Abstract
Purpose
One possibility in hip arthroplasty revisions is to combine a modular ceramic head with an adapter or sleeve in isolated acetabular cup replacement. This study consisted of an experimental part to analyse the reliability of taper damage predictions, and a clinical part to analyse the outcomes of modular ceramic head implantation in a case series of isolated cup replacements.
Methods
Analysis of scratch size on 11 explanted hip stems were examined macroscopically and by stereomicroscopy to classify damage to the conical taper. The second part consisted of a prospective analysis of isolated cup revisions using a modular ceramic head, performed in two orthopedic centres.
Results
Analysis of scratch size on the taper yielded inter-observer correlations of 0.545–0.909; comparison with stereomicroscopic data recordings yielded a moderate correlation, with values between 0.545 and 0.090. The clinical study included 47 isolated acetabular cup revisions involving modular ceramic heads. Ceramic head failure did not occur during the average clinical and radiological observation period of 26 months. Mean Harris Hip Score (HHS) at follow-up was 70 points.
Conclusion
From these results, it can be concluded that damage to the implanted stem taper cannot be reliably predicted intraoperatively. Nevertheless, the clinical outcomes did show that there were no problems with the ceramic heads over the short observation period. The application of modular ceramic heads in younger patients requiring isolated cup replacement requires proper risk-benefit analysis, but is possible and appears to be a safe procedure.
Introduction
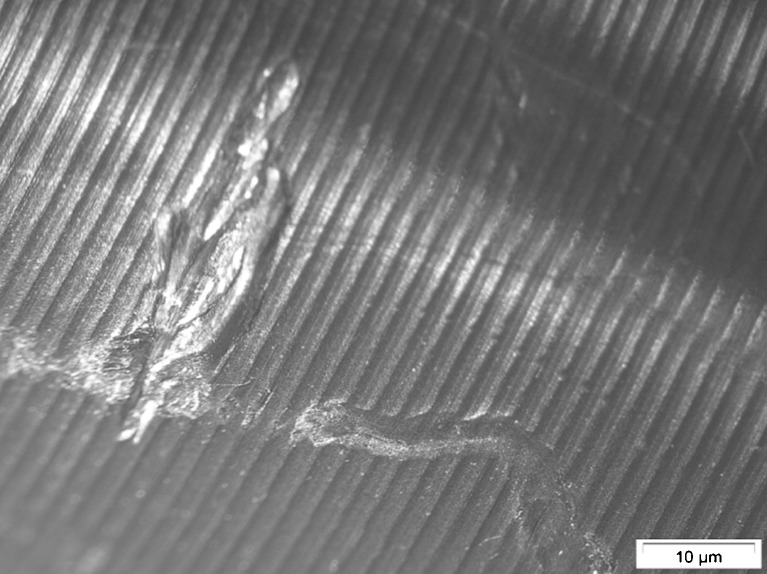
Primary implantation of hip prostheses is being performed increasingly in younger patients under the age of 60 years. These patients place high demands on their hip replacement, due to their longer life expectancy at the time of implantation and their higher levels of activity. There is a real risk that a younger patient will experience one or more revision operations during his lifetime, because of the limited service life of a prosthesis. In a simulation, polyethylene wear when combined with a ceramic head is half that of polyethylene combined with metal [1]. Clinical studies have also yielded very good long-term outcomes for this articulating couple [2, 3]. These findings show that an articulating couple with optimal wear properties is of crucial importance in revision hip surgery, especially in younger patients. Revision surgery is particularly difficult in cases of ceramic head fracture, because the situation demands a replacement ceramic couple [4]. This is not a problem in the case of exchange of the femoral stem, since there are no limitations with regard to the suitability of the prosthetic head material. The situation is different in the case of isolated replacement of the acetabular cup with retention of the existing stem. The use of a primary ceramic head is out of the question, because of microscopically small irregularities of the taper so that the risk of ceramic head fracture is too high, and furthermore, the manufacturer advises against this procedure [5]. For these cases, the manufacturer offers modular taper-to-head combinations, whereby an option adapter sleeve can be added to the ‘used’ conical taper of the hip stem, which can then be coupled with a matching option ceramic modular head. Clear findings are not yet available for these modular ceramic heads, especially since the assessment of taper status must be conducted intraoperatively and the definition of taper damage, i.e. surface irregularities due to scratching, is set at 250 μm (see Figs. 1 and 2) [5]. The aim of our study was to determine to what extent reliable macroscopic assessment of taper damage in compliance with the manufacturer’s requirements is possible, and to record the clinical outcomes of a case series of isolated acetabular cup replacement combined with a modular ceramic head.
Fig. 1.
Macroscopic view of explanted stem taper
Fig. 2.
Microscopic view of the scratches on taper of Fig. 1
Patients and methods
In the first part of the study, 11 prosthetic hip stems explanted during 11 revision procedures were examined macroscopically to classify damage to the conical taper according to the manufacturer’s guidelines and Güttler [6], who classified the cone damage as: grade I, without visible damage and intact cone shape; grade II, with visible scratches but no change of the cone shape; and grade III, with ablation of cone surfaces (bevelled, levelled, crushed) or visible abrasion on the cone. Scratch size was also evaluated as a) less than 250 μm and b) more than 250 μm. This evaluation was conducted by four independent surgeons specialised in joint replacement. The data were analysed for inter-observer reliability. Evaluation of the prosthetic stems was followed by referenced stereomicroscopy (stereomicroscope SZ61 with digital camera SC30, Olympus), in ignorance of the surgeon’s evaluations. Scratches and deformation were measured precisely by means of image analysis software (Stream, Olympus). The criteria given were the same as for the macroscopic examination. Four investigators compared the stereomicroscopic and macroscopic values to test for correlation. Statistical analysis was performed with the SPSS program, version 18. Correlation of the dichotomous variables between the different investigators and the recorded values (verum) was calculated according to the method of phi correlation as a measure of association based on the formula for “simple correlation”. A value of up to 0.2 was defined as very low correlation, up to 0.5 as low correlation, up to 0.7 as moderate correlation, up to 0.9 as high correlation and over 0.9 as very high correlation.
The second part consisted of an analysis, approved by the local ethics committee, of the isolated cup revisions using a modular ceramic head that were performed in two orthopaedic and trauma centres between 2003 and 2011. Revision surgery was performed in all cases via a transgluteal approach with the patient supine or in the lateral decubitus position. Intraoperatively, the strength of the implanted stem was tested mechanically and secure anchorage confirmed. In addition, the implanted cone was examined in all cases for damage and then checked to ensure there was only slight, irrelevant damage equivalent to grades I and II according to Güttler [6]. The parameters shown in Table 1 were derived from the case file, and include the Harris Hip Score (HHS), as achieved at the final routine follow-up. The radiographs taken at the final follow-up were also examined for ceramic head fracture or surface flaking.
Table 1.
Parameters taken from the case file
| Gender |
| Taper size (12/14 or 14/16) |
| Offset adapter or straight adapter |
| Prothesis implantation time |
| Age at revision surgery |
| Reason for revision (loosening, wear, dislocation) |
| Type of cup implant (Burch-Schneider reinforcement ring with bone grafting and cemented polyethylene cup, Trabecular-Metal cup, other cup implant (cemented or spherical and cementless) |
| Clinical and radiological follow-up in months |
| Ceramic head complications |
| Harris Hip Score (HHS) |
Results
Stereomiscroscopic evaluation revealed nine prostheses with scratches over 250 μm and two below 250 μm with no grade III damage. Laboratory analysis yielded correlations of 0.182–0.909, i.e. very different levels of agreement, for inter-observer evaluation of suitability. For scratch size on the taper, the inter-observer correlations were 0.545–0.909, which is also highly heterogeneous, but still more reliable than for suitability. Agreement with stereomicroscopic assessment yielded predominantly moderate correlations, with values of 0.545–0.090 (see Tables 2 and 3).
Table 2.
Evaluation of used taper suitability
| Measure of association from simple correlation | ||||
|---|---|---|---|---|
| Evaluation of suitability | ||||
| Observer 1 | Observer 2 | Observer 3 | Observer 4 | |
| Observer 1 | 1.000 | 0.818 | 0.182 | 0.909 |
| Observer 2 | 0.818 | 1.000 | 0.182 | 0.909 |
| Observer 3 | 0.182 | 0.182 | 1.000 | 0.273 |
| Observer 4 | 0.909 | 0.909 | 0.273 | 1.000 |
Table 3.
Association of scratch size on used tapers
| Measure of association from simple correlation | |||||
|---|---|---|---|---|---|
| Scratch size | |||||
| Observer 1 | Observer 2 | Observer 3 | Observer 4 | Stereomicroscope | |
| Observer 1 | 1.000 | 0.818 | 0.455 | 0.818 | 0.545 |
| Observer 2 | 0.818 | 1.000 | 0.455 | 0.818 | 0.545 |
| Observer 3 | 0.455 | 0.455 | 1.000 | 0.636 | 0.909 |
| Observer 4 | 0.818 | 0.818 | 0.636 | 1.000 | 0.545 |
| Stereomicroscope | 0.545 | 0.545 | 0.909 | 0.545 | 1.000 |
The clinical part consisted of retrospective study of 47 isolated cup revisions with application of modular sleeved ceramic revision heads. Average age of the patients at the time of the index operation was 61 years (SD 10 years). Average implantation time at revision surgery was ten years (SD nine years). Reasons for revision were: aseptic loosening in 41 cases, recurrent dislocation in three cases, and polyethylene inlay deterioration in three cases. Revision was performed with a Merete BioBall delta ceramic head or Biolox option head in 42 cases, and with a Merete BioBall offset adapter with BioBall delta ceramic head in five cases. There were no intraoperative handling problems and no ceramic head fractures after a mean follow-up period of 26 months (SD 16). Analysis of the radiographs did not reveal any problems with the ceramic head. Mean HHS at final follow up was 70 points (SD 17). In 13 cases, a HHS of over 80 points was recorded, corresponding to a good to excellent result, whereby 34 patients only achieved a moderate to poor HHS of under 80 points.
Discussion
Numerous studies of isolated acetabular revision have reported good long-term outcomes that are no different from those of total revision [7–12]. Chen et al. [13] showed in one study that the existing, securely anchored stem was still firmly anchored after a mean of six years in all cases. Similar findings were reported by Moskal et al. [14], who found that at a mean of eight years postoperatively, 97 % of stems had remained firmly anchored. Given this data, isolated cup replacement should be the procedure of choice in situations where it represents a less intrusive operation and avoids the difficulties of extracting a firmly anchored stem.
Hannouche et al. [15] have already presented good outcomes with no fractures of standard ceramic heads added onto used conical tapers in 61 cases. In one case of ceramic fracture of a revision head, Koo et al. [16] reported application of a primary ceramic head despite intraoperatively visible damage to the stem taper, though this was not described in detail. After four weeks, the primary ceramic head fractured. This procedure is not approved by the manufacturer [5] and, apart from the potentially serious consequences for the patient if ceramic fracture recurs as in Koo’s case, may be associated with substantial medicolegal issues and should, therefore, not be performed as a standard procedure. Metal heads are an available alternative in revision cases. The application of metal heads without the use of highly crosslinked polyethylene is associated with unfavourable wear properties [1], and should therefore be given very careful consideration in the management of a young and active patient. The option of implanting primary or spherical cups at revision surgery means that in special cases the use of a ceramic-on-ceramic articulating couple is possible. In the study by Lakemaier et al. [10], the outcomes after implantation of a spherical cup were as good as those recorded for primary implantation and, therefore, the primary articulating couple should be maintained at revision. Thorey et al. [17] recently reported the course of 91 acetabular cup replacements using a modular sleeved ceramic head and found good clinical outcomes for a short observation time. There were no problems with the ceramic heads.
Our clinical and radiological results, as indicated by the outcome scores, are in line with the data given in the current literature [9, 12], and reflect the heterogeneity of the patient sample and the conditions necessitating revision. We regard tribological optimisation as especially important, given our collective of younger patients and the fact that some of them must expect future revisions. Fracture of the ceramic head was not observed in any of our cases. The short follow-up time must, however, be seen as a weakness of this study, although ceramic head fracture, according to the case report by Koo et al. and by Takata et al. [16, 18], appears more likely to occur during the early postoperative course than after several years. In the study by Koo et al., ceramic fracture occurred 12–31 months after the index operation; but with a damaged taper and a primary ceramic head, the fixation failed after four weeks. In the study by Takata et al., the ceramic fracture occurred ten months after index operation. This means that it is likely that most ceramic head fractures should occur within 12 months, especially when used on a damaged taper. Therefore, it seems worthwhile to consider the application of a modular sleeved ceramic head in cases of isolated acetabular cup revision, even though our sample was small and our follow-up time limited.
Macroscopic analysis under laboratory conditions as reported here could not guarantee reliable evaluation of scratch size up to the specified limit of 250 μm stipulated by the manufacturer for modular ceramic heads. As far as we know, this is the first time that macro-microscopic analysis has been conducted. Therefore, it is difficult to put the results into context. In a clinical study by Kim et al. [19], the authors recorded worse outcomes for isolated cup revision on an existing monoblock prosthetic stem compared to stems with detachable head, and attributed this finding to poor intraoperative assessment of the unspoiled condition of the monoblock head. This prompts the conclusion that reliable intraoperative assessment is even more difficult and subject to error than laboratory analysis. A scratch size up to 300 μm of a grade II cone damage, according to Güttler [6], does also not lead to a more reliable macroscopic analysis. The variability in correlation between the different observers in the current study implies that the correct estimation of taper damage always remains uncertain intraoperatively. Our clinical data showed that the procedure with ceramic heads could be safe; nevertheless, if there is doubt about the magnitude of damage, the use of a metal head is a viable alternative. Since no data is given in the literature, it is not possible to estimate how great the risk of sleeved ceramic head fracture is, when there is poor intraoperative damage assessment. What is required is an investigation of defined scratch sizes on conical tapers in conjunction with mechanical testing. According to the manufacturer’s manual, a damaged taper is associated with a considerable risk of ceramic fracture, but this risk is not definitively quantified [5]. To what extent the application of a metal head in these cases is associated with increased risk or wear between the taper and the head cannot be inferred from the current literature. Numerous clinical studies report that a metal head can be regarded as very safe, at least in the short to midterm [11, 20, 21]. However, it may be that head size plays a decisive role, because failure has been described for modular metal heads of very large diameters [22, 23].
The potential advantages of improved wear properties and, consequently, a longer implantation time for ceramic-based couples needs to be critically balanced against the potential short-term disadvantages of that type of couple. This applies equally to revision surgery and primary implantations. Bozic et al. [20] found no essential differences between the articulating couples in their study over a fairly short observation time. It can be concluded that in older patients, a more favourable price wear couple should be chosen. In revision surgery in a younger patient, every effort must be made to avoid yet another revision due to wear. Therefore, patients should be selected very carefully in order to maximise benefit from the available procedural options.
Acknowledgments
Conflict of Interest
There is no conflict of interest.
References
- 1.Clarke IC, Gustafson A. Clinical and hip simulator comparisons of ceramic-on-polyethylene and metal-on-polyethylene wear. Clin Orthop Relat Res. 2000;379:34–40. doi: 10.1097/00003086-200010000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Urban JA, Garvin KL, Boese CK, Bryson L, Pedersen DR, Callaghan JJ, Miller RK. Ceramic-on-polyethylene bearing surfaces in total hip arthroplasty. Seventeen to twenty-one-year results. J Bone Joint Surg Am. 2001;83-A(11):1688–1694. doi: 10.2106/00004623-200111000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Sedrakyan A, Normand SL, Dabic S, Jacobs S, Graves S, Marinac-Dabic D. Comparative assessment of implantable hip devices with different bearing surfaces: systematic appraisal of evidence. BMJ. 2011;343:d7434. doi: 10.1136/bmj.d7434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Matziolis G, Perka C, Disch A. Massive metallosis after revision of a fractured ceramic head onto a metal head. Arch Orthop Trauma Surg. 2003;123(1):48–50. doi: 10.1007/s00402-002-0449-9. [DOI] [PubMed] [Google Scholar]
- 5.CeramTec (2007) BIOLOX®OPTION – Ceramic Femoral Ball Heads for Hip Revision Brochure. CeramTec Ag Plochingen, Germany 1–12
- 6.Güttler T. Experience with BIOLOX OPTION revision heads. Darmstadt: Steinkopff-Verlag; 2006. [Google Scholar]
- 7.Fukui K, Kaneuji A, Sugimori T, Ichiseki T, Kitamura K, Matsumoto T. Should the well-fixed, uncemented femoral components be revised during isolated acetabular revision? Arch Orthop Trauma Surg. 2011;131(4):481–485. doi: 10.1007/s00402-010-1152-x. [DOI] [PubMed] [Google Scholar]
- 8.Cho HJ, Han SB, Park JH, Park SW (2011) An analysis of stably fixed femoral components retained during revision total Hip arthroplasty. J Arthroplasty. doi:10.1016/j.arth.2011.02.015 [DOI] [PubMed]
- 9.Lawless BM, Healy WL, Sharma S, Iorio R. Outcomes of isolated acetabular revision. Clin Orthop Relat Res. 2010;468(2):472–479. doi: 10.1007/s11999-009-1104-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lakemeier S, Aurand G, Timmesfeld N, Heyse TJ, Fuchs-Winkelmann S, Schofer MD. Results of the cementless Plasmacup in revision total hip arthroplasty: a retrospective study of 72 cases with an average follow-up of eight years. BMC Musculoskelet Disord. 2010;11:101. doi: 10.1186/1471-2474-11-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vargas B, Caton J. Acetabular revision with freeze-dried irradiated and chemically treated allograft: a minimum 5-year follow-up of 17 cases. Int Orthop. 2009;33(1):35–39. doi: 10.1007/s00264-007-0444-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ochs BG, Schmid U, Rieth J, Ateschrang A, Weise K, Ochs U. Acetabular bone reconstruction in revision arthroplasty: a comparison of freeze-dried, irradiated and chemically-treated allograft vitalised with autologous marrow versus frozen non-irradiated allograft. J Bone Joint Surg Br. 2008;90(9):1164–1171. doi: 10.1302/0301-620X.90B9.20425. [DOI] [PubMed] [Google Scholar]
- 13.Chen XD, Waddell JP, Morton J, Schemitsch EH. Isolated acetabular revision after total hip arthroplasty: results at 5–9 years of follow-up. Int Orthop. 2005;29(5):277–280. doi: 10.1007/s00264-005-0674-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moskal JT, Shen FH, Brown TE. The fate of stable femoral components retained during isolated acetabular revision: a six-to-twelve-year follow-up study. J Bone Joint Surg Am. 2002;84-A(2):250–255. doi: 10.2106/00004623-200202000-00012. [DOI] [PubMed] [Google Scholar]
- 15.Hannouche D, Delambre J, Zadegan F, Sedel L, Nizard R. Is there a risk in placing a ceramic head on a previously implanted trunion? Clin Orthop Relat Res. 2010;468(12):3322–3327. doi: 10.1007/s11999-010-1505-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Koo KH, Ha YC, Jung WH, Kim SR, Yoo JJ, Kim HJ. Isolated fracture of the ceramic head after third-generation alumina-on-alumina total hip arthroplasty. J Bone Joint Surg Am. 2008;90(2):329–336. doi: 10.2106/JBJS.F.01489. [DOI] [PubMed] [Google Scholar]
- 17.Thorey F, Sakdinakiattikoon M, Thiengwittayaporn S, Windhagen H. Early results of revision Hip arthroplasty using a ceramic revision ball head. Semin Arthroplasty. 2011;22:284–289. doi: 10.1053/j.sart.2011.09.008. [DOI] [Google Scholar]
- 18.Takata ET, Basile R, Albertoni WM. Experiences with Bicontact ceramic-ceramic total hip arthroplasty. Z Orthop Unfall. 2007;145(Suppl 1):S25–S28. doi: 10.1055/s-2007-965656. [DOI] [PubMed] [Google Scholar]
- 19.Kim YS, Kim YH, Hwang KT, Choi IY. Isolated acetabular revision hip arthroplasty with the use of uncemented cup. J Arthroplasty. 2009;24(8):1236–1240. doi: 10.1016/j.arth.2009.05.032. [DOI] [PubMed] [Google Scholar]
- 20.Bozic KJ, Ong K, Lau E, Kurtz SM, Vail TP, Rubash HE, Berry DJ. Risk of complication and revision total hip arthroplasty among Medicare patients with different bearing surfaces. Clin Orthop Relat Res. 2010;468(9):2357–2362. doi: 10.1007/s11999-010-1262-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patel D, Parvizi J, Sharkey PF. Alternative bearing surface options for revision total hip arthroplasty. Instr Course Lect. 2011;60:257–267. [PubMed] [Google Scholar]
- 22.Vendittoli PA, Amzica T, Roy AG, Lusignan D, Girard J, Lavigne M. Metal Ion release with large-diameter metal-on-metal hip arthroplasty. J Arthroplasty. 2011;26(2):282–288. doi: 10.1016/j.arth.2009.12.013. [DOI] [PubMed] [Google Scholar]
- 23.Garbuz DS, Tanzer M, Greidanus NV, Masri BA, Duncan CP. The John Charnley Award: metal-on-metal hip resurfacing versus large-diameter head metal-on-metal total hip arthroplasty: a randomized clinical trial. Clin Orthop Relat Res. 2010;468(2):318–325. doi: 10.1007/s11999-009-1029-x. [DOI] [PMC free article] [PubMed] [Google Scholar]