Abstract
Background:
Caregivers of individuals suffering from psychiatric illness are at risk of being subjected to mental health consequences such as depression, anxiety and burnout. Community-based studies proved that 18–47% of caregivers land in depression. The caregiver burden can be quantified into objective, subjective and demand burdens. There is paucity of data comparing the caregiver burden of psychiatric patients and that of chronic medical illness patients.
Aims and Objectives:
(1) To compare the caregiver burden in psychiatric illness and chronic medical illness. (2) To study the association of caregiver burden with demographic factors like age, gender, duration of caregiving.
Materials and Methods:
The study included two groups of caregivers, each of 50 members. Group 1 consisted of caregivers of psychiatric patients and group 2 consisted of caregivers of chronic medical illness patients. The Montgomery Borgatta Caregiver Burden scale was used to assess the burden in terms of objective, subjective and demand burdens.
Results and Conclusion:
The caregiver burden scores in the caregivers of psychiatric patients were significantly higher than that of chronic medical illness (P<0.0001). The caregiver burden was found to increase with the duration of illness as well as with the age of caregiver. The caregiver burden in the sample population was less as the objective and demand burden did not cross the reference higher value in the given scale, whereas the emotional impact given by the subjective burden was on higher side.
Keywords: Burden, caregiver, Illness, psychiatric
INTRODUCTION
Caregiver is an individual who has the responsibility of meeting the physical and psychological needs of the dependent patient. Psychiatric patients need assistance or supervision in their daily activities and this often places a major burden on their caregivers, thereby placing the caregiver at a great risk of mental and physical health problems. The term “caregiver burden” is used to describe the physical, emotional and financial toll of providing care. As the disease progresses, it carries with it a tremendous increase of burden on the caregiver who does the caregiving. The burden perceived by caregivers of patients with psychiatric illness is a fundamental prognostic aspect as the caregiver burden is reportedly a critical determinant for negative caregiving outcomes.
The burden upon caregivers for a mentally ill patient living at home was first acknowledged by Grad and Sainbury in the early 1960s.[1] The most common mental health consequences identified are depression, anxiety and burnout which occurs when a caregiver slips beyond exhaustion or depression. Studies conducted showed that caregivers reported burden in different areas including effects on family functioning, social isolation, financial problems, and health. Most of the notable community-based studies proved that 18–47% of caregivers land in depression.[2] It is also known that caring for someone with psychiatric illness is associated with a higher level of stress than caring for someone with functional impairment from other chronic medical illnesses. Many authors opine that the level of burden does not correlate with the duration of illness, but has enough variability with age, gender and educational status.[3] A previous study concluded that poor social support and severity of illness have major role in determining the amount of burden on a caregiver.[4]
The burden perceived by caregivers of patients with psychiatric illness is a fundamental prognostic aspect in the history of the disease, and the caregiver burden is reportedly a critical determinant for negative caregiving outcomes. Different questionnaires and scales have been developed to quantify the caregiver burden. Caregiver burden is categorized in terms of objective burden (OB), subjective burden (SB) and demand burden (DB). OB is defined as “the extent of disruptions or changes in various aspects of the caregivers’ life and household. It measures the disruption of the caregiver's life”. SB is defined as “the caregivers’ attitude or emotional reactions to the caregiving experience. It measures emotional impact of caregiving on the caregiver”. DB measures “the extent to which the caregiver feels the responsibilities are overly demanding”. The assessment of burden has become a challenging task for most researchers because cultural, ethical, religious and other personal values may influence perceptions of meaning and consequences of burden.
There is a paucity of data comparing the caregiver burden of psychiatric patients to that of chronic medical illness. The objective of this study is to evaluate the contrast between the caregiver burden of psychiatric and chronic medical illness patients and to study the association between demographic factors like age, gender, duration of care-giving and caregiver burden.
MATERIALS AND METHODS
The study sample consisted of caregivers of psychiatric inpatients admitted in the Government Hospital for Mental Care who were diagnosed as per the guidelines given in ICD-10. The psychiatric sample included schizophrenia (22 cases), mood disorder (16 cases) and substance abuse (14 cases), and caregivers of patients suffering from chronic medical illnesses such as refractory tuberculosis, chronic bronchial asthma, diabetes mellitus, rheumatoid arthritis, and lodged in the King George Hospital and Tuberculosis, Chest disease Hospitals located in Visakhapatnam. The caregivers were classified as group 1 (G1) consisting of 50 caregivers of psychiatric patients and group 2 (G2) consisting of appropriately matched caregivers of patients suffering from chronic medical illness. For every patient, a single caregiver was considered.
Inclusion and exclusion criteria
Caregivers aged more than 20 years and who were staying with the patient since the onset of illness were included. The caregivers aged less than 20 years and those who were not blood related to the patients were excluded from the study. Irrespective of the blood relation, spouses were included in the study.
Each caregiver included was explained about the study and informed consent was taken. This was a case-control type of analytical, hospital-based study.
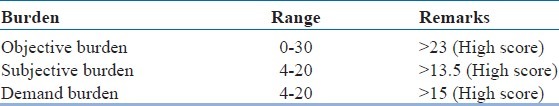
The caregivers were subjected to the Montgomery Borgatta Caregiver Burden Scale questionnaire which was applied as a self-administered questionnaire in English to those who could understand it, and to the rest of the participants it was administered by interview technique in which the interviewer translated the questionnaire into the vernacular language in which both the patient and the interviewer were well versed. This is a 14-item questionnaire with 5 item responses to each question; each response was given a score from 0 to 5. Of the 14 items in the questionnaire, a set of 6 questions measure OB, 4 questions measure SB and 4 questions measure DB. Table 1 gives the details of the scale and the reference scores.
Table 1.
Montgomery Borgatta caregiver burden scale
Statistical analysis
The obtained data were tabulated and analyzed with descriptive statistics, “Levene's” test for equality of variance and t test (SPSS software version 13.0).
RESULTS
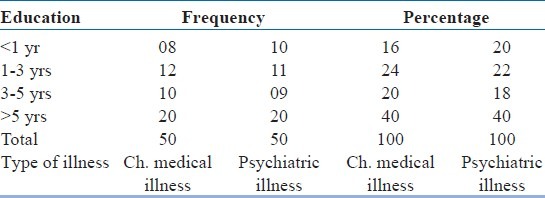
Of the 100 caregivers included in the study, 44 were males and 56 were females, with an age range of 20–60 years. Tables 2 and 3 show the distribution of sample in demographic variables such as literacy level and duration of care giving respectively. The two samples that is psychiatric illness and chronic medical illness have almost similar characteristics in the literacy rate and duration of care giving.
Table 2.
Literacy level of care givers
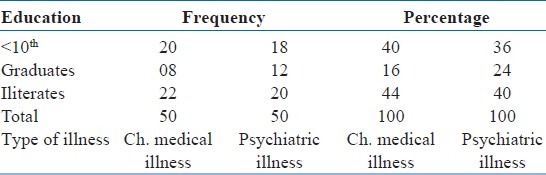
Table 3.
Duration of care giving
The Montgomery Borgatta Caregiver Burden Scale scores in the caregivers of psychiatric patients were significantly higher than that of chronic medical illness caregivers with a P value of less than 0.0001 (P<0.0001) in all the categories of caregiver burden, i.e. OB, SB and DB [Table 4 and Figure 1].
Table 4.
Comarision of various care giver burdens categories
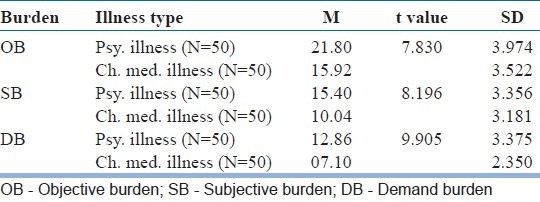
Figure 1.
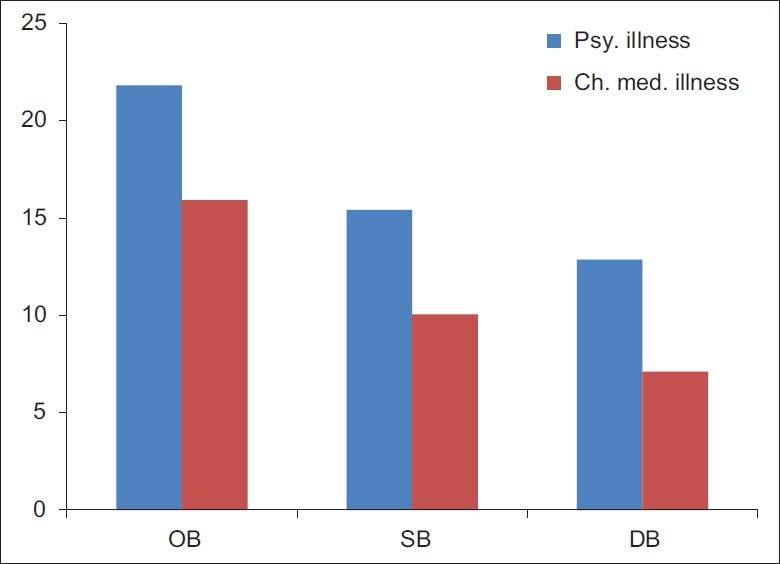
Psychiatric illness burden categories
Caregiver burden in psychiatric illness was observed to increase with the age of the caregiver except in DB which increased up to a certain age and then decreased. A similar pattern was observed in the caregivers of medical illnesses. The difference in caregiver burden among different age groups of psychiatric patient and chronic medical illness caregivers is also statistically significant with P value of less than 0.0001 (P<0.0001) [Table 5 and Figure 2].
Table 5.
Association of care giver burden with age of care giver
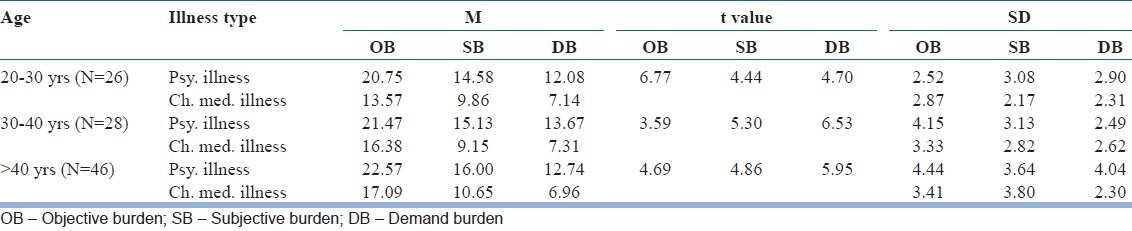
Figure 2.
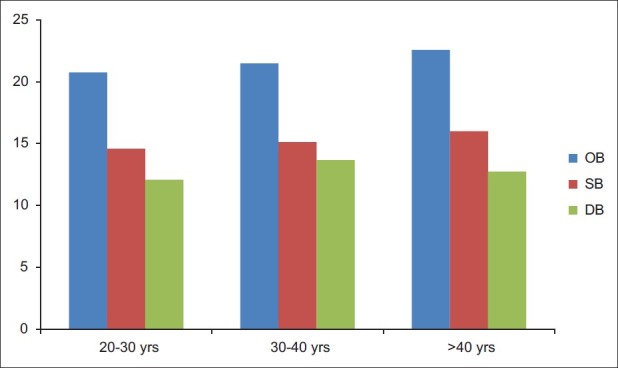
Psychiatric illness caregiver burden with age of caregiver
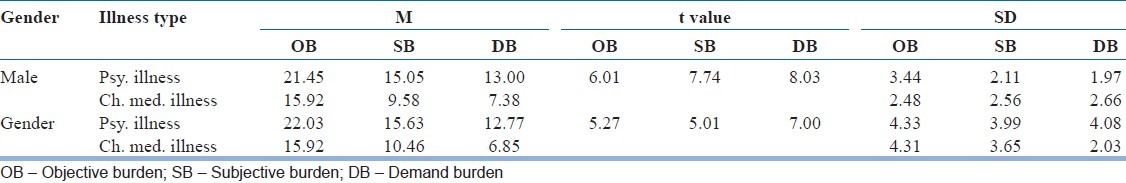
There was a minor caregiver burden variation with the gender of caregiver, with the burden being higher among females (n=44) for SB and OB and among males for DB (n=56). The difference observed is not statistically significant with P=0.4694 for OB, P=0.3851 for SB and P=0.7319 for DB [Table 6].
Table 6.
Association of care giver burden with gender
The caregiver burden in objective domain for psychiatric illness patients was observed to increase with the duration of care-giving till a certain period and then decreased. The difference in caregiver burden for various duration categories among psychiatric illness and chronic medical illness is statistically significant with P value less than 0.0001 (P<0.0001) [Table 7 and Figure 3].
Table 7.
Association of care giver burden with duration of illness
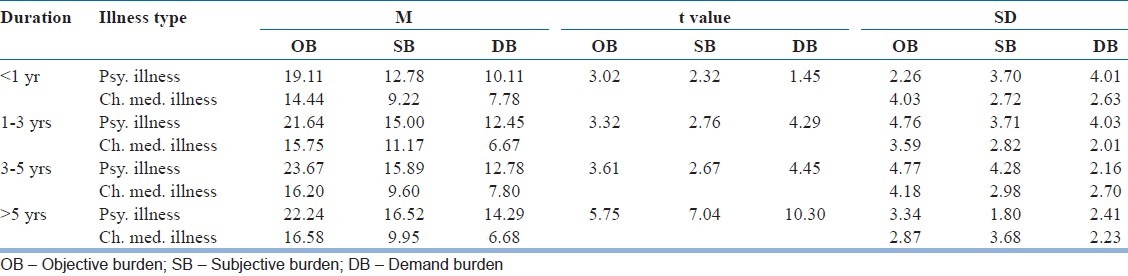
Figure 3.
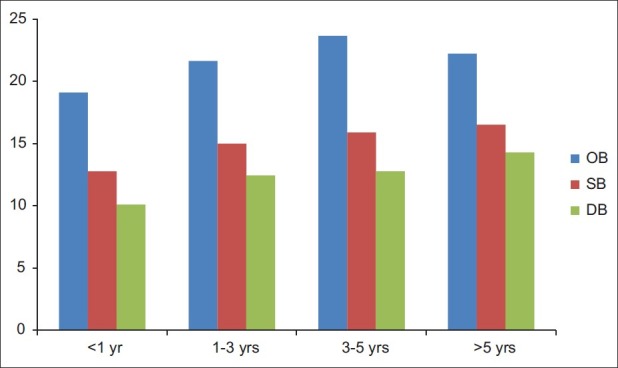
Psychiatric illness with duration
DISCUSSION
Our analysis shows that caregiver burden in our population is less as the OB which measures the disruption of the caregiver's life and the DB which measures the extent to which the caregiver feels care responsibilities are overly demanding do not cross the reference high value in the given scale, whereas SB which measures the emotional impact of caregiving responsibilities on a caregiver is on the higher side. A study conducted in 2004 by Erie County Department of Senior Service Caregiver Resource Centre[5] showed very high values of burden than those in this study. These observations can be explained by the presence of intimate family relations and social support in the Indian culture.
The results of this study comparing caregiver burden for caregivers of psychiatric illness patients and chronic medical illness patients are in agreement with those of other similar studies[1,3,6,7] and show more caregiver burden for caregivers of psychiatric illness patients. These observations may be due to the varied nature of psychiatric illness and the bizarre and inappropriate behavior of the psychiatrically ill, as these factors disrupt the relation between the caregiver and the patient. In spite of the adequate care, affection and support given by the caregiver, the nature of illness may prevent the patient from understanding the caregiver. Moreover, in some cases, the patient may even suspect the motives of the caregiver. These aspects of psychiatric illness further take a toll and worsen the burden on the caregiver. The varied mood swings, disturbed sleep pattern, aggressive and violent outbursts are some other aspects of illness that may further worsen the burden of caregiver. Lastly, the personal, social and occupational deterioration in the patient's life may reflect negatively on the burden experienced by the caregiver. Surprisingly, the level of burden did not correlate with the gender of caregiver, but had enough variability with the age of caregiver and duration of caregiving. In this study, the results show that caregiver burden in objective and subjective domains increases with increase in age of the caregiver. The ability of the caregiver to cope up with the physical and mental stress starts diminishing with increase in age due to added responsibilities of the caregivers related to their career, family and their own health, whereas the DB increases to a certain age and then decreases as the caregiver understands the disease process better after a certain age and is better adapted to the demands of the patient and his/her illness.
This study shows that there is only little difference in caregiver burden among female and male caregivers, with the OB and SB being higher in females while the DB is slightly higher in males, but these observations are not statistically significant. The caregiver burden in terms of OB was observed to increase with the duration of caregiving up to a certain extent but subsequently it decreased as the caregivers became less sensitive and began to modify their lifestyle. The SB which mainly measures the emotional impact on caregivers increased with the duration of illness, and DB also showed a similar pattern of increase with the duration of illness.
Limitations
The relationship of the caregiver to the patient was not considered in the study. The sample did not include dementia in which the caregiver burden is very high. As all people in the sample were not educated and there was no rating scale measuring caregiver burden in vernacular language, the scale had to be translated into local language, which can be a confounding factor.
CONCLUSION
The caregiver burden in families of psychiatric clients is statistically higher than that of caregivers of other medical illnesses. The caregiver burden increases with the duration of illness as well as with the age of caregivers. The caregiver burden in our population was less as the OB and DB did not cross the reference higher value in the given scale, whereas the emotional impact measured by SB was on the higher side.
The various means to reduce OB are to improve home care, adult day care, routine friendly visits and use of assistive equipment. SB can be reduced by professional counselling and by the assistance of support groups, while DB can be lowered by professional counselling and educating more about the disease.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Krupnik Y, Pilling S, Killaspy H, Dalton J. A study of family contact with clients and staff of community mental health teams. Psychiatric Bull. 2005;29:174–6. [Google Scholar]
- 2.Muscroft J, Bowl R. The impact of depression on caregivers and other family members: Implications for professional support. Couns Psychol Q. 2000;13:117–34. [Google Scholar]
- 3.Karlikay G, Yukse G, Varlibas F, Tireli H. Caregiver Burden In Dementia: A Study In The Turkish Population. Internet J Neurol. 2005;4:2. [Google Scholar]
- 4.Caregiver burden and psychotic patients’ perception of social support in a Nigerian setting by Ohaeri JU, Nigeria: University of Ibadan; Social Psychiatry and Psychiatric Epidemiology. 36:86–93. doi: 10.1007/s001270050294. [DOI] [PubMed] [Google Scholar]
- 5. Erie County Department OF University Health and Nutrition Letter: A case presentation by Miriam R. Callahan, Lisa M. Rood March 2004.
- 6.Chou KR, Chu H, Tseng CL, Lu RB. The measurement of caregiver burden. J Med Sci. 2003;23:73–82. [Google Scholar]
- 7.Ganguly KK, CHadda RK, Singh TB. Caregiver Burden and Coping in Schizophrenia and Bipolar Disorder. The American Journal of Psychiatry. 2010 Apr;161(5):850–856. [Google Scholar]


