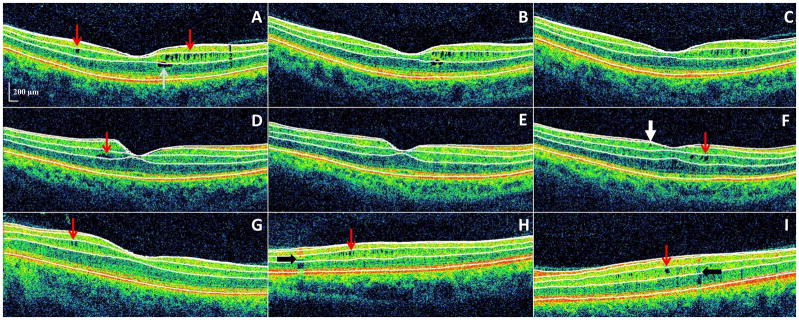
Figure 2. Microcystic macular edema (MME) of the inner nuclear layer (INL) as identified by spectral-domain optical coherence tomography, with automated segmentation lines displayed.
Panels A–C: All images were acquired from the same patient during a 3-year period of observation, and are presented in chronological order in consecutive panels. Panel A: MME of the INL (red arrows) was present at baseline, as well as a foveal cyst of the outer nuclear layer (ONL). Panels B–C: The ONL cyst progressively resolved during follow-up.
Panels D–F: All images were acquired from the same patient during a 2-year period of observation, and are presented in chronological order in consecutive panels. Panel D: A single INL cyst (red arrow) was present at baseline. Panel E: The cyst spontaneously resolved after one year. Panel F: Following fingolimod treatment (initiated after scan E) the patient developed new cystic changes of the INL (red arrow). An epiretinal membrane is noted (white arrow) that had been present on previous scans as well (not illustrated though in either panel D or E).
Panels G–I: Three different patients with MME of the INL (red arrows) are presented in each panel. Vessel artifacts (black arrows) are demonstrated for comparison.
OCT-segmentation performed in 3D identifies the inner limiting membrane, the outer boundaries of the RNFL, inner plexiform layer, and outer plexiform layer, and the inner boundary of the retinal pigment epithelium. The identification of these retinal boundaries enables the determination of the thicknesses of the following retinal layers – the macular RNFL, GCL+innerplexiform layer (GCIP; labeled 1 in panel A), INL (including the outer plexiform layer; labeled 2 in panel A), and ONL (including the inner and outer photoreceptor segments; labeled 3 in panel A).