Summary
Background
The aim of this paper is to present the physiotherapeutic program employed at the Rehabilitation Centre for the College of Physiotherapy in Wrocław, Poland and its effectiveness by demonstrating the increase in strength of knee joint extensor and flexor muscles of patients after anterior cruciate ligament (ACL) reconstruction.
Material/Methods
Thirty-seven males participated in the physiotherapeutic program from the first week up to 8 months postoperatively. Each patient underwent an individual therapeutic program. Endoscopic reconstruction of a completely ruptured ACL was performed using Mitek’s method (graft harvesting from flexor muscles). All patients previously underwent orthopedic and functional examinations, including measurements of the range of movement, knee and thigh circumference and strength of flexor and extensor muscles of the involved and uninvolved leg using a Biodex 3 System in both static and isokinetic modes.
Results
The outcome of the physiotherapeutic procedure, which is detailed in the paper, revealed a favorable effect of physiotherapy 6 months after ACL reconstruction. The observed 9% deficit in extensor muscle strength measured under isokinetic conditions of the involved knees compared with the uninvolved knees led us to conclude that the period of physiotherapy should be extended beyond 6 months for some patients.
Conclusions
1. Six months of physiotherapy following ACL reconstruction in males favorably affected muscle strength values of the involved and uninvolved knees under static and isokinetic conditions. 2. The application of individual loads during the sixth month of physiotherapy resulted in similar values of extensor and flexor muscle strength measured under static conditions, and flexor muscle strength measured under isokinetic conditions in involved and uninvolved knees.
Keywords: ACL, muscle torque, physiotherapy
Background
Physiotherapeutic procedures should restore locomotor fitness in patients after anterior cruciate ligament (ACL) reconstruction. Normal locomotion depends on, among other factors, ligamentocapsular structure stability, knee joint range of movement and an appropriate strength level of knee joint muscles, as well as on proprioception [1,2]. The aim of ACL reconstruction is to restore anatomical and biomechanical properties of this ligament, necessary to maintain anteroposterior and anteromedial knee joint stability. Woo et al. reported that selection of grafts and their placement in the bone tunnel affect the reconstruction result [3]. The tension and fixation of the graft, tunnel mobility and graft healing speed are crucial [3].
After reconstruction, the patients’ range of movement is temporarily limited and the strength of knee joint flexor muscles (sartorius, gracilis, semitendinosus, semimembranosus, biceps femoris, gastrocnemius) and extensor (quadriceps) muscles deteriorates [4]. It is assumed that on completion of the entire physiotherapeutic program, the muscle strength values should be returned to preoperative levels, both in static and dynamic conditions. One of the goals of physiotherapy after ACL reconstruction is to restore the antagonist strength ratio of knee joint muscle groups. When planning physiotherapeutic procedures, it is necessary to determine when and to what extent can muscle strength be safely restored. There are several popular rehabilitation programs for patients after ACL reconstruction [5–7]. These programs, apart from being based on common assumptions, differ in the selection of exercises, and the magnitude and time of load application after ACL reconstruction [8,9]. Physiotherapeutic procedures after ACL reconstruction should comprise several stages. The factors conditioning load selection to restore muscle strength after autologic ligament reconstruction include a minimal period following surgery, necessary for graft healing in the bone tunnel [10–12]. They also include a gradual process of ligament graft angiogenesis [13]. The use of growth factors may enhance and improve graft healing, stiffness and load-bearing ability [14]. Personal traits of the patients, particularly mentality, gender, age and level of physical activity, are important.
The aim of this paper is to present the physiotherapeutic program applied after ACL reconstruction at the Rehabilitation Centre for the College of Physiotherapy in Wrocław and the evaluation of its effectiveness, reflected by increased strength values of knee joint extensor and flexor muscles.
The tailored PT study protocol, developed by the first author, was implemented for many years at the Rehabilitation Centre of the College of Physiotherapy in Wrocław. A detailed and expanded version of this paper is part of the first author’s doctoral thesis [4].
Material and Methods
Patients
Thirty-seven males (see Table 1) participated in individual physiotherapeutic programs applied from the first week to up to 8 months after the primary endoscopic reconstruction of isolated ACL tear by Mitek’s method of JOHNSON & JOHNSON GATEWAY® company using the autografts of the patients’ own semimembranosus and gracilis muscles [15]. The grafts were prepared from flexor tendons of the operated knee joint. Graft stabilisation was performed by the Regidfix method. Twenty-one right and 16 left knee joints were operated on. Right- and left-sided lateralization was noted in 35 and 2 patients, respectively. The orthopedic surgeon qualified the patients for the first and for the subsequent stages of the physiotherapeutic procedure, and examined them after the physiotherapeutic program had finished. The orthopedist obtained case histories and performed the medical examination. This examination included Lachman’s test, anteroposterior dislocation test and evaluation of the stability of other knee structures, as well as the presence of pain and swelling compared to the uninvolved knee [16]. In the studied sample, during the entire study period of physiotherapeutic program implementation, the measurement of tibial translation, as related to the knee, did not exceed 5 mm. The patients gave their informed consent to participate in the study and the study was approved by the Bioethics Committee of the University of Physical Education in Wrocław. The patients participated in a 4-stage physiotherapeutic program at our centre. Each patient underwent an individual therapeutic program with a physiotherapist, on average 4 times a week for 2 hours each day. Additionally, the patients were instructed how to perform the exercises correctly at home and informed of possible hazards of ligament injuries. The outline of the physiotherapeutic program is presented in Table 2 detailed physiotherapeutic procedure which comprises the more detailed program is presented elsewhere [4].
Table 1.
Characteristics of patients.
| Characteristic | Unit | Mean ±SD | Min | Max |
|---|---|---|---|---|
| Age | year | 30.9±9.3 | 16 | 55 |
| Body mass | kg | 81.7±8.1 | 70 | 110 |
| Body height | cm | 178.3±5.8 | 169 | 195 |
Data sampled from 37 individuals.
Table 2.
Outline of the physiotherapeutic procedures.
| Stages and weeks after surgery | Programme of basic procedures | Special muscle-strengthening exercises |
|---|---|---|
| Stage I 1st–5th week |
Ice packs. After several days – local treatment. Passive exercises on a CPM splint with gradual increase in the range of movement of the involved joint. Mobilisation of the patellofemoral joint. Massage of the iliotibial band and the lateral head of the quadriceps. Gait learning and perfection using two crutches. Electrostimulation of the quadriceps and posterior muscles of the thigh. Proprioceptive exercises in a closed kinematic chain. Magnetic field. At the end of Stage I – learning to walk without crutches. |
Isometric tension of the quadriceps and flexor muscles of the involved knee joints and other large muscle groups. Isometric exercises with manually dosed resistance of muscle groups beyond the area of the operated knee joint, the uninvolved lower extremity, upper extremities and the trunk. Exercises (on MTD platform): gradually increasing load of the involved leg from 20 to 100% of the body weight. Restrictive two-legged squats on a stable surface. |
| Stage II 6th–12th week |
As above and additionally: Gradual increase in range of movement until a full extension and flexion of the knee joint is obtained. Gait perfection without crutches. Marching on a treadmill, on a flat surface. Initial speed ranged from 2.8 to 3.5 km/h. Desired speed range is from 5.5 to 6.5 km/h. The distance being covered was extended. Exercises on a cycloergometer at the frequency of 60 rpm, without resistance. During the subsequent week – for the first 5 minutes with power of 50 Watt and next, in 10-Watt increments, every 2 minutes. The total time was 10 minutes in increments up to 15 minutes. Every 2 weeks, the initial power value was increased by 5–10 Watt. Walking up and down stairs without crutches. Proprioceptive exercises with assistance on a soft surface: trampoline, mattress, exercise mat and other practice balance beams. Attention focused on preserving a correct Q angle. Marching with changing the inclination angle of the treadmill tape. |
Concentric exercises with gradually increased resistance for ischiotibial muscles of the operated leg. Concentric exercises with the physiotherapist’s resistance (this does not apply to the quadriceps of the involved knee joint) of muscle groups of the lower and upper extremities and the trunk. Exercises on a stepper with gradually increased resistance and gradually increased lower extremity range of movement. Squats with both and one leg on an unstable surface. Gradually increased squatting range. |
| Stage III 13th–20th week |
The same as during Stage I and additionally: During the 13th week – measurements of maximal extensor and flexor muscle strength of the operated and uninvolved knee joints on a Biodex 3 System, as the basis for training (see the next column). After obtaining 70% of muscle torque value for the operated legs, as related to unaffected legs, such exercises as running on a treadmill, on a soft surface were introduced, initially at low speed (trot). Next, running on a parquet and on a hard surface. Discipline-specific exercises, initially at low speed; later, the duration of exercises was prolonged and their intensity was gradually increased. Two-legged and next, one-legged jumps on a soft surface, gradually on platforms, then on a parquet and hard surface. Subsequently, the gravity centre shift was placed higher and the degree of difficulty was increased using the unstable surface. Once to twice a week, the exercises were followed by centrifugal massage. |
Isometric exercises with partial resistance of the involved knee joint extensor muscles on a Biodex 3 System. The exercises were started with 35% of the maximum torque recorded in the static test. The contraction lasted 5 seconds and was followed by a rest break within the next 5 seconds. The entire cycle was repeated until the patient was no longer able to bear the preset load displayed on the monitor or when the patient reported fatigue threshold or pain threshold. After adaptation to such a load (prolongation of exercise duration with a preset load and fewer errors in bearing the load equal to the value displayed on the monitor), a 40–50% load was applied of the maximum torque during subsequent weeks. After adaptation to these loads, 50–60% and greater loads were applied. From the 16th week of physiotherapy, a strength training was applied in isokinetic conditions at the angular velocity of 180°/s, and next 120°/s. Initially, the knee joint range of movement for extension and flexion of the involved limb was limited to 35–40% of the torque obtained for the preset angular velocity during the control measurement. When the patient increased the number of repetitions and his body adapted to the load in the series for the preset angular velocity, the value threshold for the strength load was increased during exercise performance to 50% and next, to 60% with Mmax and more during consecutive weeks. Exercising was interrupted when the patient could not bear the preset movement velocity any longer during a subsequent repetition or when he reported fatigue or pain threshold. After the patient’s adaptation to the above-mentioned loads during subsequent weeks of Stage III, two series of these exercises were introduced with a 3-minute rest break. At the end of Stage III, the exercises were performed at the full range of movements. |
| Stage IV 21st week to up to 8 months |
As above and additionally: Running with gradually increased speed, then with changing direction and the surface inclination angle. Deep proprioception and neuromuscular coordination were stimulated in the subjects performing discipline-specific or job-specific body movements, using balls, rockets and other sports equipment. Alternatingly, strength, balance, endurance and fitness were restored. Two-legged, one-legged and multi-jumps. Exercises with a skipping rope on different surfaces. Learning obstacle jumping, controlled slides with the physiotherapist’s assistance. Restoration of speed, power, agility and field orientation, specific for a given discipline or the patient’s job. Swimming recommended once a week. |
Continuation of strength training – alternatingly – under static and isokinetic conditions. During isokinetic training, speed reduction to 90, and next to 60°/s for extensor and flexor muscles of the operated knees. Concentric-eccentric resistance exercises on devices for large muscle groups. Similar exercises for the muscles affecting involved and uninvolved knees. Exercises in fitness rooms for the remaining muscle groups. |
Physiotherapeutic program
[see Table 2]
Tests
Circumferences and range of knee movement
Measurements of range of movement and knee joint/thigh circumferences were performed twice: during the 1st (I) and 12th week (II) after the reconstruction (Table 3). The circumference was measured at the level of knee joint fissures and 10 cm above the patellar base in both legs. The circumferences were measured in a supine position with 0.1-cm accuracy. The measurements of extension and flexion range of knees were performed in a prone position. The results were recorded with 1° accuracy.
Table 3.
Timetable of the different tests.
| Test | Weeks after reconstruction and study periods | |||||
|---|---|---|---|---|---|---|
| 1 | 12 | 13 | 16 | 21 | 24 | |
| Thigh and knee circumference | I | II | ||||
| Knee range of movement | I | II | ||||
| Maximum torque (in static) | I | II | ||||
| Peak torque (in isokinetic) | I | II | ||||
Measurements of limb circumference was not taken prior to the surgical procedures as the patients were available only after surgery performed in another centre and then referred to undergo rehabilitation at the Rehabilitation Centre of the College of Physiotherapy in Wrocław.
Torque of knee muscles
The patients underwent a 12-minute warm up on a cycloergometer at the frequency of 60 rpm and 60 watts in 6 minutes. Next, the power was increased every 2 minutes by 5–10 watts. The warm-up was followed by a break and the measurements were started after 8–10 minutes.
The measurements of muscle torque (Nm) of knee joint extensor and flexor muscles of involved and uninvolved legs were performed under static and isokinetic conditions using a Biodex 3 System (Biodex Medical Systems SHIRLEY, N.Y. 11967 USA, Model 333-250, Software – Biodex Advantage) [17]. For both measurement conditions, the trunk, pelvis and thighs were stabilized with stabilizing belts. The dynamometer head axis overlapped the axis of the examined joint. The lever arm leaning against the crus was placed at 40-cm from the knee joint axis. The measurements of maximal muscle torque of knee joint extensor and flexor muscles in static conditions were performed twice, during the 13th (I) and 21st (II) week after ACL reconstruction (Table 3). The better result was selected for further analysis. The patients assumed a seated position in the measuring chair, with the hip joint at the angle of 80° and knee joint at 70° for extensor muscles and 30° for flexor muscles. The measurement was initiated with the ‘start’ command and the result was recorded in the computer’s memory. The measurements began with the extensor muscles of the uninvolved knee. This was followed by a 1-minute break and then by the maximal muscle torque measurement of flexor muscles of the uninvolved knee. After finishing this procedure and a subsequent 1-minute break, the second measurement was performed, first for the extensor muscles, and, after a 1-minute break, for the flexor muscles of the uninvolved knee. The last measurement was followed by a 3-minute break to prepare the stand for the measurements of the operated leg. Next, the measurement of maximal torque was taken for extensor and flexor muscles of the involved knee, according to the above procedure applied to the uninvolved knee. The measurement of peak torque for knee joint extensor and flexor muscles in isokinetic conditions was also performed twice, during the 16th (I) and 24th (II) week after ACL reconstruction (Table 3), in a seated position with a hip joint angle of 80°. The test consisted of 8 alternant movements: extension and flexion of the knee of the uninvolved leg at the angular velocity of 180°/s. After a 3-minute break, the measurement of peak muscle torque was performed during a 5-fold alternant extension and flexion of the knee of the uninvolved leg at the angular velocity of 60°/s. This was followed by a 3-minute break to prepare the stand for the measurements of the involved leg and to allow the patient to rest. Next, the measurement of peak torque was taken under isokinetic conditions for the 2 groups of muscles of the operated knee, according to the above procedure performed for the uninvolved leg. The highest peak torques for the extensor and flexor muscles of the involved and uninvolved legs were selected for further analysis.
Statistic analysis
The statistic analysis used Student’s t-test for dependent trials evaluating the differences between mean values in the studied group, and Shapiro-Wilk test evaluating the normality of features distribution. The Microsoft Statistica 6 system was used for both tests. Arithmetic transformations are presented with the accuracy to the second digit after the decimal point, with the numbers rounded according to generally accepted principles. Results at the significance level minimum p<0.05 were considered significant.
Results
Knee/thigh circumferences and range of movement
The values represent means ±SD. The circumference results are given in cm and the flexion/extension results are given in degrees (ns – not significant).
The first test revealed a significant difference in knee joint circumference between the involved and uninvolved legs (Table 4). The average value of knee joint circumference of the involved extremities was 2.8 cm (7.4%) higher compared to the uninvolved legs, due to postoperative swelling. This difference disappeared in Session II, which was conducted during the 12th week of physiotherapy (Table 4). Conversely, thigh circumference measured 10 cm above the knee revealed a significant decrease in value for the involved knee joints compared to the uninvolved legs – on average a decrease of 2.3 cm (4.6%). This difference, resulting from a loss of muscle mass, was eliminated in Session II (Table 4).
Table 4.
Knee/thigh circumferences and flexion-extension range of movement tested at the 1st week (Session I) and 12 weeks (Session II) after ACL reconstruction.
| Test | Session | Uninvolved | Involved | p |
|---|---|---|---|---|
| Knee circumference | I | 38±3 | 41±4 | 0.001 |
| II | 38±3 | 38±3 | ns | |
| 10 cm above knee circumference | I | 50±4 | 48±3 | 0.01 |
| II | 50±4 | 49±3 | ns | |
| Knee flexion | I | 119±6 | 56±20 | <0.001 |
| II | 120±6 | 119±7 | ns | |
| Knee extension | I | 0.1±2.2 | 19±6 | <0.001 |
| II | 0.4±2.2 | 0.3±1.8 | ns |
From Table 4 it can be seen that the postoperative range of flexion was only 56°, which corresponded to a 53% deficit of the entire natural range as related to uninvolved knees. The patients also had a limited range of knee extension, which amounted to 19° during the first test. The 12-week physiotherapeutic program allowed the patients to restore the full range of flexion and extension of the knee, comparable to that of the uninvolved legs.
Muscle torque in static mode
The values of thigh circumference of the involved and uninvolved legs were already equalized during the 12th week of physiotherapy. During the 13th week of physiotherapy after ACL reconstruction, significantly lower values for extensor and flexor muscle torque under static conditions were noted for the operated knees as compared to the uninvolved ones (Table 5). Compared with the 13th week of physiotherapy, during the 21st week, a statistically significant increase in values was noted for the studied muscle torque for extensor and flexor muscles of the operated knees. The values for torque of the operated legs were comparable to those obtained for the uninvolved knees, amounting to 94.4% and 96.7% of the values for extensor and flexor muscles, respectively, of the uninvolved knees (Table 5).
Table 5.
Isometric torque of knee extensors and flexors tested at 13 and 21 weeks (Sessions I and II) after ACL reconstruction.
| Muscle group | Session | Uninvolved | Involved | p |
|---|---|---|---|---|
| Extensors | I | 238±51 | 117±46 | <0.001 |
| II | 265±62 | 250±66 | ns | |
| Flexors | I | 89±18 | 70±26 | <0.001 |
| II | 105±16 | 102±15 | ns |
The values represent means ± SD. The isometric torque results are given in Nm. ns = not significant.
Muscle torque in isokinetic mode
During the 16th week postoperatively, the peak torques for both angular velocities of flexor muscles of the involved knees were significantly lower than the values obtained for these muscles of the uninvolved knees (Tables 6A and 6B). In Session II (24th week of physiotherapy), the difference in torque for flexors of the involved knees and uninvolved legs was reduced for both angular velocities (Tables 6A and 6B). The value of extensor muscle torque of the involved knees, at the angular velocity of 180°/s, reached 151.98 Nm in Session II, showing a statistically significant increase of 66.57 Nm compared to the measurement taken in Session I. A similar direction of change, albeit at a higher level (Session II 204.71 Nm; Session I 104.60 Nm), was obtained for the extensor muscle torque at the angular velocity of 60°/s. This was a significant increase of 100.11 Nm. In Session II the values obtained for extensor muscle torque of the involved knees at both angular velocities were higher than the values obtained in Session I for extensor muscles of the uninvolved knees. However, when the values obtained in Session II for extensor muscle torque of the involved knees were compared with the torque values obtained in Session II for these muscles of the uninvolved knees, they were found to be about 9% lower at both angular velocities. These results were statistically significant (Tables 6A and 6B).
Table 6A.
Isokinetic peak torque at velocity 180°/s of knee extensors and flexors tested at 16 and 24 weeks (Sessions I and II) after ACL reconstruction.
| Muscle group | Session | Uninvolved | Involved | p |
|---|---|---|---|---|
| Extensors | I | 142±31 | 85±28 | <0.001 |
| II | 168±29 | 152±38 | 0.05 | |
| Flexors | I | 69±15 | 53±17 | <0.001 |
| II | 85±9 | 83±11 | ns |
The values represent means ± SD. The isokinetic peak torque results are given in Nm. ns = not significant.
Table 6B.
Isokinetic peak torque at velocity 60°/s of knee extensors and flexors tested at 16 and 24 weeks (Sessions I and II) after ACL reconstruction.
| Muscle group | Session | Uninvolved | Involved | p |
|---|---|---|---|---|
| Extensors | I | 190±39 | 105±31 | <0.001 |
| II | 226±45 | 205±55 | 0.002 | |
| Flexors | I | 82±24 | 62±20 | <0.001 |
| II | 100±19 | 94±15 | ns |
The values represent means ± SD. The isokinetic peak torque results are given in Nm. ns = not significant.
Flexion/extension ratio: the ratio of flexor to extensor torque under static conditions
In order to control the restoration process of muscle strength distribution during physiotherapeutic procedures, the flexion/extension ratio was used:
It is assumed that the flexion/extension ratio, based on the measurement performed under static conditions, is about 50%. This means that flexor muscle strength makes up about half of the strength of knee extensor muscles. Table 7 shows that the uninvolved legs diverged from the accepted norm; however, this was due to the measurement being made at other angular positions. Selection of these angular positions for the measurement of the studied muscle groups was, in our study, justified by clinical and biomechanical conditions (avoiding exposure to shear forces and conflicting location of the ligament graft toward bone canals).
Table 7.
Static strength ratio – flexor to extensor muscles.
| Session | Uninvolved | Involved |
|---|---|---|
| I (13th week) | 37% | 60% |
| II (21st week) | 40% | 41% |
In Session I, this distribution of strength was found to be disturbed in the operated knees (Table 7), due to the impairment of mainly extensor muscles (Table 5). However, during the 21st week of rehabilitation (Session II), the ratio value approached that obtained for the uninvolved legs (Table 7).
Discussion
The initial outcomes of the postoperative rehabilitation program, as compared to the positive results of the orthopaedic examination, were the improvement of the range of movement of the involved knee joints, and elimination of swelling and reconstruction of thigh muscle mass (circumference). In the first study (performed during the 1st week following reconstruction), the decrease in thigh circumference of the involved legs amounted to 4%, whereas in the second study (performed 12 weeks after reconstruction) the deficit was reduced to just over 1%, which was not statistically significant. The results from the first 2 studies also demonstrated that 12 weeks of physiotherapy restored the range of movement of the operated knee joints to almost that of the uninvolved legs. During the 13th week postoperatively, a significant deficiency was found in operated knee extensor and flexor muscle torque, measured using the static mode (by about 50% and 20%, respectively). As mentioned above, a gain in muscle mass was noted, manifested by increased thigh circumference values obtained in the second study during the 12th week of rehabilitation, before the increase in torque was measured using the static mode. This phenomenon does not conform to the sequence of training-related strength gain, involving primary strengthening of neuromuscular processes and activation of more functional units, which is then followed by an increase in muscle mass. However, this outcome of our studies can be interpreted differently. The thigh circumferences were found to be similar after 12 weeks of rehabilitation; these measurements were taken 10 cm above the knee joint. Thigh circumference is frequently measured at the area of its maximal thickness and, according to Martin’s technique, amounts to approximately 55 cm in males with body mass similar to that of our patients [18]. On the one hand, information on thigh circumference taken 10 cm above the knee joint fissure may indicate a gain in body mass of the medial quadriceps head. On the other hand, this is the region of knee joint upper recesses, whose contours may be somewhat larger, which changes the true value of knee circumference with muscle mass. Therefore, for future studies 2 measurement levels should be used, and ultrasonography of the recess region may also prove useful.
Given this point of reference, it should be assumed that the deficiency in muscle mass has not yet been fully compensated. An increase in body mass is usually triggered by alternation of isometric and dynamic training with a high load and an appropriate intensity. The content of body mass is manifested by a physiological cross-section, significantly connected with muscle strength. Intensive training with a high load during the first 2 stages, and even the first half of the third stage of the physiotherapeutic programme, is neither indicated nor applied. During the first 2 stages of the physiotherapeutic program, the patients should avoid exercises in open kinematic chains of extensor muscles of the involved knee and external rotators of the foreleg, which may result in the impact of high values of shear forces on the ACL graft. Therefore, due to biological and biomechanical conditioning related to healing rate and ligament reconstruction, the measurements, and next, isokinetic exercises, which were the basis for strength training intensification, were started as late as the 16th week postoperatively. At the end of the third stage and during the fourth stage of the physiotherapeutic program, other dynamic exercises were gradually introduced with additional load. Subsequently, the exercises were applied in several planes of movement for the whole body, including rotations of the involved knee, (PNF) proprioceptive neuromuscular facilitation dynamic elements and other concentric-eccentric exercises of different dynamics, load magnitude and degree of difficulty.
The torque results obtained for the studied muscle groups of the operated legs, performed using a static and an isokinetic mode, as compared to the results obtained for the uninvolved legs, indicate an unequal progress in torque increase during the sixth month postoperatively. During the 21st week after ACL reconstruction, the values for extensor and flexor muscle torque under isometric conditions were restored to near baseline levels. Likewise, during the 24th week after the reconstruction, similar results were noted for flexor muscle peak torque at both rotational velocities – 180 and 60°/s – of the involved and uninvolved knee joints. The values of extensor muscle peak torque of the operated knees at both angular velocities showed a significant improvement during the 24th week postoperatively compared to the 16th week postoperatively, and the results were approximately 91% of the values obtained at the same time for the uninvolved extremities. In other words, the values of the studied feature were on average 9% lower for the involved legs as compared to the values obtained for the uninvolved ones. Such an asymmetry is within normal limits in patients without knee joint injuries. Nevertheless, the results of the statistical analysis of the entire sample and evaluation of individual patient’s results suggest that in some patients it is still necessary to correct extensor muscle strength generation in the operated knees under dynamic conditions.
The lack of a standard control group in the study should now be explained. In our opinion, the inclusion of such a group in the study would positively affect the quality and transparency of the methods used in the study as well as the reliability of the obtained results. The specific points of reference for our study were the results and effects of rehabilitation procedures, obtained in similar studies by other authors, as well as the comparison of the results of precise examinations of uninvolved limbs in each patient.
Upon comparison of our study results with those obtained by other authors, we noted that Urabe et al. [19] did not obtain equalization of extensor muscle strength of the involved knees even after 12 months of rehabilitation, and at that time they reported a strength deficiency ranging from 8% to 10% in the involved legs. Such differences in time (delay) of muscle strength regain might have been due to the physiotherapeutic program. At our centre, the program of physiotherapy was implemented individually for each patient, on average 4 times a week for 6 months. The above-mentioned authors gradually instructed the patients how to carry out their physiotherapeutic program by themselves, at home. Wit and Mirowski et al. [20] obtained similar results for both legs between the 12th and 18th month after the reconstruction. Rebeyrotte et al. [21] noted a deficit in extensor muscle strength of the involved knees compared to the uninvolved ones 2.5 years after ACL reconstruction; under isokinetic conditions at the level of 15.3% for the angular velocity 60°/s and 11.3% for the angular velocity 180°/s. Andrade et al. [22] found a deficit of 34% in extensor muscle strength values of the involved knees compared to the uninvolved ones. A deficit at the level of 33% was still present in the 8th month after reconstruction when tested under isokinetic conditions at the angular velocity of 60º/s.
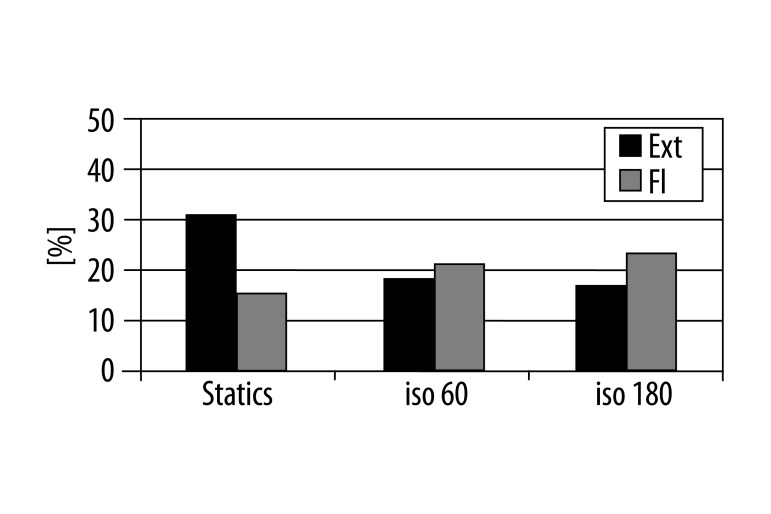
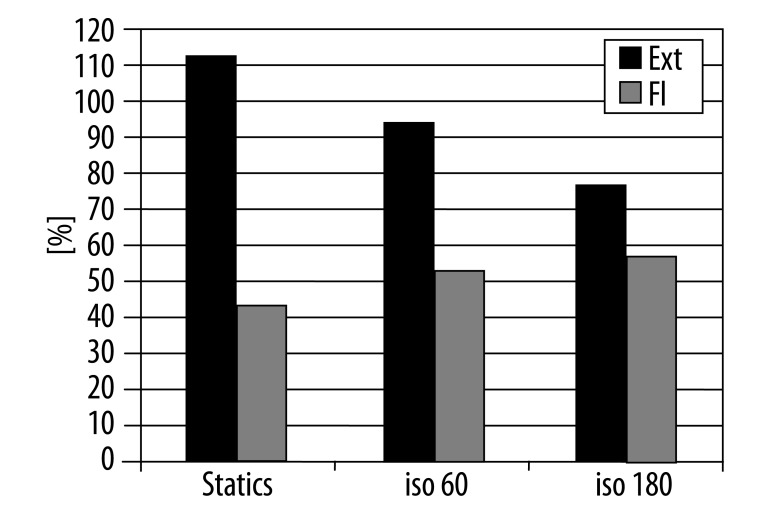
Our results should also be considered regarding the progress in training-related increase in strength. The uninvolved leg also loses strength due to limited physical activity after contusion. Therefore, the physiotherapeutic program also included application of the load on the muscles of the uninvolved legs. This resulted in the increase in muscle strength being obtained in both the affected and the unaffected limbs. Depending on the testing mode, the increase in strength of the uninvolved legs was noted to be between 18% and 30% for extensor muscles and between 15% and 22% for flexor muscles (Figure 1). The extent of muscle strength increase observed in the involved legs was greater, since the decrease in strength level was greater following the reconstruction (the baseline level of strength was lower). The increase ranged from 78% to 114% for extensor muscles and from 45% to 58% for flexor muscles (Figure 2).
Figure 1.
Percentage increase in static torque between the 13th and 21st week and peak torque in isokinetics (60 and 180°/s) between the 16th and 24th week of physiotherapy of the uninvolved legs.
Figure 2.
Percentage increase in static torque between the 13th and 21st week and peak torque in isokinetics (60 and 180°/s) between the 16th and 24th week of physiotherapy of the involved legs.
The strength ratio of flexor to extensor muscles is frequently used to control the progress in physiotherapy that attempts to gain the same distribution of muscle strength in the sagittal plane, affecting both the involved and the uninvolved knees, and may be applied in prevention and evaluation of the risk of sports-related injuries of the knee joint [21,23]. We were close to achieving this goal on the 21st week of physiotherapy.
Eitzen et al. assessed the effect of pre-operative torque deficit in quadriceps femoris muscle on the results obtained after 2 years following ACL reconstruction [24]. Other authors studied the correlation between changes in knee laxity after ACL surgery related to open kinetic chain knee extensor training load [25]. Additionally, in our study sample, we did not observe any complications presented in other papers [26].
It should be stressed, however, that despite significant progress, as demonstrated by the results for the studied features 24 weeks following the surgical procedure, the level of strength of extensor muscles of the involved knees was not fully restored under isokinetic conditions. This finding leads us to conclude that the period of physiotherapy should be extended beyond 6 months for some patients.
Conclusions
Six months of physiotherapy following ACL reconstruction in males favorably affected muscle strength values of the involved and uninvolved knees under static and isokinetic conditions.
Application of individual loads resulted in similar levels of muscle strength for extensors and flexors measured under static conditions, and in flexors muscle of the operated knees and the uninvolved knees measured under isokinetic conditions during the sixth month of physiotherapy.
After 6 months, a 9% deficit of extensor muscle strength under isokinetic conditions was observed in the involved knees, as compared to the uninvolved knees.
Footnotes
Source of support: Departmental sources
References
- 1.Jensen TQ, Fischer-Rasmussen T, Kjaer M, Magnusson S. Proprioception in poor – and well – functioning anterior cruciate ligament deficient patients. J Rehabil Med. 2002;34:141–49. doi: 10.1080/165019702753714174. [DOI] [PubMed] [Google Scholar]
- 2.Lisiński P, Gronek A, Samborski W, Dworak LB. Proposal for a rehabilitation regimen for patients after posterior cruciate ligament reconstruction surgery. A model of biomechanical study of the rehabilitation process. Polish Journal of Physiotherapy. 2010;1(4):1–11. [Google Scholar]
- 3.Woo SL-Y, Wu C, Dede O, et al. Biomechanics and anterior cruciate ligament reconstruction. J Orthop Surg Res. 2006;1(2):1–9. doi: 10.1186/1749-799X-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Czamara A. Rozprawa doktorska AWF Warszawa. 2006. Ocena postępowania fizjoterapeutycznego po rekonstrukcji więzadła krzyżowego przedniego. [in Polish] [Google Scholar]
- 5.De Carlo MS, Shelbourne KD, Mc Carroll JR, Retting AC. Traditional versus accelerated rehabilitation following ACL reconstruction: A one year follow up. J Orthop Sports Physical Therapy. 1992;15:309–16. doi: 10.2519/jospt.1992.15.6.309. [DOI] [PubMed] [Google Scholar]
- 6.Brewster CE, Seto JL. Summary of the rehabilitation program following anterior cruciate ligament reconstruction, from the Kerlan-Jobe Orthopaedic Clinic, Department of Physical Therapy. 2000. [Google Scholar]
- 7.Stefańska M, Rafalska M, Skrzek A. Functional assessment of knee muscles 13 weeks after anterior cruciate ligament reconstruction – pilot study. Ortop Traumat Rehab. 2009;11(2):145–55. [PubMed] [Google Scholar]
- 8.Tsakilis P, Abatzides G. ACL rehabilitation program using a combined isokinetic and isotonic strengthening protocol. Isokinetics and Exercise Science. 2002;10:211–19. [Google Scholar]
- 9.Czamara A. Moments of muscular strength of knee joint extensors and flexors during physiotherapeutic procedures following anterior cruciate ligament reconstruction in males. Acta Bioeng Biomech. 2008;3:37–44. [PubMed] [Google Scholar]
- 10.Rodeo SA, Arnoczky SP, Tortilli PA. Tendon- healing in bone tunel. A biomechanical and histological study in the dog. J Bone Joint Surg Am. 1993;75:1795–803. doi: 10.2106/00004623-199312000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Papageorgiou CD, Ma CB, Abramowitch SD, et al. A multidisciplinary study of the healing of an intraarticular anterior cruciate ligament graft in a goat model. Am J Sports Med. 2001;29:620–26. doi: 10.1177/03635465010290051501. [DOI] [PubMed] [Google Scholar]
- 12.Lisiński P, Samborski W. Porównanie skuteczności krioterapii i ciepłolecznictwa w urazach stawu kolanowego. Polish Journal of Sports Medicine. 2006;22(2):106–10. [in Polish] [Google Scholar]
- 13.Ari Y, Hara K, Takahashi T, et al. Evaluation of the vascular status of autogenous hamstring tendon grafts after anterior cruciate ligament reconstruction in humans using magnetic resonance angiography. Knee Surg Sports Traumatol Arthrosc. 2008;16:342–47. doi: 10.1007/s00167-007-0478-6. [DOI] [PubMed] [Google Scholar]
- 14.Yasuda K, Tomita F, Yamazaki S, et al. The effect of growth factors on biomechanical properties of the bone-patellar tendon-bone graft after anterior cruciate ligament reconstruction: a canine model study. Am J Sports Med. 2004;32:870–80. doi: 10.1177/0363546503261695. [DOI] [PubMed] [Google Scholar]
- 15.www.jnjgateway.com/commerce
- 16.Manske RC, Stovak M. In: Preoperative and Postsurgical Musculoskeletal Examination of the Knee in Postsurgical Orthopedic Sports Rehabilitation Knee & Shoulder. Manske RC, editor. Mosby; USA: 2006. [Google Scholar]
- 17.Biodex Advantage Software. Operations Manual (version 3.29 and 3.30) Biodex Medical Systems, Inc; New York: 2008. [Google Scholar]
- 18.Wojtyna J, Rodziewicz-Gruhu J. Zróżnicowanie morfologiczne kandydatów na studia wychowania fizycznego w WSP w Częstochowie w roku Akad. 1996/1997. Słupskie Prace Biologiczne. 2005;1:173–78. [in Polish] [Google Scholar]
- 19.Urabe Y, Ochi M, Onari K. Changes in Isokinetic Muscle Strength of the Lower Extremity in Recreational Athletes With Anterior Cruciate Ligament Reconstruction. J Sport Rehabil. 2002;11:252–67. [Google Scholar]
- 20.Wit A, Mirowski M. Biomechaniczna ocena własności dynamicznych mięśni stawu kolanowego. Acta Clinica. 2002;2:77–85. [Google Scholar]
- 21.Rebeyrotte I, Daviet JC, Oksman A, et al. Isokinetic evaluation of anterior cruciate ligament reconstruction using a free fascia lata graft strengthened by gracillis tendon. Isokinetics and Exercise Science. 2005;13:20–24. [Google Scholar]
- 22.Andrade MS, Cohen M, Picarro IC, Silva AC. Knee performance after anterior cruciate ligament reconstruction. Isokinet Exerc Sci. 2002;10:81–86. [Google Scholar]
- 23.Grygorowicz M, Kubacki J, Pilis W, et al. Selected isokinetic tests in knee injury prevention. Biol Sport. 2010;27:47–51. [Google Scholar]
- 24.Eitzen I, Holm I, Risberg MA. Preoperative quadriceps strength is a significant predictor of knee function two years after anterior cruciate ligament reconstruction. Br J Sports Med. 2009;43:371–76. doi: 10.1136/bjsm.2008.057059. [DOI] [PubMed] [Google Scholar]
- 25.Morrissey MC, Perry MC, King JB. Is Knee Laxity Change After ACL Injury and Surgery Related to Open Kinetic Chain Knee Extensor Training Load? American Journal of Physical Medicine & Rehabilitation. 2009;88(5):369–75. doi: 10.1097/PHM.0b013e3181a0d7ed. [DOI] [PubMed] [Google Scholar]
- 26.Almazan A, Herrera JP, Chaidez C, et al. A complication of soft tissue graft tibial fixation with the Intra Fix device. Med Sci Monit. 2009;15(1):CS19–21. [PubMed] [Google Scholar]