Abstract
Introduction
Symptomatic thoracic disc herniations (TDHs) are uncommon and can be surgically treated. Although transthoracic decompression is considered the gold standard, it is associated with significant comorbidities. In particular, approach via a posterior laminectomy has been associated with poor results. Several strategies have been developed for the resection of TDHs without manipulating the spinal cord. We describe a minimally invasive technique by using 3-D navigation and tubular retractors with the aid of a robotic holder via an oblique paraspinal approach.
Materials and Methods
The 20-mm working tube via an oblique trajectory through the fascia provides a good surgical field for thoracic discectomy through a microscope. We present our first five patients with TDHs operated using this minimally invasive approach.
Results
Neurological symptoms were improved postoperatively, and there were no surgical complications. There was no instability or recurrence during the follow-up period.
Conclusion
The oblique paraspinal approach may offer an alternative surgical option for treating TDHs.
Keywords: Oblique paraspinal approach, O-arm, Robotic arm, Thoracic disc herniation, Tubular retractor
Introduction
Thoracic disc herniations (TDHs) are less common than cervical or lumbar disc herniations and account for 0.15–1.8 % of all disc herniations treated surgically [1–3]. The primary goal of surgical treatment for TDHs is to achieve complete decompression of the spinal cord or nerve root and to prevent recurrence of disc herniation while avoiding iatrogenic cord injury. Conventional decompressive laminectomy is associated with high morbidity rates. As a result, alternative surgical approaches, such as anterior (transthoracic, transsternal, and thoracoscopic) [4, 5], lateral (lateral extracavitary and costotransversectomy) [6–9], and posterolateral (transpedicular and transfacet pedicle sparing) [10–14], have been developed for resection of TDHs.
Minimized surgical exposure has become increasingly popular in spine surgery and a percutaneous thoracic endoscopic technique has been introduced [15, 16]. Endoscopy is useful in soft disc herniation, but has limited indications. Furthermore, the use of this technique on migrated or calcified TDHs is difficult. Accordingly, we propose an oblique paraspinal approach for TDHs by using a minimally invasive tubular retractor, which is a combination of transforaminal (bony window) and percutaneous thoracic endoscopic technique (entry and trajectory).
Methods
Patients
Between January 2010 and May 2010, five patients underwent surgery via a minimally invasive oblique paraspinal approach for TDHs. The mean age of the patients was 57.6 years (range 32–79 years). All patients experienced a single-level disc herniation at the thoracic spine, with the level of herniation ranging from T6 through T11. All patients showed axial pain and four of the five patients had myelopathy. Only one surgeon (H.-Y. Lee) performed the minimally invasive oblique paraspinal approach for TDHs.
Surgical technique
Under general anesthesia with single-lumen endotracheal tube, the patient was placed in a prone position on a radiolucent frame. The patient was monitored for motor and somatosensory evoked potentials prior to turning the patient prone. We used a series of spinal needles placed at intervals to count spinal levels starting at S1. After localization, the usual skin preparation and draping were done. The navigation system (Stealthstation® TREON™ system, Medtronic Sofamor Danek, Memphis, TN) based on O-arm® (Medtronic Sofamor Danek, Memphis, TN) was activated to decide skin entry and the trajectory of the tube retractor. The skin incision was determined from a preoperative CT or MR scan by extrapolating the line from mid-pedicular annulus to the lateral margin of the facet and extending it up to the skin surface. We further confirmed the intended skin incision level with the help of spinal navigation and a longitudinal skin incision of approximately 2 cm was made approximately 5–6 cm lateral to the posterior midline. The 2-cm incision of fascia was also made via the oblique trajectory. We used a METRx tubular retractor (Medtronic Sofamor Danek, Memphis, TN) to minimize the incision (Fig. 1a). A robotic arm was then placed across the table from the surgeon. This robotic arm (Unitrac®, Aesculap, Tuttlingen, Germany) is used for a stiffer angle and because of its strong holding power as a pneumatic holding device (Fig. 1b). After the tube was inserted, we checked its position with a navigation system. To appropriately position the tube, a posterior–lateral portion of the transverse process was confirmed with navigation and drilled out. The tubular retractor of the appropriate length was subsequently placed.
Fig. 1.

A 2-cm tubular retractor was inserted using the oblique paraspinal approach (a). A robotic arm was provided for stiffer angle (b)
Then, we exposed the medial portion of the transverse process and facet joint at these levels (Fig. 2). Under an oblique view via a microscope, the lateral portion of the upper and lower facets was drilled out carefully by using a high-speed diamond burr. A careful dissection was performed to identify the exiting root. The exposed field included the lateral margin of the thecal sac and the exiting nerve root. Discectomy was performed with minimal cord retraction with oblique inclination of the microscope and operation table (Fig. 3). Finally, hemostasis was achieved, the tubular retractor was withdrawn, and a wound drain was placed.
Fig. 2.

A tubular retractor placed at the lateral part of the facet joint between transverse processes
Fig. 3.
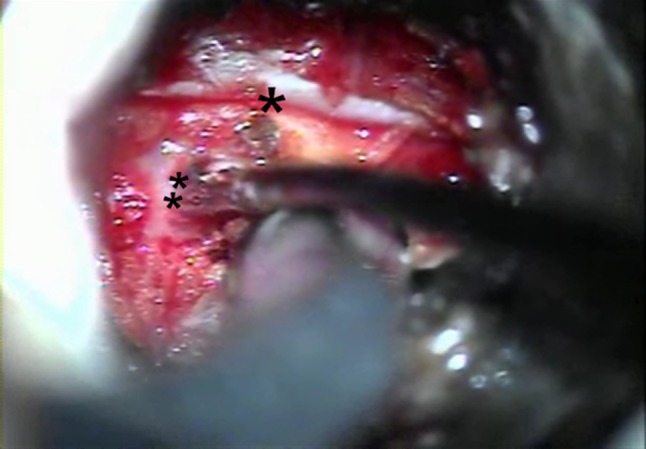
An intraoperative photograph showing the dura (*) and exiting nerve root (**). The herniated disc particle was removed after gentle dissection
Illustrative cases and results
The average operation time when using the oblique paraspinal approach was 80 min (range 60–90 min). The average estimated blood loss was 144 ml (range 70–350 ml). The average hospital stay was 7.4 days (3–13 days) (Table 1). During surgery, there was no dural tear or CSF leakage. By SSEP, MEP monitoring, there was no deterioration of neurological status at the time of surgery. All patients experienced relief from their preoperative symptoms. The average follow-up period was 9.6 months (4–13 months). Serial radiographs showed no instability during the follow-up period.
Table 1.
Summary of patient series
| Case no. | Age | Sex | Level | Date of op. | Time for op. | Blood loss (cc) | LOS (days) | Symptoms | FU (mos) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 79 | F | T9/10 | 06/01/10 | 75 | 120 | 13 | Axial pain, myelopathy | 10 |
| 2 | 66 | F | T10/11 | 27/01/10 | 60 | 100 | 13 | Axial pain, myelopathy | 4 |
| 3 | 32 | M | T7/8 | 03/03/10 | 85 | 80 | 5 | Axial pain, myelopathy | 13 |
| 4 | 43 | F | T8/9 | 17/03/10 | 90 | 70 | 3 | Axial pain, radiculopathy | 11 |
| 5 | 68 | M | T6/7 | 24/05/10 | 90 | 350 | 3 | Axial pain, myelopathy | 10 |
LOS length of hospital stay, FU follow-up
Case 3
A 32-year-old man presented with a 6-month history of axial pain and numbness of his left leg. MR images revealed a marked left paracentral T7–8 calcified disc herniation with spinal cord compression (Fig. 4a, b). The surgery was performed via an oblique paraspinal approach using a minimally invasive tubular retractor. After drilling the lateral portion of the upper and lower facets, the posterior body was drilled using a high-speed diamond burr until a thin cortical shell was left on the anterior wall of the canal with the calcified herniated disc. The herniated disc and thin bony shell were pushed down and then removed without cord retraction. Neurological symptoms improved postoperatively, and there were no surgical complications. There was no instability and recurrence during the follow-up 10 months.
Fig. 4.

MR images revealed a T7–8 disc herniation (a). A left paracentral disc herniation causes marked spinal cord compression at the coronal image (b)
Case 4
A 43-year-old woman presented with a 2-year history of mid-back, left flank, and abdominal pain. She complained of lower extremity weakness, bladder dysfunction, and paresthesia. Preoperative MRI and CT revealed a soft, up-migrated disc herniation at T8–9 with left-sided cord compression (Fig. 5a, b). The patient reported immediate postoperative relief from flank and abdominal pain. Postoperative MRI scans showed complete removal of the herniated disc (Fig. 5c). The patient was discharged on postoperative day 4 with some mild incisional pain.
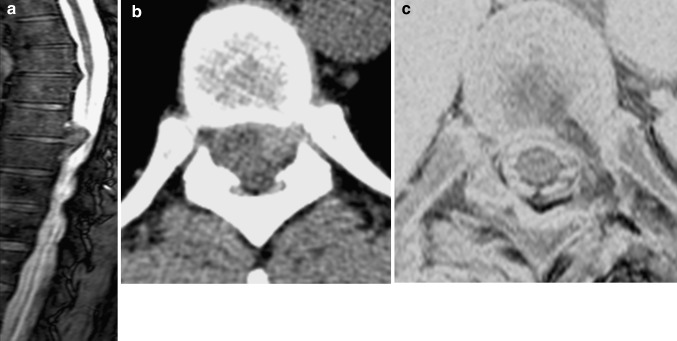
Fig. 5.
Sagittal T2-weighted MRI image showing a thoracic disc herniation at T8–9 with cord compression (a). Axial slice CT scans of T8–9 soft disc herniation (b). A postoperative T2-weighted axial MRI scan showing complete decompression of the T8–9 disc herniation (c) MRI scan obtained on postoperative day 1
Discussion
Patients with symptomatic TDHs constitute 0.15–1.8 % of the patients requiring disc operations [10]. The exposure to the disc space provided by the anterolateral and lateral approaches is excellent [6], and these approaches are best suited for calcified discs. However, these procedures are extensive, with potential surgical complications and significant morbidity due to single lung ventilation, chest tube placement, atelectasis, and intercostal neuralgia [14]. Conventional decompressive laminectomy is also associated with high morbidity rates. Significant postoperative deficits, the majority including paralysis, have been reported [17]. Therefore, Black [18] described an alternative, posterior-based technique of laminotomy and medial facet approach for thoracic discectomy, which have been performed for the treatment of lateral or paracentral TDH due to their straightforward exposure [7, 11]. However, in posterior techniques, the resection of disc and osteophytic spurs in the midline and contralaterally is performed blindly in that the instruments are inserted beneath the dura.
More limited posterolateral approaches are being introduced for the treatment of TDHs. Stillerman introduced the transfacet pedicle-sparing approach [10]. The transpedicular procedure, introduced by Patterson and Arbit [12], was followed by Stillerman et al. [7, 10]. The transfacet or transpedicular approaches introduced via posterolateral trajectory may be used for soft central discs and calcified centrolateral discs at all levels. Bransford et al. [14] reported a modified transfacet pedicle-sparing decompression and fusion, where they treated centrally or paracentrally located TDH by improved exposure.
Nowadays, a less invasive surgical procedure is in demand. A thoracic endoscopic technique has also been introduced as a minimal invasive procedure [15]. Choi et al. performed percutaneous endoscopic thoracic discectomy (PETD) using a rigid working channel endoscope and bone cutting technique (foraminoplasty). Because the thoracic intervertebral foramen is small, they suggest that a widening procedure is needed to introduce the cannula into it. Despite the foraminoplasty, the motion of the thoracic endoscope remains limited. Thus, PETD has limited indications. Sequestrated, calcified, or hard disc herniations are not indicated.
To overcome the limitations of PETD, we applied an oblique paraspinal approach in TDH. Wiltse et al. [19–21] described a paraspinal approach to the lumbar spine in 1968. Moon and Kim have also reported a paraspinal approach for disc herniation of the upper lumbar and thoracolumbar junction. In a thoracic approach, we can use the same approach of PETD. However, we suggest widening the foramen to approach the herniated disc and use a stronger instrument than PETD. Thus, it can be indicated in patients who have migrated or calcified disc. The oblique paraspinal approach allows for minimal neural retraction of the thecal sac by tilting the table and the microscope. Furthermore, it can be performed as a minimally invasive procedure by using a navigation and tube system.
The tubular retractor system achieved excellent clinical results as a minimally invasive surgical approach. A METRx system procedure divided into the paraspinal musculature and was seated firmly on bony anatomy. Usually, the flexible arm was attached to a bed rail and the selected tubular retractor. However, the holding power was weakened in an oblique angle. We applied a pneumatic holding device (Unitrac®, Aesculap, Tuttlingen, Germany). A robotic arm provided for stiffer angle.
In most posterolateral techniques, the resection of central disc and osteophytic spurs has been performed blindly. In contrast, more direct visualization of the central portion via an oblique trajectory was possible. The more central portion can be decompressed via a lateral extracavitary approach (LECA) compared to a posterolateral approach [22]. The visual angle of our oblique paraspinal approach was similar to the angle of LECA. By using a tubular retractor, a more minimally invasive surgery was possible. However, resection of a central calcified disc can be very difficult. Although a bilateral approach can be used to perform ventral decompression as a “floating method”, additional segmental fusion is needed to protect from secondary instability and re-herniation [14]. Our study is limited by the small number of patients, the short follow-up period, and the lack of clinical outcomes, ASIA scores, VAS scores, and Nurick levels. Nevertheless, we do hope that this minimally invasive oblique paraspinal approach offers an alternative approach in those with TDH.
Conclusion
The use of an oblique paraspinal approach of the tubular retractor system for thoracic discectomy is a relatively simple and effective technique. We suggest considering this approach when treating centrolateral calcified or soft migrated thoracic disc herniations using minimally invasive surgery.
Conflict of interest
None.
References
- 1.Okada Y, Shimizu K, Ido K, Kotani S. Multiple thoracic disc herniations: case report and review of the literature. Spinal Cord. 1997;35:183–186. doi: 10.1038/sj.sc.3100357. [DOI] [PubMed] [Google Scholar]
- 2.Awwad EE, Martin DS, Smith KR, Jr, Baker BK. Asymptomatic versus symptomatic herniated thoracic discs: their frequency and characteristics as detected by computed tomography after myelography. Neurosurgery. 1991;28:180–186. doi: 10.1227/00006123-199102000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Benjamin V. Diagnosis and management of thoracic disc disease. Clin Neurosurg. 1983;30:577–605. doi: 10.1093/neurosurgery/30.cn_suppl_1.577. [DOI] [PubMed] [Google Scholar]
- 4.Stillerman CB, Weiss MH. Management of thoracic disc disease. Clin Neurosurg. 1992;38:325–352. [PubMed] [Google Scholar]
- 5.Bohlman HH, Zdeblick TA. Anterior excision of herniated thoracic discs. J Bone Joint Surg Am. 1988;70:1038–1047. [PubMed] [Google Scholar]
- 6.Dietze DD, Fessler RG. Thoracic disc herniations. Neurosurg Clin N Am. 1993;4:75–90. [PubMed] [Google Scholar]
- 7.Stillerman CB, Chen TC, Couldwell WT, Zhang W, Weiss MH. Experience in the surgical management of 82 symptomatic herniated thoracic discs and review of the literature. J Neurosurg. 1998;88:623–633. doi: 10.3171/jns.1998.88.4.0623. [DOI] [PubMed] [Google Scholar]
- 8.Rossitti S. Modified lateral approach for surgery of thoracic disk herniation. Technical note. Arq Neuropsiquiatr. 1994;52:227–230. doi: 10.1590/S0004-282X1994000200013. [DOI] [PubMed] [Google Scholar]
- 9.Fessler RG, Dietze DD, Jr, Millan MM, Peace D. Lateral parascapular extrapleural approach to the upper thoracic spine. J Neurosurg. 1991;75:349–355. doi: 10.3171/jns.1991.75.3.0349. [DOI] [PubMed] [Google Scholar]
- 10.Stillerman CB, Chen TC, Day JD, Couldwell WT, Weiss MH. The transfacet pedicle-sparing approach for thoracic disc removal: cadaveric morphometric analysis and preliminary clinical experience. J Neurosurg. 1995;83:971–976. doi: 10.3171/jns.1995.83.6.0971. [DOI] [PubMed] [Google Scholar]
- 11.Bilsky MH. Transpedicular approach for thoracic disc herniations. Neurosurg Focus. 2000;9:e3. doi: 10.3171/foc.2000.9.4.4. [DOI] [PubMed] [Google Scholar]
- 12.Patterson RH, Arbit E. A surgical approach through the pedicle to protruded thoracic discs. J Neurosurg. 1978;48:768–772. doi: 10.3171/jns.1978.48.5.0768. [DOI] [PubMed] [Google Scholar]
- 13.Simpson JM, Silveri CP, Simeone FA, Balderston RA, An HS. Thoracic disc herniation. Re-evaluation of the posterior approach using a modified costotransversectomy. Spine (Phila Pa 1976) 1993;18:1872–1877. doi: 10.1097/00007632-199310000-00025. [DOI] [PubMed] [Google Scholar]
- 14.Bransford R, Zhang F, Bellabarba C, Konodi M, Chapman JR. Early experience treating thoracic disc herniations using a modified transfacet pedicle-sparing decompression and fusion. J Neurosurg Spine. 2010;12:221–231. doi: 10.3171/2009.9.SPINE09476. [DOI] [PubMed] [Google Scholar]
- 15.Choi KY, Eun SS, Lee SH, Lee HY. Percutaneous endoscopic thoracic discectomy; transforaminal approach. Minim Invasive Neurosurg. 2010;53:25–28. doi: 10.1055/s-0029-1246159. [DOI] [PubMed] [Google Scholar]
- 16.Haufe SM, Mork AR, Pyne M, Baker RA. Percutaneous laser disc decompression for thoracic disc disease: report of 10 cases. Int J Med Sci. 2010;7:155–159. doi: 10.7150/ijms.7.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Arce CA, Dohrmann GJ. Herniated thoracic disks. Neurol Clin. 1985;3:383–392. [PubMed] [Google Scholar]
- 18.Black P. Laminotomy/medial facet approach in the excision of thoracic disc herniation. Neurosurg Focus. 2000;9:e6. doi: 10.3171/foc.2000.9.4.6. [DOI] [PubMed] [Google Scholar]
- 19.Wiltse LL, Bateman JG, Hutchinson RH, Nelson WE. The paraspinal sacrospinalis-splitting approach to the lumbar spine. J Bone Joint Surg Am. 1968;50:919–926. [PubMed] [Google Scholar]
- 20.Kim JS, Lee SH, Moon KH, Lee HY. Surgical results of the oblique paraspinal approach in upper lumbar disc herniation and thoracolumbar junction. Neurosurgery. 2009;65:95–99. doi: 10.1227/01.NEU.0000348299.89232.C2. [DOI] [PubMed] [Google Scholar]
- 21.Moon KH, Lee SH, Kong BJ, Shin SW, Bhanot A, Kim DY, Lee HY. An oblique paraspinal approach for intracanalicular disc herniations of the upper lumbar spine: technical case report. Neurosurgery. 2006;59:ONSE487–ONSE488. doi: 10.1227/01.NEU.0000232772.82860.75. [DOI] [PubMed] [Google Scholar]
- 22.Khoo LT, Smith ZA, Asgarzadie F, Barlas Y, Armin SS, Tashjian V, Zarate B. Minimally invasive extracavitary approach for thoracic discectomy and interbody fusion: 1-year clinical and radiographic outcomes in 13 patients compared with a cohort of traditional anterior transthoracic approaches. J Neurosurg Spine. 2011;14:250–260. doi: 10.3171/2010.10.SPINE09456. [DOI] [PubMed] [Google Scholar]