Abstract
Background
The disease burden of patients with severe aortic stenosis is not often explored, while the incidence is increasing and many patients who have an indication for aortic valve replacement are not referred for surgery. We studied the quality of life of 191 patients with severe aortic stenosis, hypothesising that symptomatic patients have a far worse quality of life than the general population, which could enforce the indication for surgery.
Methods
The SF-36v2 Health Survey was completed by 191 consecutive patients with symptomatic or asymptomatic severe aortic stenosis.
Results
Asymptomatic patients (n = 59) had health scores comparable with the general Dutch population but symptomatic patients (n = 132) scored significantly lower across different age categories. Physical functioning, general health and vitality were impaired, as well as social functioning and emotional well-being. There was no relation between degree of stenosis and physical or mental health scores.
Conclusions
Both physical and emotional problems have a major impact on normal daily life and social functioning of symptomatic patients with severe aortic stenosis, regardless of age. If the aortic stenosis is above the ‘severe’ threshold, the degree of stenosis does not predict disease burden. These results encourage to reconsider a conservative approach in symptomatic patients with severe aortic stenosis. Using the SF-36v2 Health Survey together with this study, an individual patient’s quality of life profile can be assessed and compared with the patient group or with the general population. This can assist in decision making for the individual patient.
Keywords: Aortic valve stenosis, Heart surgery, Quality of life, SF-36, Aortic valve replacement
Introduction
Degenerative aortic stenosis is the most common valvular heart disease in developed countries and represents a growing health problem. Medical therapy does not slow the progression of severe aortic stenosis nor has it proven to reduce major adverse cardiac events; the only effective treatment is replacement of the aortic valve [1–3]. Surgical techniques and postoperative care have improved over the years and even patients with advanced age and comorbidities can be operated on relatively safely [4, 5]. Recently, the indications for transcatheter valve implantations have been evaluated, which now form a treatment option in patients with high operative risk [6, 7].
The guidelines of both the American Heart Association / American College of Cardiology and the European Society of Cardiology on the management of patients with valvular heart disease recommend prompt aortic valve replacement (AVR) once symptoms occur in patients with severe aortic stenosis [6, 8, 9]. Nonetheless, several studies show that for various reasons many patients who have an indication for aortic valve replacement are denied surgery [10–13].
Although some literature is available on the functional status and quality of life (QoL) of (elderly) patients after AVR, more high-quality studies are needed [14, 15]. Even less is known about the QoL of patients in whom the decision to operate is yet to be considered. Classical symptoms of aortic stenosis are dyspnoea, angina and syncope, and although the severity of symptoms can be used as a rough surrogate for the QoL, the impact of symptoms on daily life and the resulting disease burden remain unknown. The New York Heart Association (NYHA) classification is a functional measurement of physical performance or pain. It does not take social and emotional aspects into account and only roughly reflects one’s current health status but certainly not one’s desired health status or disease burden. Furthermore, physicians sometimes fail to recognise the functional disability of their patients [16]. An underestimation by the treating physician of the impact of symptoms on a patient’s QoL might be one of the reasons why so many symptomatic patients with severe aortic stenosis are not referred for surgery. If these patients indeed present with a low QoL and better evidence about this burden of disease could be presented, there would be an additional argument to follow the clinical guidelines more strictly.
This paper presents the results of the Short Form-36v2™ Health Survey (SF-36v2™) in patients with severe aortic stenosis compared with the general population in order to investigate if, and to what extent, patients experience impairment of their daily life. We hypothesised that in symptomatic patients QoL is far worse than in the general population, both in younger and elderly patients, which could enforce the indication for surgery. Further we hypothesised that echocardiographic parameters are not good indicators of disease burden, at least not in our patient group in whom the degree of stenosis is severe.
Methods
Patients
This study is part of a recently published multi-centre prospective cohort study among patients with severe aortic stenosis in the Rotterdam area (the Netherlands) between July 2006 and April 2009 [17]. In short, patients with severe aortic stenosis were recruited from the echocardiography laboratories of the outpatient clinics of seven local hospitals and all consecutive patients who provided written informed consent were included, regardless of whether they were referred for surgery or not. The study protocol was approved by the institutional ethics committee (MEC 2006–066).
Methods
Patients were invited for a personal assessment by the principal investigators (MvG, H.H). This assessment included an echocardiogram according to a specific study protocol focused on the aortic valve, recording of patient characteristics, NYHA class, medication and a calculation of anticipated operative mortality -for descriptive purposes only-using both the EuroSCORE model and the STS risk model (www.euroscore.org, www.sts.org). While establishing NYHA class, the investigators were blinded for the results of the health survey.
The QoL assessment was done by means of the SF-36v2™ Health Survey according to the instructions given by Ware et al. regarding data collection, scoring, interpretation and validation [18]. To allow for comparison of burden between the study patients and the general population we used the paper presented by Aaronson et al. in 1998 [19]. They took a sample of the general Dutch population, subdivided into different age categories, and generated normative SF-36® Health Survey data for use in the Netherlands. Our study population was therefore subdivided into the same age categories.
The SF-36v2™ Health Survey is an evolution of the SF-36® Health Survey and consists of 36 scale-rated health-related questions, grouped into eight multi-item domains which are not disease-specific and which measure functioning in different aspects of daily life: ‘Physical Functioning’, physical health related to age- and role-specific activities termed ‘Role Physical’, ‘Bodily Pain’, ‘General Health’, ‘Vitality’, ‘Social Functioning’, personal feelings of performance in age- and role-specific activities termed ‘Role Emotional’, and ‘Mental Health’. The eight domains form two main components: the ‘Physical’ and ‘Mental Component Summary’. The raw SF-36 scores given by Aaronson et al. are converted into a norm-based score from 0 to 100 in which 50 represents the mean score of the general population and 10 points on the scale correspond to 1 standard deviation (SD) [19].
Statistical analyses
For the statistical analyses SPSS 13.0.1 software was used (SPSS Inc. 2001). Continuous variables are displayed as means ± SD if normally distributed, skewed distributed variables as median with interquartile range. Categorical variables are displayed as proportions. One-sided Student’s T tests were used for comparisons of health scores of patient groups to the general population. A p-value below 0.05 was considered significant.
Results
We identified 459 patients with severe aortic stenosis; 268 of these patients (mean age 76 ± 14 years) declined participation (n = 185), had an operation scheduled (n = 65) or died (n = 18) before they could participate in the study. Reasons to refuse participation were most often high age and severe disability resulting in personal logistic problems or perceived high burden (data not shown). A total of 191 patients (mean age 70.6 years) agreed to participate. Table 1 shows their characteristics.
Table 1.
Patient characteristics
| Patient characteristics | Total patient group | Symptomatic patients |
|---|---|---|
| n = 191 | n = 132 | |
| Age (median, interquartile range, in years) | 72.6 (63.7–78.6) | 74.0 (64.4–79.2) |
| Age category | ||
| ≤40 | 4 (2 %) | 3 (2 %) |
| 41–60 | 28 (15 %) | 18 (14 %) |
| 61–70 | 44 (23 %) | 25 (19 %) |
| >70 | 115 (60 %) | 86 (65 %) |
| Male sex | 119 (62 %) | 75 (57 %) |
| NYHA class | ||
| I | 59 (31 %) | Not applicable |
| II | 73 (38 %) | 73 (55 %) |
| III | 49 (26 %) | 49 (37 %) |
| IV | 10 (5 %) | 10 (8 %) |
| Sort of symptom (%) | ||
| Only dyspnoea | 46.2 | |
| Only angina | 4.5 | |
| Only syncope | 3.8 | |
| Combination | 45.5 | |
| Cardiovascular history (%) | ||
| Diabetes mellitus | 20 | 19 |
| Hypertension | 52 | 54 |
| Dyslipidaemia | 49 | 49 |
| Chronic obstructive pulmonary disease | 17 | 20 |
| Renal failure | 7 | 9 |
| Peripheral vascular disease | 13 | 15 |
| Cerebrovascular accident (residual neurological deficit) | 19 | 18 |
| Previous coronary artery bypass grafting | 6 | 8 |
| Logistic EuroSCORE (median, interquartile range) | 5.4 (3.1–8.2) | 6.2 (3.9–9.6) |
| STS score (median, interquartile range) | 4.5 (2.8–7.6) | 5.1 (3.3–8.0) |
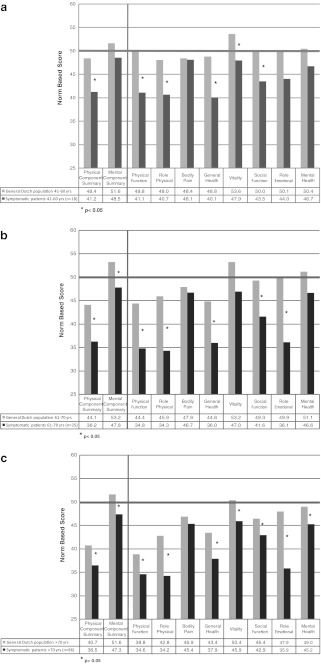
Figure 1a, b and c display the results for the symptomatic patients versus the general Dutch population in three age groups. In each age category almost all health domains were scored significantly lower than the general Dutch population except ‘Bodily Pain’. More importantly, in most health domains the differences compared with the general population were considerable. Table 2 gives the exact norm-based scores and standard deviations of each group compared with the general Dutch population.
Fig. 1.
a: Quality of life of symptomatic patients with severe aortic stenosis (AS) aged 41–60 years (n = 18) versus the general Dutch population aged 41–60 years *p < 0.05. b: Quality of life of symptomatic patients with severe aortic stenosis (AS) aged 61–70 years (n = 25) versus the general Dutch population aged 61–70 years *p < 0.05. c: Quality of life of symptomatic patients with severe aortic stenosis (AS) aged >70 years (n = 86) versus the general Dutch population aged >70 years *p < 0.05
Table 2.
Norm-based scores of symptomatic patients with severe aortic stenosis and the general Dutch population
| Health domain | Norm-based score | Norm-based score | ||||
|---|---|---|---|---|---|---|
| Symptomatic patients with severe aortic stenosis | General Dutch populationa | |||||
| 41–60 years | 61–70 years | >70 years | 41–60 years | 61–70 years | >70 years | |
| n = 18 | n = 25 | n = 86 | ||||
| Physical component summary | 41.2 ± 9.9 | 36.2 ± 9.7 | 36.5 ± 9.8 | 48.4 | 44.1 | 40.7 |
| Mental component summary | 48.5 ± 9.9 | 47.8 ± 10.2 | 47.3 ± 12.7 | 51.6 | 53.2 | 51.6 |
| Physical function | 41.1 ± 10.1 | 34.8 ± 10.1 | 34.6 ± 11.6 | 49.8 | 44.4 | 38.8 |
| Role physical | 40.7 ± 10.5 | 34.3 ± 10.9 | 34.2 ± 11.1 | 48.0 | 45.9 | 42.8 |
| Bodily pain | 48.1 ± 10.8 | 46.7 ± 12.3 | 45.4 ± 12.3 | 48.4 | 47.9 | 46.9 |
| General health | 40.1 ± 8.1 | 36.0 ± 8.6 | 37.9 ± 9.0 | 48.8 | 44.8 | 43.4 |
| Vitality | 47.9 ± 10.2 | 47.0 ± 9.7 | 45.9 ± 12.1 | 53.6 | 53.2 | 50.4 |
| Social function | 43.5 ± 10.6 | 41.6 ± 12.1 | 42.9 ± 13.7 | 50.0 | 49.3 | 46.4 |
| Role emotional | 44.0 ± 13.9 | 36.1 ± 15.0 | 35.9 ± 15.3 | 50.1 | 49.9 | 47.9 |
| Mental health | 46.7 ± 9.8 | 46.6 ± 11.1 | 45.2 ± 14.4 | 50.4 | 51.1 | 49.0 |
aNorm-Based Score calculated based on the paper by Aaronson et al. [19]
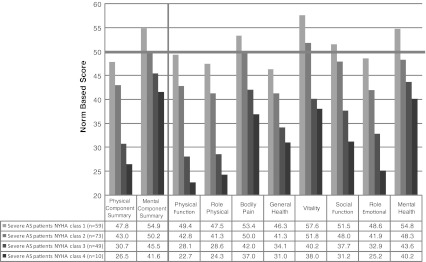
Figure 2 shows that QoL outcomes in all domains are related to the NYHA classification. Asymptomatic patients showed a trend towards high scores in most domains compared with the general population, certainly given the higher mean age of the patients (71 versus 47 years). Patients in NYHA class II had lower scores on the ‘Physical Function’, ‘Role Physical’, ‘General Health’ and ‘Role Emotional’ scales. Patients in NYHA class III and IV had lower scores on all scales, and the differences compared with the general population were large.
Fig. 2.
Quality of life of patients with severe aortic stenosis (AS) according to symptomatic status
Echocardiographic measurements indicating stenosis severity were not related to either physical or mental health scores (data not shown).
Discussion
Interpretation and discussion of main results
Quality of life decreases with increasing age both in the general population and in symptomatic severe aortic stenosis patients (Fig. 1a, b and c). However, the key point is that the differences between the general population and the symptomatic patients are large and remain significant for most health domains across all the three age groups we studied.
While angina is one of the classical symptoms of aortic stenosis, it is notable that ‘Bodily Pain’ was scored as almost normal, suggesting that pain itself only plays a modest role. The low scores on the ‘Role Physical’ domain indicate that patients do have severe physical constraints by dyspnoea or fatigue.
Not only the physical domains but also the mental health scores show large differences compared with normal. Figure 1b and c show that among patients aged over 60 years, the largest difference with the general population is observed in the ‘Role Emotional’ scale, meaning patients suffer from anxiety or a depressed state of mind affecting daily activities. Also the ‘Social Function’, ‘Vitality’ and ‘General Health’ scores indicate patients lack energy and have a negative view on their health, hampering social contact.
There was no relation between stenosis severity and physical or mental QoL in our patient cohort. Thus, whenever the aortic stenosis is above the ‘severe’ threshold, ‘objective’ measures of valve function do not correlate to disease burden. Since we only studied the ‘severe’ category, a relation between disease burden and stenosis severity in mild or moderate aortic stenosis cannot be ruled out.
We did demonstrate that scores of the SF-36v2™ correspond well with the severity of symptoms according to NYHA classification (Fig. 2). Although asymptomatic patients have a normal health perception, patients in NYHA class II -thus having only ‘mild’ symptoms- clearly experience a lower QoL. With the increase of the severity of the symptoms, scores are lower on both the physical and mental part of the survey. This is what one would expect and indicates that the SF-36v2™ is a valid measure of QoL in this patient population.
Policy implication
AVR is recommended both by American and European guidelines in symptomatic patients with severe aortic stenosis because even elderly patients can be operated on with acceptable risks and can expect improvement in functional class and survival compared with non-operated patients [4–6, 8, 9, 14, 20–22]. Still, 30 to 60 % of them do not undergo AVR [10, 12, 20, 23, 24]. Exercise testing is highly underused and downgraded from a class 2a to a 2b recommendation in the ACC/AHA guidelines, although it is reported to elicit symptoms in approximately 37 % of patients with aortic stenosis who were previously regarded as ‘asymptomatic’ [8, 25, 26]. Therefore, the proportion of patients who would deserve operative treatment could even be underestimated. Years ago it was already shown that doctors have difficulty in recognising functional disability in patients -not so much the symptoms themselves- and one could speculate this is even more true for emotional impairment [16]. Although we are unable to draw any conclusions based on the results of the current study, one could hypothesise that underestimating the impact of symptoms represents another cause of underestimating the need for treatment. Given the highly conservative approach towards patients with symptomatic severe aortic stenosis, we feel that this burden should receive more attention.
Quality of life is of utmost importance for a patient, yet there is hardly any literature on this subject in patients with severe aortic stenosis. Although some retrospective studies report on functional status and QoL in patients after AVR, they are often troubled by several limitations [5, 14, 15, 27]. Furthermore, these studies used patients with aortic stenosis who were referred (selected) for surgery. The effect of AVR on QoL among patients with severe aortic stenosis is discussed in the companion paper [28]. Importantly, in our current study we focussed not on the QoL of AVR selected patients before or after surgery, but on the quality of life when the decision to operate or not is yet to be made. Therefore these results can also be used for decision making in the individual patient. A patient could fill in a survey, online or on paper (www.qualitymetric.com), and the cardiologist or heart team could then compare these results with the general population or with similar patients (Fig. 2a, b, c), and use this information in deciding whether or not to advise AVR.
Limitations
Although enrolment from the outpatient cardiology echocardiography departments was encouraged, some patients may not have been identified and also a substantial number of patients declined participation. Mostly these patients were the elderly, or the more sick patients for whom an extra study trip to the hospital was unfeasible. Therefore, it is likely that we even underestimated the magnitude of quality-of-life impairment in the total patient population with symptomatic severe aortic stenosis and are only able to present the tip of the iceberg.
A limitation of using the SF-36v2™ survey could be the number of questions. This problem may be improved by easier, but often less specific, surveys, such as the EuroQOL survey (www.euroqol.org).
Conclusions
Our results encourage to reconsider a conservative approach in symptomatic patients with severe aortic stenosis. If the aortic stenosis is above the ‘severe’ threshold, the degree of stenosis does not predict disease burden. This study provides a quantification of this burden, especially in symptomatic patients: even minor symptoms have a major impact on patient well-being and result in a strongly impaired QoL compared with the general population. Not only do physical complaints affect daily life to a great extent, patients also suffer from emotional problems hampering normal daily activities and social functioning.
When considering to send a patient for AVR or to treat conservatively, one should not only consider the operative risks and the lifespan gained after AVR, but also the current state of the patient both physically and mentally. Using the SF-36v2™ Health Survey together with this study, an individual patient’s QoL profile can be assessed and compared with the patient group or with the general population. This can assist in decision making for the individual patient.
Acknowledgments
The authors would like to thank the patients, cardiologists, echo laboratory staff and secretaries of the following hospitals for their kind cooperation: Havenziekenhuis, Rotterdam; St. Franciscus Gasthuis, Rotterdam; IJsselland Hospital, Capelle aan den IJssel; Vlietland Hospital, Vlaardingen; Albert Schweitzer Hospital, Dordrecht; Medisch Centrum Rijnmond Zuid, Rotterdam; and Erasmus University Medical Center, Rotterdam.
Disclosures
None of the authors have any competing interests.
Footnotes
The questions can be answered after the article has been published in print. You have to log in to: www.cvoi.nl.
References
- 1.Chan KL, Teo K, Dumesnil JG, et al. Effect of Lipid lowering with rosuvastatin on progression of aortic stenosis: results of the aortic stenosis progression observation: measuring effects of rosuvastatin (ASTRONOMER) trial. Circulation. 2010;121(2):306–14. doi: 10.1161/CIRCULATIONAHA.109.900027. [DOI] [PubMed] [Google Scholar]
- 2.Cowell SJ, Newby DE, Prescott RJ, et al. A randomized trial of intensive lipid-lowering therapy in calcific aortic stenosis. N Engl J Med. 2005;352(23):2389–97. doi: 10.1056/NEJMoa043876. [DOI] [PubMed] [Google Scholar]
- 3.Rossebo AB, Pedersen TR, Boman K, et al. Intensive lipid lowering with simvastatin and ezetimibe in aortic stenosis. N Engl J Med. 2008;359(13):1343–56. doi: 10.1056/NEJMoa0804602. [DOI] [PubMed] [Google Scholar]
- 4.Melby SJ, Zierer A, Kaiser SP, et al. Aortic valve replacement in octogenarians: risk factors for early and late mortality. Ann Thorac Surg. 2007;83(5):1651–6. doi: 10.1016/j.athoracsur.2006.09.068. [DOI] [PubMed] [Google Scholar]
- 5.Kolh P, Kerzmann A, Honore C, et al. Aortic valve surgery in octogenarians: predictive factors for operative and long-term results. Eur J Cardiothorac Surg. 2007;31(4):600–6. doi: 10.1016/j.ejcts.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 6.Vahanian A, Alfieri O, Andreotti F, et al. Guidelines on the management of valvular heart disease (version 2012): the joint task force on the management of valvular heart disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2012. [DOI] [PubMed]
- 7.Lefevre T, Kappetein AP, Wolner E, et al. One year follow-up of the multi-centre European PARTNER transcatheter heart valve study. Eur Heart J. 2011;32(2):148–57. doi: 10.1093/eurheartj/ehq427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bonow RO, Carabello BA, Kanu C, et al. ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): developed in collaboration with the Society of Cardiovascular Anesthesiologists: endorsed by the Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons. Circulation. 2006;114(5):e84–231. doi: 10.1161/CIRCULATIONAHA.106.176857. [DOI] [PubMed] [Google Scholar]
- 9.Vahanian A, Baumgartner H, Bax J, et al. Guidelines on the management of valvular heart disease: the task force on the management of valvular heart disease of the European Society of Cardiology. Eur Heart J. 2007;28(2):230–68. doi: 10.1093/eurheartj/ehm354. [DOI] [PubMed] [Google Scholar]
- 10.Geldorp MW, Gameren M, Kappetein AP, et al. Therapeutic decisions for patients with symptomatic severe aortic stenosis: room for improvement? Eur J Cardiothorac Surg. 2009;35(6):953–7. doi: 10.1016/j.ejcts.2009.01.043. [DOI] [PubMed] [Google Scholar]
- 11.Charlson E, Legedza AT, Hamel MB. Decision-making and outcomes in severe symptomatic aortic stenosis. J Heart Valve Dis. 2006;15(3):312–21. [PubMed] [Google Scholar]
- 12.Iung B, Cachier A, Baron G, et al. Decision-making in elderly patients with severe aortic stenosis: why are so many denied surgery? Eur Heart J. 2005;26(24):2714–20. doi: 10.1093/eurheartj/ehi471. [DOI] [PubMed] [Google Scholar]
- 13.Bouma BJ, Meulen JH, Brink RB, et al. Variability in treatment advice for elderly patients with aortic stenosis: a nationwide survey in The Netherlands. Heart. 2001;85(2):196–201. doi: 10.1136/heart.85.2.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sundt TM, Bailey MS, Moon MR, et al. Quality of life after aortic valve replacement at the age of >80 years. Circulation. 2000;102(19 Suppl 3):III70–4. doi: 10.1161/01.cir.102.suppl_3.iii-70. [DOI] [PubMed] [Google Scholar]
- 15.Noyez L, Jager MJ, Markou AL. Quality of life after cardiac surgery: underresearched research. Interact Cardiovasc Thorac Surg. 2011;13(5):511–5. doi: 10.1510/icvts.2011.276311. [DOI] [PubMed] [Google Scholar]
- 16.Calkins DR, Rubenstein LV, Cleary PD, et al. Failure of physicians to recognize functional disability in ambulatory patients. Ann Intern Med. 1991;114(6):451–4. doi: 10.7326/0003-4819-114-6-451. [DOI] [PubMed] [Google Scholar]
- 17.Heuvelman HJ, van Geldorp MW, Kappetein AP, et al. Clinical course of patients diagnosed with severe aortic stenosis in the Rotterdam area: insights from the AVARIJN study. Neth Heart J. 2012. doi:10.1007/s12471-012-0309-3 [DOI] [PMC free article] [PubMed]
- 18.Ware JE, Jr, Kosinski M, Bjorner JB, et al. User’s manual for the SF-36v2 TM health survey. 2. Lincoln: Quality Metric; 2007. [Google Scholar]
- 19.Aaronson NK, Muller M, Cohen PD, et al. Translation, validation, and norming of the Dutch language version of the SF-36 Health Survey in community and chronic disease populations. J Clin Epidemiol. 1998;51(11):1055–68. doi: 10.1016/S0895-4356(98)00097-3. [DOI] [PubMed] [Google Scholar]
- 20.Bouma BJ, Brink RB, Meulen JH, et al. To operate or not on elderly patients with aortic stenosis: the decision and its consequences. Heart. 1999;82(2):143–8. doi: 10.1136/hrt.82.2.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu Y, Jin R, Gao G, et al. Cost-effectiveness of aortic valve replacement in the elderly: an introductory study. J Thorac Cardiovasc Surg. 2007;133(3):608–13. doi: 10.1016/j.jtcvs.2006.10.044. [DOI] [PubMed] [Google Scholar]
- 22.Wu Y, Grunkemeier GL, Starr A. The value of aortic valve replacement in elderly patients: an economic analysis. J Thorac Cardiovasc Surg. 2007;133(3):603–7. doi: 10.1016/j.jtcvs.2006.08.042. [DOI] [PubMed] [Google Scholar]
- 23.Bach DS, Cimino N, Deeb GM. Unoperated patients with severe aortic stenosis. J Am Coll Cardiol. 2007;50(20):2018–9. doi: 10.1016/j.jacc.2007.08.011. [DOI] [PubMed] [Google Scholar]
- 24.Varadarajan P, Kapoor N, Bansal RC, et al. Clinical profile and natural history of 453 nonsurgically managed patients with severe aortic stenosis. Ann Thorac Surg. 2006;82(6):2111–5. doi: 10.1016/j.athoracsur.2006.07.048. [DOI] [PubMed] [Google Scholar]
- 25.Iung B, Baron G, Butchart EG, et al. A prospective survey of patients with valvular heart disease in Europe: the euro heart survey on Valvular Heart Disease. Eur Heart J. 2003;24(13):1231–43. doi: 10.1016/S0195-668X(03)00201-X. [DOI] [PubMed] [Google Scholar]
- 26.Das P, Rimington H, Chambers J. Exercise testing to stratify risk in aortic stenosis. Eur Heart J. 2005;26(13):1309–13. doi: 10.1093/eurheartj/ehi250. [DOI] [PubMed] [Google Scholar]
- 27.Sjogren J, Thulin LI. Quality of life in the very elderly after cardiac surgery: a comparison of SF-36 between long-term survivors and an age-matched population. Gerontology. 2004;50(6):407–10. doi: 10.1159/000080179. [DOI] [PubMed] [Google Scholar]
- 28.van Geldorp MWA, Heuvelman HJ, Kappetein AP, et al. The effect of aortic valve replacement on quality of life in symptomatic patients with severe aortic stenosis. Neth Heart J. 2013;21. doi:10.1007/s12471-012-0362-y [DOI] [PMC free article] [PubMed]