Abstract
The arylamine N-acetyltransferase 2 (NAT2) enzymes detoxify a wide range of naturally occurring xenobiotics including carcinogens and drugs. Point mutations in the NAT2 gene result in the variant alleles M1 (NAT2 *5A), M2 (NAT2*6A), M3 (NAT2*7) and M4 (NAT2 *14A) from the wild-type WT (NAT2 *4) allele. The current study was aimed at screening genetic polymorphisms of NAT2 gene in 49 lung cancer patients, 54 colorectal cancer patients and 99 cancer-free controls, using PCR-RFLP. There were significant differences in allele frequencies between lung cancer patients and controls in the WT, M2 and M3 alleles (p < 0.05). However, only M2 and M3 allele frequencies were different between colorectal cancer patients and controls (p < 0.05). There was a marginal significant difference in the distribution of rapid and slow acetylator genotypes between lung cancer patients and controls (p = 0.06 and p = 0.05, respectively), but not between colorectal cancer patients and controls (p = 1.0 and p = 0.95, respectively). Risk of lung cancer development was found to be lower in slow acetylators [odds ratio (OR): 0.51, 95% confidence interval (95% CI): 0.25, 1.02, p-value = 0.07]. No effect was observed in case of colorectal cancer. Our results showed that NAT2 genotypes and phenotypes might be involved in lung cancer but not colorectal cancer susceptibility in Jordan.
Keywords: NAT2, lung cancer, colorectal cancer, polymorphisms
Introduction
Lung cancer is one of the most prevalent cancers worldwide and comprises three major histological subtypes, adenocarcinoma, squamous cell carcinoma, and small cell carcinoma. In Jordan, 299 lung cancer cases were registered in 2009, accounting for (6.2%) of all newly diagnosed cases among Jordanians. It ranked third among all new cancers. Among males it ranked second, affecting 256 (11.2%) of the individuals, and among females it ranked twelfth, with 43 (1.7%) affected individuals (Tarawneh et al., 2009).
Colorectal cancer is one of the most common cancers in the world. In recent years, a dramatic increase in colorectal cancer incidence has been reported in several countries (Shin and Kim, 2010). In Jordan, there were 554 colorectal cancer cases in 2009; accounting for (11.9%) of all newly diagnosed cases among Jordanians. It ranked second among all new cancers, and first among males, where it affected 290 (12.7%) and second among females, with 264 (10.5%) affected individuals (Tarawneh et al., 2009).There are several risk factors involved in the formation of colorectal and lung cancers including diet, cigarette smoking, aging, as well as different susceptibilities to carcinogens (Vineis, 2003; Donaldson, 2004).
N-acetyltransferase 2 (NAT2) is an enzyme found in a large number of organs such as the lungs, colon, breast, prostate, and liver. The expression of this enzyme suggests that it plays a key role in the protection against reactive molecules resulting from environmental insults, not only in the liver but in all target tissues (Windmill et al., 2000). The NAT2 gene, located in short arm of chromosome 8(8p22), has no introns. It contains an 870 bp open reading frame that encodes a protein of 290 amino acids (Blum et al., 1990). It is an important phase II enzyme that catalyzes the acetylation of aromatic and heterocyclic amines and hydrazines present in carcinogenic compounds and medicines. NAT2 is involved in the initial biotransformation metabolism of aromatic amines and hydrazines. It catalyzes the transfer of an acetyl group from acetyl CoA to the nitrogen of substrate. Polymorphisms at the NAT2 gene locus result in impaired enzyme activity (Borlak and Reamon-Buettner, 2006).There are three NAT2 phenotypes: The fast acetylation phenotype which consists of two copies of wild type allele (WT), an intermediate phenotype with one wild type allele and a mutant allele, and a slow acetylator phenotype comprising two mutated alleles. Individuals homozygous or heterozygous for the NAT2 WT allele are classified as rapid acetylators whereas those homozygous for any of the remaining (mutant) alleles are classified as slow acetylators (Seow et al., 1999). The functional state of the phenotype is due to the impairment of protein translation or stability. No changes in mRNA levels were detected (da Silva et al., 2011).
The association between genetic polymorphisms in the NAT2 gene and lung and colorectal cancers has been studied extensively; however, the results are not conclusive, possibly because of ethnic differences and differences in the life style and number of patients studied. Some studies indicate that fast acetylators are not associated with the incidence of colorectal cancer (Hubbard et al., 1997), while other studies suggest that NAT1 and NAT2 genotypes may jointly contribute to individual susceptibility. Furthermore, heterocyclic amines may play an important role in colorectal cancer associated with red meat and also exposure to tobacco smoke (Lilla et al., 2006). Some studies have detected a positive association of lung cancer risk with NAT2 polymorphisms (Hou et al., 2000; Zhou et al., 2002).
The proportion and number of fast and slow acetylation phenotypes varies markedly depending on ethnicity and geographic origin (Garte et al., 2001). The populations of Europe and North America contain from 40 to 70% of slow acetylators, whereas only 10 to 30% of slow acetylators were found among populations of the Asian pacific coast; Japanese, Chinese and Koreans (Meyer and Zanger, 1997). Thus, there is an urgent need for studies investigating the distribution of NAT2 genotypes in different countries. The aim of this study was to investigate NAT2 polymorphisms in colorectal and lung cancer patients and cancer-free controls from Jordan.
Materials and Methods
Patients and controls
A case-control study involving 49 patients (5 women and 44 men) histopathologically diagnosed for lung cancer, 54 patients (26 women and 28 men) histopathologically diagnosed for colorectal cancer, and 99 cancer-free controls (7 women and 92 men) presented at the Urology Clinic of the King Abdullah University Hospital in Irbid during July 2004 to September 2005 were included in this study. The mean age for the lung, colorectal cancer patients and controls was 58, 56, and 53 years, respectively. The age ranged from 36 to 82 years in lung cancer patients, from 21 to 90 years in colorectal cancer patients, and from 26 to 80 years in controls. The study was approved by the University Review Committee for Research on Humans and all patients and controls signed an informed consent form. All participants provided a sample of blood (stored at −80 °C until use) for isolation of DNA and completed a questionnaire covering demographic factors. The study design was also approved by the Institutional Review Board at King Abdullah University Hospital.
Genomic DNA extraction
Genomic DNA of all participants was extracted from peripheral venous blood collected with ethlendiaminetetraacetic acid (EDTA) tubes using Wizard Genomic DNA Purification kit (Promega, USA) according to the protocol supplied by the manufacturer.
Genotype analysis
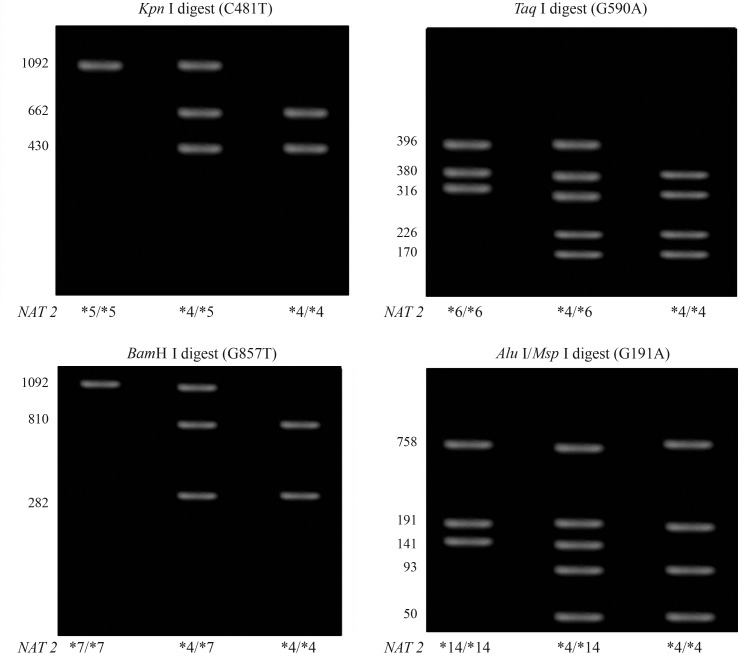
A 1092 bp fragment of the NAT2 gene locus containing the region of interest was amplified by the polymerase chain reaction (PCR) as described previously (He et al., 2005) using a MyCycler Thermal Cycler (BioRad, Italy) and respective reagents (Promega, USA). NAT2-specific primers were synthesized by Alpha DNA Inc. (Montreal, Canada). The primer sequences were 5′-GGA ACA AAT TGG ACT TGG-3′ and 5′-TCT AGC ATG AAT CAC TCT GC-3′. After amplification, PCR-products were digested with Kpn I (M1 allele), Taq I (M2 allele), BamH I (M3 allele), and Msp I/Alu I (M4 allele) according to the protocol supplied by the manufacturer (Promega, USA). The digested fragments were separated on Agarose gels stained with ethidium bromide and visualized under UV light. The different sizes of the digested products that allowed the individual’s genotype to be determined are shown diagrammatically (Figure 1). The WT/WT and WT/Mx genotypes were classified as conferring the fast acetylation phenotype and the Mx/Mx genotype as conferring the slow acetylation phenotype.
Figure 1.
Genotype determination by using PCR-RFLP of the NAT2 gene fragment. Following PCR amplification separate digestions of each PCR product were carried out with the restriction enzymes Kpn I, Taq I, BamH I and Alu I/Msp I to detect the substitutions C481T, G590A, G857A and G191A, respectively. The different sizes of the digested products for each restriction enzyme which allow the individual’s genotype to be determined are shown diagrammatically.
Statistical analysis
Differences in allele and genotype frequency distributions in cases and controls were determined by Chi-square test. A Chi-square test was also used to confirm Hardy-Weinberg equilibrium for the three groups (lung, colorectal and controls).
The association between the NAT2 polymorphisms and the risk of colorectal and lung cancer was assessed by calculating the odds ratios (OR) and 95% confidence intervals (CIs) by unconditional logistic regression. The fast acetylators (WT/WT and WT/Mx genotypes) were used as reference and ORs were calculated with respect to this reference as the WT/WT numbers were very small. A p-value < 0.05 was considered to be statistically significant and a p-value of 0.05 to 0.1 as marginally so. The SPSS 14.0 statistical package was used for all statistical analyses.
Results
A total of 202 blood samples were collected at the King Abdullah University Hospital, including 49 samples from lung cancer patients, 54 samples from colorectal cancer patients, and 99 samples from cancer-free controls. Table 1 shows selected demographic characteristics of the patients and controls. Genotyping of NAT2 polymorphisms was done using PCR-RFLP. The 1093 bp PCR product of the NAT2 gene was digested with Kpn I, Taq I, BamH I, and Alu I/Msp I restriction enzymes (Figure1). Four types of NAT2 alleles were found in all groups, including the wild-type WT allele and polymorphisms of M1, M2, and M3 alleles. The M4 polymorphism was not found in any of the groups.
Table 1.
Demographic characteristics of cancer-free controls, lung and colorectal cancer patients (n = 202).
| Characteristic | Cancer-free controls
|
Lung cancer
|
Colorectal cancer
|
|||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Sex | ||||||
| Males | 92 | 93 | 44 | 90 | 28 | 52 |
| Females | 7 | 7 | 5 | 10 | 26 | 48 |
|
| ||||||
| Race | ||||||
| Caucasian | 95 | 96 | 48 | 98 | 50 | 93 |
| Other | 4 | 4 | 1 | 2 | 4 | 7 |
|
| ||||||
| Family history of cancer | ||||||
| Yes | 0 | 0 | 3 | 6 | 4 | 7 |
| No | 99 | 100 | 46 | 94 | 50 | 93 |
|
| ||||||
| Smoking status | ||||||
| Never | 43 | 42 | 11 | 22 | 33 | 6 |
| Current | 56 | 58 | 38 | 78 | 21 | 39 |
|
| ||||||
| Type of lung cancer | ||||||
| Non small cell carcinoma | 41 | 84 | ||||
| Small cell carcinoma | 4 | 8 | ||||
| Other | 4 | 8 | ||||
|
| ||||||
| Type of colorectal cancer | ||||||
| Colon | ||||||
| Adenocarcinoma | 25 | 46 | ||||
| Mucinous carcinoma | 3 | 6 | ||||
| Rectum | ||||||
| Adenocarcinoma | 24 | 44 | ||||
| Mucinous carcinoma | 2 | 4 | ||||
|
| ||||||
| Mean ± SD | ||||||
| Age (years) | 53 ± 14 | 57 ± 10 | 56 ± 11 | |||
Lung cancer
The NAT2 allele and genotype frequencies for lung cancer patients and cancer-free controls are shown in Table 2. There was a statistically significant difference in allele frequencies between lung cancer patients and the controls in the WT, M2 and M3 alleles (p < 0.05) but not in the M1 allele (p > 0.05). M1 was apparent as the major polymorphism in the control group (37%), while M2 was the major one in the lung cancer patients (34%) (Table 2).
Table 2.
Allele frequency of NAT2 gene in cancer-free controls and lung cancer patients.
| Cancer-free controls | Lung cancer patients | X2 statistics | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Allele | n | Frequency | n | Frequency | X2 | P |
| WT* | 39 | 0.19 | 28 | 0.28 | 5.47 | 0.019 |
| M1 | 73 | 0.37 | 32 | 0.33 | 0.53 | 0.46 |
| M2* | 41 | 0.21 | 33 | 0.34 | 5.91 | 0.015 |
| M3* | 45 | 0.23 | 5 | 0.05 | 14.48 | 0.001 |
| Total | 198 | 1 | 98 | 1 | ||
Significant p < 0.05.
There was a marginal statistically significant difference in the distribution of rapid and slow acetylator genotypes between controls and lung cancer patients (p = 0.05 and p = 0.06 respectively) (Tables 3 and 4). Lung cancer patients showed a higher frequency for rapid acetylators (55.1%) than controls (38.4%) and a lower frequency of slow acetylators (44.9%) compared to controls (61.6%) (Tables 3 and 4). A statistically significant difference was observed between controls and lung cancer patients with respect to the WT/M2 genotype (p < 0.05) among rapid acetylators and the M1/M3 genotype (p < 0.05) which can be explained by the absence of the M1/M3 genotype in the lung cancer group (Table 3).
Table 3.
The percentage of rapid acetylator genotypes in cancer-free controls and lung cancer patients.
| Cancer-free controls | Lung cancer patients | X2 statistics | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Genotype | n | % | n | % | X2 | p |
| WT/WT | 1 | 1.01 | 2 | 4.08 | 1.50 | 0.2 |
| WT/M1 | 29 | 29.29 | 10 | 20.41 | 1.38 | 0.2 |
| WT/M2* | 1 | 1.01 | 14 | 28.57 | 27.30 | 0.000001 |
| WT/M3 | 7 | 7.07 | 1 | 2.04 | 1.62 | 0.2 |
| Total | 38 | 38.40 | 27 | 55.10 | 3.85 | 0.05 |
Significant p < 0.05.
Table 4.
The percentage of slow acetylator genotypes in cancer-free controls and lung cancer patients.
| Cancer-free controls | Lung cancer patients | X2 statistics | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Genotype | n | % | n | % | X2 | p |
| M1/M1 | 3 | 3.03 | 5 | 10.20 | 3.20 | 0.07 |
| M1/M2 | 12 | 12.12 | 11 | 22.45 | 2.53 | 0.10 |
| M1/M3* | 26 | 26.26 | 0 | 0 | 15.5 | 0.0006 |
| M2/M2 | 8 | 8.08 | 2 | 4.08 | 0.91 | 0.34 |
| M2/M3 | 12 | 12.12 | 4 | 8.16 | 0.59 | 0.44 |
| M3/M3 | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | 61 | 61.62 | 22 | 44.89 | 3.40 | 0.06 |
Significant p < 0.05.
Logistic regression analysis was performed to check the association between NAT2 genotypes and risk of developing lung cancer. Due to the low number of homozygous wild type genotypes (rapid acetylators), we pooled homozygotes (WT/WT) and heterozygotes (WT/Mx) as reference for calculating odd ratios. A marginal statistically significant decrease in risk for developing lung cancer was observed in slow acetylator genotypes when the WT/WT and WT/Mx genotypes were used as reference (Table 5). The ORs and 95% CIs were 0.51 [0.25–1.02] and p = 0.06.
Table 5.
Crude OR relationship between NAT2 genotypes and lung cancer by using rapid acetylators as a reference.
| Cancer-free controls | Lung cancer patients | Statistics | |||
|---|---|---|---|---|---|
|
|
|
||||
| Genotype | n | % | n | % | OR (95% CI)* |
| WT/WT & WT/Mx | 38 | 38.4 | 27 | 55.1 | 1.0 (Reference) |
| Mx/Mx | 61 | 61.6 | 22 | 44.9 | 0.51 [0.25 1.02] |
p = 0.06.
X = 1, 2, 3; OR: odd ratio; CI: confidence interval.
Colorectal cancer
The NAT2 allele and genotype frequencies for colorectal cancer patients and cancer-free controls are shown in Table 6. There was a statistically significant difference in allele frequencies between colorectal cancer patients and the cancer-free controls in the M2 and M3 alleles (p < 0.05) but not in the WT and M1 alleles (p > 0.05). M1 was the major polymorphism in the control group (37%), while M2 is the major one in the colorectal cancer patients (36%).
Table 6.
Allele frequency of NAT2 gene in cancer-free controls and colorectal cancer patients in Jordan.
| Cancer-free controls | Colorectal cancer patients | X2 statistics | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Allele | n | Frequency | n | Frequency | X2 | p |
| WT | 39 | 0.20 | 26 | 0.24 | 0.77 | 0.38 |
| M1 | 73 | 0.37 | 31 | 0.29 | 2.00 | 0.16 |
| M2* | 41 | 0.21 | 39 | 0.36 | 8.59 | 0.003 |
| M3* | 45 | 0.23 | 14 | 0.13 | 4.23 | 0.04 |
| Total | 198 | 1 | 108 | 1 | ||
Significant p < 0.05.
There was no statistically significant difference in the distribution of rapid and slow acetylator genotypes between controls and colorectal cancer patients (p = 0.95 and p = 1.0, respectively). Both controls and colorectal cancer patients had similar frequencies for rapid acetylators (38.4 and 38.9%, respectively) and for slow ones (61.6% and 61.1%, respectively) (Tables 7 and 8). Nonetheless, a statistically significant difference was observed between cancer-free controls and colorectal cancer patients concerning the frequency of WT/WT, WT/M1 and WT/M2 genotypes among rapid acetylators (p < 0.05) but not so in the WT/M3 genotype frequency (Table 7). On the other hand, among slow acetylator genotypes, there was a statistically significant difference between controls and colorectal cancer patients in the frequencies of M1/M1, M1/M2, M1/M3 and M3/M3 genotypes (p < 0.05) but not in the frequency of M2/M2 and M2/M3 genotypes (Table 8).
Table 7.
The percentage of rapid acetylator genotypes in cancer-free controls and colorectal cancer patients.
| Cancer-free controls | Colorectal cancer patients | X2 statistics | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Genotype | n | % | n | % | X2 | p |
| WT/WT* | 1 | 1.01 | 5 | 9.26 | 6.38 | 0.01 |
| WT/M1* | 29 | 29.29 | 5 | 9.26 | 8.10 | 0.004 |
| WT/M2* | 1 | 1.01 | 9 | 16.67 | 14.10 | 0.0001 |
| WT/M3 | 7 | 7.07 | 2 | 3.70 | 0.73 | 0.4 |
| Total | 38 | 38.38 | 21 | 38.89 | 0 | 0.95 |
Significant p < 0.05.
Table 8.
The percentage of slow acetylator genotypes in cancer-free controls and colorectal cancer patients.
| Cancer-free controls | Colorectal cancer patients | X2 statistics | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Genotype | n | % | n | % | X2 | p |
| M1/M1* | s3 | 3.03 | 3 | 5.55 | 4.88 | 0.03 |
| M1/M2* | 12 | 12.12 | 19 | 35.19 | 11.50 | 0.0007 |
| M1/M3* | 26 | 26.26 | 1 | 1.85 | 14.20 | 0.0001 |
| M2/M2 | 8 | 8.08 | 3 | 5.56 | 0.33 | 0.56 |
| M2/M3 | 12 | 12.12 | 5 | 9.26 | 0.32 | 0.56 |
| M3/M3* | 0 | 0 | 2 | 3.7 | 4 | 0.045 |
| Total | 61 | 61.62 | 33 | 61.11 | 0 | 1 |
Significant p < 0.05.
Logistic regression analysis was performed to look at the association between NAT2 genotypes and risk of developing colorectal cancer. Due to the low number of homozygous wild type genotypes (rapid acetylators), both homozygotes (WT/WT) and heterozygotes (WT/Mx) were used as reference for calculating odd ratios. There was no reduction or increase in the risk of developing colorectal cancer when the WT/WT and WT/Mx genotypes were used as a reference (Table 9). The ORs and 95% CIs were 0.98 [0.50–1.93] and p = 1.0.
Table 9.
Crude OR and 95% CI of NAT2 genotypes and colorectal cancer by using rapid acetylator genotypes as reference.
| Cancer-free controls | Colorectal cancer patients | Statistics | |||
|---|---|---|---|---|---|
|
|
|
||||
| Genotype | n | % | n | % | OR (95%CI)* |
| WT/WT & WT/Mx | 38 | 38.4 | 21 | 38.9 | 1.0 (Reference) |
| Mx/Mx | 61 | 61.6 | 33 | 61.1 | 0.98 [0.50 1.93] |
p = 1.0.
x = 1, 2, 3; OR: odd ratio; CI: confidence interval.
Discussion
This study is the first to examine NAT2 polymorphisms in cancer-free individuals; lung and colorectal cancer patients in Jordan and the Middle East in general. The most important finding of this investigation is that differences in the frequency of NAT2 genotypes/phenotypes do exist among different populations and ethnic groups. In this regard, a high frequency of the slow acetylator phenotype among cancer-free Jordanians is similar to what has been observed in populations of European and African descent (Garte et al., 2001). Other populations such as Japanese, Chinese and Amerindians are characterized by a high frequency of fast acetylation phenotypes (da Silva et al., 2011). Although only marginally significant, slow acetylator genotypes were found to be protective when comparing lung cancer patients to cancer-free controls. No positive or negative effects were seen in case of colorectal cancer.
Bell et al. (1993) reported a significant difference in the frequencies of WT, M1, and M4 alleles between Caucasian and African-Americans, while the frequencies of M2 and M3 alleles were similar. No M4 allele was found in Caucasian-Americans, whereas 18% of African-Americans carried at least one M4 allele (He et al., 2005). In this study the frequencies of WT, M1, M2, M3 and M4 were 0.2, 0.37, 0.21 and 0.23, respectively. These frequencies are comparable to those found in the United Arab Emirates, being 0.18, 0.54, 0.21, and 0.070, respectively (Woodhouse et al., 1997), in Egypt with 0.22, 0.5, 0.26 and 0.03 (Anwar et al., 1996) and in Oman with 0.19, 0.52, 0.25 and 0.04 respectively (Tanira et al., 2003).
NAT2 polymorphisms and lung cancer
Lung cancer ranked second among Jordanian men and tenth in women. We studied three polymorphisms involved in the metabolism of carcinogens associated with lung cancer in Jordan. We did not detect any association between lung cancer and these polymorphisms. However, upon grouping the genotypes into rapid and slow acetylators, the slow acetylation genotypes showed an unexpected marginal reduction in lung cancer risk.
Many previous studies had reported that there was no overall association of NAT2 acetylator genotypes with lung cancer risk, but indicated increased risk with other factors, such as age, gender and smoking (Oyama et al., 1997; Hou et al., 2000; Zhou et al., 2002; Sorensen et al., 2005; Osawa et al., 2007). In a study consisting of 1,115 lung cancer cases, in which age, gender, smoking status and pack years of smoking were considered, no overall relationship was found between NAT2 genotypes and lung cancer risk (Zhou et al., 2002).On the other hand, other epidemiological studies showed a significant association between NAT2 acetylation genotypes and lung cancer. A slow acetylator genotype was associated with increased risk of lung cancer among non-smoking Chinese women in Singapore (Seow et al., 1999), while a rapid acetylator genotype was associated with an increased risk for developing lung cancer among never smoking Chinese women in Taiwan (Chiou et al., 2005). Notwithstanding, no overall association was found between NAT2 genotypes and lung cancer risk (Borlak and Reamon-Buettner, 2006).
This discrepancy over results could be due to lack of uniformity in the design, analysis, reporting, and exposure variables. In addition to NAT2, other factors could modify the susceptibility of the individual to lung cancer. NAT2 genotypes might confer a lung cancer risk when combined with other genes. For example, individuals with NAT2 slow acetylator genotypes combined with NAT1 had a significantly elevated adenocarcinoma risk. Moreover, the combination of slow acetylator genotypes and GSTM1 null genotype might increase adduct formation, gene mutation and lung cancer with smoking (Oyama et al., 1997).
NAT2 polymorphisms and colorectal cancer
We found no association between studied NAT2 polymorphisms and risk of colorectal cancer. This is in agreement with findings reported by (Borlak and Reamon-Buettner, 2006) who detected no overall association between colorectal cancer and acetylator genotypes. However, the same authors reported had an inverse association of the M1/M1 genotype to colon cancer risk, and thus an apparent protection against the disease. On the other hand, other genetic epidemiological studies (UK population and Singapore Chinese), showed that rapid acetylator phenotype might be associated with a higher incidence of colorectal cancer (Barrett et al., 2003; Lee et al., 1998).
Moreover, Kiss et al. (2000) provided evidence that the carriers of rapid acetylator alleles presented higher levels of DNA strand breaks in exfoliated colorectal mucosa cells following a two-day “high meat” diet. Thus, the NAT1 and NAT2 genotypes coding for the rapid acetylator phenotype carry a higher risk for colorectal cancer (Roberts-Thomson et al., 1999). This association was also confirmed in a Chinese population with diagnosed colorectal carcinoma (Frazier et al., 2001).
It has been reported that NAT2 alone could not be a risk factor for colon cancer (Ye and Parry, 2002). Heterocyclic amine (HCA) from consumption of meat and fish could increase the risk for rectal cancer in men, but did not appreciably affect the risk for rectal cancer in women or for colon cancer in either sex (Le March et al., 2002; Chan et al. 2005) reported an association between high intake of red meat and incidence of colorectal cancer risk, particularly among women with rapid acetylator NAT2 genotypes. Another study done in the southern region of Turkey suggested that the exposure to carcinogens through a high-protein diet might increase the risk of colorectal carcinoma only in genetically-susceptible individuals, with smoking status not differing between the control and patient group (Tamer et al., 2006).
In summary, our results showed significant differences in allele frequencies between cancer-free controls and both lung and colorectal cancer patients. There was a marginal significant difference in the distribution of rapid and slow acetylator genotypes between lung cancer patients and controls, but not between colorectal cancer patients and controls. A risk for developing lung cancer was found to be lower in slow acetylators. No effect was observed with regard to colorectal cancer. In conclusion, NAT2 genotypes might be involved in lung cancer but not in colorectal cancer be susceptibility in Jordan, and correspondingly, NAT2 can used as a potential marker for lung cancer risk. However, further studies are needed on a larger number of patients to confirm these results.
Acknowledgments
The authors would like to thank all participants of the study as well as the staff at King Abdullah University Hospital for their assistance in collecting samples. We also would like to acknowledge the Deanships of Research at University of Sharjah and at Jordan University of Science and Technology for financial support.
Footnotes
Associate Editor: Jeremy A. Squire
References
- Anwar WA, Abdel-Rahman SZ, El-Zein RA, Mostafa HM, Au WW. Genetic polymorphism of GTM1, CYP2E1 and CYP2D6 in Egyptian bladder cancer patients. Carcinogenesis. 1996;17:1923–1929. doi: 10.1093/carcin/17.9.1923. [DOI] [PubMed] [Google Scholar]
- Barrett JH, Smith G, Waxman R, Gooderham N, Lightfoot T, Garner RC, Augustsson K, Wolf CR, Bishop DT, Forman D. Investigation of interaction between N-acetyltransferase 2 and heterocyclic amines as potential risk factors for colorectal cancer. Carcinogenesis. 2003;24:275–282. doi: 10.1093/carcin/24.2.275. [DOI] [PubMed] [Google Scholar]
- Bell DA, Taylor JA, Butler MA, Stephens EA, Wiest J, Brubaker LH, Kadlubar FF, Lucier GW. Genotype/phenotype discordance for human arylamine N-acetyltransferase (NAT2) reveals a new slow-acetylator allele common in African-Americans. Carcinogenesis. 1993;14:1689–1692. doi: 10.1093/carcin/14.8.1689. [DOI] [PubMed] [Google Scholar]
- Blum M, Grant DM, McBride W, Heim M, Meyer UA. Human arylamine N-acetyltransferase genes: Isolation, chromosomal localization, and functional expression. DNA Cell Biol. 1990;9:193–203. doi: 10.1089/dna.1990.9.193. [DOI] [PubMed] [Google Scholar]
- Borlak J, Reamon-Buettner SM. N-acetyltransferase 2 (NAT2) gene polymorphisms in colon and lung cancer patients. BMC Med Genet. 2006;7:e58. doi: 10.1186/1471-2350-7-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan AT, Tranah GJ, Giovannucci EL, Willett WC, Hunter DJ, Fuchs CS. Prospective study of N-acetyltransferase-2 genotypes, meat intake, smoking and risk of colorectal cancer. Int J Cancer. 2005;115:648–652. doi: 10.1002/ijc.20890. [DOI] [PubMed] [Google Scholar]
- Chiou HL, Wu MF, Chien WP, Cheng YW, Wong RH, Chen CY, Lin TS, Lee H. NAT2 fast acetylator genotype is associated with an increased risk of lung cancer among never-smoking women in Taiwan. Cancer Lett. 2005;223:93–101. doi: 10.1016/j.canlet.2004.12.015. [DOI] [PubMed] [Google Scholar]
- da Silva TD, Felipe AV, de Lima JM, Oshima CTF, Forones NM. N-acetyltransferase 2 genetic polymorphisms and risk of colorectal cancer. World J Gastroenterol. 2011;17:760–765. doi: 10.3748/wjg.v17.i6.760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donaldson MS. Nutrition and cancer: A review of the evidence for an anti-cancer diet. Nutr J. 2004;3:19. doi: 10.1186/1475-2891-3-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frazier ML, O’Donnell FT, Kong S, Gu X, Campos I, Luthra R, Lynch PM, Amos CI. Age-associated risk of cancer among individuals with N-acetyltransferase 2 (NAT2) mutations and mutations in DNA mismatch repair genes. Cancer Res. 2001;61:1269–1271. [PubMed] [Google Scholar]
- Garte S, Gaspari L, Alexandrie AK, Ambrosone C, Autrup H, Autrup JL, Baranova H, Bathum L, Benhamou S, Boffetta P, et al. Metabolic gene polymorphism frequencies in control populations. Cancer Epidemiol Biomarkers Prev. 2001;10:1239–1248. [PubMed] [Google Scholar]
- He LJ, Yue YM, Qiao F, Liu JS, Sun XF, Jiang LL. Genetic polymorphisms of N-acetyltransferase 2 and colorectal cancer risk. World J Gastroenterol. 2005;11:4268–4271. doi: 10.3748/wjg.v11.i27.4268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou SM, Ryberg D, Fält S, Deverill A, Tefre T, Børresen AL, Haugen A, Lambert B. GSTM1 and NAT2 polymorphisms in operable and non-operable lung cancer patients. Carcinogenesis. 2000;21:49–54. doi: 10.1093/carcin/21.1.49. [DOI] [PubMed] [Google Scholar]
- Hubbard AL, Harrison DJ, Moyes C, Wyllie AH, Cunningham C, Mannion E, Smith CA. N-acetyltransferase 2 genotype in colorectal cancer and selective gene retention in cancers with chromosome 8p deletions. GUT. 1997;41:229–234. doi: 10.1136/gut.41.2.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiss I, Sandor J, Ember I. Allelic polymorphism of GSTM1 and NAT2 genes modifies dietary-induced DNA damage in colorectal mucosa. Eur J Cancer Prev. 2000;9:429–432. doi: 10.1097/00008469-200012000-00009. [DOI] [PubMed] [Google Scholar]
- Lee EJ, Zhao B, Seow-Choen F. Relationship between polymorphism of N-acetyltransferase gene and susceptibility to colorectal carcinoma in a Chinese population. Pharmacogenetics. 1998;8:513–517. doi: 10.1097/00008571-199812000-00008. [DOI] [PubMed] [Google Scholar]
- Le Marchand L, Hankin JH, Pierce LM, Sinha R, Nerurkar PV, Franke AA, Wilkens LR, Kolonel LN, Donlon T, Seifried A, et al. Well-done red meat, metabolic phenotypes and colorectal cancer in Hawaii. Mutat Res. 2002;506:205–214. doi: 10.1016/s0027-5107(02)00167-7. [DOI] [PubMed] [Google Scholar]
- Lilla C, Verla-Tebit E, Risch A, Jager B, Hoffmeister M, Brenner H, Chang-Claude J. Effect of NAT1 and NAT2 genetic polymorphisms on colorectal cancer risk associated with exposure to tobacco smoke and meat consumption. Cancer Epidemiol Biomarkers Prev. 2006;15:99–107. doi: 10.1158/1055-9965.EPI-05-0618. [DOI] [PubMed] [Google Scholar]
- Meyer UA, Zanger UM. Molecular mechanisms of genetic polymorphisms of drug metabolism. Annu Rev Pharmacol Toxicol. 1997;37:269–296. doi: 10.1146/annurev.pharmtox.37.1.269. [DOI] [PubMed] [Google Scholar]
- Oyama T, Kawamoto T, Mizoue T, Yasumoto K, Kodama Y, Mitsudomi T. N-acetylation polymorphism in patients with lung cancer and its association with p53 gene mutation. Anticancer Res. 1997;17:577–581. [PubMed] [Google Scholar]
- Roberts-Thomson IC, Butler WJ, Ryan P. Meat, metabolic genotypes and risk for colorectal cancer. Eur J Cancer Prev. 1999;8:207–211. doi: 10.1097/00008469-199906000-00008. [DOI] [PubMed] [Google Scholar]
- Seow A, Zhao B, Poh WT, Teh M, Eng P, Wang YT, Tan WC, Lee EJ, Lee HP. NAT2 slow acetylator genotype is associated with increased risk of lung cancer among non-smoking Chinese women in Singapore. Carcinogenesis. 1999;20:1877–1881. doi: 10.1093/carcin/20.9.1877. [DOI] [PubMed] [Google Scholar]
- Shin A, Kim J. Effect of meat intake by genetic polymorphisms on colorectal neoplasia susceptibility. Asian Pac J Cancer Prev. 2010;11:281–287. [PubMed] [Google Scholar]
- Sorensen M, Autrup H, Olsen A, Tjonneland A, Overvad K, Raaschou-Nielsen O. Genetic polymorphisms in CYP1B1, GSTA1, NQO1 and NAT2 and the risk of lung cancer. Cancer Lett. 2005;221:185–190. doi: 10.1016/j.canlet.2004.11.012. [DOI] [PubMed] [Google Scholar]
- Tamer L, Ercan B, Ates NA, Degirmenci U, Unlu A, Ates C, Dirlik M, Atik U. N-acetyltransferase 2 gene polymorphism in patients with colorectal carcinoma. Cell Biochem Funct. 2006;24:131–135. doi: 10.1002/cbf.1191. [DOI] [PubMed] [Google Scholar]
- Tanira MO, Simsek M, Al Balushi K, Al Lawatia K, Al Barawani H, Bayoumi R. Distribution of arylamine N-acetyltransferase 2 (NAT2) genotypes among Omanis. SQU J Scient Res Med Sci. 2003;5:9–14. [PMC free article] [PubMed] [Google Scholar]
- Vineis P. Cancer as an evolutionary process at the cell level: An epidemiological perspective. Carcinogenesis. 2003;24:1–6. doi: 10.1093/carcin/24.1.1. [DOI] [PubMed] [Google Scholar]
- Windmill KF, Gaedigk A, Hall PM, Samaratunga H, Grant DM, McManus ME. Localization of N-acetyltransferases NAT1 and NAT2 in human tissues. Toxicol Sci. 2000;54:19–29. doi: 10.1093/toxsci/54.1.19. [DOI] [PubMed] [Google Scholar]
- Woodhouse NM, Qureshi MM, Bastaki SMA, Patel M, Abdulrazzaq Y, Bayoumi R. Polymorphic N-acetyltransferase (NAT2) genotyping of Emiratis. Pharmacogenetics. 1997;7:73–82. doi: 10.1097/00008571-199702000-00010. [DOI] [PubMed] [Google Scholar]
- Osawa Y, Osawa K, Miyaishi A, Higuchi M, Tsutou A, Matsumura S, Tabuchi Y, Tsubota N, Takahashi J. NAT2 and CYP1A2 polymorphisms and lung cancer risk in relation to smoking status. Asian Pac J Cancer Prev. 2007;8:103–108. [PubMed] [Google Scholar]
- Ye Z, Parry JM. Meta-analysis of 20 case-control studies on the N-acetyltransferase 2 acetylation status and colorectal cancer risk. Med Sci Monit. 2002;8:CR558–565. [PubMed] [Google Scholar]
- Zhou W, Liu G, Thurston SW, Xu LL, Miller DP, Wain JC, Lynch TJ, Su L, Christiani DC. Genetic polymorphisms in N-acetyltransferase-2 and microsomal epoxide hydrolyase, cummulative cigarette smoking and lung cancer. Cancer Epidemiol Biomarkers Prev. 2002;11:15–21. [PubMed] [Google Scholar]
Internet Resources
- Tarawneh M, Nimri O, Arqoub K, Zaghal M. Jordan Cancer Registry, Ministry of health; 2009. Cancer incidence in Jordan 2009. http://www.moh.gov.jo (January 15, 2012). [Google Scholar]