Abstract
Purpose
Although total knee arthroplasty (TKA) is regularly associated with favorable outcomes, considerable research efforts are still underway to improve its ability to achieve a neutral postoperative mechanical axis. Patient-specific instrumentation (PSI) was introduced with this and other goals in mind. The current retrospective study was designed to determine whether PSI would lead to a hip-knee-ankle angle (HKA) within ±3° of the ideal alignment of 180°.
Methods
A long-leg x-ray of the knee was performed after an average of 3.5 months (SD, three to four months), following 124 TKAs performed by a single surgeon using PSI technology (VISIONAIRE; Smith & Nephew). In addition to HKA, the zone of the mechanical axis (ZMA; zone of the tibial base plate where the mechanical axis of the limb intersects with the tibial base plate) was analysed, with the ideal intersection occurring centrally.
Results
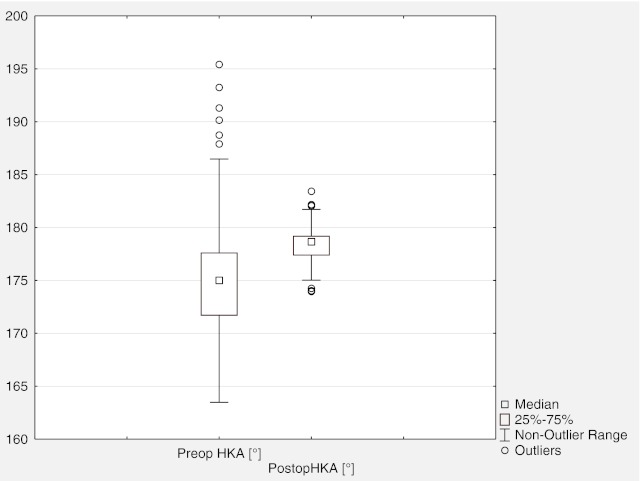
There were 100 knees (average age, 66.8 years) with follow-up data available. The average HKA changed from 175.5±5.6° preoperatively to 178.5±1.7° postoperatively. The rate of ±3° and ±5° HKA outliers was 11 % and 3 %, respectively. In terms of ZMA, the mechanical axis passed through the central third of the knee in the majority of cases (93 knees, 93 %). There were no intra-operative complications with the use of PSI.
Conclusions
The use of PSI technology was able to achieve a neutral mechanical axis on average in patients undergoing TKA. Further follow-up will be needed to ascertain the long-term impact of these findings.
Introduction
Total knee arthroplasty (TKA) is one of the most commonly performed contemporary surgeries, with a high success rate for reducing pain and improving function in arthritic knees [1]. Given the rising mean age of the global population and the associated increase in disorders of the knee, it is self-evident that an even larger number of patients will seek out this surgery in years to come [1]. As TKA nonetheless still has several limitations necessitating improvement, it is essential that research efforts continue to refine this procedure in order to avoid a concomitant increase in otherwise avoidable complications and revisions.
Incorrect positioning and malalignment of the TKA components has been cited as one of the key underlying factors leading to a variety of negative postoperative outcomes, including patient dissatisfaction, loss of thickness of polyethylene tibial bearings, eccentric loading, implant loosening, and eventual early revision [2–6]. It has been commonly accepted for decades that obtaining a postoperative alignment within the range of 0° ± 3° of the mechanical axis is optimal for reducing the occurrence of these negative outcomes [7, 8]. However, manual intramedullary/extramedullary guides have been noted to produce postoperative axes outside of this range, even when used by experienced surgeons [9, 10]. Although computer-assisted navigation has been shown to improve mechanical alignment over conventional instrumentation, it has also been associated with increased surgical times and no significant improvement in short-term clinical outcomes [10, 11]. This has prompted efforts to produce more precise surgical technology for reconstructing the mechanical axis of the knee.
Patient-specific instrumentation (PSI) represents an emerging technology in TKA that was introduced as an alternative to computer navigation and conventional instrumentation, with the key goal of improving postoperative alignment and positioning [12]. PSI uses anatomical data obtained primarily from preoperative axial computed tomography (CT) or magnetic resonance imaging (MRI) to create disposable cutting jigs individualized to the patient’s unique anatomy. One such PSI system is the VISIONAIRE (Smith & Nephew, Memphis, TN, USA), which was designed to restore a neutral postoperative mechanical axis using an MRI and a long leg x-ray. One of the coauthors previously reported this system’s superior ability to position femoral components in optimal rotational alignment during TKA in comparison with conventional instrumentation [13].
The aim of the current retrospective study was to supplement this earlier data by analysing postoperative mechanical axis in patients undergoing TKA with this technology, with the hypothesis that PSI would lead to a neutral mechanical axis on average.
Methods
This study follows the principles set forth in the Declaration of Helsinki. In Germany, where this study was conducted, retrospective epidemiological studies without personally identifiable data do not need to be sent to the ethical committee for approval.
Between October 2009 and January 2012, the senior author (C.O.T.) performed 124 TKAs (120 patients; Table 1) using VISONAIRE technology. The senior author is an experienced surgeon, who personally performs over 500 TKAs per year. All participants were required to have a diagnosis of primary osteoarthritis, to have no signs of a mediolateral instability or a massive varus/valgus deformity with a deviation of > 20°, and to be able to undergo pre-operative MRI, with no metallic hardware in close proximity to the operated knee. Additionally, they needed to be willing to wait the four to six weeks typically required for this specialized instrumentation to be prepared.
Table 1.
Baseline demographics for 120 patients (124 knees)
| Variables | |
|---|---|
| Mean age, years (SD) | 66.8 (24.4−88.3) |
| Mean BMI (SD) | 26.4 (23.9−29.2) |
| Gender (n, %) | |
| Male | 78 (65 %) |
| Female | 42 (35 %) |
| Operated side (n, %) | |
| Left | 51 (41 %) |
| Right | 73 (59 %) |
| Diagnosis (n, %) | |
| Varus OA | 90 (73 %) |
| Valgus OA | 15 (12 %) |
| Posttraumatic OA | 11 (9 %) |
| Patellofemoral OA | 8 (6 %) |
| Operative time, minutes | 52.5 (35−86) |
BMI Body mass index, OA osteoarthritis
All patients received a cemented Genesis II™ (Smith and Nephew, Memphis, TN) posterior-stabilized high-flexion prosthesis, with femoral components fabricated from an oxidized zirconium alloy (Oxinium™, Smith and Nephew, Memphis, TN), and were operated upon using a conventional medial parapatellar approach. Patients underwent a full-leg radiograph standing on both legs and a MRI pre-operatively.
The process by which the VISIONAIRE instrumentation is produced has been described in detail by the coauthor in a previous study, as well as by others [13–16]. In brief, pre-operative MRI data was processed by engineers at Smith and Nephew (Memphis, TN). In addition, full-length anterior/posterior radiographs were utilized to ascertain the current and planned mechanical axis. After review and final approval of the specifications by the surgeon, the engineers produced the tibial and femoral resection guides. These PSI jigs were then shipped to the surgeon, who attempted to attain optimal fit and positioning in accordance with the pre-operative plan and through the use of conventional landmarks. Surgical settings called for a 9-mm proximal resection and a posterior slope alignment of 3°.
Standing long-leg x-rays were performed postoperatively to ascertain all radiographic endpoints. An independent orthopaedic surgeon (K.D.) then performed radiographic measurements for the four following endpoints: (1) hip-knee-ankle angle (HKA), defined as the angle between the mechanical axis of the femur and the mechanical axis of the tibia, with both lines crossing at the centre of the knee (Fig. 1a–b); (2) zone of mechanical axis (ZMA), in which the tibial base plate is divided into three equal zones (lateral, medial, and central) and the mechanical axis (drawn from the centre of the femoral head to the centre of the ankle) that intersects the tibial base plate is used to define which zone it passes through (Fig. 2); (3) tibial mechanical axis (TMA), defined as the angle between the line connecting the centre of the ankle and the centre of the knee and a tangent along the surface of the tibial component; and (4) femoral mechanical axis (FMA), defined as the angle between the connecting line between the centre of the femoral head and the centre of the knee and a tangent along the surface of the femoral component. The following were considered the ideal (i.e., normal or in-range) values for these radiographic measurements: 0° ± 3° varus/valgus for HKA; the central zone for ZMA; and 90° for TMA and FMA. HKA was calculated as a mean for the entire patient cohort, and additionally patients outside the ± 3° range were noted.
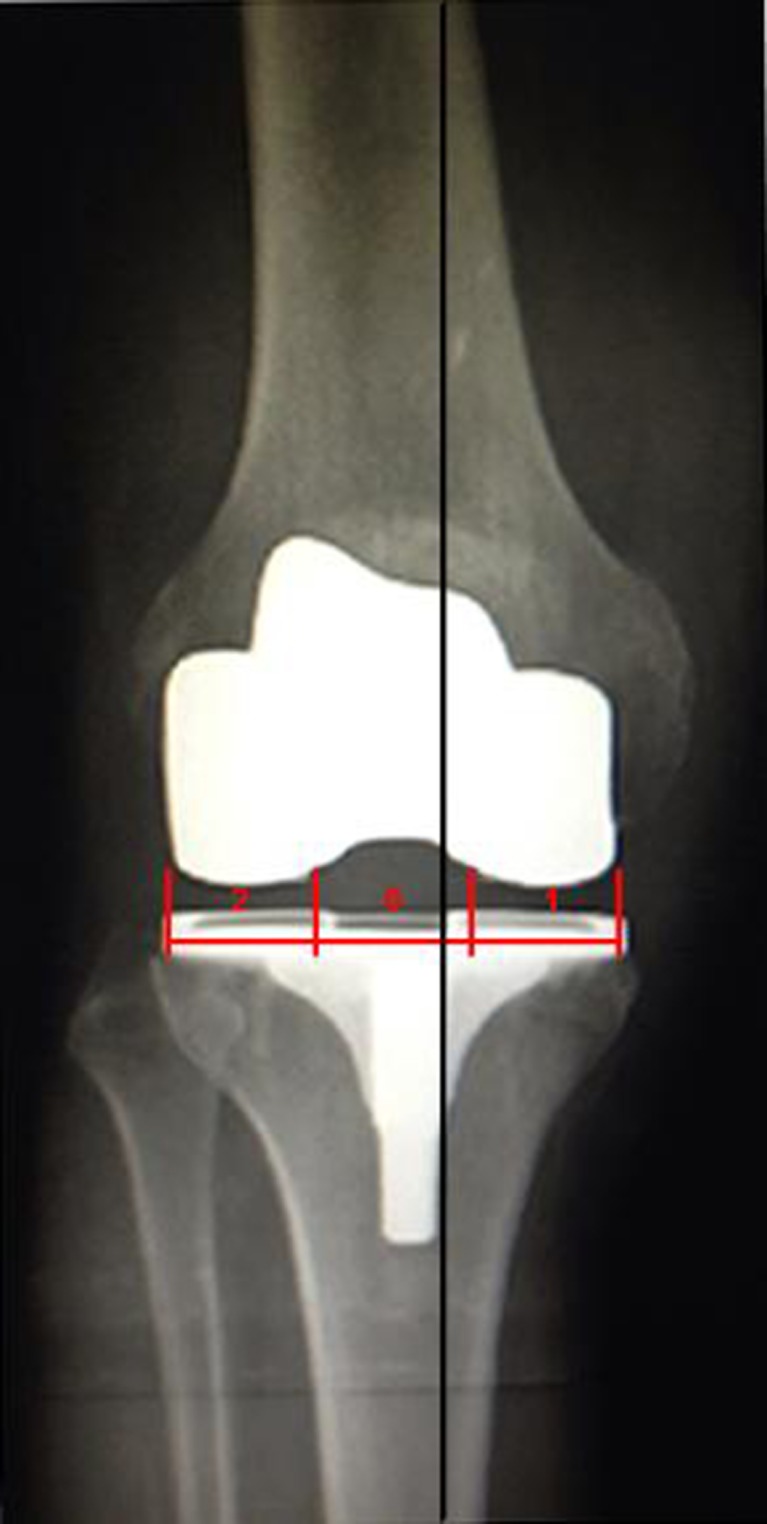
Fig. 1.
The hip-knee-ankle angle (HKA) was determined as the angle between the mechanical axis of the femur and the mechanical axis of the tibia. Both lines cross the center of the knee (red marked circle). In this preoperative image, HKA value is 168.72° (a). The postoperative HKA value is 179.42° (b)
Fig. 2.
To determine the zone of the mechanical axis, the tibial plate was divided into three equal zones (lateral = 2, central = 0, medial = 1) and the mechanical axis (black line) that passes the tibial plate was defined according to which zone it passes through (central, in the present image)
Descriptive analysis (mean ± standard deviation was done using Microsoft Excel (Microsoft Corporation, Seattle, USA) and IBM SPSS Statistics 18 (PASW 18, SPSS Inc., Chicago, IL, USA).
Results
Of the 124 knees in the original cohort, 17 (13.7 %) did not have available x-ray data (seven did not want to undergo x-ray analysis and ten did not wish to return for a follow-up visit). In addition, x-ray data from seven knees (5.6 %) could not be properly evaluated due to the following reasons: incorrect rotation on the long leg x-ray (two knees), femoral head did not appear on the long-leg x-ray (one), flexion contracture > 10° (one), and the considerable extent of pre-operative extra-articular deformity precluded even the attempt to establish a neutral alignment (two with pronounced bowing of the femur bone and one with posttraumatic malalignment following fracture of the tibia). This left a cohort of 100 knees (96 patients) with complete data available for analysis. Postoperative x-ray analysis for these remaining patients occurred at a mean interval of 3.5 months (range, three to four) after the index procedure.
On average, patients experienced a neutral mechanical alignment within ±3° of the ideal alignment of 180° HKA after undergoing TKA with PSI technology (Table 2). PSI also had the effect of substantially reducing the number of outlier knees falling outside this range (Table 2; Fig. 3).
Table 2.
Mean hip-knee-ankle angle (HKA) findings for follow-up cohort (n=100), including outliers beyond the ideal alignment of 180°
| SD of Alignment | |||||||
|---|---|---|---|---|---|---|---|
| Mean±SD | < 177° | > 183° | < 175° | > 185° | Outlier ±3° | Outlier ±5° | |
| HKA preop | 175.5±5.6(163.5−195.4) | 67 | 7 | 0 | 7 | 74 % | 7 % |
| HKA postop | 178.5±1.7(174.0−-183.4) | 10 | 1 | 3 | 0 | 11 % | 3 % |
HKA hip-knee-ankle angle
Fig. 3.
Range of knees falling ±3° outside of the ideal hip-knee-ankle angle (HKA) alignment of 180°, preoperatively and postoperatively
In terms of ZMA, the mechanical axis passed through the central third of the knee in the majority of cases (93 knees). It passed medial to the central third in six knees, with data missing in the one remaining knee. Mean FMA and TMA were 90.0±0.8 (87−92.5) and 90.0±0.7 (87−92.4), respectively.
The surgeon encountered no intra-operative complications with the use of PSI. The specialized instrumentation provided by the manufacturer was optimally fitted to the patient’s individual anatomy in all instances, and therefore did not require any additional modifications to the cutting jigs.
Discussion
The most important finding of the current study is that the constructed hypothesis that patients undergoing TKA with the use of PSI would on average experience a neutral mechanical axis has been confirmed, with the mean HKA changing from 175.5±5.6 preoperatively to 178.5±1.7 postoperatively. Additionally, the 11 % rate of outliers ±3° from neutral compares favorably to the average 10.2 % rate resulting from computer-assisted navigation in prior studies, and substantially improves on the 28.2 % rate encountered with conventional instrumentation [10].
Of the four studies conducted to date with this specific PSI technology, this is the third to support its accuracy [13, 15]. In comparing conventional instrumentation against the VISONAIRE technology in a small cohort of patients undergoing TKA, Noble et al. reported that mechanical alignment in the latter cohort was statistically closer to neutral zero (2.8° vs. 1.7°; p= 0.03), which is in line with the results of the current analysis [15]. This technology was also recently the first to be shown effective in reducing positional outliers of femoral component rotation following TKA [13]. However, it must be noted that the fourth study investigating this specific PSI technology observed only a fair rate of accuracy, with higher risk of error > 3° in the sagittal plane [14]. Regardless of the contradictory nature of these results, it would appear that all four studies are in agreement that this technology presents little additional difficulty to the operating surgeon, given that there have been no intra-operative complications yet reported [13–16].
Contrary results with other PSI systems have also been noted. Initial support for PSI technology was provided in a cadaveric/plastic bone study that observed mean errors for alignment within 1.7° [12]. More recently, Ng et al. observed a lower rate of rate of outliers ±3° from neutral with PSI in comparison with manual instrumentation (14.4 % vs. 27.7 %, respectively), although the rate was slightly higher than in our series (11 %) [10]. Conversely, Klatt et al. found a disconcertingly wide-range of alignment (from 5° valgus to 7.5° varus) with custom-fit technology, although with data from only four patients available, the study does not seem sufficiently powered to draw substantial conclusions, and is disputed by a larger series of 21 patients with this system that found a more encouraging average deviation of 1.2° varus from the mechanical axis [17]. Nunley et al. added further uncertainty to the debate in their three-arm study comparing the two current forms of this technology (PSI that restores the mechanical axis and PSI that restores the kinematic axis) against conventional instrumentation [19]. They found no differences in coronal alignment between PSI that restores the mechanical axis over conventional instrumentation, and further noted that PSI that restores the kinematic axis had a substantial number of valgus outliers.
If this small amount of initial data has somewhat predictably failed to establish an explicit advantage for the use of PSI in terms of improved alignment, outcomes have been more unambiguously supportive in other areas. PSI has been shown to shorten surgical steps and operative times, reduce the burden for surgical instrumentation, and lessen adverse outcomes such as blood loss, infection, and systematic fat emboli [12, 14–20]. Therefore, the proposed utility of this technology should not be limited to radiographic aspects.
The current analysis has several limitations worth considering. Firstly, the study does not offer a control arm with which to compare these results. A similar cohort undergoing TKA with conventional instrumentation would have been a valuable resource for interpreting the true impact of PSI technology. Secondly, the operating surgeon undertakes a high volume of TKAs annually, and it is possible that this level of experience positively influenced the results. The learning curve for beginner surgeons has been shown to be acceptably low with computer-assisted navigation systems, with the exception of a general increase in operative and tourniquet times during initial cases [21–23]. Additional research is required, however, to ascertain whether less-experienced surgeons would encounter a similar learning curve with this particular PSI technology. Thirdly, results in this study were limited to the radiographic outcomes of interest, despite the fact that success in TKA is defined in a multifactorial fashion. Designing the study to record pain, stiffness, range of motion, and other essential clinical outcomes would have provided a fuller picture of this technology’s true impact on patients. Assessing such outcomes, however, requires a longer follow-up period, which was beyond the scope of the current study.
In conclusion, the use of PSI technology allowed for the achievement of a neutral mechanical axis on average, and other favorable radiographic alignment outcomes. This is the largest cohort of patients described in the literature to date to undergo TKA with this specific technology. Further follow-up will be needed to ascertain the long-term impact of these findings.
Acknowledgments
The authors wish to thank the medical assistants Ms. Christina Andrusiak, Ms. Sandra Schaefer, and Ms. Evi Schwarz for the collection of radiographic and patient data.
Conflict of Interest
No benefits in any form have been received or will be received from a commercial party related, directly or indirectly, to the subject of this article. C.O.T is a paid teaching consultant for Smith & Nephew. The authors declare that there are no other potential conflicts of interest in connection with this paper.
Contributor Information
Kiriakos Daniilidis, Email: kraj@gmx.net.
Carsten O. Tibesku, Phone: +49-9421-99570, FAX: +49-9421-9957199, Email: carsten@tibesku.de
References
- 1.Bjorgul K, Novicoff WM, Saleh KJ. Evaluating comorbidities in total hip and knee arthroplasty: available instruments. J Orthop Traumatol. 2010;11:203–209. doi: 10.1007/s10195-010-0115-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Collier MB, Engh CA, Jr, McAuley JP, Engh GA. Factors associated with the loss of thickness of polyethylene tibial bearings after knee arthroplasty. J Bone Joint Surg Am. 2007;89-A:1306–1314. doi: 10.2106/JBJS.F.00667. [DOI] [PubMed] [Google Scholar]
- 3.Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Insall Award paper. Why are total knee arthroplasties failing today? Clin Orthop Relat Res. 2002;404:7–13. doi: 10.1097/00003086-200211000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Sikorski JM. Alignment in total knee replacement. J Bone Joint Surg Br. 2008;90:1121–1127. doi: 10.1302/0301-620X.90B9.20793. [DOI] [PubMed] [Google Scholar]
- 5.Srivastava A, Lee GY, Steklov N, Colwell CW Jr, Ezzet KA, D’Lima DD (2011) Effect of tibial component varus on wear in total knee arthroplasty. Knee [Epub ahead of print] [DOI] [PubMed]
- 6.Werner FW, Ayers DC, Maletsky LP, Rullkoetter PJ. The effect of valgus/varus malalignment on load distribution in total knee replacements. J Biomech. 2005;38:349–355. doi: 10.1016/j.jbiomech.2004.02.024. [DOI] [PubMed] [Google Scholar]
- 7.Jeffery RS, Morris RW, Denham RA. Coronal alignment after total knee replacement. J Bone Joint Surg Br. 1991;73:709–714. doi: 10.1302/0301-620X.73B5.1894655. [DOI] [PubMed] [Google Scholar]
- 8.Ritter MA, Faris PM, Keating EM, Meding JB. Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop Relat Res. 1994;299:153–156. [PubMed] [Google Scholar]
- 9.Stulberg SD, Loan P, Sarin V. Computer-assisted navigation in total knee replacement: results of an initial experience in thirty-five patients. J Bone Joint Surg Am. 2002;84-A(Suppl 2):90–98. [PubMed] [Google Scholar]
- 10.Ng VY, DeClaire JH, Berend KR, Gulick BC, Lombardi AV., Jr Improved accuracy of alignment with patient-specific positioning guides compared with manual instrumentation in TKA. Clin Orthop Relat Res. 2012;470:99–107. doi: 10.1007/s11999-011-1996-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cheng T, Pan XY, Mao X, Zhang GY, Zhang XL. Little clinical advantage of computer-assisted navigation over conventional instrumentation in primary total knee arthroplasty at early follow-up. Knee. 2012;19:237–245. doi: 10.1016/j.knee.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 12.Hafez MA, Chelule KL, Seedhom BB, Sherman KP. Computer-assisted total knee arthroplasty using patient-specific templating. Clin Orthop Relat Res. 2006;444:184–192. doi: 10.1097/01.blo.0000201148.06454.ef. [DOI] [PubMed] [Google Scholar]
- 13.Heyse TJ, Tibesku CO (2012) Improved femoral component rotation in TKA using patient-specific instrumentation. Knee. doi:10.1016/j.knee.2012.10.009. [DOI] [PubMed]
- 14.Conteduca F, Iorio R, Mazza D, Caperna L, Bolle G, Argento G, Ferretti A. Are MRI-based, patient matched cutting jigs as accurate as the tibial guides? Int Orthop. 2012;36:1589–1593. doi: 10.1007/s00264-012-1522-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Conteduca F, Iorio R, Mazza D, Caperna L, Bolle G, Argento G, Ferretti A (2012) Evaluation of the accuracy of a patient-specific instrumentation by navigation. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-012-2098 [DOI] [PubMed]
- 16.Noble JW, Jr, Moore CA, Liu N. The value of patient-matched instrumentation in total knee arthroplasty. J Arthroplast. 2012;27:153–155. doi: 10.1016/j.arth.2011.07.006. [DOI] [PubMed] [Google Scholar]
- 17.Klatt BA, Goyal N, Austin MS, Hozack WJ. Custom-fit total knee arthroplasty (OtisKnee) results in malalignment. J Arthroplast. 2008;23:26–29. doi: 10.1016/j.arth.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 18.Spencer BA, Mont MA, McGrath MS, Boyd B, Mitrick MF. Initial experience with custom-fit total knee replacement: intra-operative events and long-leg coronal alignment. Int Orthop. 2009;33:1571–1575. doi: 10.1007/s00264-008-0693-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nunley RM, Ellison BS, Zhu J, Ruh EL, Howell SM, Barrack RL. Do patient-specific guides improve coronal alignment in total knee arthroplasty? Clin Orthop Relat Res. 2012;470:895–902. doi: 10.1007/s11999-011-2222-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Howell SM, Kuznik K, Hull ML, Siston RA. Results of an initial experience with custom-fit positioning total knee arthroplasty in a series of 48 patients. Orthopedics. 2008;31:857–863. doi: 10.3928/01477447-20080901-15. [DOI] [PubMed] [Google Scholar]
- 21.Confalonieri N, Chemello C, Cerveri P, Manzotti A (2012) Is computer-assisted total knee replacement for beginners or experts? Prospective study among three groups of patients treated by surgeons with different levels of experience. J Orthop Traumatol [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 22.Jenny JY, Miehlke RK, Giurea A. Learning curve in navigated total knee replacement. A multi-centre study comparing experienced and beginner centres. Knee. 2008;15:80–84. doi: 10.1016/j.knee.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 23.Sampath SA, Voon SH, Sangster M, Davies H. The statistical relationship between varus deformity, surgeon’s experience, BMI and tourniquet time for computer assisted total knee replacements. Knee. 2009;16:121–124. doi: 10.1016/j.knee.2008.09.008. [DOI] [PubMed] [Google Scholar]