Abstract
Hepatocellular carcinoma (HCC) is sexually dimorphic in both rodents and humans, with significantly higher incidence in males, an effect that is dependent on sex hormones. The molecular mechanisms by which estrogens prevent and androgens promote liver cancer remain unclear. Here, we discover that sexually dimorphic HCC is completely reversed in Foxa1- and Foxa2-deficient mice after diethylnitrosamine-induced hepatocarcinogenesis. Coregulation of target genes by Foxa1/a2 and either the estrogen receptor (ERα) or the androgen receptor (AR) was increased during hepatocarcinogenesis in normal female or male mice, respectively, but was lost in Foxa1/2-deficient mice. Thus, both estrogen-dependent resistance to and androgen-mediated facilitation of HCC depend on Foxa1/2. Strikingly, single nucleotide polymorphisms at FOXA2 binding sites reduce binding of both FOXA2 and ERα to their targets in human liver and correlate with HCC development in women. Thus, Foxa factors and their targets are central for the sexual dimorphism of HCC.
Despite recent breakthroughs in the management of hepatocellular carcinoma (HCC), it is still the fastest-rising cause of cancer-related death in the United States [1]. Unfortunately, most patients are diagnosed at intermediate-advanced stages, when curative therapies are not a primary option. HCC natural history is fairly well known, since most tumors arise from a traceable underlying liver disease (i.e., cirrhosis), allowing for early diagnosis in the setting of surveillance programs. In patients with cirrhosis, there is a striking gender imbalance in HCC incidence, with a solid predominance for males regardless of geographic area, etiologic factor, and ethnicity. Male to female ratio averages between 2:1 and >4:1 across studies [2]. These discrepancies are not merely explained by gender-specific differences in exposure to cirrhosis risk factors (e.g., viral hepatitis or alcohol abuse), since experimental models of chemically-induced HCC also demonstrate a clear male predominance, although molecular mechanisms behind gender bias remain unknown. There is also preliminary evidence suggesting that specific genomic profiles, once HCC has developed, are predominant according to patient’s gender, reflected by an enrichment in certain molecular subclasses [3,4].
In a recent study by Li et al. [5], the authors report a central role for the winged helix transcription factors Foxa1/Foxa2 in controlling estrogen and androgen signaling via the recruitment of estrogen receptor alpha (ERα) and androgen receptor (AR) to hepatocyte target genes. They found that the effects of sex hormones in the liver are Foxa1/Foxa2-dependent and provide a novel molecular mechanism responsible for gender dimorphism in HCC. Sexually dimorphic HCC was completely reversed in Foxa1- and Foxa2-deficient mice after chemically-induced (diethylnitrosamine) HCC. The authors also included human samples in their analysis, and despite the fact that no mutations in any of the FOXA genes have been reported so far in HCC, the authors provide evidence that certain single nucleotide polymorphisms at FOXA2 binding sites reduce its affinity with ERα, and this correlates with increased incidence of HCC development in women. A similar gender bias occurrence was observed in a recent forward genetic screen using the Sleeping Beauty transposon insertional mutagenesis system [6]. Overall, the study by Li et al. [5] reveals a novel interplay between Foxa and hormone receptors binding sites that justifies gender disparities in HCC.
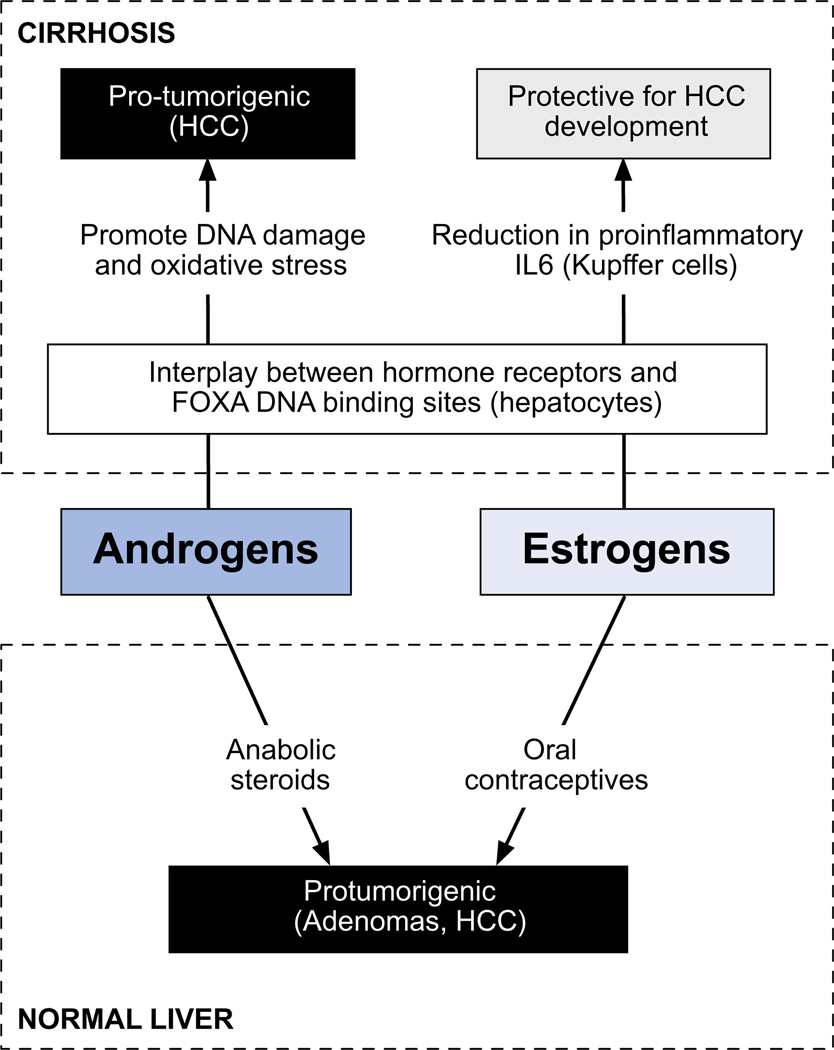
Molecular data indicate that androgens contribute to the HCC development by acting as tumor promoters via induction of DNA damage and oxidative stress [7]. Conversely, estrogens have been suggested to act as general suppressors of HCC through reduction in the proinflammatory effects of MyD88-mediated secretion of IL6 [8]. In addition, estrogens seem to exert different tumorigenic properties depending on the tissue type, since contrary to the epidemiological data in cirrhotic women, chronic exposure to estrogens favors carcinogenesis in breast and uterus. Paradoxically, both androgens (i.e., anabolic steroids) and estrogens (e.g., oral contraceptives) are able to induce benign liver tumors (i.e., adenomas) and ultimately HCC in individuals without underlying liver disease (Fig. 1). Overall, the effects of estrogens in terms of cancer development are largely tissue and environment-dependent, protective in experimental models of cirrhosis but inducing oncogenesis in the normal liver, and promoting tumor growth in full-blown HCC. Strikingly, the study by Li et al. [5] found that tumor load in female Foxa-deficient mice far exceeded that of control males, suggesting that estrogens could have a pro-tumorigenic effect in the absence of Foxa1/Foxa2. Whether Foxa is the link that explains these opposing effects of estrogens requires further investigation. Background inflammation in cirrhosis could play an additional confounding role, emphasized by the crosstalk between IL6-STAT signaling and estrogens in experimental models of HCC [8].
Fig. 1. Summary of the role of sex hormones in HCC.
Different data indicate a pro-tumorigenic role of androgens in both the cirrhotic and normal liver. However, evidence from experimental models of chemically-induced HCC suggests that estrogens may be protective in this setting by interfering with IL6 production and FOXA DNA binding sites.
From a therapeutic standpoint, several studies have tried to evaluate the role of anti-estrogen therapy (e.g., tamoxifen) in patients with overt HCC. Evidence of expression of ER in some tumors and experimental data of estrogen-dependent HCC growth provided the scientific rational for this approach. Most of the studies were small trials, conducted in the 1990s and including a heterogeneous patient population. A meta-analysis including close to 700 patients revealed no impact of tamoxifen in 1-year survival in patients with HCC [9]. Data on anti-androgens or a possible role of hormone therapy in the chemo-preventive scenario are even less informative.
In summary, we are at the beginning of unraveling the complex molecular mechanisms behind gender disparities in HCC. Among them, estrogens seem to play a role in IL6 production and modulation of gene expression through FOXA transcription factors, what prevents HCC development in experimental models of HCC. However, more data are still needed to define the implication of sexual hormones in the molecular pathogenesis of HCC. This could provide the proof-of-principle to rescue hormone-based drugs for further evaluation as systemic therapies of HCC in certain clinical contexts.
Footnotes
Conflict of interest
The authors declared that they do not have anything to disclose regarding funding or conflict of interest with respect to this manuscript.
References
- 1.Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun M. Cancer statistics, 2009. CA Cancer J Clin. 2009;59:225. doi: 10.3322/caac.20006. [DOI] [PubMed] [Google Scholar]
- 2.El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology. 2007;132:2557–2576. doi: 10.1053/j.gastro.2007.04.061. [DOI] [PubMed] [Google Scholar]
- 3.Boyault S, Rickman DS, De Reyniès A, Balabaud C, Rebouissou S, Jeannot E, et al. Transcriptome classification of HCC is related to gene alterations and to new therapeutic targets. Hepatology. 2006;45:42–52. doi: 10.1002/hep.21467. [DOI] [PubMed] [Google Scholar]
- 4.Villanueva A, Newell P, Chiang D, Friedman SL, Llovet JM. Genomics and signaling pathways in hepatocellular carcinoma. Semin Liver Dis. 2007;27:55–76. doi: 10.1055/s-2006-960171. [DOI] [PubMed] [Google Scholar]
- 5.Li Z, Tuteja G, Schug J, Kaestner KH. Foxa1 and Foxa2 are essential for sexual dimorphism in liver cancer. Cell. 2012;148:72–83. doi: 10.1016/j.cell.2011.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Keng VW, Villanueva A, Chiang DY, Dupuy AJ, Ryan BJ, Matise I, et al. A conditional transposon-based insertional mutagenesis screen for genes associated with mouse hepatocellular carcinoma. Nat Biotechnol. 2009;27:264–274. doi: 10.1038/nbt.1526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ma WL, Hsu CL, Yeh CC, Wu MH, Huang CK, Jeng LB, et al. Hepatic androgen receptor suppresses hepatocellular carcinoma metastasis through modulation of cell migration and anoikis. Hepatology. 2012 Feb 9; doi: 10.1002/hep.25644. [Epub ahead of print]. http://dx.doi:10.1002/hep.25644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Naugler WE, Sakurai T, Kim S, Maeda S, Kim K, Elsharkawy AM, et al. Gender disparity in liver cancer due to sex differences in MyD88-dependent IL-6 production. Science. 2007;317:121–124. doi: 10.1126/science.1140485. [DOI] [PubMed] [Google Scholar]
- 9.Llovet JM. Systematic review of randomized trials for unresectable hepatocellular carcinoma: chemoembolization improves survival. Hepatology. 2003;37:429–442. doi: 10.1053/jhep.2003.50047. [DOI] [PubMed] [Google Scholar]