Abstract
We present a case of middle ear rhabdomyosarcoma with intracranial erosion and later presented with diffuse leptomeningeal spread. Such lesions are difficult to eradicate and have a poor prognosis
Keywords: Middle ear rhabdomyosarcoma, leptomeningeal spread
Rhabdomyosarcomas of the head and neck may spread by diffuse local invasion resulting in erosion of the base of skull with possible extension to the leptomeninges, brain and cranial nerves as well as invasion of the ventricular system with possible intradural extramedullary metastasis anywhere along the neuraxis. Meningeal spread of tumor is difficult to eradicate and has a poor prognosis. Patients with erosion of skull base have risk of seeding the meninges.[1,2]
A 3-year-old male child presented with left ear ache with hearing loss and left facial and abducens palsy for 4 months. There was no history of ear discharge, altered sensorium, ataxia or seizures. The examination revealed congested external auditory canal and VI and VII nerve palsy on the left side. The tympanic membrane could not be visualised. The HRCT temporal bone was suggestive of infiltrative lesion in left ear with bone destruction [Figure 1a]. The MRI brain showed a lesion in the petrous extending in the cerebellopontine angle and temporal fossa [Figure 1b–d]. The left mastoid exploration with debulking of the mass was done. There was infiltrative fleshy vascular tissue in aditus, attic, and antrum with gross destruction of the posterior canal wall. Partial decompression was achieved. The histopathology was suggestive of ‘embryonal rhabdomyosarcoma’ [Figure 2a–e].
Figure 1.
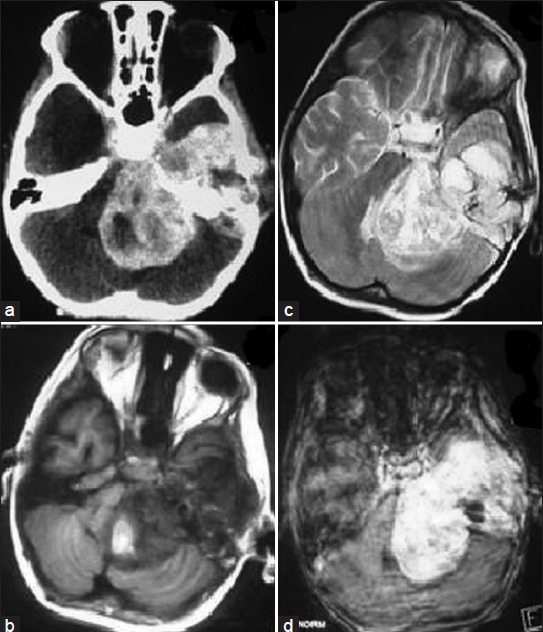
(a) Contrast CT showing well-defined petrous lesion extending into the posterior fossa and middle cranial fossa. (b) Axial T1-weighted image showing hypointense lesion pushing the brain stem to the right. (c) Axial T2-weighted image showing hyperintense lesion (d) Contrast MRI axial image showing good enhancement without any leptomeningeal spread
Figure 2.
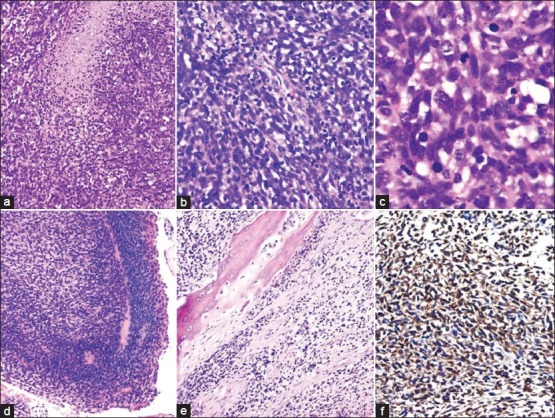
(a) Diffuse sheets of small, round to oval cells with high N/C ratio interspersed with areas of necrosis (H and E, × 200). (b) Small fascicles of spindle shaped cells were also seen scattered in between (H and E, × 200). (c) Higher magnification of closely packed cells with high N/C ratio. Many mitotic figures and apoptotic bodies are seen (H and E, × 1000). (d) Cam bium layer with clustering of neoplastic cells beneath the epit helial lining (H and E, ×200). (e) Tumor cells infiltrating and destroying the bone (H and E ×200). f) Tumor cells showing strong cytoplasmic positivity with desmin (immunoperoxidase, ×400)
Postoperatively, the patient had persistent altered sensorium with features of raised intracranial pressure. The computed tomography (CT) scan revealed hydrocephalus for which patient underwent VP shunt. The patient received chemotherapy (Ifosfamide, Vincristine, Actinomycin-D, Doxorubicin) along with 36 grays of radiation. After about 6 months of the primary surgery, the patient's neurological status deteriorated and features were suggestive of “locked in syndrome”, necessitating withholding further chemoradiation. His cranio-spinal MRI was suggestive of diffuse leptomeningeal spread with minimal lesion seen at the primary site [Figure 3a–c]. The child expired in 1 week.
Figure 3.
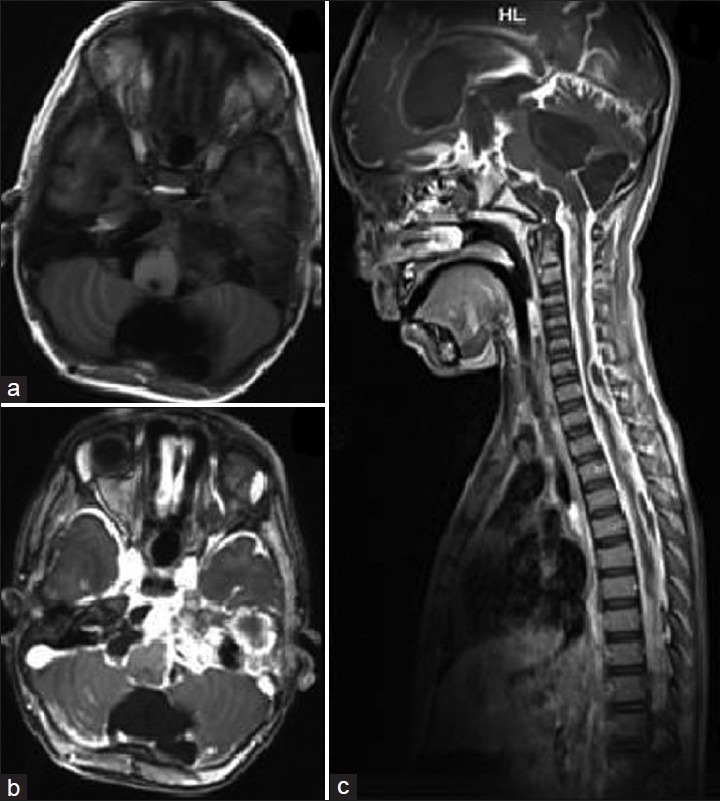
(a) T1-weighted axial MRI showing minimal lesion in petrous following surgical decompression and chemotherapy. (b) Contrast axial MRI showing enhancement of the leptomeninges. (c) Contrast sagittal MRI showing diffuse enhancement of the leptomeninges of the entire craniospinal axis. The enhancement is so diffuse that it appears like a T2 image
Secondary central nervous system (CNS) involvement in head and neck rhabdomyosarcoma is a known complication and is usually seen as leptomeningeal spread, though primary CNS involvement is rare.[3–5] Such spread is usually rapid and fatal. Cerebrospinal fluid (CSF) from lumbar puncture and radiological screening in cases of rhabdomyosarcomas, even when not in parameningeal location has been suggested. In parameningeal location, regular CSF examination for malignant cytology and craniospinal screening is of paramount importance.[4] Use of craniospinal irradiation and chemotherapeutic drugs that cross the blood brain barrier has been suggested in case of metastatic or parameningeal rhabdomyosarcomas, though the involvement of CNS may not be apparent.[4,5] Most of the chemotherapeutic drugs used in our patient have good CSF penetration. Despite all these drugs, the patient developed leptomeningeal metastases and had a poor outcome. This report highlights the spread of rhabdomyosarcomas through CSF pathways after intracranial extension thereby making cranio-spinal screening important. Besides, diffuse leptomeningeal spread is poorly controlled by chemotherapy and usually bears a poor prognosis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
References
- 1.Gerson JM, Jaffe N, Donaldson MH, Tefft M. Meningeal seeding from rhabdomyosarcoma of the head and neck with base of the skull invasion: Recognition of the clinical evolution and suggestions for management. Med Pediatr Oncol. 1978;5:137–44. doi: 10.1002/mpo.2950050120. [DOI] [PubMed] [Google Scholar]
- 2.Shellenberger TD, Sturgis EM. Sarcomas of the head and neck region. Curr Oncol Rep. 2009;11:135–42. doi: 10.1007/s11912-009-0020-8. [DOI] [PubMed] [Google Scholar]
- 3.Dropcho EJ, Allen JC. Primary intracranial rhabdomyosarcoma: Case report and review of the literature. J Neurooncol. 1987;5:139–50. doi: 10.1007/BF02571302. [DOI] [PubMed] [Google Scholar]
- 4.Arush MW, Kollender Y, Issakov J, Shalom RB, Arieh YB, Malkin L, et al. Unusual leptomeningeal dissemination in a child with extracranial metastatic alveolar rhabdomyosarcoma. Pediatr Hematol Oncol. 2009;26:473–8. doi: 10.3109/08880010902993218. [DOI] [PubMed] [Google Scholar]
- 5.Ahola DT, Provenzale JM, Longee DC. Metastatic rhabdomyosarcoma presenting as intracranial hemorrhage: Imaging findings. Eur J Radiol. 1998;26:241–3. doi: 10.1016/s0720-048x(97)00030-2. [DOI] [PubMed] [Google Scholar]


