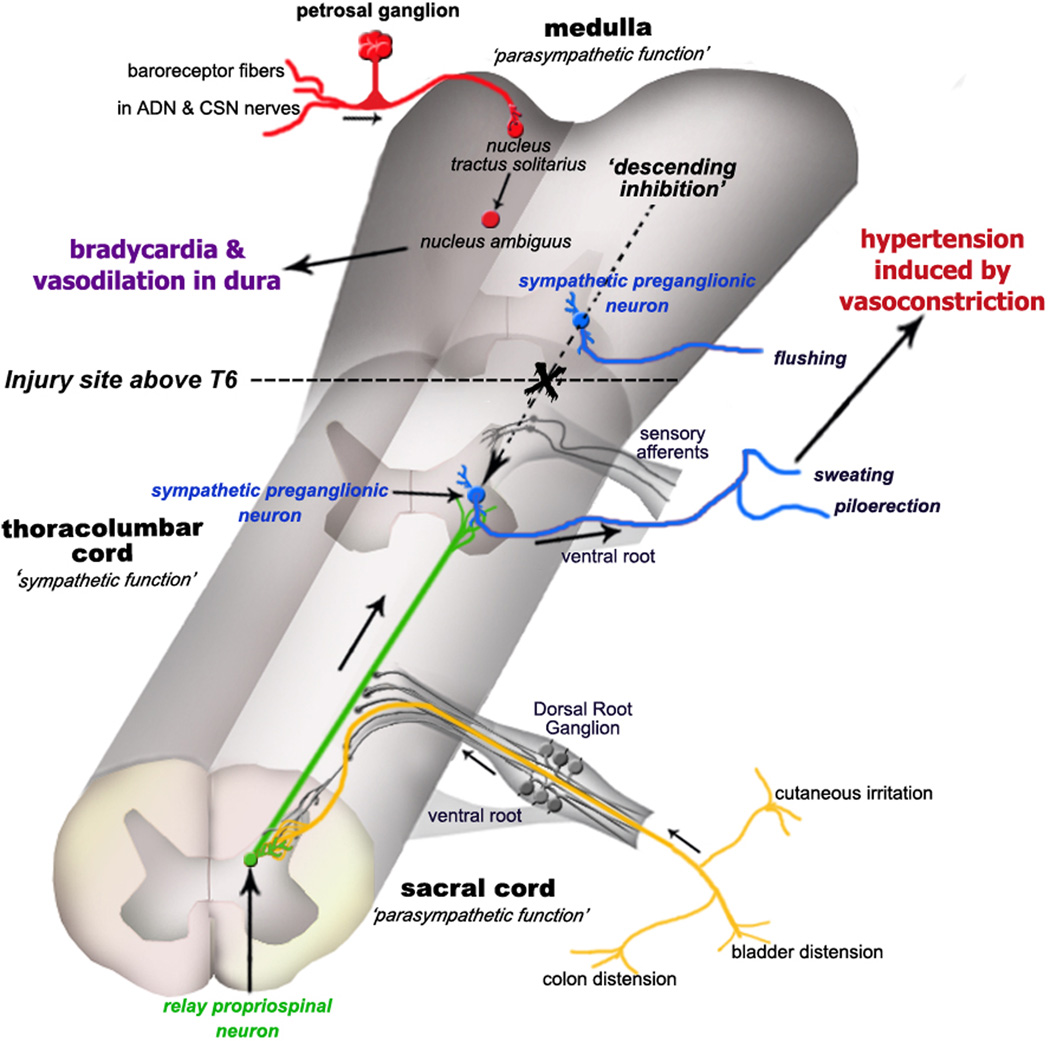
Figure 5.
Schematic illustration depicting the etiology of autonomic dysreflexia evoked by pelvic visceral distension and other stimuli. Following complete spinal cord injury above the T6 level, sympathetic preganglionic neurons (blue) are released from descending medullo-spinal control (dashed arrow) and autonomic spinal reflexes are rendered hyperactive. Consequently, pelvic visceral sensory input (yellow) is relayed by propriospinal neurons (green) projecting from the dorsal gray commissure at the lumbosacral level to sympathetic preganglionic neurons and/or sympathetically-correlated interneurons located in the thoracolumbar cord (blue). Post-traumatic C-fiber sprouting into the lumbosacral cord (yellow) further amplifies the central signals (green) to elicit hypertension, ultimately causing profound peripheral vasoconstriction of splanchnic, muscle and cutaneous vascular beds. Subsequent stimulation of aortic depressor nerve (ADN) and carotid sinus nerve (CSN) baroreceptor afferents of the petrosal ganglion (red) is conveyed to the nucleus tractus solitarius that elicits bradycardia via activation of the nucleus ambiguus. Note that flushing is likely the result of inhibition of skin vasoconstrictor preganglionic neurons above the lesion by the baroreceptor reflex, and not due to the activation of sympathetic preganglionic neurons below the lesion by the dysreflexia-inducing stimulus.