In this “clinical” contribution to the Bench to Clinic Symposia, we will show data to support the hypothesis that fasting hyperinsulinemia is the initial underlying cause of type 2 diabetes mellitus (T2DM) and that the remission of the disease following bariatric surgery may be due to the correction of hyperinsulinemia. The intent of this article is to elicit critical thinking about the pathophysiology of T2DM in view of the effects of surgery and to open debate. If our hypothesis is correct, then more research resources should be focused on the cause(s) of fasting hyperinsulinemia and the therapies that may correct it.
The questionable, traditional focus on hyperglycemia
The study of diabetes has always focused on glucose. Whether the diagnosis was made by the attraction of flies to urine as described in ancient India in 1552 BC (1), the sweet taste of the urine noted by Shushruta in 400 BC (2), or our current dependence on fasting blood glucose levels, HbA1c, and glucose tolerance curves, the severity of the disease is still measured by the level of hyperglycemia.
Similarly, our therapeutic directions also aim, almost exclusively, to reverse the hyperglycemia. In 1921 when Banting and Best reported that a pancreatic extract reversed the soaring glucose levels following a pancreatectomy in a dog, the use of insulin spread rapidly to children and adults alike. By the time Sir Harold Percival Himsworth noted, in 1936, that there were at least two types of diabetes (3), the objectives of T2DM treatment were already set; goals that still continue today. Even though type 1 diabetes mellitus (T1DM) and T2DM are virtually two opposite diseases, i.e., a total lack of insulin production versus abnormally high levels, the therapeutic goals for both entities continue to be the same: lower glucose levels by 1) giving insulin, 2) increasing insulin production, and/or 3) decreasing insulin resistance.
Is the primary lesion of T2DM insulin resistance or insulin secretion?
The prevailing view of T2DM progression (4) is that the disease is due to an early and progressive loss of insulin sensitivity. To maintain homeostatic levels of glucose, β-cells increase insulin secretion to overcome insulin resistance in peripheral tissues (glucose disposal) and liver (glucose production). T2DM occurs when the β-cells “fail” to produce adequate insulin to meet these demands.
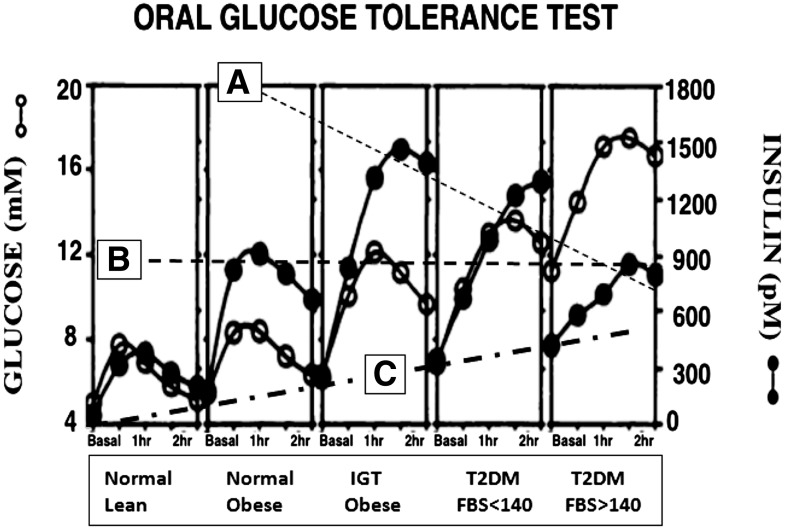
The rise and later fall in insulin secretion with the progression of T2DM is depicted nicely by the glucose tolerance curves that we published in 1992 (Fig. 1) (5). In the lean subjects, glucose homeostasis is achieved by relatively low concentrations of insulin. Glucose-induced insulin secretion increases with the development of obesity and rises even more in the prediabetic state, i.e., impaired glucose tolerance (IGT). As susceptible individuals progress from early T2DM (FBS <140 mg/dL) to advanced disease (FBS >140 mg/dL), peak insulin secretion declines.
Figure 1.
Glucose tolerance curves in five cohorts: normal lean, normal obese, IGT, early T2DM, and advanced T2DM (data previously published [5]). While there is a reduction in peak insulin secretion with progress of T2DM (A), the peak insulin secretion is still higher in advanced disease than in normal subjects (B) and there is an increase in basal insulin secretion (C).
In the traditional view of T2DM, the rise in insulin secretion is due to the primary lesion, i.e., increasing insulin resistance and the hyperglycemia is due to the failure of β-cells to produce enough insulin. The curves in Fig. 1, however, in addition to documenting the decreasing levels of insulin secretion with the progression from IGT to T2DM with FBS >140 (line A in Fig. 1), also show that even with progression of the disease, the maximum insulin concentration is still twice as high as in euglycemic lean individuals (line B in Fig. 1) and, more important, the basal levels of insulin secretion continue to rise as the disease worsens (line C in Fig. 1).
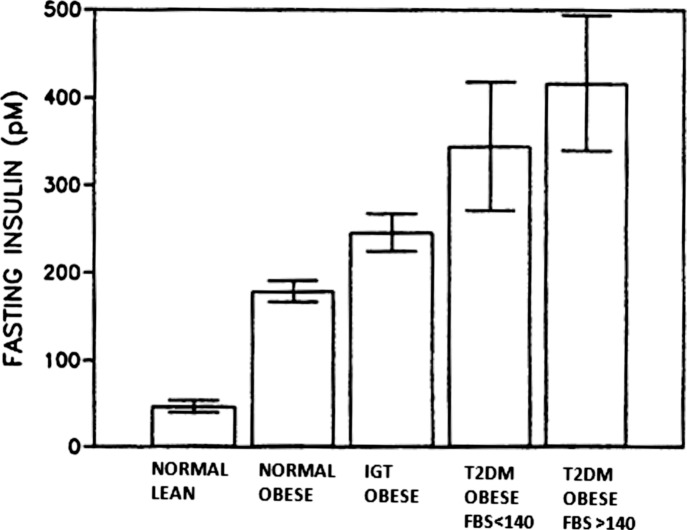
The remarkable extent of the hyperinsulinemia is also documented in Fig. 2. T2DM patients with FBS>140 have basal insulin levels that are nine times higher than those measured in euglycemic lean patients.
Figure 2.
Fasting insulin in normal lean, normal obese, IGT, early T2DM, and advanced T2DM (data previously published [5]).
These data suggest that the difference between the nondiabetic and the diabetic patients is the “insulin baseline,” perhaps due to too much insulin production in the fasting state rather than an inability to secrete enough insulin in response to a meal. Such a view would be supported by the finding that basal-state hyperinsulinemia in healthy normoglycemic adults is predictive of T2DM over a 24-year follow-up (6).
Because the focus of our hypothesis is on the initial cause of T2DM, our discussion is limited to early- and mid-stage disease, i.e., patients with FBS ≤200 mg/dL. We are fully aware of studies in patients with severe, late-stage diabetes, i.e., with FBS levels ≥250 mg/dL, in which the hyperinsulinemia of T2DM is reversed as the β-cells eventually fail to produce enough insulin (7). With final progression of the disease, T2DM becomes similar to clinical presentation of T1DM in that a more absolute state of insulin deficiency exists.
Correction of hyperinsulinemia and prompt remission of diabetes after Roux-en-Y gastric bypass
The unexpected and remarkable ability of bariatric surgery to produce full and durable remission of T2DM (8–13) now offers a new opportunity to review our concepts about the onset of diabetes since, providentially, the Roux-en-Y gastric bypass (RYGB) provides the unusual opportunity to study patients with T2DM and, after the surgery, to assess these same individuals again without the disease.
Our studies as early as 1992 had demonstrated that correction of fasting glucose after bariatric surgery was accompanied by the rapid correction of hyperinsulinemia and, as far as we can determine, most, if not all, of the studies of diabetes remission after RYGB have also observed lowering of fasting insulin levels.
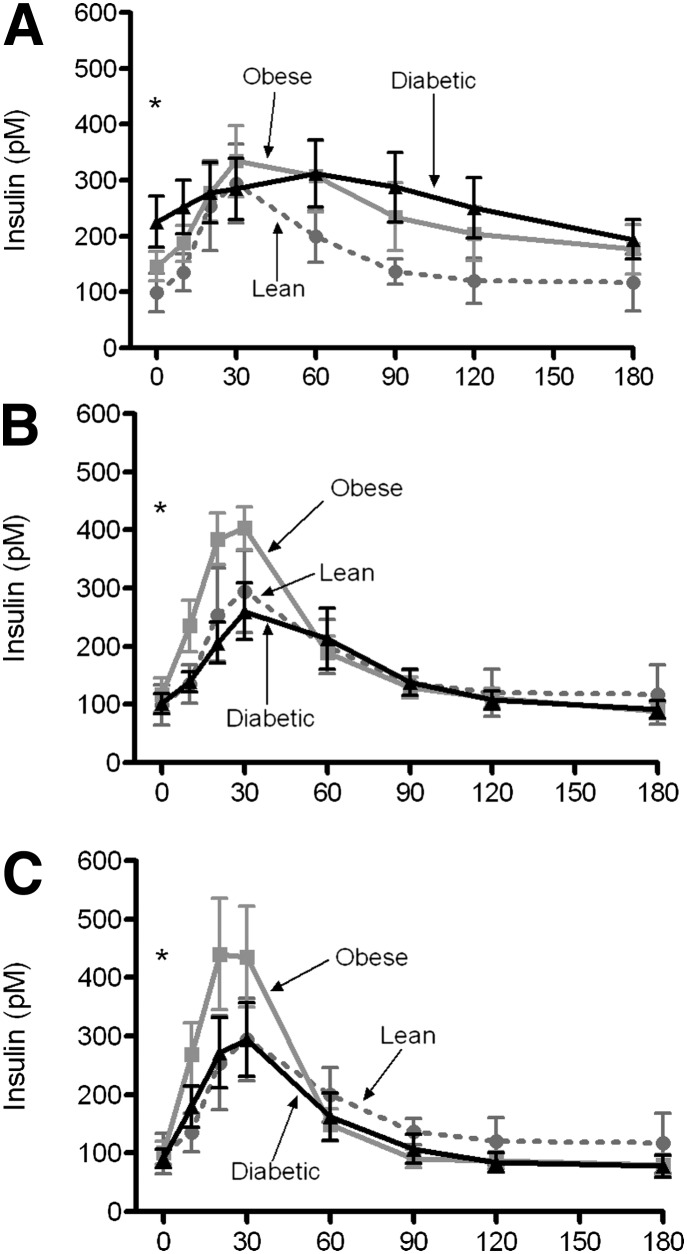
To investigate the relative importance of excessive insulin secretion in early- and mid-stage T2DM, we studied obese-nondiabetic and obese-diabetic patients (FBS of 164 ± 16 and HbA1c of 8.7 ± 0.5) before they had gastric bypass surgery and again 1 week and 3 months after surgery. A group of lean control subjects was also studied for comparison. Data from our article by Reed et al. (14) has been redrawn and is shown in Fig. 3.
Figure 3.
Plasma insulin in obese nondiabetic and diabetic patients after a mixed-meal challenge. Redrawn from the data published by Reed et al. (14). A lean control group is shown each time for comparison before surgery (A), a week after surgery (B), and 3 months after surgery (C).
Prior to the Roux-en-Y surgery, basal insulin levels in obese T2DM subjects are so high that the β-cells can no longer respond to food intake with additional insulin secretion (Fig. 3A). Within a week after the surgery, however, along with the correction of glucose levels and resolution of the T2DM, basal insulin levels return to normal and the food stimulated spike of insulin secretion is restored to levels equal to normal lean control subjects (Fig. 3B and C).
These data demonstrate that the β-cells in the diabetic patients, even after a decade of disease, still retain capacity for insulin secretion sufficient to produce a completely normal insulin response immediately after surgery. Accordingly these results suggest that hyperinsulinemia is the primary lesion in T2DM, and the inability to respond to a mixed meal before surgery is due to the already elevated basal insulin secretion.
Exploring the hyperinsulinemia of T2DM
There are at least three possible explanations for the excessive basal insulin secretion in T2DM that seem reasonable: insulin secretion is elevated 1) as a feedback mechanism to overcome insulin resistance, 2) in response to changes in plasma glucose or plasma free fatty acids, or 3) in response to a signal from the gut. Since the only intervention with bariatric surgery is imposed on the gut, the third explanation seems most plausible and forms the basis of a new hypothesis that will be discussed later.
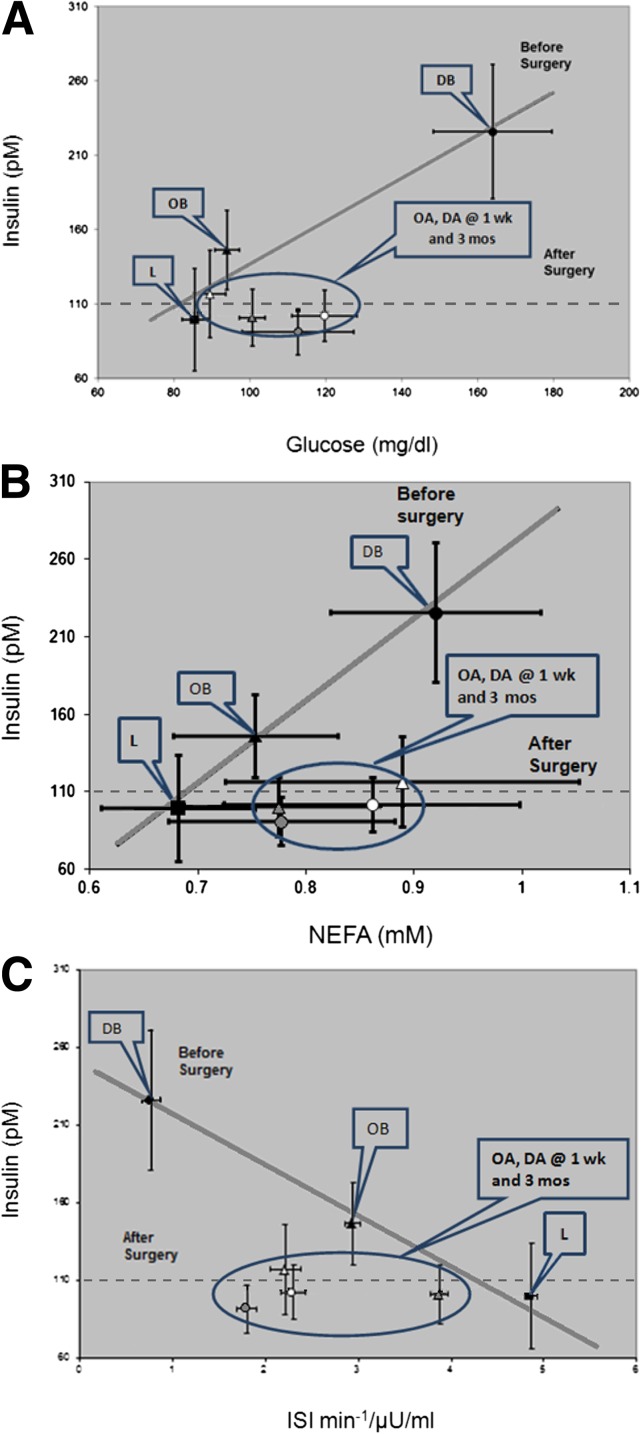
To investigate if fasting insulin is reduced after gastric bypass surgery because of changes in glucose, free fatty acids, and/or insulin resistance, the values for fasting insulin from our study mentioned above (14) are plotted against values for glucose, NEFA, and insulin sensitivity index (Fig. 4A–C)
Figure 4.
Correlations of fasting insulin with fasting plasma glucose (A), fasting plasma free fatty acids (NEFAs) (B), and insulin sensitivity index (ISI) (C). Fasting glucose, fasting insulin, and ISI were previously reported (14). Group symbols: square = lean control group; triangle = obese (nondiabetic) group; circle = diabetic group. Time symbols: black square, triangle, and circle = presurgery; white triangle and circle = week of surgery; gray triangle and circle = 3 months postsurgery. L = lean control group; OB = obese (nondiabetic) group before surgery; DB = diabetic (obese) group before surgery; OA = obese group after surgery; DA = diabetic group after surgery. wk, week; mos, months.
In agreement with many other reports, prior to surgery, fasting glucose, nonesterified fatty acids (NEFAs), and insulin were higher in obese than in lean subjects and even higher in patients with diabetes. Prior to surgery there was a clear direct relationship between 1) fasting glucose and fasting insulin (Fig. 4A), as well as 2) NEFAs and insulin (Fig. 4B), and 3) an inverse relationship between insulin sensitivity and insulin (Fig. 4C).
If fasting insulin is reduced after bariatric surgery because of changes in glucose, free fatty acids, and/or insulin sensitivity, then plasma insulin would be predicted to follow the presurgery regression line to a lower level of both parameters. The results were in stark contrast to this prediction because after surgery fasting insulin levels were as low as those of lean control subjects irrespective of the fasting glucose, free fatty acids, or insulin sensitivity (Fig. 4A–C).
These findings demonstrate that after gastric bypass surgery, fasting insulin is independent of the effects of fasting glucose, fasting free fatty acids, and insulin sensitivity. This “uncoupling” or disassociation of fasting insulin from BMI (kg/m2), fasting glucose, and insulin sensitivity was also seen in nondiabetic subjects who were studied in a weight stable condition more than one year after gastric bypass surgery (14,15). From these results we conclude that correction of hyperinsulinemia is not secondary to changes in glucose, free fatty acids, insulin sensitivity, or BMI but is a primary metabolic change that occurs in response to gastric bypass surgery.
How does correcting hyperinsulinemia result in reversal of diabetes?
It is not intuitively obvious that lowering fasting insulin would also reduce glucose levels, i.e., improve diabetes. If insulin is suppressing liver glucose production, then lowering insulin should increase glucose, i.e., make diabetes worse with a corresponding increase in hepatic glucose output.
Plasma glucose concentration after a 12-h fast is primarily regulated by the rate of hepatic gluconeogenesis, which in turn is regulated by insulin, glucagon, and glucocorticoids. The decrease in insulin after RYGB would be counter-regulatory to reducing gluconeogenesis. Likewise, the changes in the concentrations of glucagon, cortisol, and corticocosterone in patients with diabetes after RYGB do not provide a mechanism to explain the reduction in gluconeogenesis (W.J.P., G.L.D., unpublished data).
Another explanation could be regulation of gluconeogenesis through substrate supply. Consoli et al. (16) demonstrated that appearance rates of lactate and alanine were greater in diabetic patients than in nondiabetic patients. Likewise, conversion rates of lactate and alanine to glucose were greater in diabetic subjects.
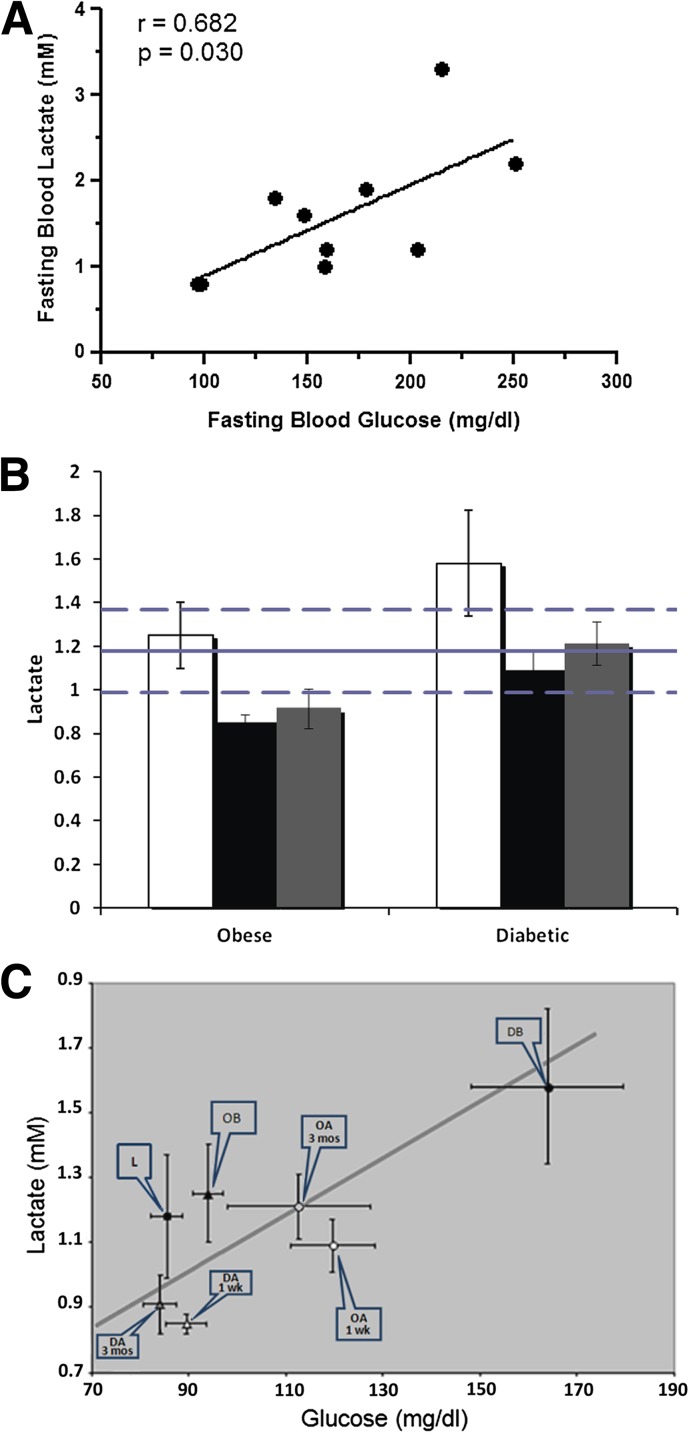
To examine if changes in lactate production might explain the changes in fasting glucose, we assayed plasma samples from the study mentioned above (14). Before surgery, fasting lactate concentrations were significantly correlated with fasting glucose in the diabetic group (Fig. 5A). After RYGB surgery, lactate was dramatically reduced in diabetic patients (Fig. 5B). We also have preliminary data (W.J.P., G.L.D., unpublished data) that fasting concentrations of pyruvate and alanine are reduced after RYGB in the same fashion as lactate. The reduction in lactate after surgery is related to the decreases in fasting glucose (Fig. 5C). Although correlations do not prove cause and effect, these data lead us to speculate that a reduction in production of lactate reduces the substrate for gluconeogenesis and thus leads to lower plasma glucose concentration after RYGB.
Figure 5.
Plasma lactate in normal lean control subjects and in diabetic and nondiabetic (obese) patients before and after RYGB. Fasting plasma samples from the study reported by Reed et al. (14) were analyzed for lactate. A: Correlation of fasting plasma lactate with fasting plasma glucose in diabetic patients before surgery. B: Fasting plasma lactate in diabetic and nondiabetic (obese) patients before and after surgery. The mean value ± SEM for a control lean group is shown as a solid ± the dashed lines. White bars show data prior to surgery, black bars show data at 1 week after surgery, and gray bars show data at 3 months after surgery. C: Correlation of fasting plasma lactate and fasting plasma glucose in lean, obese, and diabetic groups before and after RYGB. Group symbols: square = lean control group; triangle = obese (nondiabetic) group; circle = diabetic group. Time symbols: black square, triangle, and circle = presurgery; white triangle and circle = week of surgery; gray triangle and circle = 3 month postsurgery. L = lean control group; OB = obese (nondiabetic) group before surgery; DB = diabetic (obese) group before surgery; OA = obese group after surgery; DA = diabetic group after surgery. wk, week; mos, months.
The questions that remain are why is fasting lactate high in a diabetic patient, and how does RYGB reduce it to normal? The most likely answer is that the muscle cannot manage the large excess of “fuel.” In spite of insulin resistance, it is likely that the muscle is taking up more glucose than it needs or can store during fasting hyperinsulinemia. Once it is converted to glucose 6-phosphate, the only way for the muscle to “export” carbons is through conversion to pyruvate with subsequent conversions to lactate and alanine and transport into blood.
The concurrently elevated levels in fasting glucose and lactate in diabetic patients suggest an upregulated Cori cycle. In the Cori cycle, lactate produced by muscle goes to the liver where it is converted to glucose and then returned to the muscle where lactate is again formed through glycolysis. Since hyperglycemia is an undesirable outcome we might say that we have a “vicious Cori cycle” in diabetic patients. After RYGB, both fasting insulin and lactate are reduced, which leads us to speculate that the correction of hyperinsulinemia leads to less gluconeogenic substrate production and resolution of hyperglycemia.
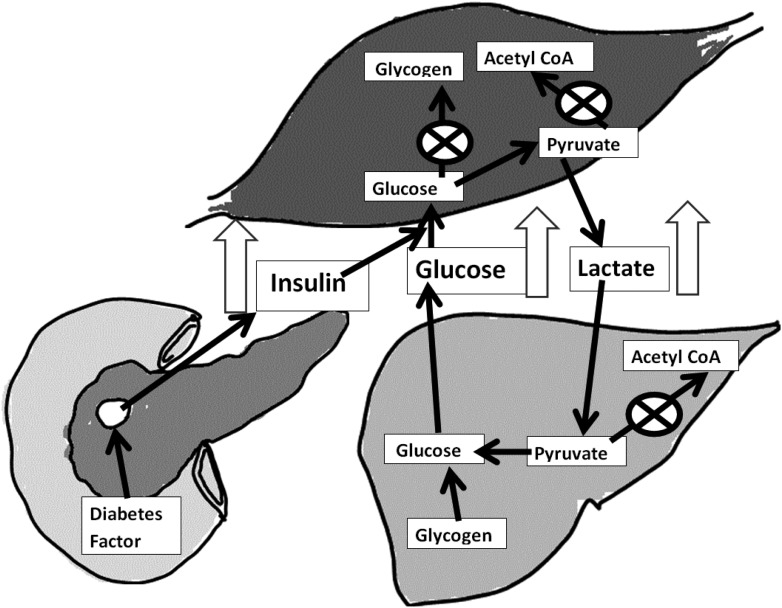
A new hypothesis for the cause of diabetes
Our results from these studies of diabetic patients who have remission of diabetes after RYGB lead us to propose a new hypothesis for the mechanism causing diabetes and how RYGB is able to reverse the disease. T2DM starts with a diabetogenic signal from the gastrointestinal (GI) tract to the islets that causes a chronic and increasing basal hyperinsulinemia that in turn blunts the normally spiking insulin response to a meal. This, plus the muscle insulin resistance that accompanies diabetes, reduces glucose clearance. Further, during overnight fasting, this continuous basal hyperinsulinemia causes the muscle to release chronically high amounts of gluconeogenic substrates with subsequent chronically elevated hepatic production of glucose. This situation is diagramed in Fig. 6.
Figure 6.
Fasting metabolism in T2DM. When glycogen stores are full and there is no energy demand on the muscle, acetyl-CoA and NADH accumulate. These are feedback regulators of pyruvate dehydrogenase, and thus pyruvate will accumulate. The NADH generated from glycoloysis is used to reduce pyruvate to lactate, which is transported by the blood to the liver where it is converted to glucose by gluconeogenesis.
When a diabetic patient has an RYGB, the GI diabetogenic signal is no longer generated, and the fasting hyperinsulinemia is corrected. Lowering fasting insulin results in lower production of pyruvate, lactate, and alanine in muscle. and gluconeogenesis in liver is subsequently reduced. With lower concentrations of insulin in the fasting state, insulin secretion in response to a meal is “normalized,” and the muscle can respond by lower glucose uptake during fasting and increased glucose uptake in response to a meal.
Conclusions and implications
The hypothesis that hyperinsulinemia is the underlying mechanism causing diabetes is not new. Jesse Roth and colleagues (6,17) made a strong case for fasting hyperinsulinemia causing insulin resistance and development of diabetes. In her Banting Lecture at the 2011 American Diabetes Association Scientific Sessions, Dr. Barbara Corkey (18) (who has authored the “bench” contribution for this Bench to Clinic Symposia) presented convincing evidence in animals for the development of hyperinsulinemia and insulin resistance. Our contribution to the discussion comes from the observation in man that fasting insulin rises with the progression of T2DM and normalizes to levels like lean control subjects almost immediately after gastric bypass surgery. This correction of hyperinsulinemia after RYGB occurs simultaneously with the full and durable resolution of diabetes and is independent of changes in weight loss, insulin sensitivity, glucose, or free fatty acids. The primary manipulation in the surgery is exclusion of food from a portion of the GI track. Thus, it seems reasonable to propose that a diabetogenic signal from the gut to the islets is the cause of hyperinsulinemia. Remission of diabetes and correction of pathologically high fasting levels of insulin after RYGB is accompanied by reduced levels of lactate. From this we further propose that remission of diabetes is due to reduced lactate production in muscle and subsequent normalization of substrate driven glucose production through gluconeogenesis.
If this hypothesis, i.e., that the critical lesion in T2DM is hyperinsulinemia, is true, the treatment of T2DM with insulin needs review. While insulin may be required in the very late stages of T2DM when there is no longer enough β-cell reserve, it might be harmful to administer the hormone when the intrinsic fasting basal levels are still elevated. We do not treat hyperthyroidism with thyroxine or Cushing syndrome with cortisone; should we be treating T2DM, a disease characterized by hyperinsulinemia, with insulin?
Acknowledgments
W.J.P. receives grant funding from the National Institutes of Health, Johnson & Johnson, Health Resources and Services Administration, and Golden Leaf. G.L.D. receives grant funding from GlaxoSmithKline and Johnson & Johnson. No other potential conflicts of interest relevant to this article were reported.
Footnotes
See accompanying article, p. 2432.
References
- 1.Das AK, Shah S. History of diabetes: from ants to analogs. J Assoc Physicians India 2011;59(Suppl.):6–7 [PubMed] [Google Scholar]
- 2.Tipton CM. Susruta of India, an unrecognized contributor to the history of exercise physiology. J Appl Physiol 2008;104:1553–1556 [DOI] [PubMed] [Google Scholar]
- 3.Kim SH. Measurement of insulin action: a tribute to Sir Harold Himsworth. Diabet Med 2011;28:1487–1493 [DOI] [PubMed] [Google Scholar]
- 4.DeFronzo RA. Banting Lecture. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus. Diabetes 2009;58:773–795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pories WJ, MacDonald KG, Jr, Morgan EJ, et al. Surgical treatment of obesity and its effect on diabetes: 10-y follow-up. Am J Clin Nutr 1992;55(Suppl.):582S–585S [DOI] [PubMed] [Google Scholar]
- 6.Dankner R, Chetrit A, Shanik MH, Raz I, Roth J. Basal-state hyperinsulinemia in healthy normoglycemic adults is predictive of type 2 diabetes over a 24-year follow-up: a preliminary report. Diabetes Care 2009;32:1464–1466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reaven GM, Hollenbeck C, Jeng CY, Wu MS, Chen YD. Measurement of plasma glucose, free fatty acid, lactate, and insulin for 24 h in patients with NIDDM. Diabetes 1988;37:1020–1024 [DOI] [PubMed] [Google Scholar]
- 8.Pories WJ, Flickinger EG, Meelheim D, Van Rij AM, Thomas FT. The effectiveness of gastric bypass over gastric partition in morbid obesity: consequence of distal gastric and duodenal exclusion. Ann Surg 1982;196:389–399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pories WJ, MacDonald KG, Jr, Flickinger EG, et al. Is type II diabetes mellitus (NIDDM) a surgical disease? Ann Surg 1992;215:633–642; discussion 643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pories WJ, Swanson MS, MacDonald KG, et al. Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg 1995;222:339–350; discussion 350–352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Buchwald, H, Estok R, Fahrbach K, et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med 2009;122:248–256.e5 [DOI] [PubMed]
- 12.Schauer PR, Kashyap SR, Wolski K, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med 2012;366:1567–1576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mingrone G, Panunzi S, De Gaetano A, et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med 2012;366:1577–1585 [DOI] [PubMed] [Google Scholar]
- 14.Reed MA, Pories WJ, Chapman W, et al. Roux-en-Y gastric bypass corrects hyperinsulinemia implications for the remission of type 2 diabetes. J Clin Endocrinol Metab 2011;96:2525–2531 [DOI] [PubMed] [Google Scholar]
- 15.Bikman BT, Zheng D, Pories WJ, et al. Mechanism for improved insulin sensitivity after gastric bypass surgery. J Clin Endocrinol Metab 2008;93:4656–4663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Consoli A, Nurjhan N, Reilly JJ, Jr, Bier DM, Gerich JE. Mechanism of increased gluconeogenesis in noninsulin-dependent diabetesmellitus. Role of alterations in systemic, hepatic, and muscle lactate and alanine metabolism. J Clin Invest 1990;86:2038–2045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shanik MH, Xu Y, Skrha J, Dankner R, Zick Y, Roth J. Insulin resistance and hyperinsulinemia: is hyperinsulinemia the cart or the horse? Diabetes Care 2008;31(Suppl. 2):S262–S268 [DOI] [PubMed] [Google Scholar]
- 18.Corkey BE. Banting Lecture 2011. Hyperinsulinemia: cause or consequence? Diabetes 2012;61:4–13 [DOI] [PMC free article] [PubMed] [Google Scholar]