Abstract
Background:
We sought to determine the prevalence of and clinical variables associated with learned helplessness, a psychologic state characterized by reduced motivation, difficulty in determining causality, and depression, in family members of patients admitted to ICUs.
Methods:
We conducted an observational survey study of a prospectively defined cohort of family members, spouses, and partners of patients admitted to surgical, medical, and trauma ICUs at a large academic medical center. Two validated instruments, the Learned Helplessness Scale and the Perceived Stress Scale, were used, and self-report of patient clinical characteristics and subject demographics were collected.
Results:
Four hundred ninety-nine family members were assessed. Of these, 238 of 460 (51.7%) had responses consistent with a significant degree of learned helplessness. Among surrogate decision-makers, this proportion was 50% (92 of 184). Characteristics associated with significant learned helplessness included grade or high school education (OR, 3.27; 95% CI, 1.29-8.27; P = .01) and Perceived Stress Scale score > 18 (OR, 4.15; 95% CI, 2.65-6.50; P < .001). The presence of a patient advance directive or do not resuscitate (DNR) order was associated with reduced odds of significant learned helplessness (OR, 0.56; 95% CI, 0.32-0.98; P = .05).
Conclusions:
The majority of family members of patients in the ICU experience significant learned helplessness. Risk factors for learned helplessness include lower educational levels, absence of an advance directive or DNR order, and higher stress levels among family members. Significant learned helplessness in family members may have negative implications in the collaborative decision-making process.
ICU admissions are associated with significant patient morbidity and mortality. Patients’ family members experience substantial stress,1‐3 high rates of anxiety,3‐8 depression,3,4,6‐8 and posttraumatic stress symptoms.4,8 This emotional burden is concerning, considering that, for approximately 95% of the critically ill, these individuals are patients’ surrogate decision-makers.9 Prior studies have found that up to 78% of surrogate decision-makers wished to limit or eliminate their role in medical decision-making.10‐12 Given the crucial role of the surrogate decision-maker in the ICU, it is important to delineate potential reasons for reluctance to participate in the collaborative decision-making process.
Helplessness is a consequence of experiencing uncontrollable events. Learning that outcomes are uncontrollable leads to three main deficits: reduced motivation, difficulty in recognizing the relationship between actions and outcomes, and depression.13‐16 The resultant psychologic state is termed “learned helplessness.”16 Learned helplessness has been described in numerous clinical populations, including individuals with drug dependence17 or chronic illness.18‐22 It is associated and interwoven with depression23 and worsening physical health.18,19,22,24,25 We hypothesized that family members of the critically ill are at risk of the development of learned helplessness as a result of the stressful, uncontrollable experiences encountered in the ICU.
The prevalence of learned helplessness among families of the critically ill and its association with clinical variables is unknown. To our knowledge, we are the first to assess the prevalence of learned helplessness and to evaluate these characteristics using validated measures and a questionnaire in family members of patients admitted to medical, surgical, and trauma ICUs.
Materials and Methods
Environment
We conducted a single-center observational study of a prospectively defined cohort of family members, including spouses and partners, of critically ill patients admitted to one of the eight ICUs at the University of Maryland Medical Center between February 26, 2010, and February 11, 2011. These consisted of medical (29 beds), surgical (19 beds), cardiac surgical (19 beds), complex cardiology (15 beds), neurologic (12 beds), and trauma (30 beds) ICUs. The University of Maryland Medical Center is an urban 705-bed teaching hospital. The institutional review board of the University of Maryland Baltimore approved this study with a waiver of consent (HP-00044462).
Patient Selection
Subjects were approached by study investigators in ICU common areas. Investigators described the purpose of the study, explained that participation did not affect their loved ones’ care, and made clear that the study was anonymous for both respondents and their ill family members. All members of the family were included, consonant with prior studies.6,10,11,26 Family members were provided a Research Information Form and a self-administered survey. The survey consisted of the Learned Helplessness Scale, the Perceived Stress Scale, demographic questions, questions regarding the patient’s clinical characteristics, and respondents’ opinion of the quality of physician communication during this admission. The Learned Helplessness Scale is a self-administered 20-item measure of learned helplessness ideation using a four-point Likert scale. Higher scores reflect a greater degree of learned helplessness, with scores ranging from 20 to 80. The internal consistency of the Learned Helplessness Scale has been widely validated, including in healthy populations (α = 0.8521 and α = 0.9227), in individuals with drug dependence (α = 0.90),17 and in patients with chronically ill oncology (α = 0.83), hemodialysis (α = 0.92), and spinal cord injury (α = 0.94).21 The 10-item Perceived Stress Scale possesses high construct validity and reliability for measuring perceived stress across age, sex, socioeconomic status (SES), and race/ethnic group, as well as other demographic characteristics (Cronbach α = 0.85).28,29 Clinical characteristics were assessed by subject self-report. Median household income and percentage below poverty line by zone improvement plan (ZIP) code were assessed by self-reported ZIP code and the US census data.30
Analytic Approach
Our primary outcome was learned helplessness. We defined a score > 40 as consistent with a significant degree of learned helplessness. Scores > 40 correlate with subjects who at least “somewhat agree” with a majority of the statements of the Learned Helplessness Scale21,31 and are associated with behavioral, cognitive, and affective deficits.31 Learned Helplessness Scale scores > 40 correlate with scores in individuals with drug dependence17,32 and chronic illness.21,22 The Perceived Stress Scale was used to measure stress as a continuous variable, with a score > 18 correlating with subject responses of at least “sometimes” agreeing with a majority of statements indicating a high degree of perceived stress.28
Survey completion was defined by a ≥ 95% response rate (19 of 20) on the Learned Helplessness Scale and a ≥ 90% response rate (nine of 10) on the Perceived Stress Scale. Single imputation was used to replace each scale’s missing value using the predicted value from the regression model constructed using observed values. Surveys with response rates lower than those stated were excluded from the analysis. The distribution of Learned Helplessness Scale scores is described. Characteristics in subjects by score were presented as mean values with SDs and were compared using two-sample t tests for continuous variables and comparisons of proportions for categorical variables. A Pearson product-moment correlation coefficient was assessed between the variables of the Learned Helplessness Scale score and the Perceived Stress Scale score. In selecting potential confounders for the multivariable logistic regression, we included variables meeting a significance test of .20 in univariate testing. An exploratory logistic regression model containing all variables was also performed.
Analyses were performed using SAS, version 9.1.3 (SAS Institute, Inc). We applied the traditional definition of P ≤ .05 for statistical significance.
Results
Four hundred ninety-nine respondents were recruited from all ICUs: trauma, 29.5% (147 of 499); medical, 23.9% (119 of 499); surgical, 20.2% (101 of 499); cardiothoracic, 10.0% (50 of 499); neurologic, 8.0% (40 of 499); and cardiac, 7.8% (39 of 499). Survey completion rates for the Learned Helplessness Scale and the Perceived Stress Scale were 92.2% (460 of 499) and 97.6% (487 of 499), respectively. Respondents completing both scales were included in the complete analysis (n = 457). High reliability for both instruments was found in this population (Learned Helplessness Scale, Cronbach α = 0.84; Perceived Stress Scale, Cronbach α = 0.84).
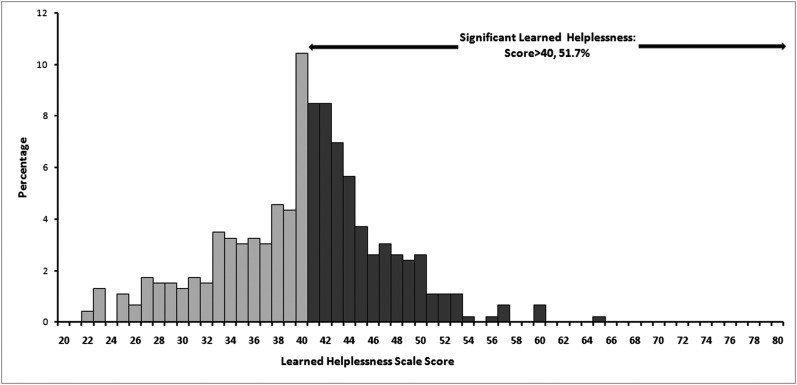
The mean (± SD) Learned Helplessness Scale score was 40.0 ± 7.2, with a similar median of 41.0 (interquartile range, 35-44). The distribution of scores is shown in Figure 1. Among subjects, 238 of 460 (51.7%) had scores consistent with significant learned helplessness (> 40). Respondents with significant Learned Helplessness Scale scores had lower educational levels and higher Perceived Stress Scale scores (26.2% vs 63.1%, P < .001), and were less likely to have a loved one with an advance directive or a do not resuscitate (DNR) order (33.2% vs 24.3%, P = .05) (Table 1). In univariate analysis, no difference in Learned Helplessness Scale score based on age, sex, race, familial relationship, medical decision-making capacity, ICU length of stay, previous ICU admission, median household income or proportion below poverty line in ZIP code of residence, or perception of quality of physician communication was found. Among surrogate decision-makers, 92 of 184 (50%) had Learned Helplessness Scale scores > 40. A sensitivity analysis using Markov Chain Monte Carlo methodology (SAS Proc MI; SAS Institute, Inc) and a comparison of complete and imputed Learned Helplessness Scale and Perceived Stress Scale scores found our results robust.
Figure 1.
Distribution of Learned Helplessness Scale scores.
Table 1.
—Subject Characteristics and Association With LHS Score > 40
| Characteristic | LHS Score ≤ 40 | LHS Score > 40 | P Value |
| Age, y | 46.7 ± 15.3 | 48.6 ± 15.4 | .19 |
| Male sex | 76 of 222 (34.2) | 70 of 238 (29.4) | .26 |
| Relationship to patients | .21 | ||
| Child | 52 of 222 (23.4) | 56 of 236 (23.7) | |
| Other relative | 71 of 222 (32.0) | 56 of 236 (23.7) | |
| Spouse/partner | 35 of 222 (15.8) | 49 of 236 (20.8) | |
| Parent | 35 of 222 (15.8) | 34 of 236 (14.4) | |
| Sibling | 29 of 222 (13.1) | 41 of 236 (17.4) | |
| Surrogate decision-maker | 92 of 222 (41.4) | 92 of 236 (39.0) | .59 |
| Presence of advance directive or DNR order | 66 of 199 (33.2) | 50 of 206 (24.3) | .05 |
| Current ICU length of stay, d | 7.2 ± 15.6 | 5.7 ± 7.4 | .36 |
| > 3 d | 112 of 218 (51.4) | 101 of 232 (43.5) | .10 |
| ICU type | .95 | ||
| Trauma | 67 of 222 (30.2) | 73 of 236 (30.9) | |
| Medical | 56 of 222 (25.2) | 53 of 236 (22.5) | |
| Surgical | 46 of 222 (20.7) | 48 of 236 (20.3) | |
| Cardiac surgical | 21 of 222 (9.5) | 25 of 236 (10.6) | |
| Neurologic | 19 of 222 (8.6) | 19 of 236 (8.1) | |
| Cardiac | 13 of 222 (5.9) | 18 of 236 (7.6) | |
| History of previous patient ICU admission | 77 of 215 (35.8) | 88 of 228 (38.6) | .54 |
| Race | .59 | ||
| White | 142 of 217 (65.4) | 146 of 234 (62.4) | |
| Black | 64 of 217 (29.5) | 71 of 234 (30.3) | |
| Other | 11 of 217 (5.1) | 17 of 234 (7.3) | |
| Median household income, $ | 47,901.7 ± 11,288.6 | 48,315.3 ± 11,697.4 | .70 |
| Below poverty line, % | 10.2 ± 8.6 | 11.3 ± 9.1 | .44 |
| ≥ US average (12.4%) | 156 of 210 (74.3) | 152 of 224 (67.9) | .14 |
| Educational level | < .001 | ||
| Grade school/high school | 79 of 222 (35.6) | 138 of 238 (58.0) | |
| College/university | 116 of 222 (52.3) | 89 of 238 (37.4) | |
| Advanced degree | 27 of 222 (12.2) | 11 of 238 (4.6) | |
| Did doctors explain things well? | .55 | ||
| Strongly agree | 101 of 213 (47.4) | 97 of 229 (42.4) | |
| Agree | 97 of 213 (45.5) | 113 of 229 (49.3) | |
| Disagree or strongly disagree | 15 of 213 (7.0) | 19 of 229 (8.3) | |
| Perceived Stress Scale score | 14.4 ± 6.7 | 20.3 ± 6.4 | < .001 |
| > 18 | 58 of 221 (26.2) | 149 of 236 (63.1) | < .001 |
Data are presented as mean ± SD or No. (%).DNR = do not resuscitate; LHS = Learned Helplessness Scale.
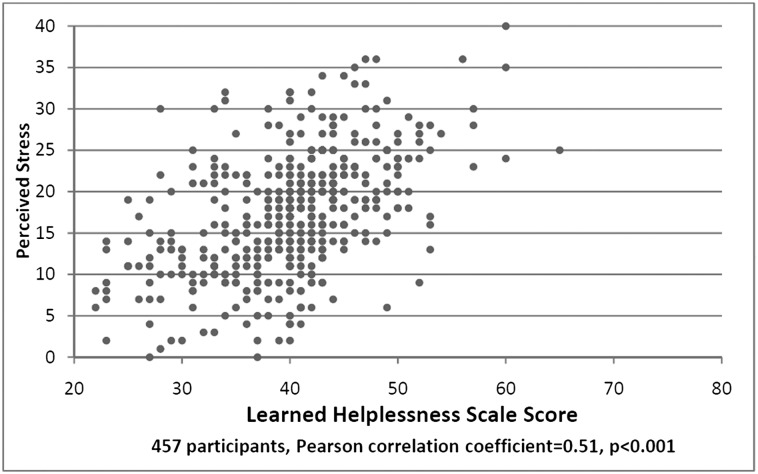
The Pearson correlation coefficient between the Learned Helplessness Scale and Perceived Stress Scale scores among subjects was 0.51 (P < .001) (Fig 2). In the multivariable model including covariates meeting prespecified significance, the presence of advance directives, ICU length of stay, and family member educational level and stress level were included in the model (Table 2). Patient ICU length of stay of ≤ 3 days was associated with an OR of 1.78 (95% CI, 1.14-2.78; P = .01) for significant learned helplessness. Family members with grade or high school education were at higher risk of learned helplessness (OR, 3.27; 95% CI, 1.29-8.27; P = .01). A Perceived Stress Scale score > 18 was also associated with learned helplessness (OR, 4.15; 95% CI, 2.65-6.50; P < .001). In this model, the presence of an advance directive or DNR order was associated with reduced odds of significant learned helplessness (OR, 0.64) but did not meet traditional definitions of significance (95% CI, 0.39-1.07; P = .09), although it was significant and consistent in point estimate in the complete multivariable model (OR, 0.56; 95% CI, 0.32-0.98; P = .05).
Figure 2.
Learned Helplessness Scale vs Perceived Stress Scale scores.
Table 2.
—Risk Factors for Learned Helplessness: Multivariable Model
| Risk Factor | OR (95% CI) | P Value |
| Current ICU length of stay | ||
| ≤ 3 d | 1.78 (1.14-2.78) | .01 |
| Education level | ||
| Grade school/high school | 3.27 (1.29-8.27) | .01 |
| College/university | 2.01 (0.79-5.08) | .14 |
| Advanced degree | 1.00 (reference group) | … |
| Stress levels | < .001 | |
| > 18 | 4.15 (2.65-6.50) | |
| ≤ 18 | 1.00 (reference group) |
Discussion
We found a high prevalence of learned helplessness in family members of patients admitted to ICUs, with the majority of subjects having significant Learned Helplessness Scale scores. Lower educational levels, the absence of an advance directive or DNR order, and high Perceived Stress Scale scores were associated with learned helplessness. In the multivariable model, lower educational levels, shorter length of stay, and high Perceived Stress Scale scores were associated with learned helplessness. To our knowledge, this is the first study to assess the prevalence of and risk factors for learned helplessness in family members of critically ill patients.
The levels of learned helplessness we found in this population are substantial. Providing context, the mean Learned Helplessness Scale score of ICU family members is higher than that of patients with spinal cord injury (40.0 ± 7.2 vs 36.9 ± 5.10)21 and is similar to alcoholics enrolling in a 12-step program (40.81 ± 9.34)32 and unemployed patients with multiple sclerosis (40.7 ± 10.6).22 This level is only slightly lower than that of patients receiving hemodialysis (41.9 ± 9.71), patients receiving cancer treatment (44.5 ± 6.02),21 and individuals with cocaine dependence (45.97 ± 9.68).17 Of the surrogate decision-makers studied, 50% suffered significant learned helplessness. Learned helplessness leads individuals to reason that outcomes are independent of their actions, resulting in decreased participation and disengagement from the collaborative decision-making process, and may lead to defensive behaviors such as avoidance and withdrawal.13‐17,33 The development of learned helplessness is a potential mechanism for the reluctance of the majority of surrogate decision-makers to generate crucial medical decisions.10‐12
Our findings are consistent with prior studies demonstrating that family members involved in decision making often report feeling overwhelmed or burdened.34,35 A review of 40 studies found that a sizeable proportion of surrogates experience significant emotional burden persisting years after the hospitalization.36 Consistently, a high prevalence of stress, anxiety, depression, and posttraumatic stress are found in this population.1‐6,8 Significant Perceived Stress Scale scores correlate with learned helplessness, as evidenced by the univariate and multivariable analyses and the Pearson coefficient.
Family members of the critically ill were more likely to have significant learned helplessness if an advance directive or DNR order was absent. In previous studies, the presence of an advance directive was associated with lowered emotional burden34,37 and stress37,38 among family members, while increasing the likelihood that patients received care concordant with their preferences.39 Family members reported less stressful end-of-life decisions when their loved one’s preferences were known.40,41 Potential reasons for our finding include a reduction in decision-making pressure in the background of learned helplessness, as well as the clear wishes of their loved one providing a source of empowerment.
Large variations exist in end-of-life care and expenditure in the ICU. Prior research has focused on patient,42 practice,43 and organizational44 characteristics. Less attention has been directed to delineating the impact of the surrogate decision-maker on end-of-life care. Many of these studies are qualitative and/or limited in sample size.40,45,46 The lack of a systematic approach has been noted.47 Randomized studies attempting to improve end-of-life care and the experience of surrogates have had divergent results. In France, in one multicenter study, provision of leaflets did not change family members’ satisfaction or reduce their emotional distress,48 whereas another study, of 126 subjects, found that a brochure combined with family conferences reduced posttraumatic stress and depression in family members.49 A larger multicenter American study (N = 2,318)50 assessed a multicomponent intervention providing physician and administrator education, evaluation of family feedback, and the creation of system supports. No difference was found in family member satisfaction, ICU length of stay, or time to ventilator withdrawal. Although the study’s low response rates may have limited statistical power, these low rates may also point to disengagement of the family members from the study, a symptom of learned helplessness. Interventions designed to improve physician performance without appropriately addressing the psychologic state of family members will be unlikely to enhance the collaborative decision-making process. Clearly, further study is needed to identify the cognitive mechanisms behind family member maladaptive behaviors and to develop interventions to help alleviate them.
Our finding of an inverse association between educational level and learned helplessness is concordant with prior findings that family members with lower educational levels suffer higher rates of stress2 and anxiety5 when their loved ones are admitted to the ICU. Educational level is a component of SES, along with income and occupation, and may be used to reflect overall SES.51 Our findings, then, may suggest that lower SES is associated with increased risk of learned helplessness. However, the lack of association with median income and proportion of those living in poverty, as measured by respondents’ ZIP codes, and the lack of association with race suggest that educational status’ association with learned helplessness may potentially be independent of SES. This finding regarding race is consistent with research showing that the relative emotional burden of decision making extends across racial boundaries.45
Several limitations should be considered. We conducted a convenience sample recruited by study staff from ICU common areas and, as such, it is subject to recruiting bias. Data suggest that family members responding to ICU surveys are more satisfied with the care their family member receives than are nonrespondents. Subjects were more highly educated than the general US population.30 Because learned helplessness is associated with lower educational levels, we likely underestimated the prevalence of learned helplessness in family members, making our findings more striking. As with all survey studies, our results are subject to participant reporting and recall bias. Although this study was conducted at a single academic medical center, the sample size and the consistency of the data derived from family members of ICU patients across medical, surgical, neurologic, cardiac, and trauma ICUs suggest that these findings may be more generalizable than other single-center studies.
Our findings provide a potential mechanism for surrogates’ reluctance to participate in decision making, and a potential cognitive barrier to collaboration between medical caregivers and families that may negatively impact the decision-making process. However, this study did not assess the relationship of learned helplessness with the attitudes of surrogates regarding decision-making; nor did it evaluate the relationship between learned helplessness and decision making. Because we preserved patient confidentiality to maximize recruitment and minimize selection bias, we did not link patients to their corresponding family member study participants. Therefore, we are unable to provide an in-depth analysis of the impact of patients’ characteristics on the development of learned helplessness. The above are crucial next steps in establishing the full impact of learned helplessness in the ICU.
Strategies for therapeutic intervention are communication-centric. In learned helplessness, caregivers must adjust family members’ expectations of outcomes and change their attributions for failures.13 This may be particularly salient, because family members of ICU patients often have expectations that are unrealistic52 or discordant with physicians’ estimations.53 Providing alternative explanations to modify the attribution of surrogates, that poor outcomes result from their decisions, may help reduce or eliminate learned helplessness.15 Targeted behavioral therapy15 may also lessen the symptoms of concomitant depression. Members of the multidisciplinary care team could be trained in recognizing and addressing learned helplessness in family members, potentially reducing their morbidity and improving the decision-making process.
Conclusions
In summation, the majority of family members, spouses, and partners of ICU patients have significant learned helplessness. Risk factors for learned helplessness include lower educational levels, the absence of a patient’s advance directive or DNR order, and higher levels of stress among family members. These findings suggest a mechanism for the reluctance of ICU surrogate decision-makers to participate in the collaborative decision-making process.
Acknowledgments
Author contributions: Dr Sullivan is the guarantor of the manuscript and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Dr Sullivan: contributed to the concept and design of the study; collection and assembly of data; analysis and interpretation of data; provision of study materials or patients; administrative, technical, or logistic support; drafting of the article; and final approval of the article.
Dr Liu: contributed to the concept and design of the study; collection and assembly of data; analysis and interpretation of data; statistical expertise; administrative, technical, or logistic support; drafting of the article; and final approval of the article.
Dr Corwin: contributed to the concept and design of the study; provision of study materials or patients; collection and assembly of data; analysis and interpretation of data; administrative, technical, or logistic support; and final approval of the article.
Dr Verceles: contributed to the concept and design of the study, analysis and interpretation of data, and final approval of the article.
Dr McCurdy: contributed to the concept and design of the study, analysis and interpretation of data, and final approval of the article.
Dr Pate: contributed to the concept and design of the study; analysis and interpretation of data; administrative, technical, or logistic support; and final approval of the article.
Ms Davis: contributed to the concept and design of the study; provision of study materials or patients; collection and assembly of data; analysis and interpretation of data; administrative, technical, or logistic support; and final approval of the article.
Dr Netzer: contributed to the concept and design of the study; collection and assembly of data; analysis and interpretation of data; statistical expertise; administrative, technical, or logistic support; drafting of the article; and final approval of the article.
Financial/nonfinancial disclosures: The authors have reported to CHEST that no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
Role of sponsors: The sponsors had no role in the design of the study, the collection and analysis of the data, or in the preparation of the manuscript.
Other contributions: The authors thank Frances M. Ward, PhD, RN, for her assistance and for use of the Learned Helplessness Scale. Helpful criticism was received from Theodore J. Iwashyna, MD, PhD. We are grateful for the participation of the ICU directors in this study: Carl Shanholtz, MD (medical); William Chiu, MD, and Matthew Lissauer, MD (surgical); Shawn Robinson, MD (cardiac); Daniel Hess, MD (cardiac surgical); David Shreibman, MD, and Kevin Sheth, MD (neurologic); Deborah Stein, MD, Nader Habashi, MD, and H. Neal Reynolds, MD (trauma); and the nursing staffs of these ICUs. This study was performed at the University of Maryland Medical Center.
Abbreviations
- DNR
do not resuscitate
- SES
socioeconomic status
- ZIP
zone improvement plan
Footnotes
Funding/Support: This work was supported by the National Institutes of Health [5K12RR023250-04] to Dr Netzer.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians. See online for more details.
References
- 1.Azoulay E, Pochard F, Kentish-Barnes N, et al. ; FAMIREA Study Group Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med. 2005;171(9):987-994 [DOI] [PubMed] [Google Scholar]
- 2.Chui WY, Chan SW. Stress and coping of Hong Kong Chinese family members during a critical illness. J Clin Nurs. 2007;16(2):372-381 [DOI] [PubMed] [Google Scholar]
- 3.Fumis RR, Deheinzelin D. Family members of critically ill cancer patients: assessing the symptoms of anxiety and depression. Intensive Care Med. 2009;35(5):899-902 [DOI] [PubMed] [Google Scholar]
- 4.Anderson WG, Arnold RM, Angus DC, Bryce CL. Posttraumatic stress and complicated grief in family members of patients in the intensive care unit. J Gen Intern Med. 2008;23(11):1871-1876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Delva D, Vanoost S, Bijttebier P, Lauwers P, Wilmer A. Needs and feelings of anxiety of relatives of patients hospitalized in intensive care units: implications for social work. Soc Work Health Care. 2002;35(4):21-40 [DOI] [PubMed] [Google Scholar]
- 6.Pochard F, Azoulay E, Chevret S, et al. ; French FAMIREA Group Symptoms of anxiety and depression in family members of intensive care unit patients: ethical hypothesis regarding decision-making capacity. Crit Care Med. 2001;29(10):1893-1897 [DOI] [PubMed] [Google Scholar]
- 7.Pochard F, Darmon M, Fassier T, et al. ; French FAMIREA study group Symptoms of anxiety and depression in family members of intensive care unit patients before discharge or death. A prospective multicenter study. J Crit Care. 2005;20(1):90-96 [DOI] [PubMed] [Google Scholar]
- 8.Paparrigopoulos T, Melissaki A, Efthymiou A, et al. Short-term psychological impact on family members of intensive care unit patients. J Psychosom Res. 2006;61(5):719-722 [DOI] [PubMed] [Google Scholar]
- 9.Smedira NG, Evans BH, Grais LS, et al. Withholding and withdrawal of life support from the critically ill. N Engl J Med. 1990;322(5):309-315 [DOI] [PubMed] [Google Scholar]
- 10.Azoulay E, Pochard F, Chevret S, et al. ; FAMIREA Study Group Half the family members of intensive care unit patients do not want to share in the decision-making process: a study in 78 French intensive care units. Crit Care Med. 2004;32(9):1832-1838 [DOI] [PubMed] [Google Scholar]
- 11.Anderson WG, Arnold RM, Angus DC, Bryce CL. Passive decision-making preference is associated with anxiety and depression in relatives of patients in the intensive care unit. J Crit Care. 2009;24(2):249-254 [DOI] [PubMed] [Google Scholar]
- 12.Heyland DK, Cook DJ, Rocker GM, et al. Decision-making in the ICU: perspectives of the substitute decision-maker. Intensive Care Med. 2003;29(1):75-82 [DOI] [PubMed] [Google Scholar]
- 13.Garber J, Seligman MEP. Human Helplessness: Theory and Applications. New York, NY: Academic Press; 1980 [Google Scholar]
- 14.Maier SF, Seligman ME. Learned helplessness: theory and evidence. J Exp Psychol Gen. 1976;105(1):3-46 [Google Scholar]
- 15.Abramson LY, Seligman ME, Teasdale JD. Learned helplessness in humans: critique and reformulation. J Abnorm Psychol. 1978;87(1):49-74 [PubMed] [Google Scholar]
- 16.Seligman ME, Maier SF. Failure to escape traumatic shock. J Exp Psychol. 1967;74(1):1-9 [DOI] [PubMed] [Google Scholar]
- 17.Sterling RC, Gottheil E, Weinstein SP, Lundy A, Serota RD. Learned helplessness and cocaine dependence: an investigation. J Addict Dis. 1996;15(2):13-24 [DOI] [PubMed] [Google Scholar]
- 18.Smith TW, Peck JR, Ward JR. Helplessness and depression in rheumatoid arthritis. Health Psychol. 1990;9(4):377-389 [DOI] [PubMed] [Google Scholar]
- 19.Engle EW, Callahan LF, Pincus T, Hochberg MC. Learned helplessness in systemic lupus erythematosus: analysis using the Rheumatology Attitudes Index. Arthritis Rheum. 1990;33(2):281-286 [DOI] [PubMed] [Google Scholar]
- 20.Rydholm L, Pauling J. Contrasting feelings of helplessness in peritoneal and hemodialysis patients: a pilot study. ANNA J1991;18(2):183-186, 200 [PubMed] [Google Scholar]
- 21.Quinless FW, Nelson MA. Development of a measure of learned helplessness. Nurs Res. 1988;37(1):11-15 [PubMed] [Google Scholar]
- 22.McGuinness S. Learned helplessness in the multiple sclerosis population. J Neurosci Nurs1996;28(3):163-170 [DOI] [PubMed] [Google Scholar]
- 23.Seligman ME. Learned helplessness. Annu Rev Med. 1972;23(407-412 [DOI] [PubMed] [Google Scholar]
- 24.Peterson C, Seligman ME. Explanatory style and illness. J Pers. 1987;55(2):237-265 [DOI] [PubMed] [Google Scholar]
- 25.Peterson C, Seligman ME, Vaillant GE. Pessimistic explanatory style is a risk factor for physical illness: a thirty-five-year longitudinal study. J Pers Soc Psychol. 1988;55(1):23-27 [DOI] [PubMed] [Google Scholar]
- 26.Johnson SK, Bautista CA, Hong SY, Weissfeld L, White DB. An empirical study of surrogates’ preferred level of control over value-laden life support decisions in intensive care units. Am J Respir Crit Care Med. 2011;183(7):915-921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McDermott MA. The Relationship Between Learned Helplessness and Self-Care Agency in Adults as a Function of Gender and Age [PhD thesis]. New York, NY: New York University; 1989.
- 28.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385-396 [PubMed] [Google Scholar]
- 29.Cohen S. Spacapan S, Oskamp S. The social psychology of health. In: eds. Perceived Stress in a Probability Sample of the United StatesThousand Oaks, CA: Sage Publications, Inc; 1988;31-67 [Google Scholar]
- 30. 2000 Census of Population and Housing, Summary File 1 & 3. Washington, DC: US Census Bureau; 2002.
- 31.McKean KJ. Using multiple risk factors to assess the behavioral, cognitive, and affective effects of learned helplessness. J Psychol. 1994;128(2):177-183 [DOI] [PubMed] [Google Scholar]
- 32.Pellegrino PJ. Does Alcoholics Anonymous Participation Decrease Learned Helplessness and Increase Self-efficacy?. [dissertation]. Paper 113. Philadelphia, PA: Philadelphia College of Osteopathic Medicine;2009 [Google Scholar]
- 33.Zuroff DC. Learned helplessness in humans: an analysis of learning processes and the roles of individual and situational differences. J Pers Soc Psychol. 1980;39(1):130-146 [Google Scholar]
- 34.Jacobson JA, Francis LP, Battin MP, et al. Dialogue to action: lessons learned from some family members of deceased patients at an interactive program in seven Utah hospitals. J Clin Ethics. 1997;8(4):359-371 [PubMed] [Google Scholar]
- 35.Norton SA, Tilden VP, Tolle SW, Nelson CA, Eggman ST. Life support withdrawal: communication and conflict. Am J Crit Care. 2003;12(6):548-555 [PubMed] [Google Scholar]
- 36.Wendler D, Rid A. Systematic review: the effect on surrogates of making treatment decisions for others. Ann Intern Med. 2011;154(5):336-346 [DOI] [PubMed] [Google Scholar]
- 37.Tilden VP, Tolle SW, Nelson CA, Fields J. Family decision-making to withdraw life-sustaining treatments from hospitalized patients. Nurs Res. 2001;50(2):105-115 [DOI] [PubMed] [Google Scholar]
- 38.Davis BA, Burns J, Rezac D, et al. Family stress and advance directives: a comparative study. Journal of Hospice & Palliative Nursing. 2005;7(4):):219-227. [Google Scholar]
- 39.Silveira MJ, Kim SY, Langa KM. Advance directives and outcomes of surrogate decision making before death. N Engl J Med. 2010;362(13):1211-1218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vig EK, Starks H, Taylor JS, Hopley EK, Fryer-Edwards K. Surviving surrogate decision-making: what helps and hampers the experience of making medical decisions for others. J Gen Intern Med. 2007;22(9):1274-1279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Abbott KH, Sago JG, Breen CM, Abernethy AP, Tulsky JA. Families looking back: one year after discussion of withdrawal or withholding of life-sustaining support. Crit Care Med. 2001;29(1):197-201 [DOI] [PubMed] [Google Scholar]
- 42.Kelley AS, Ettner SL, Morrison RS, Du Q, Wenger NS, Sarkisian CA. Determinants of medical expenditures in the last 6 months of life. Ann Intern Med. 2011;154(4):235-242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Ann Intern Med. 2003;138(4):273-287 [DOI] [PubMed] [Google Scholar]
- 44.Lin CY, Farrell MH, Lave JR, Angus DC, Barnato AE. Organizational determinants of hospital end-of-life treatment intensity. Med Care. 2009;47(5):524-530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Braun UK, Beyth RJ, Ford ME, McCullough LB. Voices of African American, Caucasian, and Hispanic surrogates on the burdens of end-of-life decision making. J Gen Intern Med. 2008;23(3):267-274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Meeker MA. Family surrogate decision making at the end of life: seeing them through with care and respect. Qual Health Res. 2004;14(2):204-225 [DOI] [PubMed] [Google Scholar]
- 47.Rid A, Wendler D. Can we improve treatment decision-making for incapacitated patients?. Hastings Cent Rep. 2010;40(5):36-45 [DOI] [PubMed] [Google Scholar]
- 48.Azoulay E, Pochard F, Chevret S, et al. Impact of a family information leaflet on effectiveness of information provided to family members of intensive care unit patients: a multicenter, prospective, randomized, controlled trial. Am J Respir Crit Care Med. 2002;165(4):438-442 [DOI] [PubMed] [Google Scholar]
- 49.Lautrette A, Darmon M, Megarbane B, et al. A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med. 2007;356(5):469-478 [DOI] [PubMed] [Google Scholar]
- 50.Curtis JR, Nielsen EL, Treece PD, et al. Effect of a quality-improvement intervention on end-of-life care in the intensive care unit: a randomized trial. Am J Respir Crit Care Med. 2011;183(3):348-355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Winkleby MA, Jatulis DE, Frank E, Fortmann SP. Socioeconomic status and health: how education, income, and occupation contribute to risk factors for cardiovascular disease. Am J Public Health. 1992;82(6):816-820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Berge KH, Maiers DR, Schreiner DP, et al. Resource utilization and outcome in gravely ill intensive care unit patients with predicted in-hospital mortality rates of 95% or higher by APACHE III scores: the relationship with physician and family expectations. Mayo Clin Proc. 2005;80(2):166-173 [DOI] [PubMed] [Google Scholar]
- 53.Lee Char SJ, Evans LR, Malvar GL, White DB. A randomized trial of two methods to disclose prognosis to surrogate decision makers in intensive care units. Am J Respir Crit Care Med. 2010;182(7):905-909 [DOI] [PMC free article] [PubMed] [Google Scholar]