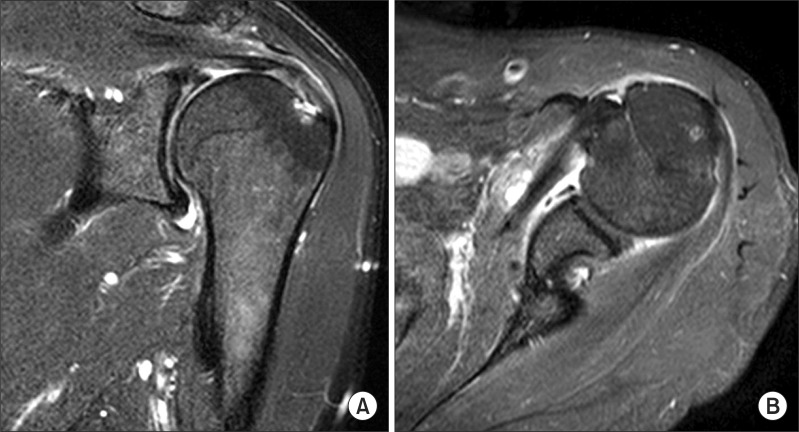
Fig. 1.
Conventional magnetic resonance imaging with T2-weighted images in the oblique coronal and axial planes show partial tear of supraspinatus tendon (A) and subscapularis tendon (B). The disrupted transverse ligament covering the bicipital groove was noted.
Evaluation
At the time of the initial diagnosis as well as at the time of follow-up, the clinical assessment included a structured interview and a detailed, standardized physical examination including the provocation test for impingement and special tests sensitive to subscapularis tendon tear including lift-off and belly-press test. Yergason's and Speed's tests as well as O'Brien test in predicting biceps tendon pathology and SLAP lesions were also performed. All patients were evaluated using the American Shoulder and Elbow Surgeons (ASES) score, constant score and the pain level on a visual analogue scale (VAS). These were assessed preoperatively, after 3 months, 12 months, and at the time of the final follow-up. We used an abbreviated constant score, which excludes the strength measurement. A standard shoulder evaluation, which included the passive ranges of motion and strengths, was performed preoperatively and at the time of the final follow-up using an electrogoniometer and an Isobex digital strength analyzer with a setting of 60°/sec angular velocity. The strength of the contralateral shoulder was measured as a control. In addition, the patients were asked to assign a subjective shoulder value as a percentage of an entirely normal shoulder.
Imaging
A magnetic resonance imaging scan at the time of diagnosis was available for all patients. Partial tear of supraspinatus tendon or continuity of the tendon was assessed on coronal oblique proton-density-weighted MR images. The final diagosis was confirmed when additional findings such as a high signal within subscapularis tendon, fluid halo around the biceps tendon or/and medial subluxation of biceps tendon from bicipital groove were detected on T2-weighted images.
Statistical Methods
SPSS ver. 15.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. The paired Wilcoxon signed-rank test was used to compare the values at the time of diagnosis with those at the time of follow-up. Null hypotheses of no difference were rejected if p-values were less than 0.05.
Surgical Technique
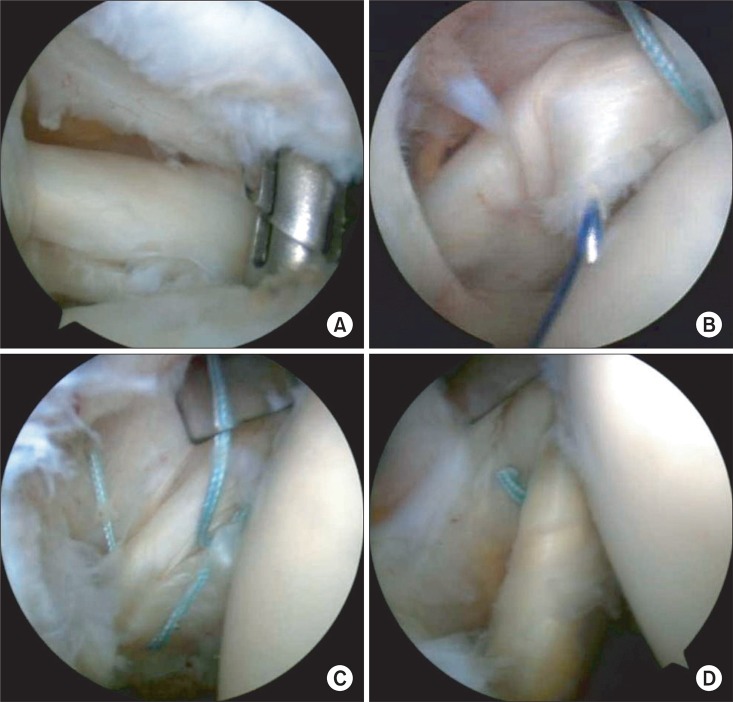
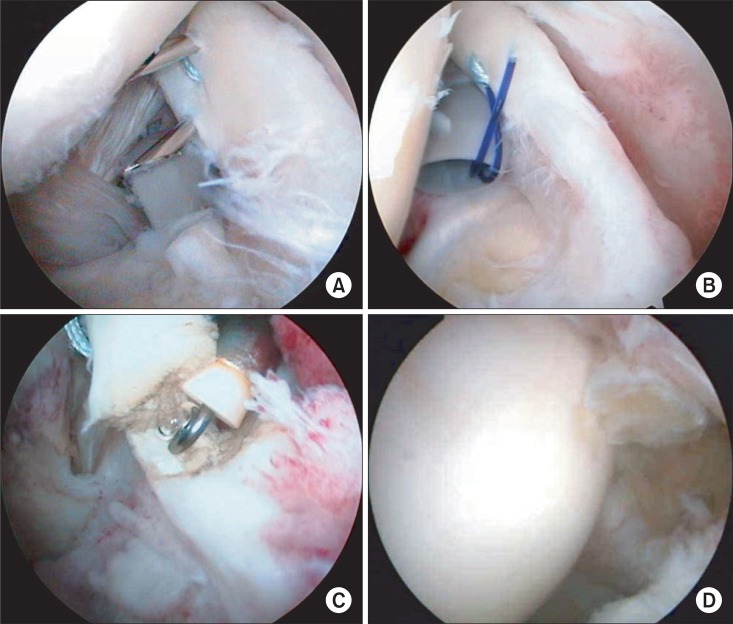
Patients were positioned in the lateral decubitus position with the affected arm upwards and in 45° of abduction and 15° of forward flexion in a traction device. As with any other arthroscopic procedure, a standard posterior portal was created approximately 2 cm inferior and medial from the posterolateral corner of the acromion. An anterior portal was placed just medial to the point formed by the biceps and subscapularis tendon near the most medial portion of the subscapularis tendon footprint, which is approximately 1 cm distal to the acromion. The extent and depth of tear in supraspinatus tendon were measured as accurately as possible with a graduated probe, calibrated in millimeters, in both the anteroposterior and the mediolateral plane. The free edge of the subscapularis tendon was freshened with a shaver and the bone bed on the most medial side of the footprint was prepared through the anterior portal by means of electrocautery and a high speed burr. A 3.7-mm anchor double-loaded with number-2 FiberWire (Arthrex Inc., Naples, FL, USA) is placed at center of the exposed subscapularis tendon footprint through the anterior portal. After the anchor screw was purchased, a spinal needle was inserted from the outside of the shoulder into the interval capsule. Under direct visualization, the spinal needle pierced the superolateral healthy tissue of the subscapularis tendon. A No. 1 polydioxanone (PDS) monofilament absorbable suture (Ethicon, Cornelia, GA, USA) was threaded through the spinal needle to switch it into the loaded suture. These procedures were repeated for the second suture. After each suture had been passed through the torn end of the subscapularis tendon, each pair of suture limbs was sutured through the anterior portal using a surgeon's knot (Fig. 2). After the repair of the subscapularis tendon, biceps tenodesis using the PITT technique was performed in the same manner. Under the direct visualization of biceps tendon, the skin was palpated to identify a proper entry point overlying biceps tendon. A paired 18-gauge spinal needles were passed through the most anterolateral part of rotator interval tissue and finally into biceps tendon. No. 1 PDS monofilament absorbable sutures are threads into the needles. The two sutures are grasped and pulled out of the anterior portal. Each free end of the PDS suture that had been passed out the anterior portal is then tied to the two ends of a No. 2 braided non-absorbable suture (FiberWire). The two monofilament absorbable sutures are then with-drawn for their percutaneous entry, thereby pulling the No. 2 braided non-absorbable suture through the biceps tendon. This creates a mattress suture pattern with the free ends of the suture lying outside the skin (Fig. 3). A second mattress suture is created with same manner but right angle to former mattress suture pattern to finally be cruciate pattern of double mattress suture. The biceps tendon is transected proximally and the biceps origin is debrided from the superior labrum. The sutures were tied using standard arthroscopic knot-tying techniques simultaneously with tie for supraspinatus tendon repair at subacromial space.
Fig. 2.
The procedure for subscapularis tendon repair. (A) 3.7 mm punch for a suture anchor at the footprint of the subscapularis tendon. (B) Polydioxanone monofilament absorbable suture passed through the spinal needle and substance of the subscapularis tendon. (C) FiberWire suture limbs of the anchor passed through the subscapularis tendon. (D) The subscapularis tendon securely fixed to its insertion site and its tension restored.
Fig. 3.
(A, B) Introduction of 18-G spinal needles through the biceps tendon through most of the superolateral rotator interval tissue followed by passing the polydioxanone suture through the 18-G needles to switch to FiberWire suture. (C) The root of the biceps long head cut by an electrocautery device through the anterior portal. (D) Intra-articular view after biceps tenodesis using the percutaneous intra-articular transtendon technique.
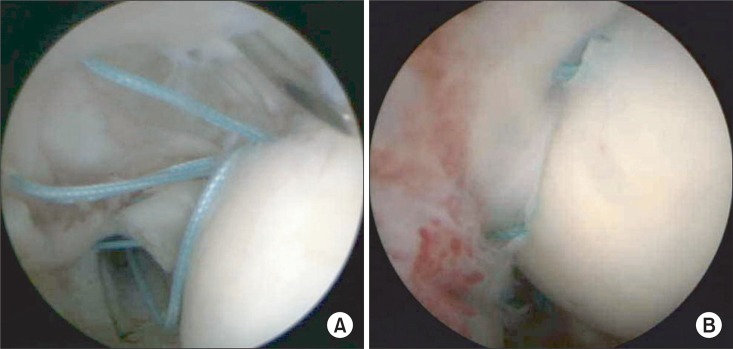
For partial thickness tear of the supraspinatus tendon, a 3.7 mm double-loaded Bio-Suture Tak anchor (Arthrex Inc.) was introduced through the anterosuperior portal or trans-tendon portal and inserted at the center of the exposed footprint, just lateral to the articular cartilage, maintaining an appropriate dead man's angle. For a large tear greater than 1 cm in anterior posterior direction, 2 such anchors were used. We used two medial suture anchors in 15 patients and one anchor in the other 5 patients.
Next, two 18-gauge spinal needles were inserted percutaneously 2 mm from the torn edge and 5 mm apart, centered over each corresponding suture anchor. No. 0 PDS passed through each of the spinal needles was retrieved though the anterosuperior portal with grasper forceps and used for relaying the anchor sutures which were then pulled out percutaneously. These sutures including sutures for biceps tenodesis were tied down on the bursal side using a non-sliding knot after subacromial buesectomy (Fig. 4). From the day after the operation, passive range of motion (ROM) and partial active ROM exercises were allowed while wearing a shoulder sling under the supervision of a physical therapist. From 2 weeks after the operation, gentle active ROM exercises, limited to the waist level, were allowed without the shoulder sling.
Fig. 4.
(A) The polydioxanone suture passing through each of the 18-G spinal needles to exchange it into a loaded suture on the anchor following the insertion of 3.7 mm suture tak anchor at the far medial edge of the footprint at a dead man's angle of 45° or less. (B) Intra-articular view after complete repair of the partial articular side tear of suparaspinatus tendon lesion.
RESULTS
The tenderness over the biceps groove, painful motion, and positive impingement sign seen preoperatively in all patients disappeared at the time of follow-up, over a mean duration of 32 months (range, 24 to 56 months). Eight patients with positive lift-off test preoperatively turned negative at final follow-up. Thirteen patients out 19 patients who had a positive belly press test preoperatively went negative. Five patients had a Popeye deformity, indicative of fixation loss of biceps tenodesis, but no patient complained of this after follow-up.
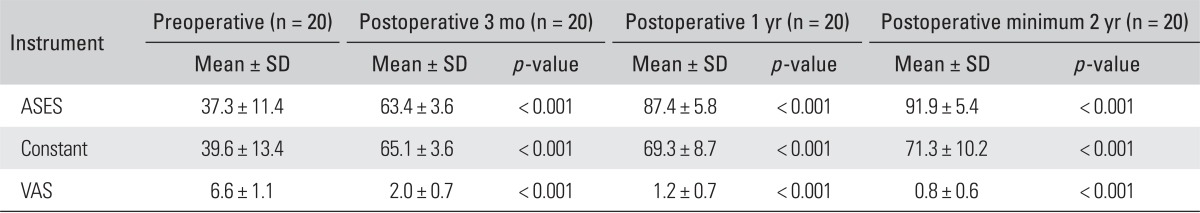
Yergason's test was positive in 12 patients, and Speed's test was positive in 13 patients preoperatively. All patients who had a positive Yergason's test and Speed's test preoperatively could completely perform the test without pain (negative test results) at the time of follow-up. The positive in O'Brien test in 14 patients turned into a negative at the time of follow-up. The preoperative subjective and objective functional scores improved with serial time of follow-up. Overall functional results according to the ASES score, constant score and VAS scores were summarized in Table 1.
Table 1.
Overall Subjective Scores Comparing Preoperative Status versus Status at 3 Months, 1 Year, and 2 Years Postoperatively
ASES: American Shoulder and Elbow Surgeons, VAS: visual analogue scale.
The strengths of all patients had increased compared to preoperative levels at the time of the last follow-up. The forward flexion strength increased from a mean of 26.3 ± 6.7 Nm preoperatively to 38.9 ± 5.1 Nm at the final follow-up (p < 0.001). External rotation and internal rotation strengths also increased significantly from a mean of 14.2 ± 1.7 to 19.1 ± 3.03 and 12.3 ± 3.2 to 18.1 ± 2.8 Nm, respectively, at the final follow-up (p = 0.03 and p = 0.01, respectively). No significant differences were noted between the affected and unaffected shoulders at the final follow-up with regard to forward flexion strength (p = 0.753), external rotation strength (p = 0.123), or internal rotation strength (p = 0.523). The passive range of motion in forward flexion and internal rotation improved to the level which was nearly equivalent to those of the contralateral shoulder at the final follow-up (p = 0.083 for forward flexion and p = 0.087 for internal rotation). However, the passive range of motion in external rotation did not improve completely at the final follow-up. Statistical difference was found between the affected and unaffected shoulders in external rotation (p = 0.042). The mean subjective shoulder value was 86% (range, 78% to 97%). The outcome measures regarding strength and passive range of motion are summarized in Table 2. Follow-up MRI was available to 12 patients at time of final follow-up.
Table 2.
Overall Muscle Strength and Passive Range of Motion Comparing Preoperative Status versus Status at the Time of Final Follow-up and Contralateral Shoulder as Control
Values are presented as mean ± standard deviation.
*p-value (preoperative vs. final follow-up). †p-value (follow-up vs. contralateral).
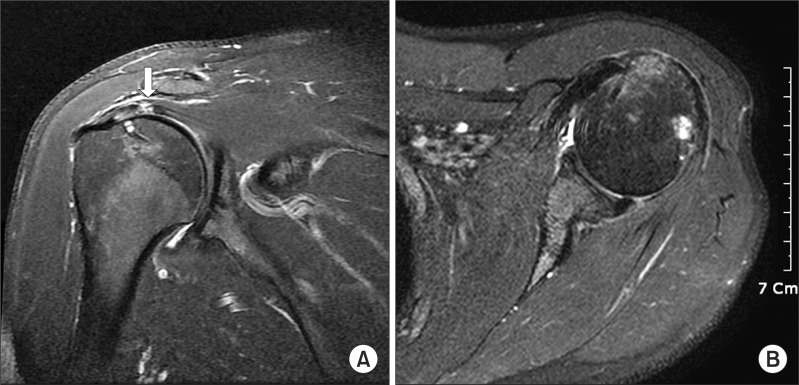
Of the 12 patients, 11 (82%) had no evidence of a propagation to full-thickness or near full-thickness defect on follow-up MRI. However, 4 of 11 patients had an evident retear of inner portion of supraspinatus tendon which was initially fixed (Fig. 5). One patient had a suspicion of subscapularis tendon retear which demonstrated high density within upper part of tendon. Nevertheless, the functional results were good to excellent regardless of an evident radiologic retear at final follow-up.
Fig. 5.
(A) Follow-up magnetic resonance imaging taken at 2 years indicates incomplete healing defect (arrow) of supraspatus tendon. (B) Subscapularis tendon that was simultaneously repaired shows complete integrity. The 4 of 11 patients had an evident partial thickness defect under supraspinatus tendon that was initially fixed, but no correlation with clinical outcome.
DISCUSSION
The most important finding of the present study is that the arthroscopic percutaneous repair for partial thickness tear of anterosuperior cuff in combination with biceps long head lesion yielded favorable functional results regardless of radiologic retear in some patients at the time of the final follow-up. In addition, ASES and VAS scores significantly improved after only 3 months, and by 12 months, all patients reported favorable functional recovery and high subjective satisfaction, indicating a quick return to original activities. However, 5 patients failed to correct a positive belly press test at the time of final follow-up. That observation might be associated with a subscapularis tendon retear although they all were not confirmed by follow-up MRI. Partial-thickness tears involving the subscapularis, supraspinatus, and biceps tendon are more frequently recognized because many clinicians pay particular attention to diagnosis with high index of suspicion in both MRI and arthroscopy since its increased recognition.8,17)
Since Habermeyer et al.11) first stressed the possibility of tear propagation of partial-thickness tears in the upper edge of the subscapularis tendon to the biceps and adjacent supraspinatus tendon, partial-thickness tears of the supraspinatus tendon and concomitant biceps lesions such as degeneration, fissure, and subluxation combined with subscapularis tendon tears have been considered to be early pathologic signs of an upcoming wide full thickness rotator cuff tear. Patients with subscapularis tendon tears have a variety of symptoms depending on the tear size, the degree of tear propagation to the adjacent cuff, and involvement of the biceps long head. Some patients may have no symptoms or only mild symptoms despite having several lesions, while others may be completely disabled and in severe pain with only an isolated subscapularis tendon lesion. Thus, because of the inconsistent preoperative symptoms and uncertain pathologic cascade after type I or II subscapular tendon tears, surgeons are posed with a dilemma whether they should repair or not the concomitant partial thickness tear of supraspinatus or biceps lesion. Recently, active repair as a standard treatment for partial-thickness tears of an isolated supraspinatus tendon has yielded more favorable results than simple debridement.7,18) In addition, biceps tenodesis has been found to be one of the most effective modalities for lesions of the biceps long head, thought to be a major source of pain of the shoulder joint. Based on these concepts, we reasoned that an aggressive treatment approach consisting of simultaneous repair of the subscapularis and supraspinatus tendons and biceps tenodesis would yield results superior to the isolated repair of selected structures. Ultimately, the surgeon's interpretation of the pathogenesis of the subscapularis tendon tear and the resultant pathology will inform his/her choice of treatment methodology.
Several studies have documented high success rates following arthroscopic or open treatment of isolated partial-thickness subscapularis tendon tears.4-6,17) In contrast, only a few studies have reported outcomes after combined surgical treatment of anterosuperior cuff partial-thickness tears with biceps pathology.19) In general, meticulous intraoperative estimation of the depth and location of the tear, as well as tendon quality, are important factors when choosing the best operative technique for a successful outcome.8,17)
Our method adheres to the principles of other arthroscopic repair methods of partial-thickness supraspinatus and subscapularis tendon tears such as the technique of passing the loaded suture on an anchor through the tendon percutaneously with a simple instrument i.e., an 18-gauge spinal needle. This method and the use of simple instruments simplify the operating procedure and slants the learning curve. Our method negates the need for additional arthroscopic portals other than the most superolateral working portal within the rotator interval.
Rotator cuff power in terms of forward elevation, abduction, and internal and external rotation strengths at the time of the last follow-up were significantly better than the preoperative power. Furthermore, the affected and unaffected shoulders had similar strengths at the final follow-up. However, the passive range of external rotation motion did not improve to the level of the contralateral shoulder for 10 shoulders at the final follow-up. This might be due to over tightening of the subscapularis tendon during the procedure or a teno-capsulodesis effect caused by adhesion to the adjacent anterosuperior capsule. Although these patients had a restricted external rotation motion, the average of a loss of 20 degree of external rotation does not seem to restrict the daily activities. As seen on magnetic resonance imaging, although it was observed in a small number of patients, the retear of repaired tendon might indicate a subsequent risk of partial thickness tear progressing into full thickness tear. Otherwise, PITT method may have a potential problem with healing, which can be caused by small area of healing bed or tensional unbalance among each layer of the supraspinatus tendon or among each rotator cuff tendon.
With regard to the results in this study, there are several limitations that have to be considered before applying in clinical practice. The case number might not be appropriate to show significant difference when comparing pre and postoperative data. The second limitation of our study is the lack of a control group which would be treated with conservative method. Forthcoming studies in this regard are warranted.
Despite the lack of long-term clinical outcomes and lack of surgical background for impending full thickness tears of the rotator cuff, the implementation of complete rotator cuff repair with concomitant tenodesis of the biceps long head using arthroscopic percutaneous repair allowed full recovery of the functions of a normal rotator cuff, and achieved both maximum therapeutic efficacy and patient satisfaction although there was no complete radiologic healing evidence.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Fox J, Romeo AA. Arthroscopic subscapularis repair; Annual Meeting of the American Academy of Orthopaedic Surgeons; 2003 Feb 5-9; New Orleans, LA, USA. [Google Scholar]
- 2.Lafosse L, Jost B, Reiland Y, Audebert S, Toussaint B, Gobezie R. Structural integrity and clinical outcomes after arthroscopic repair of isolated subscapularis tears. J Bone Joint Surg Am. 2007;89(6):1184–1193. doi: 10.2106/JBJS.F.00007. [DOI] [PubMed] [Google Scholar]
- 3.Arai R, Sugaya H, Mochizuki T, Nimura A, Moriishi J, Akita K. Subscapularis tendon tear: an anatomic and clinical investigation. Arthroscopy. 2008;24(9):997–1004. doi: 10.1016/j.arthro.2008.04.076. [DOI] [PubMed] [Google Scholar]
- 4.Burkhart SS, Tehrany AM. Arthroscopic subscapularis tendon repair: technique and preliminary results. Arthroscopy. 2002;18(5):454–463. doi: 10.1053/jars.2002.30648. [DOI] [PubMed] [Google Scholar]
- 5.Deutsch A, Altchek DW, Veltri DM, Potter HG, Warren RF. Traumatic tears of the subscapularis tendon: clinical diagnosis, magnetic resonance imaging findings, and operative treatment. Am J Sports Med. 1997;25(1):13–22. doi: 10.1177/036354659702500104. [DOI] [PubMed] [Google Scholar]
- 6.Gerber C, Hersche O, Farron A. Isolated rupture of the subscapularis tendon. J Bone Joint Surg Am. 1996;78(7):1015–1023. doi: 10.2106/00004623-199607000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Ide J, Tokiyoshi A, Hirose J, Mizuta H. Arthroscopic repair of traumatic combined rotator cuff tears involving the subscapularis tendon. J Bone Joint Surg Am. 2007;89(11):2378–2388. doi: 10.2106/JBJS.G.00082. [DOI] [PubMed] [Google Scholar]
- 8.Pfirrmann CW, Zanetti M, Weishaupt D, Gerber C, Hodler J. Subscapularis tendon tears: detection and grading at MR arthrography. Radiology. 1999;213(3):709–714. doi: 10.1148/radiology.213.3.r99dc03709. [DOI] [PubMed] [Google Scholar]
- 9.Smith JG. The classic: pathological appearances of seven cases of injury of the shoulder-joint: with remarks 1834. Clin Orthop Relat Res. 2010;468(6):1471–1475. doi: 10.1007/s11999-010-1231-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gerber C, Sebesta A. Impingement of the deep surface of the subscapularis tendon and the reflection pulley on the anterosuperior glenoid rim: a preliminary report. J Shoulder Elbow Surg. 2000;9(6):483–490. doi: 10.1067/mse.2000.109322. [DOI] [PubMed] [Google Scholar]
- 11.Habermeyer P, Magosch P, Pritsch M, Scheibel MT, Lichtenberg S. Anterosuperior impingement of the shoulder as a result of pulley lesions: a prospective arthroscopic study. J Shoulder Elbow Surg. 2004;13(1):5–12. doi: 10.1016/j.jse.2003.09.013. [DOI] [PubMed] [Google Scholar]
- 12.Nho SJ, Frank RM, Reiff SN, Verma NN, Romeo AA. Arthroscopic repair of anterosuperior rotator cuff tears combined with open biceps tenodesis. Arthroscopy. 2010;26(12):1667–1674. doi: 10.1016/j.arthro.2010.04.008. [DOI] [PubMed] [Google Scholar]
- 13.Boileau P, Krishnan SG, Coste JS, Walch G. Arthroscopic biceps tenodesis: a new technique using bioabsorbable interference screw fixation. Arthroscopy. 2002;18(9):1002–1012. doi: 10.1053/jars.2002.36488. [DOI] [PubMed] [Google Scholar]
- 14.Lo IK, Burkhart SS. Transtendon arthroscopic repair of partial-thickness, articular surface tears of the rotator cuff. Arthroscopy. 2004;20(2):214–220. doi: 10.1016/j.arthro.2003.11.042. [DOI] [PubMed] [Google Scholar]
- 15.Lopez-Vidriero E, Costic RS, Fu FH, Rodosky MW. Biomechanical evaluation of 2 arthroscopic biceps tenodeses: double-anchor versus percutaneous intra-articular transtendon (PITT) techniques. Am J Sports Med. 2010;38(1):146–152. doi: 10.1177/0363546509343803. [DOI] [PubMed] [Google Scholar]
- 16.Sekiya JK, Elkousy HA, Rodosky MW. Arthroscopic biceps tenodesis using the percutaneous intra-articular transtendon technique. Arthroscopy. 2003;19(10):1137–1141. doi: 10.1016/j.arthro.2003.10.022. [DOI] [PubMed] [Google Scholar]
- 17.Flury MP, John M, Goldhahn J, Schwyzer HK, Simmen BR. Rupture of the subscapularis tendon (isolated or in combination with supraspinatus tear): when is a repair indicated? J Shoulder Elbow Surg. 2006;15(6):659–664. doi: 10.1016/j.jse.2005.07.013. [DOI] [PubMed] [Google Scholar]
- 18.Waibl B, Buess E. Partial-thickness articular surface supraspinatus tears: a new transtendon suture technique. Arthroscopy. 2005;21(3):376–381. doi: 10.1016/j.arthro.2004.11.008. [DOI] [PubMed] [Google Scholar]
- 19.Bennett WF. Arthroscopic repair of anterosuperior (supraspinatus/subscapularis) rotator cuff tears: a prospective cohort with 2- to 4-year follow-up. Classification of biceps subluxation/instability. Arthroscopy. 2003;19(1):21–33. doi: 10.1053/jars.2003.50023. [DOI] [PubMed] [Google Scholar]