Abstract
AIM
To evaluate postoperative visual acuity and contrast sensitivity results following deep anterior lamellar keratoplasty (DALK) and penetrating keratoplasty (PK) in patients with keratoconus (KC).
METHODS
All the patients' records with KC who had PK or DALK surgery between May 2010 and May 2011 were retrospectively reviewed. Sixty patients who underwent successful corneal transplantation for KC: 30 eyes underwent DALK and 30 eyes underwent PK were included in this study. Preoperative and postoperative mean logarithm of the minimum angle of resolution (logMAR) uncorrected visual acuity (UCVA), logMAR best spectacle-corrected visual acuity (BSCVA) and intraocular pressure (IOP) were evaluated. Contrast sensitivity tests (CS) were done preoperative and 2 months after all sutures had removed. All surgeries were performed under regional anesthesia (retrobulbar anesthesia) by 1 surgeon (B.K.) who was experienced in penetrating and lamellar keratoplasty techniques.
RESULTS
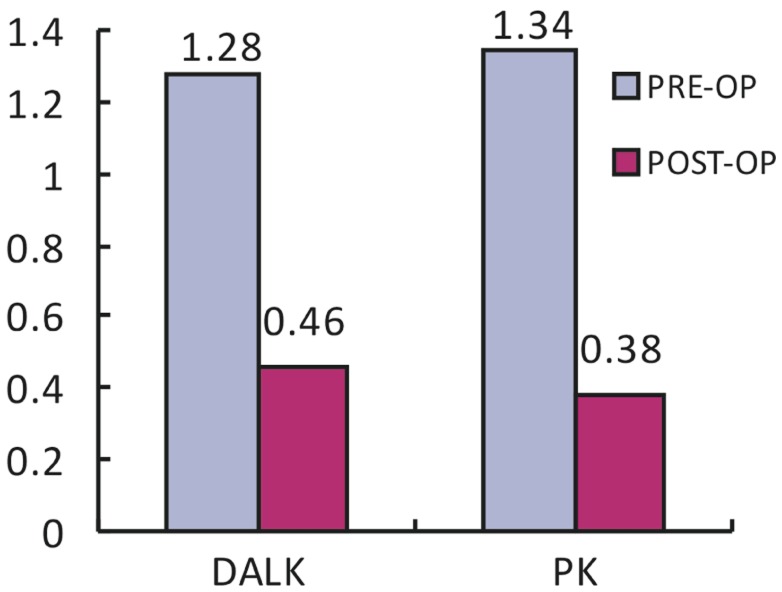
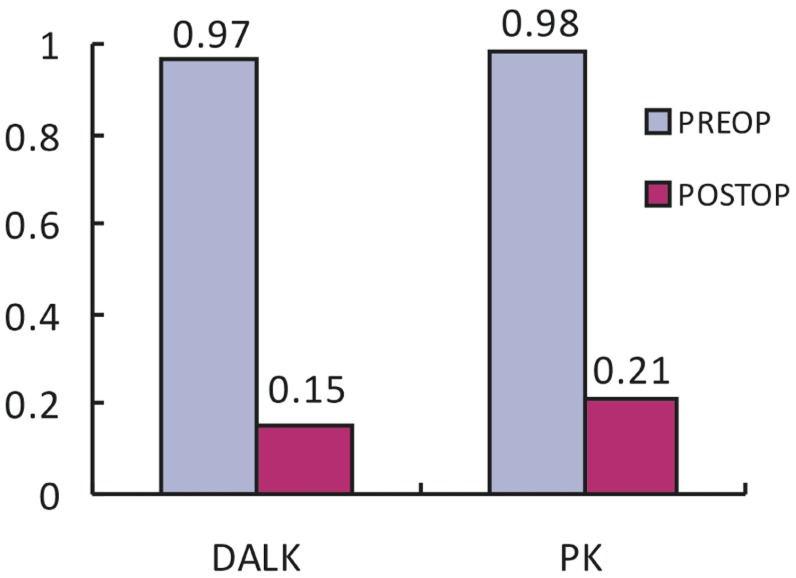
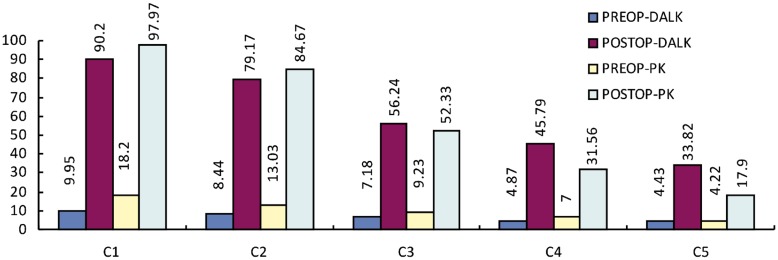
The mean age of the DALK group was 29.67±4.95 (range 18-40) years and the PK group was 28.7±3.53 (range 18-39) years. Preoperatively there was no significant difference in the logMAR UCVA, logMAR BSCVA and IOP between the DALK (1.281±0.56; 0.97±0.85; 12.07±2.12mmHg) and PK (1.34±0.21; 0.98±0.21; 13±2.12mmHg) groups. One-year after surgery there was no significant difference in the mean logMAR UCVA and IOP between the DALK (0.46±0.37; 11.73±2.1mmHg) and PK (0.38±0.21; 12±2.12mmHg) groups. The mean contrast sensitivity was evaluated by CC-100 Topcon LCD at 1.5, 2.52, 4.23, 7.10 and 11.91 cycles per degree (cs/deg) spatial frequencies before and 2 months after the all sutures had removed.
CONCLUSION
All patients with keratoconus in both DALK and PK groups performed good visual function postoperatively. The mean contrast sensitivity increased considerably at all spatial frequencies compared with preoperative levels in the DALK and PK groups. The mean post-operative evaluation of contrast sensitivity measurements was not significantly different between the two groups.
Keywords: contrast sensitivity, keratoconus, corneal transplantation
INTRODUCTION
Keratoconus is a progressive non-inflammatory ectatic disease of the cornea[1]. Penetrating keratoplasty was the most popular surgery for advanced keratoconus in the past and it has some disadvantages like endothelial rejection[2]. Therefore, new techniques were investigated and deep anterior lamellar keratoplasty is considered as an alternative procedure which leaves the host corneal endothelium and Descemet's membrane intact. This provides the advantage of the absence of potential corneal endothelial rejection and preservation of the endothelial cells during the surgery[3]. Two procedures have similar results in terms of visual acuity and refractive error[4]. However visual acuity and refractive error alone cannot be used as a parameter for quality of vision. Therefore some other parameters must be used to evaluate. Contrast sensitivity is one of the mostly used parameter to measure visual quality[5].
The aim of present study is to compare the contrast sensitivities also visual quality of DALK and PK surgeries for keratoconus.
SUBJECTS AND METHODS
Subjects
All the patients' records with KC who had PK or DALK surgery between May 2010 and May 2011 were retrospectively reviewed. Patients that had any other ophthalmic surgery, complications during DALK or PK surgery, DALK surgeries which bare Descemet's membrane could not be created, any rejection episodes, continuous intraocular pressure increase, any concomitant ophthalmic disease, any systemic disease and who had not came to routine controls were not included in present study. Written informed consent was obtained from all participants and the study was conducted in accordance with the tenets of the Declaration of Helsinki. All patients had underwent a detailed ophthalmologic examination including best spectacle corrected visual acuity, slit lamp biomicroscopy, intraocular pressure (IOP) measurements, fundus examination with B-scan ultrasound or biomicroscopy, contrast sensitivity tests (CS) done by CC-100 Topcon LCD at 1.5, 2.52, 4.23, 7.10 and 11.91 cycles per degree (cs/deg) spatial frequencies preoperatively and postoperative 2 months after all sutures had been removed.
Methods
Surgery decision was made with the patient after informing the patient about advantages and disadvantages of the surgical procedures. All the patients had moderate to advanced keratoconus (mean K reading >52D or undetectable) and had not enough visual acuity to perform their daily activities with spectacle or contact lens correction. All the surgeries were done by 1 surgeon (B.K) who was experienced in penetrating and lamellar keratoplasty techniques.
Penetrating keratoplasty was performed under regional (retrobulbar) anesthesia. Donor corneas were punched out from the endothelial side with a Hessburg Barron donor punch (JedMed Instrument Co, St Louis, Missouri) with a diameter 0.5mm larger than that of the recipient. The recipient cornea was trephined with a Hessburg-Barron vacuum trephine (Katena Products, Denville, NJ) with a 7.5mm diameter. Removal of the cornea was completed with curved corneal scissors. Then, graft was fixed with 16 bites interrupted sutures. At the end of the surgery, corneal astigmatism was adjusted by replacing tight or loose sutures.
Deep anterior lamellar keratoplasty was performed under regional anesthesia (retrobulbar), using the big-bubble technique described by Anwar and Teichmann[6]. A Hessburg Barron (JedMed Instrument Co, St Louis, Missouri, USA) suction trephine (7.5mm) was used for partial thickness trephination of the host cornea up to 60%-80% depth. Anterior and middle stromas were removed with a crescent knife. A 30-gauge needle with 5mL filled syringe was inserted bevel down in to the midperipheral stroma and push forward 3-4mm toward the center of the cornea, parallel to the corneal plane. Air was injected with increased pressure to dissect the Descemet's membrane from stroma by forming a big bubble. After the achievement of a successful big bubble, an incision was done to the posterior stroma to reach Descemet's membrane. After remnants of posterior stromal lamellae were removed with blunt tip corneal scissors, clear Descemet's membrane was exposed. The donor cornea was cut from the endothelial side with a 0.25mm larger Barron donor punch (Katena Products, Inc, Denville, New Jersey, USA). The endothelium was stained with trypan blue and scrapped completely from the button using the technique described by Melles et al[7]. Donor cornea was placed on the recipient bed and fixed with 16 bites interrupted sutures.
After the surgeries, ofloxacin eye drop q2h and prednisolone acetate 1% q2h had started postoperative 1st day routinely. Ofloxacin eye drops were stopped after 2 weeks in all patients and prednisolone acetate 1% was decreased to qid. After 3 months, the topical prednisolone acetate 1% was gradually tapered over a 3-month period and changed to low dose steroid (fluorometholone or loteprednol etabonate) in PK group. After 2 months, the topical prednisolone acetate 1% was gradually tapered over a 2 month period and changed to low dose steroid (fluorometholone or loteprednol etabonate) in DALK group.
Statistical Analysis
In present study, statistical analysis performed with NCSS 2007 software package. Descriptive statistical methods (mean, standard deviation), Mann-Whitney-U test for comparison of two groups, Wilcoxon test for comparison of before and after treatment results, Chi-square test for comparing qualitative data were used in evaluating the data. The results were evaluated as significant at P<0.05 values.
RESULTS
We found 60 eyes (50% DALK surgery n=30, 50% PK surgery n=30) with keratoconus, treated with DALK or PK in 16 months follow up period that cover our inclusion and exclusion criteria.
We had formed two homogenous groups that surgeries were done without any complications to compare the results. Mean age of the patients were 29.67±4.95 (18-40) years in DALK group and 28.7±3.53 (18-39) years in PK group. Difference between ages of two groups was not statistically significant (P>0.05). In DALK group 14 patients (46.6%) were male and 16 patients (53.4%) were female, in PK group 16 patients (53.4%) were male and 14 patients (46.6%) were female. Mean follow up period was 12.58±3.67 months (12-16 months).
There was no significant difference in preoperative logMAR UCVA (P=0.326), logMAR BSCVA (P=0.965) and IOP between the DALK (1.28±0.56; 0.97±0.85; 12.07±2.12mmHg) and PK (1.34±0.21; 0.98±0.21; 13±2.12mmHg) groups (P>0.05).
One-year after surgery, mean logMAR UCVA of DALK group was 0.46±0.37, logMAR BSCVA was 0.15±0.15 and IOP was 11.73±2.1mmHg. There was a statistically significant increase in postoperative UCVA and BSCVA (P<0.05).
In PK group postoperative 12 months, mean logMAR UCVA was 0.38±0.30 and logMAR BSCVA was 0.21±0.13. Mean IOP was 12.07±1.87 at 12 months surgery. Postoperative UCVA and BSCVA were higher than preoperative values. These results were statistically significant (P<0.05).
In spite of higher UCVA and BSCVA in PK group, difference between the postoperative mean logMAR UCVA (P=0.326) and logMAR BSCVA (P=0.965) of two groups were not statistically significant (P>0.05, Figures 1, 2).
Figure 1. Comparison of preoperative and postoperative mean logMAR UCVA.
Figure 2. Comparison of preoperative and postoperative mean logMAR BSCVA.
The contrast sensitivity was evaluated by CC-100 Topcon LCD at 1.5 (C1), 2.52 (C2), 4.23 (C3), 7.10 (C4) and 11.91 (C5) cycles per degree (cs/deg) spatial frequencies before surgery and 2 months after all suture had been removed. Mean suture removal time of the DALK group was 6.3 months (5.7-6.5 months) and 11.2 months (10.5-12.2 months) of the PK group. The mean preoperative and postoperative contrast sensitivity results were summarized at Figure 3. Postoperative CS measurements were better in all the patients that were included in this study. When comparing the two groups' postoperative CS results, we found that there was no statistically difference between the CS results of two groups (Figure 3, Table 1) (P>0.05).
Figure 3. Comparison of preoperative and postoperative each contrast sensitivity test.
Table 1. Comparison of contrast sensitivity.
| Sum of squares | df | Mean square | F | P | |
| Preop C1 | |||||
| Between groups | 510.056 | 1 | 510.056 | 19.274 | 0.000 |
| Within groups | 740.966 | 28 | 26.463 | ||
| Total | 1251.023 | 29 | |||
| Preop C2 | |||||
| Between groups | 158.057 | 1 | 158.057 | 9.724 | 0.004 |
| Within groups | 455.105 | 28 | 16.254 | ||
| Total | 613.162 | 29 | |||
| Preop C3 | |||||
| Between groups | 31.621 | 1 | 31.621 | 3.861 | 0.059 |
| Within groups | 229.329 | 28 | 8.190 | ||
| Total | 260.950 | 29 | |||
| Preop C4 | |||||
| Between groups | 34.133 | 1 | 34.133 | 9.842 | 0.004 |
| Within groups | 97.110 | 28 | 3.468 | ||
| Total | 131.244 | 29 | |||
| Preop C5 | |||||
| Between groups | 0.354 | 1 | 0.354 | 0.350 | 0.559 |
| Within groups | 28.340 | 28 | 1.012 | ||
| Total | 28.695 | 29 | |||
| Postop C1 | |||||
| Between groups | 452.253 | 1 | 452.253 | 0.257 | 0.616 |
| Within groups | 49194.274 | 28 | 1756.938 | ||
| Total | 49646.527 | 29 | |||
| Postop C2 | |||||
| Between groups | 226.490 | 1 | 226.490 | 0.123 | 0.729 |
| Within groups | 51745.847 | 28 | 1848.066 | ||
| Total | 51972.338 | 29 | |||
| Postop C3 | |||||
| Between groups | 115.013 | 1 | 115.013 | 0.076 | 0.785 |
| Within groups | 42598.846 | 28 | 1521.387 | ||
| Total | 42713.859 | 29 | |||
| Postop C4 | |||||
| Between groups | 1518.839 | 1 | 1518.839 | 1.273 | 0.269 |
| Within groups | 33395.561 | 28 | 1192.699 | ||
| Total | 34914.400 | 29 | |||
| Postop C5 | |||||
| Between groups | 1900.052 | 1 | 1900.052 | 1.794 | 0.191 |
| Within groups | 29650.800 | 28 | 1058.957 | ||
| Total | 31550.852 | 29 |
DISCUSSION
Lamellar surgeries have gained more popularity at last decade. Especially in DALK surgery, with increased experience, increase of visual outcome is noteworthy since the beginning. DALK surgery has the advantages over PK which are less rejection, stronger graft host junction, easier visual rehabilitation and keeping host endothelium[2]. Results were comparable with PK for keratoconus.
Bahar et al[8] stated that DALK and PK which were done for keratoconus had similar results comparing visual acuity, refractive results and complications. In their study the median BSCVA at 12 months was 20/40 in DALK group and 20/30 in PK group. The median astigmatism was 2.5D in DALK group while 2.4D in PK group. Finally they conclude that complications were comparable. In another study Kim et al[2] noted that there was no significant difference between the DALK and PK groups in terms of postoperative UCVA, BCVA and astigmatism. Moreover Cohen et al[9] also found that treatment of keratoconus with PK or DALK had similar visual outcomes, graft survival and prevalence of sight threatening complications. Similar results of different studies caused that most of the ophthalmologists accepted DALK as an alternative to PK in treating keratoconus[9]-[13]. Our visual acuity results were similar and compatible with these studies. However we also know visual acuity is not the only parameter that affects the patients' visual quality and also quality of life.
Visual acuity is not enough for measuring quality of vision and some other factors influence vision. One of the important parameters of visual quality is contrast sensitivity and also it's important for patients treated for keratoconus[14]. Silva et al[15] reported that contrast sensitivity measurements after PK and DALK were similar. They reported BSCVA in penetrating keratoplasty group was 20/30 in 7, 20/25 in 7 patients, 20/20 in 1 patient and in DALK group was 20/30 in 8, 20/25 in 7 patients. These differences were not statistically significant and there was no statistically significant difference in contrast sensitivity in any spatial frequency (1.5, 3, 6, 12, 18 cpd)[15]. Fontana et al[16] investigated the influence of graft-host interface on the quality of vision after DALK surgery. They compared the results of PK, DALK with DM baring and DALK without DM baring. They found that median logMAR BSCVA was 0.1 in PK group, 0.06 in DALK with DM baring group and 0.12 in DALK without DM baring group. They resulted that PK and DM baring DALK group had comparable results in visual acuity and also contrast sensitivity (P=0.974, P=0.408). However in DALK without DM baring group, both visual acuity and contrast sensitivity results were worse than the other groups[16]. We also evaluated the results of PK and DALK surgery that bare Descemet's membrane can be created in our study.
Fontana et al[16] and Ardjomand et al[17] stated that recipient stromal thickness was important in visual acuity and quality results. Ardjomand et al[17] emphasized that DALK surgeries with a recipient tissue more than 80µm resulted in reduction in photopic contrast sensitivity, even the results were not statistically significant. It seems that bare Descemet's membrane formation is important for the success of DALK surgery with the results of these studies. Our study supports the results in which comparison of bare Descemet's membrane DALK and PK surgeries were evaluated.
New studies investigate the difference between visual quality parameters of DALK and PK surgeries. They represent that DALK and PK groups performed compatible visual quality results in patients with keratoconus. Our study also shows the same result. The limitations of our study included the lack of investigations for higher order aberrations. However, contrast sensitivity is one of the important factors for evaluating the quality of vision that affects the comfort of the patients in their daily life. The results emphasize that not only visual results, but also the contrast sensitivity results are similar. The results of both operations showed us that these surgeries were good alternatives for each other.
REFERENCES
- 1.Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42(4):297–319. doi: 10.1016/s0039-6257(97)00119-7. [DOI] [PubMed] [Google Scholar]
- 2.Kim KH, Choi SH, Chung ES, Chung TY. Comparison of refractive changes after deep anterior lamellar keratoplasty and penetrating keratoplasty for keratoconus. Jpn J Ophthalmol. 2011;55(2):93–97. doi: 10.1007/s10384-010-0914-x. [DOI] [PubMed] [Google Scholar]
- 3.Reinhart WJ, Musch DC, Jacobs DS, Lee WB, Kaufman SC, Schtein RM. Deep anterior lamellar keratoplasty as an alternative to penetrating keratoplasty a report by american academy of ophthalmology. Ophthalmology. 2011;118(1):209–218. doi: 10.1016/j.ophtha.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 4.Javadi MA, Feizi S, Yazdani S, Mirbabaee F. Deep anterior lamellar keratoplasty versus penetrating keratoplasty for keratoconus. A clinical trial. Cornea. 2010;29(4):365–371. doi: 10.1097/ICO.0b013e3181b81b71. [DOI] [PubMed] [Google Scholar]
- 5.McLeod SD. Beyond snellen acuity: The assesment of visual function after refractive surgery. Arch Ophthalmol. 2001;119(9):1371–1373. doi: 10.1001/archopht.119.9.1371. [DOI] [PubMed] [Google Scholar]
- 6.Anwar M, Teichmann KD. Big-bubble technique to bare Descemet's membrane in anterior lamellar keratoplasty. J Cataract Refract Surg. 2002;28(3):398–403. doi: 10.1016/s0886-3350(01)01181-6. [DOI] [PubMed] [Google Scholar]
- 7.Melles GR, Lander F, Rietveld FJ, Remeijer L, Beekhuis WH, Binder PS. A new surgical technique for deep stromal anterior lamellar keratoplasty. Br J Ophthalmol. 1997;81(3):184–188. doi: 10.1136/bjo.83.3.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bahar I, Kaıserman I, Srinivasan S, Ya-Ping J, Slomovic AR, Rootman DS. Comparison of three different techniques of corneal transplantation for keratoconus. Am J Ophthalmol. 2008;146(6):905–912. doi: 10.1016/j.ajo.2008.06.034. [DOI] [PubMed] [Google Scholar]
- 9.Cohen AW, Goins KM, Sutphin JE, Wandling GR, Wagoner MD. Penetrating keratoplasty versus deep anterior lamellar keratoplasty for the treatment of keratoconus. Int Ophthalmol. 2010;30(6):675–681. doi: 10.1007/s10792-010-9393-9. [DOI] [PubMed] [Google Scholar]
- 10.Han DC, Mehta JS, Por YM, Htoon HM, Tan DT. Comparison of outcomes of lamellar keratoplasty and penetrating keratoplasty in keratoconus. Am J Ophthalmol. 2009;148(5):744–751. doi: 10.1016/j.ajo.2009.05.028. [DOI] [PubMed] [Google Scholar]
- 11.Fontana L, Parente G, Tassinari G. Clinical outcomes after deep anterior lamellar keratoplasty using the big-bubble technique in patients with keratoconus. Am J Ophthalmol. 2007;143(1):117–124. doi: 10.1016/j.ajo.2006.09.025. [DOI] [PubMed] [Google Scholar]
- 12.Watson SL, Ramsay A, Bunce C, Craig E. Comparison of deep lamellar keratoplasty and penetrating keratoplasty in patients with keratoconus. Ophthalmology. 2004;111(9):1676–1682. doi: 10.1016/j.ophtha.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 13.Jones MN, Armitage WJ, Ayliffe W, Larkin DF, Kaye SB. NHSBT Ocular Tissue Advisory Group and Contributing Ophthalmologists (OTAG Audit Study 5). Penetrating and deep anterior lamellar keratoplasty for keratoconus: a comparison of graft outcomes in the United Kingdom. Invest Ophthalmol Vis Sci. 2009;50(12):5625–5629. doi: 10.1167/iovs.09-3994. [DOI] [PubMed] [Google Scholar]
- 14.Holladay JT. Optical quality and refractive surgery. Int Ophthalmol Clin. 2003;43(2):119–136. doi: 10.1097/00004397-200343020-00012. [DOI] [PubMed] [Google Scholar]
- 15.Silva CA, Schweitzer de Oliveira E, Souza de Sena Júnior MP, Barbosa de Sousa L. Contrast sensitivity in deep anterior lamellar keratoplasty versus penetrating keratoplasty. Clinics (Sao Paulo) 2007;62(6):705–708. doi: 10.1590/s1807-59322007000600008. [DOI] [PubMed] [Google Scholar]
- 16.Fontana L, Parente G, Sincich A, Tassinari G. Influence of graft-host interface on the quality of vision after deep anterior lamellar keratoplasty in patients with keratoconus. Cornea. 2011;30(5):497–502. doi: 10.1097/ico.0b013e3181d25e4d. [DOI] [PubMed] [Google Scholar]
- 17.Ardjomand N, Hau S, McAlister JC, Bunce C, Galaretta D, Tuft SJ, Larkin DF. Quality of vision and graft thickness in deep anterior lamellar and penetrating corneal allografts. Am J Ophthalmol. 2007;143(2):228–235. doi: 10.1016/j.ajo.2006.10.043. [DOI] [PubMed] [Google Scholar]