Abstract
Aloe barbadensis Miller (Aloe vera) is an herbal remedy promoted to treat a variety of illnesses; however, only limited data are available on the safety of this dietary supplement. Drinking water exposure of F344/N rats and B6C3F1 mice to an Aloe vera whole-leaf extract (1, 2, and 3%) for 13 weeks resulted in goblet cell hyperplasia of the large intestine in both species. Based upon this observation, 2-year drinking water studies were conducted to assess the carcinogenic potential of an Aloe vera whole-leaf extract when administered to F344/N rats (48 per sex per group) at 0.5, 1, and 1.5%, and B6C3F1 mice (48 per sex per group) at 1, 2, and 3%. Compared with controls, survival was decreased in the 1.5% dose group of female rats. Treatment-related neoplasms and nonneoplastic lesions in both species were confined primarily to the large intestine. Incidences of adenomas and/or carcinomas of the ileo-cecal and cecal-colic junction, cecum, and ascending and transverse colon were significantly higher than controls in male and female rats in the 1 and 1.5% dose groups. There were no neoplasms of the large intestine in mice or in the 0 or 0.5% dose groups of rats. Increased incidences of mucosa hyperplasia of the large intestine were observed in F344/N rats, and increased incidences of goblet cell hyperplasia of the large intestine occurred in B6C3F1 mice. These results indicate that Aloe vera whole-leaf extract is an intestinal irritant in F344/N rats and B6C3F1 mice and a carcinogen of the large intestine in F344/N rats.
Key Words: natural products, metabolism, histopathology, chronic, gastrointestinal, carcinogenesis, dietary supplement, Aloe vera, Aloe barbadensis Miller, colon cancer, rodents
Aloe barbadensis Miller (Aloe vera) has enjoyed a long history as an herbal remedy, and there are numerous references in the literature to document its use for over 3500 years (Hecht, 1981). In recent times, the chronic oral consumption of Aloe vera leaf extracts has been promoted as a prophylaxis and treatment to alleviate a variety of unrelated systemic conditions (Marshall, 1990). As a herbal remedy, Aloe vera whole-leaf extract is advertised for detoxification; it is claimed to cure constipation, help flush out toxins and wastes from the body, promote digestion, and reduce the risk of illnesses (Ayushveda, 2010; Bisi-Johnson et al., 2011). Powdered forms of the Aloe vera whole-leaf extracts are used to produce capsules that provide 100 to 500mg per dose. Manufacturers produce liquid forms of the Aloe vera whole-leaf extract at its natural strength and at various levels of concentration by evaporation, typically from twice the natural strength to 10 times or more. Based upon a consumption of 240ml, four times per day, individuals would be exposed to up to 14.4g Aloe vera whole-leaf extract per day. As is the case of many other folk medicines, the efficacy of Aloe vera remains controversial and its safety as a dietary supplement and herbal remedy uncertain.
The Aloe vera plant leaf is composed primarily of water (99.0–99.5%); the remaining 0.5–1.0% solid material is reported to contain over 75 different potentially bioactive compounds, including vitamins, minerals, enzymes, simple and complex polysaccharides, phenolic compounds, and organic acids (Atherton, 1998). The leaf of the Aloe vera plant consists of two main parts: an inner central leaf pulp that produces and stores Aloe vera gel, and an outer leaf pulp that produces and transports Aloe vera latex (Briggs, 1995; Klein and Penneys, 1988).
Aloe vera gel contains high-molecular-weight (≥ 30–40kDa) nonstarch polysaccharides in addition to other constituents. The high-molecular-weight polysaccharides are composed mainly of glucose and mannose subunits linked by β-(1→4)-glycosidic bonds (Chow et al., 2005; Femenia et al., 1999; Gowda et al., 1979; Mandal and Das, 1980; Yaron, 1993). The chemical bonds within the polysaccharides contribute to the viscous and opaque qualities of the gel but also render it susceptible to degradation by endogenous and exogenous bacteria (Gorloff, 1983; Waller et al., 2004; Yaron, 1993). The β-(1→4)-glycosidic bonds of the polysaccharides are an important consideration when examining the reported therapeutic effects of Aloe vera gel because these bonds are resistant to hydrolysis by acid in the stomach and α-glucosidase activity in the small intestine. Inasmuch as humans and most mammals lack the β-glycosidase enzymes that are needed to hydrolyze the β-(1→4)-glycosidic bonds, many of the Aloe vera gel polysaccharides reach the colon as mostly undigested fiber that can be fermented to short-chain fatty acids and other compounds by colonic microflora (Boudreau and Beland, 2006; Pogribna et al., 2008).
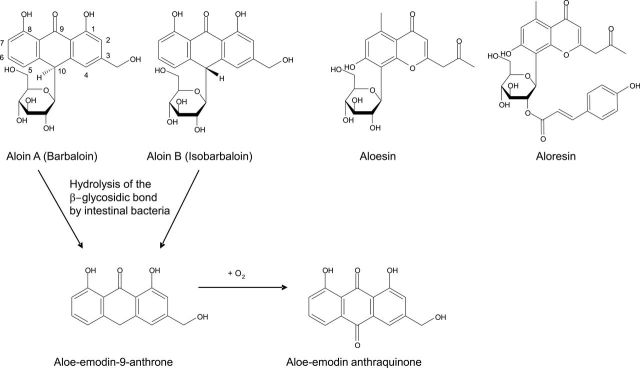
Aloe vera latex, a bitter exudate of the outer margins of the leaf pulp, contains anthraquinones and other phenolic substances (Reynolds, 1985). In plants, anthraquinones are present mostly as glycosides, where the sugar molecules are bound to the anthracene ring by a β-glycosidic linkage (van Gorkom et al., 1999). Aloin A and its epimer, aloin B, are the major anthraquinone glycosides of the Aloe vera latex (Birch and Donovan, 1955; Hay and Haynes, 1956; Reynolds, 1985). The sugar moiety in the aloin compounds is D-glucose, where carbon atom 1 of the D-glucose moiety is linked directly to carbon atom 10 of the anthracene ring in a β-configuration (Fig. 1). The β-(1→10) C–C bond is resistant to β-glycosidase of plants and most plant bacteria (Joshi, 1998; Vyth and Kamp, 1979); however, the intestinal microflora of humans and animals can cleave the β-C-glucosyl bond although considerable variation in response among animal species occurs (Che et al., 1991; Hattori et al., 1988; Mapp and McCarthy, 1970). Cleavage of the β-C-glucosidic bond results in the formation of aloe-emodin and other free anthraquinones and anthrones (Fig. 1); many of these anthraquinones are irritants to the gastrointestinal tract and possess cathartic activity (Atherton, 1998; Saito et al., 1989; Teradaira et al., 1993).
FIG. 1.
Structure of Aloe vera latex–derived anthraquinone C-glycosides, anthrones, and anthraquinones.
The intact leaves of the Aloe vera plant are utilized to produce Aloe vera whole-leaf extract, where just the rind components of the leaf are removed. The resulting extract is yellow in color and retains the full complement of the β-linked high-molecular-weight polysaccharides of the inner leaf gel and the β-linked C-glycoside anthraquinones of the outer leaf latex.
Several studies have attempted to determine whether or not Aloe vera is toxic to animals or humans (Fogleman et al., 1992a , b; Herlihy et al., 1998a , b; Ikeno et al., 2002; Logarto Parra et al., 2001; Lim et al., 2003; Shah et al., 1989; Siegers et al., 1993a , b). One area of testing that has not been addressed is the potential effects of the β-glycosidic compounds, i.e., β-(1→4) polysaccharides and β-C-glycoside anthraquinones, in the gastrointestinal tract, where their concentrations would be higher and where the microflora environment may actively participate in their metabolism. In a 1-year study of Aloe arborescens Miller, another commercial Aloe species, diarrhea, reduced body weight gains, and severe sinus dilatation of the ileo-cecal lymph nodes were observed in Wistar Hannover rats administered a whole-leaf powdered extract in the diet at a dose of 4.0% (wt/wt) (Matsuda et al., 2008). In a subsequent 2-year study, adenomas and adenocarcinomas of the cecum, colon, and rectum developed in male Wistar Hannover rats administered an A. arborescens whole-leaf powdered extract in the diet at the 4.0% level (Yokohira et al., 2009).
Although Aloe vera has been used as a herbal remedy to treat a variety of illnesses, few toxicity or carcinogenesis studies have been reported in the literature. This article presents the results of 2-year oral carcinogenicity bioassays that were conducted to provide more information on the toxic and carcinogenic effects from long-term ingestion of this widely used herbal remedy. Drinking water, rather than diet, was the selected route of administration because Aloe vera products are consumed mostly in liquid form by the public.
MATERIALS AND METHODS
Test agent procurement, exposure concentration selection, and characterization.
Aloe vera whole-leaf plant extract was obtained from Pangea Phytoceuticals, Inc. (Harlingen, TX) and was the product obtained solely from mature, fresh A. barbadensis Miller (Aloe vera) leaves. The Aloe vera whole-leaf extract was produced by grinding the whole leaves and treating the slurry with cellulase (23mg/l). The pulp was removed from the extract by filtration, and lyophilization of the product (max. 6% moisture content) began within 6h of harvesting. Sterilization to maintain stability and kill endogenous bacteria in the Aloe vera whole-leaf extract was achieved by γ-ray irradiation delivered at a range of 8–20 kGy (IBA/SteriGenics International, Schaumburg, IL). The lyophilized and γ-irradiated Aloe vera whole-leaf plant extract was stored at −20°C to maintain the quality and stability of the components.
A 13-week toxicity study was conducted to set the doses of the Aloe vera whole-leaf extract for the 2-year study. In the 13-week study, F344/N rats and B6C3F1 mice were administered an Aloe vera whole-leaf extract in their drinking water at concentrations of 1, 2, and 3% (wt/wt). Shorter transit times and depressed body weights (> 20%) were observed in rats, but not in mice, at doses of 2 or 3%. Goblet cell hyperplasia (Table 1), with mucus present in the lumen, and lymph node hyperplasia were observed in the large intestine of both species.
TABLE 1 .
Incidence and Severity of Goblet Cell Hyperplasia in Male and Female F344/N Rats and B6C3F1 Mice Administered Aloe Vera Whole-Leaf Extract in the Drinking Water for 13 Weeks
| Species | Site of lesion | Sex | Aloe vera whole-leaf extract (%) | |||
|---|---|---|---|---|---|---|
| 0 | 1.0 | 2.0 | 3.0 | |||
| F344/N Rats | Cecum | Male | 0/12 (0.0%)a | 6/11 (54.5%)2.2 | 10/10 (100.0%)2.2 | 7/7 (100.0%)3.0 |
| Female | 1/12 (8.3%)1.0 | 6/12 (50.0%)1.5 | 8/8 (100.0%)2.3 | 4/4 (100.0%)2.3 | ||
| Colon | Male | 0/12 (0.0%) | 10/11 (90.9%)2.0 | 10/10 (100.0%)2.4 | 7/7 (100.0%)2.7 | |
| Female | 0/12 (0.0%) | 8/12 (66.7%)1.5 | 8/8 (100.0%)2.5 | 4/4 (100.0%)3.0 | ||
| Rectum | Male | 0/12 (0.0%) | —b | 9/10 (90.0%)2.0 | 4/7 (57.1%)2.5 | |
| Female | 0/12 (0.0%) | — | 7/8 (87.5%)1.6 | 3/4 (75.0%)1.7 | ||
| B6C3F1 Mice | Cecum | Male | 0/12 (0.0%) | 1/12 (8.3%)1.0 | 5/12 (41.7%)1.2 | 9/12 (75.0%)1.0 |
| Female | 0/12 (0.0%) | 0/12 (0.0%) | 0/11 (0.0%) | 1/12 (8.3%)1.0 | ||
| Colon | Male | 0/12 (0.0%) | 3/12 (25.0%)1.0 | 9/12 (75.0%)1.4 | 11/12 (91.7%)1.1 | |
| Female | 0/12 (0.0%) | 0/12 (0.0%) | 4/11 (36.4%)1.0 | 7/12 (58.3%)1.1 | ||
| Rectum | Male | 0/12 (0.0%) | — | — | 4/11 (36.4%)1.0 | |
| Female | 0/12 (0.0%) | — | — | 5/11 (45.4%)1.0 | ||
aThe data are reported as the number of animals with a lesion per number of animals examined microscopically, the % incidence (in parentheses), and the mean severity of the lesion, where 1 = minimal, 2 = mild, 3 = moderate, 4 = marked.
bAnimals without reported incidence were not evaluated by histopathology.
The highest exposure concentrations of the Aloe vera whole-leaf extract for the 2-year study were set just below the concentrations that were determined to contribute to depressed body weights of rodents in the 13-week study. Exposure concentrations for the 2-year study were 0, 0.5, 1, and 1.5% (wt/wt) in rats and 0, 1, 2, and 3% (wt/wt) in mice. Millipore 0.2-µm-filtered tap water served as the diluent for the dosed water formulations and as the control group treatment. The dissolution of the Aloe vera whole-leaf extract in water was achieved by stirring for 2h at 4°C.
Drinking water formulations were prepared twice weekly and stored at 4°C to ensure the quality and stability of Aloe vera whole-leaf extract. HPLC detection and quantification of malic acid and aloin A was used to confirm the concentration levels of the Aloe vera whole-leaf extract in the drinking water formulations. The mean percentages of targeted values and standard deviations for malic acid and aloin A in the dosed water, measured weekly over the 2-year study, were 95±7% and 100±12%, respectively. Malic acid and aloin A were not detected in control water samples, with the limits of quantitation estimated to be 100 ppm for malic acid and 0.1 ppm for aloin A.
Animal source, housing, treatment, and monitoring.
This study was conducted in accordance with the Food and Drug Administration Good Laboratory Practice Regulations (CFR Title 21, Part 58). The care of the animals and all experimental procedures were performed in accordance with an animal study protocol approved by the National Center for Toxicological Research (NCTR) Institutional Animal Care and Use Committee.
Specific-pathogen-free in-house bred male and female F344/N Nctr rats and B6C3F1 Nctr mice were used. They were randomly assigned to treatment groups on a weight-ranked basis at 5 weeks of age. Animals were individually identified by tail tattoo (AIMS, Inc., Bud Lake, NJ) and were 6 to 7 weeks of age at the start of the treatment.
The rats and mice were housed in separate animal rooms in individually ventilated polycarbonate rodent cages with hardwood chip bedding, two rats or four mice of the same sex per cage. The environmentally controlled animal rooms were set to maintain temperature and humidity at 23±3°C and 50±20%, respectively, with at least 10 air changes per hour and a 12-h light cycle. Autoclaved NIH 31 rodent chow pellets (Purina Mills, Richmond, NJ) and dosed water formulations were provided ad libitum. Microbiological surveillance of the drinking water, feed, cage waste, and room environments was conducted on a routine basis.
Groups of 48 animals per sex were administered drinking water that contained the Aloe vera whole-leaf extracts for 7 days a week and for a period of 104 weeks, with no recovery period, or until intercurrent death or euthanasia for humane reasons.
Body weights and feed consumption were measured weekly. Dosed water bottles were changed and weighed on Monday, Wednesday, Friday, and Sunday of each week. At study termination, rats and mice were weighed individually and fasted overnight. Animals continued to receive dosed water until euthanized by carbon dioxide asphyxiation.
Necropsy and pathology.
Complete necropsies and microscopic examinations were performed on all animals. At necropsy, all organs and tissues were examined for grossly visible lesions; the cecum and cecal-colic junction were opened and examined. Tissues were preserved in 10% neutral buffered formalin (with the exception that Davidson’s fixative was used for the eyes and testes) and were trimmed, processed, embedded in paraffin, sectioned, and stained with hematoxylin and eosin. When possible, a microscopic finding was recorded with the corresponding gross observation, and a primary cause of death, along with any contributing cause of death, was assigned. Following completion of the study, the accuracy of the histopathologic findings was determined by microscopic reviews of neoplasms and target organs by a pathology working group (Boorman and Eustis, 1986).
Statistical analyses.
The dose-response survival analysis was conducted by calculating Kaplan-Meier estimates of mean survival times for each species by sex and dose and using a Cox proportional hazard model to test the effect of treatment relative to control.
Body weights and feed and water consumptions were analyzed using one-way repeated measures mixed model ANOVA. Body weight data at 4-week intervals and the average food or water consumption per animal per day in 4-week intervals from week 0 through 104 were included in these comparisons. Dunnett’s tests were performed for comparisons of dosed groups to the control groups.
The Poly-3 test, which takes into account the survival differences of animals, was used to assess neoplasm and nonneoplastic lesion incidence (Bailer and Portier, 1988; Piegorsch and Bailer, 1997; Portier and Bailer, 1989). A variation introduced by the use of risk weights, which reflects differential mortality, was accommodated by adjusting the variance of the Poly-3 statistic as recommended by Bieler and Williams (1993). Tests of significance included pairwise comparisons of each dosed group with controls and a test for an overall dose-related trend.
RESULTS
Survival and Body Weights
The survival of all exposed groups of male and female rats and male and female mice was similar to that of the controls (Table 2), with the exception of 1.5% Aloe vera whole-leaf group of female rats where the mean survival (91.9 weeks) was significantly reduced compared with the control group (95.7 weeks; p = 0.044).
TABLE 2.
Mean Body Weight, Survival, Feed Intake, Water Consumption, and Estimated Daily Consumption of Aloe Vera Whole-Leaf Extract, Malic Acid, Aloin A, and Aloe-Emodin Administered to F344/N Rats and B6C3F1 Mice in the Drinking Water for 2 Years
| Male F344/N Rats | Female F344/N Rats | |||||||
|---|---|---|---|---|---|---|---|---|
| Aloe vera whole-leaf concentration (wt/wt) | 0% | 0.5% | 1.0% | 1.5% | 0% | 0.5% | 1.0% | 1.5% |
| Mean bw for study (g) | 457.5 | 452.2 | 436.6*** | 412.7*** | 276.7 | 276.4 | 260.1*** | 238.5*** |
| Mean survival for study (weeks) | 94.4 | 93.0 | 96.3 | 90.0 | 95.7 | 97.6 | 94.6 | 91.9* |
| Mean feed intake (g/day) | 18.9 | 18.5 | 18.6 | 17.8*** | 13.5 | 13.3 | 13.0*** | 12.3*** |
| Mean water consumption (g/day) | 21.7 | 22.5 | 27.0*** | 31.0*** | 17.9 | 18.2 | 19.1 | 20.4** |
| Mean water consumption (g/kg bw/day) | 47.6 | 49.7 | 61.8 | 75.1 | 64.8 | 65.7 | 73.4 | 85.3 |
| Mean Aloe vera whole-leaf extract consumption (g/kg bw/day) | 0 | 0.25 | 0.62 | 1.13 | 0 | 0.33 | 0.73 | 1.28 |
| Mean malic acid consumption (mg/kg bw/day)a | 0 | 49 | 122 | 223 | 0 | 65 | 145 | 253 |
| Mean aloin A consumption (mg/kg bw/day)a | 0 | 1.59 | 3.95 | 7.21 | 0 | 2.10 | 4.69 | 8.19 |
| Mean aloe-emodin consumption (mg/kg bw/day)a | 0 | 0.02 | 0.04 | 0.08 | 0 | 0.02 | 0.05 | 0.09 |
| Male B6C3F1 Mice | Female B6C3F1 Mice | |||||||
| Aloe vera whole-leaf concentration (wt/wt) | 0% | 1.0% | 2.0% | 3.0% | 0% | 1.0% | 2.0% | 3.0% |
| Mean bw for study (g) | 43.2 | 40.9** | 40.7** | 40.3*** | 36.7 | 37.9 | 37.4 | 35.7 |
| Mean survival for study (weeks) | 94.2 | 97.2 | 93.6 | 93.1 | 101.2 | 98.3 | 101.0 | 97.1 |
| Mean feed intake (g/day) | 6.3 | 6.4 | 6.8* | 6.6 | 5.3 | 5.6 | 5.7** | 5.7** |
| Mean water consumption (g/day) | 7.8 | 12.0*** | 14.2*** | 15.8*** | 5.4 | 8.3*** | 11.7*** | 14.1*** |
| Mean water consumption (g/kg bw/day) | 181 | 294 | 348 | 392 | 147 | 218 | 314 | 394 |
| Mean Aloe vera whole-leaf extract (g/kg bw/day) | 0 | 2.94 | 6.95 | 11.76 | 0 | 2.18 | 6.28 | 11.83 |
| Mean malic acid consumption (mg/kg bw/day)a | 0 | 582 | 1377 | 2329 | 0 | 431 | 1243 | 2343 |
| Mean aloin A consumption (mg/kg bw/day)a | 0 | 16.8 | 39.6 | 67.0 | 0 | 12.41 | 35.79 | 67.44 |
| Mean aloe-emodin consumption (mg/kg bw/day)a | 0 | 0.21 | 0.49 | 0.84 | 0 | 0.15 | 0.45 | 0.84 |
aThe Aloe vera leaf whole extract preparation contained 198mg malic acid/g Aloe vera whole leaf, 5.70mg aloin A/g Aloe vera whole leaf, and 0.07mg aloe-emodin/g Aloe vera whole leaf.
p Values that are significant are annotated with * to indicate p < 0.05, ** to indicate p < 0.01, or *** to indicate p < 0.001.
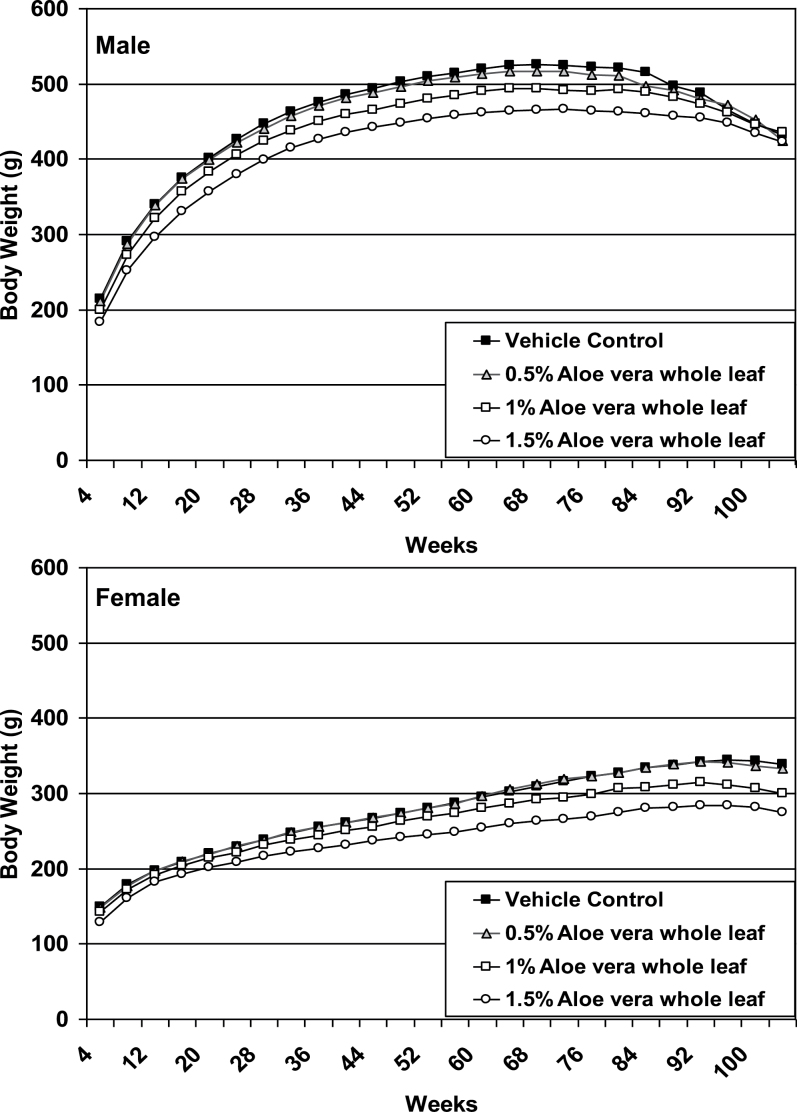
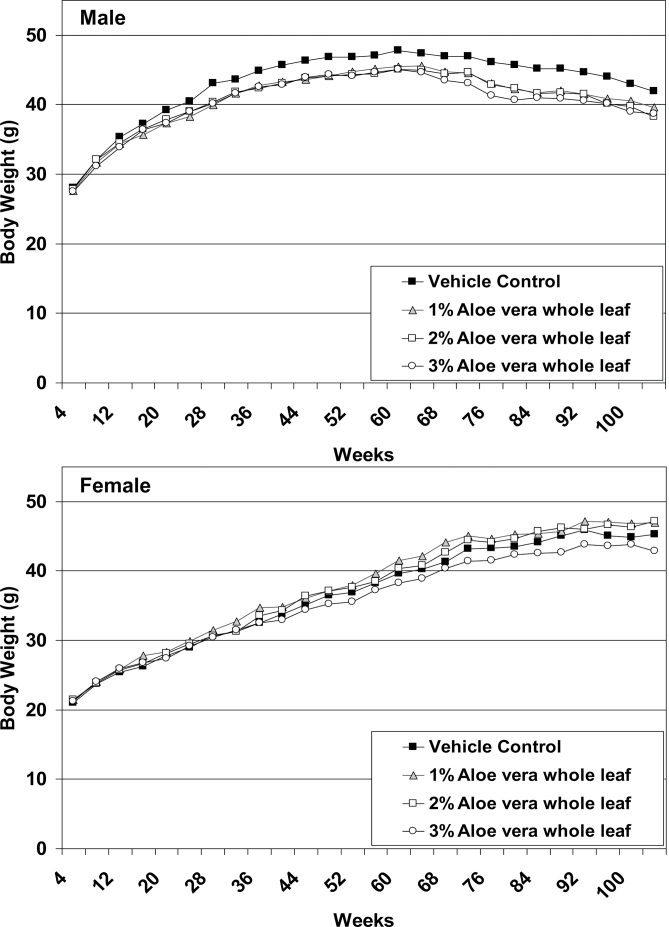
The mean body weights of rats and mice throughout the 2-year study are graphically depicted in 4-week increments in Fig. 2 and 3, respectively. Significant dose-related trend decreases in the body weights were observed in male and female rats throughout the study, and significantly lower body weights were observed for the 1 and 1.5% dose groups of rats when compared with controls (Table 2). Final mean body weights of the 1 and 1.5% dose of male rats were 95.4 and 90.2% and female rats were 94.0 and 86.2% of controls, respectively. Significant dose-related trend decreases in the body weights were observed in male mice throughout the study, and significantly lower body weights were observed for each Aloe vera exposed group when compared with controls (Table 2). Final mean body weights of the 2 and 3% doses of male mice were 92.0 and 90.7% of controls, respectively. The body weights of female mice were not affected by the Aloe vera treatment.
FIG. 2.
Growth curves of F344/N rats administered Aloe vera whole-leaf extract in the drinking water for 2 years.
FIG. 3.
Growth curves of B6C3F1 mice administered Aloe vera whole-leaf extract in the drinking water for 2 years.
Feed and Water Consumption
Feed consumption patterns were similar to controls in 0.5 and 1% groups of male and the 0.5% group of female rats and across all treatment groups of male and female mice (Table 2). When compared with controls, lower feed consumption values were observed for the 1% treatment group of female rats and the 1.5% treatment groups of male and female rats; mean feed consumptions relative to controls for 1.5% male and female rats were 94.1 and 90.9%, respectively (p < 0.001).
Polydipsia was pronounced in male and female rats and mice administered the Aloe vera whole-leaf extract (Table 2), and dose-trend increases in water consumption were observed throughout the study. Mean overall water consumptions (g/day) relative to control values for the 0.5, 1, and 1.5% dose groups of rats were 104, 124, and 143%, respectively, for male rats and 102, 107, and 114%, respectively, for female rats. Mean overall water consumptions (g/day) relative to control values for the 1, 2, and 3% dose groups of mice were 154, 182, and 203%, respectively, for male mice and 154, 217, and 261%, respectively, for female mice.
Water consumption was used to estimate compound consumption (Table 2). The mean consumption of Aloe vera whole-leaf extract in the 0.5, 1, and 1.5% dose groups of rats was 0.25, 0.62, and 1.13g/kg bw/day for male rats and 0.33, 0.73, and 1.28g/kg bw/day for female rats. The mean consumption of Aloe vera whole-leaf extract in the 1, 2, and 3% dose groups of mice was 2.94, 6.95, and 11.76g/kg bw/day for male mice and 2.18, 6.28, and 11.83g/kg bw/day for female mice.
Pathology and Histopathology
The major target organ in the Aloe vera whole-leaf 2-year carcinogenesis study was the large intestine of rats and mice. Few tissues, other than the intestine, demonstrated a positive dose-related response to the Aloe vera whole-leaf extract treatment, and the incidences in such tissues were relatively low. Because the 13-week study identified the colon as a potential target organ (Table 1), additional sampling sites of the rat intestinal tract were examined by histopathology, including the ileo-cecal and cecal-colic junction, the cecum, and the ascending, transverse, and descending colon.
Neoplastic findings—Rats.
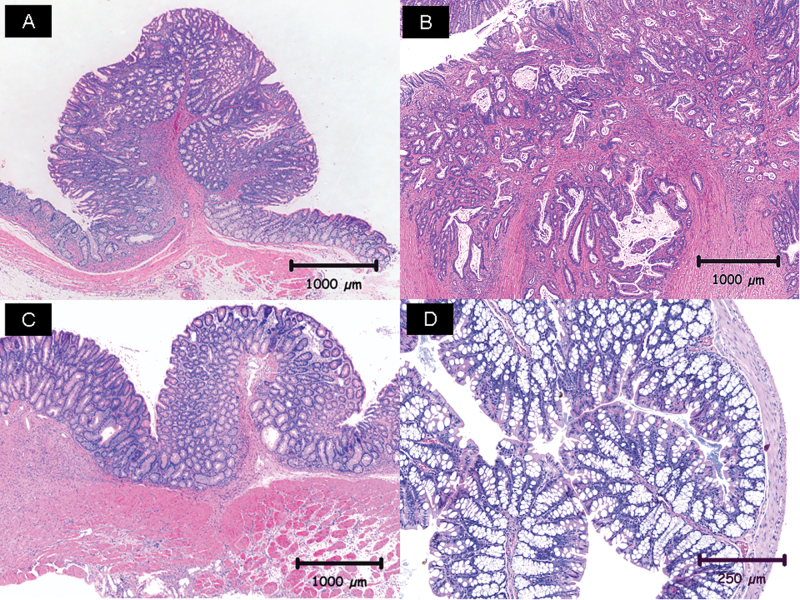
The incidences of neoplasms in male and female rats as related to the administration of the Aloe vera whole-leaf extract are summarized in Table 3. Histologically, adenomas of the large intestine were either pedunculated nodules that consisted of polyploid masses that protruded into the intestinal lumen or plaque-like lesions in the mucosa (Fig. 4A). Epithelial cells in adenomas were well-differentiated and resembled cells in adjacent hyperplastic mucosal epithelium; however, the adenomas formed distorted and sometimes coiled glandular arrangements and often demonstrated mild compression of adjacent mucosa. A histological diagnosis of carcinoma was based on invasion through the muscularis mucosa of the intestinal wall and anaplastic changes in the neoplastic epithelial cells, including hyperchromatic staining and distortion of cellular size and shape that were often accompanied by the production of abundant scirrhous stroma in invasive carcinoma (Fig. 4B).
Table 3.
Incidence of Neoplasms in the Large Intestine of Male and Female F344/N Rats Administered Aloe Vera Whole-Leaf Extract in the Drinking Water for 2 Yearsa
| Aloe vera whole-leaf extract (%)b | |||||
|---|---|---|---|---|---|
| Neoplasm | Sex | 0 | 0.5 | 1.0 | 1.5 |
| Ileo-cecal and cecal-colic junction adenoma | Male | 0/44 (0%)*** | 0/44 (0%) | 7/46 (15%)* | 10/41 (24%)*** |
| Female | 0/43 (0%)*** | 0/45 (0%) | 4/42 (10%)* | 5/39 (13%)* | |
| Ileo-cecal and cecal-colic junction carcinoma | Male | 0/44 (0%)** | 0/44 (0%) | 4/46 (9%) | 4/41 (10%) |
| Female | 0/43 (0%)** | 0/45 (0%) | 2/42 (5%) | 4/39 (10%)* | |
| Cecum adenoma | Male | 0/46 (0%)*** | 0/45 (0%) | 8/48 (17%)** | 8/48 (17%)** |
| Female | 0/47 (0%)*** | 0/48 (0%) | 1/47 (2%) | 6/48 (13%)* | |
| Ascending colon adenoma | Male | 0/47 (0%)*** | 0/47 (0%) | 19/48 (40%)*** | 8/46 (17%)** |
| Female | 0/47 (0%)** | 0/48 (0%) | 1/46 (2%) | 5/46 (11%)* | |
| Ascending colon carcinoma | Male | 0/47 (0%)*** | 0/47 (0%) | 4/48 (8%) | 8/46 (17%)** |
| Transverse colon adenoma | Male | 0/47 (0%)* | 0/47 (0%) | 6/47 (13%)* | 3/47 (6%) |
| Large intestine total adenoma | Male | 0/47 (0%)*** | 0/48 (0%) | 26/48 (54%)*** | 23/48 (48%)*** |
| Female | 0/48 (0%)*** | 0/48 (0%) | 6/48 (13%)* | 13/48 (27%)*** | |
| Large intestine total carcinoma | Male | 0/47 (0%)*** | 0/48 (0%) | 10/48 (21%)*** | 14/48 (29%)*** |
| Female | 0/48 (0%)** | 0/48 (0%) | 3/48 (6%) | 4/48 (8%)* | |
| Large intestine total adenoma or carcinomac | Male | 0/47 (0%)*** | 0/48 (0%) | 28/48 (58%)*** | 31/48 (65%)*** |
| Female | 0/48 (0%)*** | 0/48 (0%) | 8/48 (17%)** | 15/48 (31%)*** | |
aThe data are reported as the number of animals with a neoplasm per number of animals examined microscopically and the % incidence (in parentheses).
b p values that are significant are annotated with * to indicate p < 0.05, ** to indicate p <0.01, or *** to indicate p < 0.001. p values associated with the 0% Aloe vera whole-leaf incidence correspond to Poly-3 trend tests. p values associated with a specific treatment correspond to differences compared to the 0% Aloe vera whole-leaf incidence
cThe total number of rats with an adenoma, carcinoma, or adenoma or carcinoma in the ileo-cecal and cecal-colic junction, cecum, ascending colon, transverse colon, or descending colon.
FIG. 4.
Neoplasms and nonneoplastic lesions in the large intestine of F344/N rats and B6C3F1 mice treated with Aloe vera whole-leaf extract. (A) Large intestine section of an adenoma from a female rat treated with 1.5% Aloe vera whole-leaf extract; (B) large intestine section of a carcinoma from a male rat treated with 1.5% Aloe vera whole-leaf extract; (C) large intestine section of mucosal hyperplasia from a male rat treated with 1.5% Aloe vera whole-leaf extract; (D) colon section of goblet cell hyperplasia from a male mouse treated with 2.0% Aloe vera whole-leaf extract.
In male rats, there were significant dose-trend increases in the incidences of adenomas and carcinomas of the ileo-cecal and cecal-colic junction and ascending colon and increased incidences of adenomas of the cecum and transverse colon. When compared with controls, significantly higher incidences of adenomas of the ileo-cecal and cecal-colic junction, cecum, and ascending colon were observed for the 1 and 1.5% male rats. Higher incidences of adenomas of the transverse colon were observed for the 1% male rats, and significantly higher incidences of carcinomas of the ascending colon were observed for 1.5% male rats (Table 3). The inclusion of all adenomas of the large intestine, all carcinomas of the large intestine, or the combined total of adenomas or carcinomas of the large intestine resulted in significant dose-trend increases in the incidences for each of these categories of neoplasms, and significantly higher incidences were observed for the 1 and 1.5% Aloe vera whole-leaf male rat groups when compared with controls (Table 3). Adenomas or carcinomas in the cecum or colon have not been observed in F344/N control male rats (0/567) in bioassays conducted previously at NCTR.
Significant dose-trend increases in the incidences of adenomas and carcinomas of the ileo-cecal and cecal-colic junction and adenomas of the cecum and ascending colon were observed in female rats (Table 3). When compared with controls, significantly higher incidences of carcinomas of the ileo-cecal and cecal-colic junction and adenomas of ascending colon and cecum were observed for the 1.5% female rats. Significantly higher incidences of adenomas of the ileo-cecal and cecal-colic junction were observed for the 1 and 1.5% female rats. The inclusion of all adenomas of the large intestine, all carcinomas of the large intestine, or combined adenomas or carcinomas of the large intestine resulted in significant dose-trend increases in the incidences for each of these categories of neoplasms. When compared with controls, significantly higher incidences of adenomas and combined adenomas or carcinomas were found for the 1 and 1.5% groups of female rats, and significantly higher incidences of carcinomas of the large intestine were observed for the 1.5% group of female rats (Table 2). Adenomas or carcinomas in the cecum or colon have not been observed in F344/N control female rats (0/519) in bioassays conducted previously at NCTR.
Neoplastic findings—Mice.
There were no significant treatment-related increases in the incidences of neoplastic lesions in male or female mice.
Nonneoplastic findings—Rats.
The observed incidences and severity scores of nonneoplastic lesions are summarized for male and female rats in Table 4. Mucosal hyperplasia was a frequent finding in the large intestines of rats that consumed the Aloe vera whole-leaf extract in the drinking water (Fig. 4C). Mucosal intestinal hyperplasia was characterized by a thickening of the mucosa due to increased length and complexity of mucosal glands caused by the increased numbers of hyperplastic basophilic epithelial cells with goblet cell differentiation. The severities were greater and the incidences of mucosal hyperplasia were higher in the proximal (ascending and transverse colon) compared with the distal (descending colon) sites of the large intestine of rats—the same sites that had increased incidences of neoplasms.
TABLE 4.
Incidence of Nonneoplasic Lesions in Male and Female F344/N Rats Administered Aloe Vera Whole-Leaf Extract in the Drinking Water for 2 Yearsa
| Aloe vera whole-leaf extract (%)b | |||||
|---|---|---|---|---|---|
| Lesion | Sex | 0 | 0.5 | 1.0 | 1.5 |
| Forestomach stomach mucosa hyperplasia | Female | 1/48 (2%)**3.0 | 7/48 (15%)*2.6 | 10/48 (21%)**2.4 | 9/48 (19%)**2.3 |
| Glandular stomach mucosa hyperplasia | Male | 1/48 (2%)*2.0 | 12/47 (26%)***2.3 | 7/48 (15%)*2.4 | 11/48 (23%)**2.4 |
| Female | 0/48 (0%)*— | 1/48 (2%)2.0 | 3/48 (6%)2.3 | 3/48 (6%)2.0 | |
| Ileum mucosa hyperplasia | Female | 0/47 (0%)**— | 2/48 (4%)2.5 | 2/43 (5%)1.5 | 6/44 (14%)**2.5 |
| Jejunum mucosa hyperplasia | Male | 0/45 (0%)*— | 1/44 (2%)2.0 | 2/46 (4%)2.0 | 3/46 (7%)2.0 |
| Ileo-cecal and cecal-colic junction mucosa hyperplasia | Male | 0/44 (0%)***— | 29/44 (66%)***2.0 | 36/46 (78%)***2.5 | 32/41 (78%)***3.0 |
| Female | 0/43 (0%)***— | 30/45 (67%)***2.1 | 33/42 (79%)***2.5 | 32/39 (82%)***2.5 | |
| Cecum mucosa hyperplasia | Male | 0/46 (0%)***— | 13/45 (29%)***1.5 | 24/48 (50%)***1.9 | 25/48 (52%)***2.4 |
| Female | 0/47 (0%)***— | 4/48 (8%)1.8 | 17/47 (36%)***2.2 | 27/48 (56%)***2.2 | |
| Cecum dilatation | Male | 1/46 (2%)***—c | 0/45 (0%)— | 8/48 (17%)*—c | 17/48 (35%)***—c |
| Female | 0/47 (0%)***— | 0/48 (0%)— | 9/47 (19%)**—c | 25/48 (52%)***—c | |
| Asending colon mucosa hyperplasia | Male | 0/47 (0%)***— | 30/47 (64%)***1.9 | 38/48 (79%)***2.8 | 32/46 (70%)***3.2 |
| Female | 0/47 (0%)***— | 40/48 (83%)***2.0 | 35/46 (76%)***2.3 | 39/46 (85%)***2.6 | |
| Transverse colon mucosa hyperplasia | Male | 0/47 (0%)***— | 30/47 (64%)***1.8 | 42/47 (89%)***2.2 | 34/47 (72%)***2.4 |
| Female | 0/47 (0%)***— | 40/48 (83%)***1.7 | 33/46 (72%)***1.8 | 42/46 (91%)***2.1 | |
| Desending colon mucosa hyperplasia | Male | 0/47 (0%)***— | 17/46 (37%)***1.5 | 31/46 (67%)***1.6 | 30/47 (64%)***1.7 |
| Female | 0/47 (0%)***— | 17/48 (35%)***1.4 | 18/46 (39%)***1.4 | 27/47 (57%)***1.5 | |
| Rectum mucosa hyperplasia | Male | 0/47 (0%)*— | 1/47 (2%)1.0 | 1/48 (2%)2.0 | 4/48 (8%)2.0 |
| Female | 0/48 (0%)**— | 0/48 (0%)— | 0/47 (0%)— | 5/47 (11%)*1.6 | |
| Large intestine all sites mucosa hyperplasiad | Male | 0/47 (0%)***— | 35/48 (73%)***2.2 | 48/48 (100%)***3.1 | 41/48 (85%)***3.4 |
| Female | 0/48 (0%)***— | 42/48 (88%)***2.3 | 42/48 (88%)***2.8 | 45/48 (94%)***3.0 | |
| Mesenteric lymph node cystic degeneration | Male | 8/47 (17%)***2.5 | 11/48 (23%)2.8 | 42/48 (88%)***3.8 | 41/48 (85%)***3.6 |
| Female | 0/46 (0%)***— | 16/47 (34%)***3.2 | 40/48 (83%)***3.8 | 43/47 (92%)***3.5 | |
aThe data are reported as the number of animals with a lesion per number of animals examined microscopically, the % incidence (in parentheses), and the mean severity of the lesion, where 1 = minimal, 2 = mild, 3 = moderate, 4 = marked.
b p values that are significant are annotated with * to indicate p < 0.05, ** to indicate p <0.01, or *** to indicate p < 0.001. p values associated with the 0% Aloe vera whole-leaf incidence correspond to Poly-3 trend tests. p values associated with a specific treatment correspond to differences compared to the 0% Aloe vera whole-leaf incidence.
cSeverity not indicated. Lesion reported as present or absent.
dTotal number of rats with mucosa hyperplasia in the cecum, ascending colon, transverse colon, descending colon, or rectum.
In male and female rats, significant dose-trend increased incidences of mucosal hyperplasia were observed in the ileo-cecal and cecal-colic junction, cecum, and ascending, transverse, and descending colon. When compared with controls, significant increased incidences of mucosal hyperplasia were observed at all doses levels for the ileo-cecal and cecal-colic junction, and ascending, transverse, and descending colon of male and female rats. An increased incidence of mucosal hyperplasia was observed in the cecum at all doses of Aloe vera whole-leaf extract in male rats and in the 1 and 1.5% dose groups in female rats. Significant dose-trend increased incidences of mucosal hyperplasia were also observed for the forestomach, glandular stomach, ileum, and the rectum in female rats and for the glandular stomach, jejunum, and rectum of male rats.
Dose-related increases in cecal dilatation was observed in male and female rats, with significantly higher incidences in the 1 and 1.5% Aloe vera whole-leaf groups. Degeneration and atrophy of mesenteric lymph nodes also showed significant dose-trend increases.
Nonneoplastic findings—Mice.
The observed incidences and severity scores of nonneoplastic lesions are summarized for male and female mice in Table 5. Treatment-related nonneoplastic lesions appeared primarily in the colon of mice as goblet cell hyperplasia. The diagnosis of goblet cell hyperplasia was characterized by the crypts and glands of the colon being lined by an increased number of well-differentiated goblet cells with excess mucus on the luminal surface (Fig. 4D). In male and female mice alike, significant dose-trend increased incidences of goblet cell hyperplasia were observed in the ascending, transverse, and descending colon. When compared with controls, significantly increased incidences of goblet cell hyperplasia were observed for each dose level of the Aloe vera whole-leaf extract at each site of the colon examined, with the exception of the descending colon in the 0.5% group of female mice. Average severity scores for goblet cell hyperplasia tended to increase similarly with the dose of Aloe vera whole-leaf extract administered to male and female mice.
TABLE 5.
Incidence of Nonneoplasic Lesions in Male and Female B6C3F1 Mice Administered Aloe Vera Whole-Leaf Extract in the Drinking Water for 2 Yearsa
| Aloe vera whole-leaf extract (%)b | |||||
|---|---|---|---|---|---|
| Lesion | Sex | 0 | 1.0 | 2.0 | 3.0 |
| Asending colon goblet cell hyperplasia | Male | 2/47 (4%)***1.0 | 16/44 (36%)***1.3 | 20/45 (44%)***1.6 | 19/42 (45%)***1.6 |
| Female | 1/43 (2%)***1.0 | 15/43 (35%)***1.2 | 20/44 (46%)***1.3 | 25/43 (58%)***1.7 | |
| Tranvserse colon goblet cell hyperplasia | Male | 4/47 (9%)***1.0 | 14/44 (32%)***1.4 | 21/45 (47%)***1.7 | 22/43 (51%)***1.6 |
| Female | 2/42 (5%)***1.0 | 18/42 (43%)***1.2 | 23/44 (52%)***1.3 | 26/43 (61%)**1.7 | |
| Decending colon goblet cell hyperplasia | Male | 0/47 (0%)***— | 7/44 (16%)**1.3 | 12/45 (27%)***1.5 | 17/43 (40%)***1.4 |
| Female | 0/43 (0%)***— | 4/43 (9%)1.3 | 7/44 (16%)**1.4 | 17/43 (40%)***1.6 | |
| Large intestine all sites goblet cell hyperplasiac | Male | 4/47 (9%)***1.0 | 17/44 (39%)***1.4 | 22/45 (49%)***1.9 | 22/44 (50%)1.7 |
| Female | 3/43 (7%)***1.0 | 19/43 (44%)***1.2 | 24/44 (55%)***1.3 | 28/43 (65%)***1.7 | |
| Mesenteric lymph node cellular infiltration | Male | 0/48 (0%)**— | 1/45 (2%)3.0 | 4/45 (9%)2.3 | 6/43 (14%)*3.2 |
| Nose hyaline droplets | Male | 6/48 (13%)*1.2 | 31/47 (66%)***1.8 | 39/47 (83%)***2.0 | 13/47 (28%)1.8 |
aThe data are reported as the number of animals with a lesion per number of animals examined microscopically, the % incidence (in parentheses), and the mean severity of the lesion, where 1 = minimal, 2 = mild, 3 = moderate, 4 = marked.
b p values that are significant are annotated with * to indicate p < 0.05, ** to indicate p <0.01, or *** to indicate p < 0.001. p values associated with the 0% Aloe vera whole-leaf incidence correspond to Poly-3 trend tests. p values associated with a specific treatment correspond to differences compared to the 0% Aloe vera whole-leaf incidence.
cTotal number of mice with goblet cell hyperplasia in the ascending colon, transverse colon, or descending colon.
In association with goblet cell hyperplasia of the colon, cellular infiltration of the mesenteric lymph nodes showed significant dose-related increases, and significantly higher cellular infiltration was observed in the mesenteric lymph nodes of the 3.0% Aloe vera whole-leaf group of male mice when compared with the controls (Table 5). The accumulation of hyaline droplets in the nasal cavity also showed a significant dose response and levels were significantly higher in the 1 and 2% groups of male mice. Hyaline droplets are a commonly observed nonspecific change in the epithelial lining of the nasal cavity, usually representing a nonspecific adaptive response to an irritant.
Discussion
This study demonstrates the diverse responses that can occur in the gastrointestinal tract from long-term ingestion of a herbal remedy that consumers deem safe because it is a natural plant product.
In the 2-year mouse study, there were no treatment-related effects on the survival of mice (Table 2), and the changes in body weights (Table 2) were not considered of biological significance. Polydipsia was a pronounced Aloe vera whole-leaf dose-related phenomenon observed in dosed mice that resulted in water consumption amounts of greater than 200% relative to controls and average daily doses of approximately 11.8g Aloe vera whole leaf per kg bw per day for mice in the 3.0% dose groups (Table 2). Goblet cell hyperplasia of the large intestine was a prominent nonneoplastic lesion, and treatment-related increased incidences of goblet cell hyperplasia were observed in the colon of male and female mice. There were no treatment-related neoplasms in mice.
Goblet cell hyperplasia and increased mucus production are features of compensatory growth of the intestinal tract after surgical shortening and in ulcerative colitis and Crohn’s disease (Ehsanullah et al., 1982; Kilgore et al., 2000; Olubuyide et al., 1984). Moreover, ulcerative colitis and inflammatory bowel disease predispose humans to intestinal cancer, and small-bowel resection enhances colorectal carcinogenesis in rats (Prior et al., 1982; Sigel et al., 1999; Williamson et al., 1982). Vaiphei et al. (2004) evaluated biopsies from patients with long-standing (five or more years) idiopathic ulcerative colitis and correlated the incidence of atypical epithelium, goblet cell hyperplasia, and disease duration with the expression of genes known to play a role in cell cycle control and apoptosis. Of the factors evaluated, only goblet cell hyperplasia showed strong correlations with disease duration, p53 gene expression—a tumor suppressor gene that has an important role in cell cycle control and apoptosis, and argyrophilic nucleolar organizer regions index—a prognostic indicator of early cancer development (Ribeiro Rodrigues et al., 1997). Lee (1988) examined histologically the entire colonic mucosa of 51 cases of colorectal carcinoma. In 80% of the cases, goblet cell hyperplasia was particularly prominent in the mucosa immediately adjacent to the carcinoma; the mucosa further away from the carcinoma was less frequently (51%) affected. The results of these studies suggest that goblet cell hyperplasia may indicate the presence of epithelial cell dysplasia, a precancerous change.
In the 2-year rat study, the survival of all exposed groups of rats was similar to controls, with the exception that lower survival was observed for the 1.5% female rats. A major contributor to early death in this group was cecal dilatation, which was the probable cause of death for 12 animals. As observed in the 2-year mouse study, treatment-related increases in water consumption were observed in rats although the effects on water consumption were less marked in rats. Polydipsia was more evident in males than in females; the average daily amount of water consumed by 1.5% Aloe vera whole-leaf dose group of male rats was greater than 143% of control values, whereas that of female rats from the same treatment group was 114% (Table 2).
Mucosal hyperplasia was observed throughout the large intestine of rats, with dose-related increases in incidences and severities. Higher incidences of mucosal hyperplasia were observed in the proximal compared with the distal colon and, in this respect, were similar to the incidence patterns of colonic goblet cell hyperplasia that was observed in the 13-week study (Table 1).
Because rodents do not usually develop spontaneous neoplasms of the colon, carcinogen induction of neoplasms in rodent colons has been used as a model for human colon cancer development and for evaluating chemopreventive regimens (Holt et al., 1996; Tanaka, 2009). A review of the National Toxicology Program database and the Carcinogenic Potency Database indicated that the most commonly induced tumors of the rodent gastrointestinal tract are squamous neoplasms of the forestomach in mice and intestinal carcinoma of the colon in rats (Chandra et al., 2010). In this 2-year rat study, treatment-related neoplasms were limited to the large intestine and occurred as adenomas and carcinomas in the ileo-cecal junction, cecum, and the ascending and transverse colons of the male and female rats. The neoplasms were confined within the mucosal wall of the large intestine and did not metastasize to regional mesenteric lymph nodes or more distant sites. Higher incidences of neoplastic lesions occurred in the proximal sites of the large intestine than in more distal sections, and no neoplasms occurred in the rectum of either sex or in the large intestine of the 0.5% Aloe vera whole-leaf groups. In high-incidence countries of North America and Europe, human colon cancer occurs predominantly in the lower (distal) colon, which may reflect the larger population of gut microflora at this site capable of metabolizing xenobiotics (Kune et al., 1986).
The carcinogenic response to Aloe vera whole-leaf administration was greater in male rats than in female rats. For example, male rats administered 1.0% Aloe vera whole-leaf extract (0.62g Aloe vera whole-leaf extract per kg bw per day) had a higher incidence (58%) of combined adenoma or carcinoma when compared with the incidence (17%) of female rats administered 1.0% Aloe vera whole-leaf extract (0.73g Aloe vera whole-leaf extract per kg bw per day). A similar differential existed in male and female rats administered the 1.5% Aloe vera whole-leaf extract. On the other hand, the incidences of nonneoplastic lesions, i.e., mucosal hyperplasia, were similar among male and female rats.
The Aloe vera whole-leaf extract used in these studies contained the components of the Aloe vera gel and Aloe vera latex. Many of the polysaccharides in Aloe gel are polydispersed β-(1→4)-linked glucomannans, mannans, or pectins of a wide range of molecular weights and interspersed with O-acetyl groups (Tanaka et al., 2006). Due to the β-glycosidic linkage between sugar moieties (primarily mannose and glucose), many of these nonstarch polysaccharides, like cellulose, are resistant to hydrolysis by acid in the stomach and α-glucosidase activity in the small intestine and reach the colon as undigested fiber, where they may be fermented by the colonic microflora.
Most small herbivorous birds and some omnivorous mammals, such as rats and other rodents, compensate for a limited gut capacity and a higher rate of metabolism by selective retention of fluid and small particles in their cecum (Johnson et al., 1960). Rodents and herbivorous monogastric species of vertebrates, such as rabbits and horses, obtain a substantial portion of their nutrients by the retention and microbial fermentation of plant material in the cecum. In this respect, the cecum is somewhat analogous to the bovine rumen and serves as an important organ of absorption (Stevens and Hume, 1998). Dietary components incompletely digested and/or absorbed in the small intestine, such as cellulose, give rise to an increased amount of osmotically active material in the intestinal contents. The increase in the amount of osmotically active material results in an increase in water retention, so the animals tend to drink more fluid, and the cecum distends in size due to the increase in contents. The muscular contractions of the cecum pass digested and incompletely digested dietary bulk to the next region of the large intestine, the proximal colon. Evidence suggests that the rate at which fluid and small particles leave the cecum is determined by the rate of cecal fermentation and the degree of fluid distention (Stevens and Hume, 1998). Cecal dilatation (enlargement) is a physiological adaptation process that in itself is of no toxicological significance; however, side effects of cecal impaction and severe diarrhea have detrimental effects on the health of animals (Jain et al., 2007; Johnson et al., 1960).
Dilatation of the rodent cecum, often accompanied with severe diarrhea, has been reported for a variety of compounds (Birnbaum et al., 1986; Courtney, 2000; Leegwater et al., 1974; Smits-Van Prooije et al., 1990; Til et al., 1986). Polydipsia, diarrhea, and cecal dilatation were common observances in this study, and cecal dilatation was the noted cause of death for a number of rats. Cecal dilatation may have resulted from an accumulation of undigested Aloe vera whole-leaf carbohydrates or volatile gases produced by microbiota in their efforts to digest the β-glycosidic linked carbohydrates. Cecal impaction and diarrhea were observed in rats in this 2-year study. These effects were not observed by Ikeno et al. (2002) during the life-long administration to F344/N rats of whole-leaf charcoal–processed Aloe vera (0.02%) in the drinking water or when the rats were fed diets containing 1.0% Aloe gel or 1.0% charcoal-processed Aloe gel. In the production of charcoal-processed Aloe gel, the anthraquinone components of Aloe latex are removed; the process also removes some of the high-molecular-weight polysaccharides of the inner leaf Aloe gel (Waller et al., 2004). The lower concentration of Aloe vera materials in the Ikeno et al. (2002) study plus the loss of some of the polysaccharides may have prevented the effects observed in the present study.
Due to the β-glycosidic linkage between the sugar and the anthracene ring structure and the hydrophilic nature of the molecules, the anthraquinone C-glycosides in Aloe vera latex are protected after oral administration from acid hydrolysis in the stomach and enzymatic activity in small intestine and are transported unabsorbed to the cecum of rats, where Eubacterium sp. act upon the C-glycoside anthranoids to release glucose and the free aglycone (Dreessen and Lemli, 1988; Dreessen et al., 1981; Hattori et al., 1993; van Gorkom et al., 1999). Studies have shown that the cathartic effects of the Aloe vera latex are not due to the ingested form of the C-glycoside anthraquinone, aloin, but rather to the aglycone, aloe-emodin-9-anthrone, formed by bacterial metabolism of the aloin (Akao et al., 1996). The Eubacterium sp. is expressed differentially across mammalian species, e.g., humans > rats > mice; therefore, not all mammalian species are capable of transforming aloin to the aloe-emodin anthrone (Canny and McCormick, 2008; EMEA, 2007).
The potency of aloin to exert cathartic activities is known to vary across animal species, e.g., aloin shows purgative potency in humans but has little activity in the rat and mouse (Che et al., 1991; Hattori et al., 1988; Joshi, 1998). Therefore, whether aloin is metabolized to its pugative principle in amounts sufficient to induce catharsis by microflora in the rat large intestine is uncertain. Soft and mud-like feces and neoplasms in rat colons were observed in this 2-year study, suggesting that the presence of Aloe latex in the drinking water may be a causative cathartic and/or carcinogenic factor in rats. Similar findings were observed in rats that received dietary administration of A. arborescens Miller, a species of Aloe used commercially as a food additive. Shimpo et al. (2001) studied the modifying effects of freeze-dried whole-leaf A. arborescens Miller var. natalensis Berger on azoxymethane-induced intestinal carcinogenesis in male F344 rats fed diets containing 1 or 5% A. arborescens whole leaf for 5 weeks. The 5% A. arborescens whole-leaf dose level decreased body weights and induced soft feces in rats; however, both 1 and 5% A. arborescens whole leaf–enriched diets were found to offer protection from azoxy- methane-induced intestinal carcinogenesis.
The same species and variety of Aloe, A. arborescens Miller, was used for assessment of toxicity and carcinogenic potential in 1- and 2-year studies in Wistar Hannover rats (Matsuda et al., 2008; Yokohira et al., 2009). In the 1-year study, the A. arborescens whole-leaf extract was added to the basal diet of the rats at 0, 0.16, 0.8, and 4.0%, and both male and female rats showed diarrhea, reduced body weight gains, and severe sinus dilatation of the ileo-cecal lymph nodes (Matsuda et al., 2008). In the 2-year studies, rats received A. arborescens whole-leaf extract at concentrations of 0, 0.8, and 4.0% in the diet (Yokohira et al., 2009). Diarrhea or loose stools, decreased body weights, severe sinus dilatation in the ileo-cecal lymph, and adenomas and adenocarcinomas of the large intestine developed in the 4% dose group of rats. The effects and lesions found in the 2-year study of A. arborescens Miller were remarkably similar, albeit to a much lesser degree of severity, as those found in the present 2-year study on Aloe vera.
The associations between colorectal cancer risk and anthraquinone laxative use remain controversial (Nascimbeni et al., 2002; WHO-IARC, 2002; Willems et al., 2003). It has been well documented that 1,8-dihydroxyanthraquinone (danthrone) exerts tumor-promoting effects and tumorigenic activities in the large intestine of rodents (Mori et al., 1985 , 1990). Furthermore, Nishikawa et al. (1997) showed that danthrone enhanced epithelial mucosal cell replication in the large intestine, especially in the cecum of rats, and was associated with elevated prostaglandin E2 levels that correlated with the dose of danthrone and the severity of diarrhea. Paradoxically, antitumorigenic effects are equally well documented for some anthraquinones (El-Shemy et al., 2010; Grimaudo et al., 1997; Zhao et al., 1999). A purified senna extract did not show any carcinogenic potential when administered via the drinking water at daily doses of 0, 5, 15, and 25mg/kg bw to male and female Sprague Dawley rats for 2 years (Lydén-Sokolowski et al., 1993).
Increased incidences of mesenteric lymph node hyperplasia and degeneration were also observed in rats exposed to the Aloe vera whole-leaf extract, suggesting that the Aloe vera whole-leaf extract might induce an immune response. Microscopic examination of the enlarged cystic lymph nodes of rats revealed dilated medullary sinuses. The mesenteric lymph nodes of rats exposed to the Aloe vera whole-leaf extract appeared to have reduced numbers of lymphoid cells, likely a result of the dramatically enlarged fluid-filled cystic nodes. In rodents, lymph node hyperplasia may be found to varying degrees depending upon the age and health status of the animal, the location of the lymph node, or due to stimulation by antigens in the intestinal tract (Elmore, 2006a ,b). Lymph node hyperplasia is generally a reactive or immune response and is not considered a preneoplastic lesion (Cesta, 2006). Neither gross examination nor microscopic evaluation revealed the pathogenesis of this lesion in affected rats, suggesting that the increased incidences of mesenteric lymph node hyperplasia and degeneration may have been due to test article irritation of the intestinal tract, rather than an immune response.
The whole-leaf extract of the Aloe vera plant contains Aloe gel from the inner leaf pulp and Aloe latex from the leaf pericyclic tubules. Both of these components, separately or synergistically, may have played a role in the development of colon cancer in rats in this 2-year study. The constituents of Aloe gel and Aloe latex are each composed of β-linked glycosyl residues that, like cellulose, reach the large intestine in mostly undigested form. Rats have a large cecum that serves as the principal site of microbial fermentation, and the microflora in the rat cecum have been shown capable of metabolizing β-linked glycosyl residues.
There is some debate in the literature as to whether the fermentability of a fiber plays a role in its protection or promotion of colon carcinogenesis (Hamer et al., 2008; Lupton, 2004). Additionally, there is a strong association with an increased risk of colon carcinoma and anthranoid self-medication for constipation and purgative purposes (Nascimbeni et al., 2002; Siegers et al., 1993b; van Gorkom et al., 1999).
The combined results from this study suggest that the long-term exposure of rats to the Aloe vera whole-leaf extract induced an insult to the intestinal tract and caused a progression in lesion types from goblet cell hyperplasia to mucosal hyperplasia to adenoma and carcinoma in the large intestine. Additional investigations are planned to determine whether the exposure of rats to Aloe vera gel or Aloe vera decolorized whole-leaf extracts elicits similar responses in the gastrointestinal tract as those observed with Aloe vera whole-leaf extract.
Funding
Interagency Agreement Nos. 224-12-0003 and AES12013 between the National Center for Toxicological Research/Food and Drug Administration and the National Institute of Environmental Health Sciences/National Toxicology Program.
This study formed the basis of NTP Technical Report 577. The views presented in this article do not necessarily reflect those of the Food and Drug Administration.
References
- Akao T., Che Q.-M., Kobashi K., Hattori M., Namba T. (1996). A purgative action of barbaloin is induced by Eubacterium sp. strain BAR, a human intestinal anaerobe, capable of transforming barbaloin to aloe-emodin anthrone. Biol. Pharm. Bull. 19: 136–138. [DOI] [PubMed] [Google Scholar]
- Atherton P. (1998). Aloe vera: Magic or medicine? Nurs. Stand. 12: 49–52, 54. [DOI] [PubMed] [Google Scholar]
- Ayushveda (2010). Aloe Drink - Benefits of Aloe vera Juice Available at: http://www.us.ayushveda.com/aloe-dring-benefits-of-aloe-vera-juice/ Ayushveda Infomatics: Panchkula, Haryana, India: Accessed March 2, 2010. [Google Scholar]
- Bailer A. J., Portier C. J. (1988). An illustration of dangers of ignoring survival differences in carcinogenic data. J. Appl. Toxicol. 8: 185–189. [DOI] [PubMed] [Google Scholar]
- Bieler G. S., Williams R. L. (1993). Ratio estimates, the delta method, and quantal response tests for increased carcinogenicity. Biometrics 49: 793–801. [PubMed] [Google Scholar]
- Birch A. J., Donovan F. W. (1955). Barbaloin. I. Some observations on its structure. Aust. J. Chem. 8: 523–528. [Google Scholar]
- Birnbaum L. S., Deskin R., Grumbein S. L., Kurtz P., Fowler K. L., Peters A. C. (1986). Prechronic toxicity of o-benzyl-p-chlorophenol in rats and mice. Fundam. Appl. Toxicol. 7: 615–625. [DOI] [PubMed] [Google Scholar]
- Bisi-Johnson M. A., Obi C. L., Hattori T., Oshima Y., Li S., Kambizi L., Eloff J. N., Vasaikar S. D. (2011). Evaluation of the antibacterial and anticancer activities of some South African medicinal plants. BMC Complement. Altern. Med. 11: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boorman G. A., Eustis S. L. (1986). The pathology working group as a means for assuring pathology quality in toxicologic studies. In Managing Conduct and Data Quality of Toxicologic Studies (Hoover B. K., Baldwin J. K., Uelner A. F., Whitmire C. E., Davis C. L., Bristol D. W, Eds.), pp. 271–275 Princeton Scientific Publishing Co., Inc., Princeton, NJ: [Google Scholar]
- Boudreau M. D., Beland F. A. (2006). An evaluation of the biological and toxicological properties of Aloe barbadensis Miller, Aloe vera. J. Environ. Sci. Health. C. Environ. Carcinog. Ecotoxicol. Rev. 24: 103–154. [DOI] [PubMed] [Google Scholar]
- Briggs C. (1995). Herbal medicine: Aloe. CPJ 128: 48–50. [Google Scholar]
- Canny G. O., McCormick B. A. (2008). Bacteria in the intestine, helpful residents or enemies from within? Infect. Immun. 76: 3360–3373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cesta M. F. (2006). Normal structure, function, and histology of mucosa-associated lymphoid tissue. Toxicol. Pathol. 34: 599–608. [DOI] [PubMed] [Google Scholar]
- Chandra S. A., Nolan M. W., Malarkey D. E. (2010). Chemical carcinogenesis of the gastrointestinal tract in rodents: An overview with emphasis on NTP carcinogenesis bioassays. Toxicol. Pathol. 38: 188–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Che Q.-M., Akao T., Hattori M., Kobashi K., Namba T. (1991). Isolation of a human intestinal bacterium capable of transforming barbaloin to aloe-emodin anthrone. Planta Med. 57: 15–19. [DOI] [PubMed] [Google Scholar]
- Chow J. T.-N., Williamson D. A., Yates K. M., Goux W. J. (2005). Chemical characterization of the immunomodulating polysaccharide of Aloe vera L. Carbohydr. Res. 340: 1131–1142. [DOI] [PubMed] [Google Scholar]
- Courtney C. L. (2000). Cecal torsion in rodents associated with chronic administration of clinafloxacin. Toxicol. Pathol. 28: 643–648. [DOI] [PubMed] [Google Scholar]
- Dreessen M., Eyssen H., Lemli J. (1981). The metabolism of sennosides A and B by the intestinal microflora: In vitro and in vivo studies on the rat and the mouse. J. Pharm. Pharmacol. 33: 679–681. [DOI] [PubMed] [Google Scholar]
- Dreessen M., Lemli J. (1988). Studies in the field of drugs containing anthraquinone derivatives. XXXVI. The metabolism of cascarosides by intestinal bacteria. Pharm. Acta Helv. 63: 287–289. [PubMed] [Google Scholar]
- Ehsanullah M., Filipe M. I., Gazzard B. (1982). Mucin secretion in inflammatory bowel disease: Correlation with disease activity and dysplasia. Gut 23: 485–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Shemy H. A., Aboul-Soud M. A. M., Nassr-Allah A. A., Aboul-Enein K. M., Kabash A., Yagi A. (2010). Antitumor properties and modulation of antioxidant enzymes’ activity by Aloe vera leaf active principles isolated via supercritical carbon dioxide extraction. Curr. Med. Chem. 17: 129–138. [DOI] [PubMed] [Google Scholar]
- Elmore S. A. (2006a). Enhanced histopathology of mucosa-associated lymphoid tissue. Toxicol. Pathol. 34: 687–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elmore S. A. (2006b). Histopathology of the lymph nodes. Toxicol. Pathol. 34: 425–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EMEA (2007). Committee on Herbal Medicinal Products (HMPC). Assessment Report on Aloe barbadensis Miller and Aloe (Various Species, Mainly Aloe ferox Miller and Its Hybrids). Evaluation of Medicines for Human Use, pp. 1–24 European Medicines Agency,London, England. [Google Scholar]
- Femenia A., Sánchez E. S., Simal S., Rosselló C. (1999). Compositional features of polysaccharides from Aloe vera (Aloe barbadensis Miller) plant tissues. Carbohydr. Polym. 39: 109–117. [Google Scholar]
- Fogleman R. W., Chapdelaine J. M., Carpenter R. H., McAnalley B. H. (1992a). Toxicologic evaluation of injectable acemannan in the mouse, rat and dog. Vet. Hum. Toxicol. 34: 201–205. [PubMed] [Google Scholar]
- Fogleman R. W., Shellenberger T. E., Balmer M. F., Carpenter R. H., McAnalley B. H. (1992b). Subchronic oral administration of acemannan in the rat and dog. Vet. Hum. Toxicol. 34: 144–147. [PubMed] [Google Scholar]
- Gorloff D. R. (1983). Study of the organoleptic properties of the exuded mucilage from Aloe barbadensis leaves. Erde Internat 1: 46–59. [Google Scholar]
- Gowda D. C., Neelisiddaiah B., Anjaneyalu Y. V. (1979). Structural studies of polysaccharides from Aloe vera . Carbohydr. Res. 72: 201–205. [Google Scholar]
- Grimaudo S., Tolomeo M., Gancitano R., D’Alessandro N., Aiello E. (1997). Effects of highly purified anthraquinoid compounds from Aloe vera on sensitive and multidrug resistant leukemia cells. Oncol. Rep. 4: 341–343. [DOI] [PubMed] [Google Scholar]
- Hamer H. M., Jonkers D., Venema K., Vanhoutvin S., Troost F. J., Brummer R.-J. (2008). Review article: The role of butyrate on colonic function. Aliment. Pharmacol. Ther. 27: 104–119. [DOI] [PubMed] [Google Scholar]
- Hattori M., Akao T., Kobashi K., Namba T. (1993). Cleavages of the O- and C-glucosyl bonds of anthrone and 10,10’-bianthrone derivatives by human intestinal bacteria. Pharmacology 47:(Suppl. 1)125–133. [DOI] [PubMed] [Google Scholar]
- Hattori M., Kanda T., Shu Y.-Z., Akao T., Kobashi K., Namba T. (1988). Metabolism of barbaloin by intestinal bacteria. Chem. Pharm. Bull. 36: 4462–4466. [DOI] [PubMed] [Google Scholar]
- Hay J. E., Haynes L. J. (1956). The aloins. Part I. The structure of barbaloin. J. Chem. Soc 3141–3147. [Google Scholar]
- Hecht A. (1981). The overselling of Aloe vera. FDA Consumer 15: 26–29. [Google Scholar]
- Herlihy J. T., Bertrand H. A., Kim J. D., Ikeno Y., Yu B. P. (1998a). Effects of Aloe vera ingestion in the rat. I. Growth, food and fluid intake and serum chemistry. Phytother. Res. 12: 183–188. [Google Scholar]
- Herlihy J. T., Kim J. D., Kalu D. N., Nelson J. F., Ward W. F., Ikeno Y., Yu B. P. (1998b). Effects of Aloe vera ingestion in the rat. II. Hormonal and metabolic characteristics. Phytother. Res. 12: 355–360. [Google Scholar]
- Holt P. R., Mokuolu A. O., Distler P., Liu T., Reddy B. S. (1996). Regional distribution of carcinogen-induced colonic neoplasia in the rat. Nutr. Cancer 25: 129–135. [DOI] [PubMed] [Google Scholar]
- Ikeno Y., Hubbard G. B., Lee S., Yu B. P., Herlihy J. T. (2002). The influence of long-term Aloe vera ingestion on age-related disease in male Fischer 344 rats. Phytother. Res. 16: 712–718. [DOI] [PubMed] [Google Scholar]
- Jain A., Gupta Y., Jain S. K. (2007). Perspectives of biodegradable natural polysaccharides for site-specific drug delivery to the colon. J. Pharm. Pharmaceut. Sci. 10: 86–128. [PubMed] [Google Scholar]
- Johnson R. B., Peterson D. A., Tolbert B. M. (1960). Cellulose metabolism in the rat. J. Nutr. 72: 353–356. [DOI] [PubMed] [Google Scholar]
- Joshi S. P. (1998). Chemical constituents and biological activity of Aloe barbadensis - a review. J. Med. Arom. Plant. Sci. 20: 768–773. [Google Scholar]
- Kilgore S. P., Sigel J. E., Goldblum J. R. (2000). Hyperplastic-like mucosal change in Crohn’s disease: An unusual form of dysplasia? Mod. Pathol. 13: 797–801. [DOI] [PubMed] [Google Scholar]
- Klein A. D., Penneys N. S. (1988). Aloe vera. J. Am. Acad. Dermatol. 18: 714–720. [DOI] [PubMed] [Google Scholar]
- Kune S., Kune G. A., Watson L. (1986). The Melbourne colorectal cancer study: Incidence findings by age, sex, site, migrants and religion. Int. J. Epidemiol. 15: 483–493. [DOI] [PubMed] [Google Scholar]
- Logarto Parra A., Silva Yhebra R., Guerra Sardiñas I., Iglesias Buela L. (2001). Comparative study of the assay of Artemia salina L. and the estimate of the medium lethal dose (LD50 value) in mice, to determine oral acute toxicity of plant extracts. Phytomedicine 8: 395–400. [DOI] [PubMed] [Google Scholar]
- Lee Y.-S. (1988). Background mucosal changes in colorectal carcinomas. Cancer 61: 1563–1570. [PubMed] [Google Scholar]
- Leegwater D. C., de Groot A. P., van Kalmthout-Kuyper M. (1974). The aetiology of caecal enlargement in the rat. Food Cosmet. Toxicol. 12: 687–697. [DOI] [PubMed] [Google Scholar]
- Lim B. O., Seong N. S., Choue R. W., Kim J. D., Lee H. Y., Kim S. Y., Yu B. P., Jeon T. I., Park D. K. (2003). Efficacy of dietary aloe vera supplementation on hepatic cholesterol and oxidative status in aged rats. J. Nutr. Sci. Vitaminol. 49: 292–296. [DOI] [PubMed] [Google Scholar]
- Lupton J. R. (2004). Microbial degradation products influence colon cancer risk: The butyrate controversy. J. Nutr. 134: 479–482. [DOI] [PubMed] [Google Scholar]
- Lydén-Sokolowski A., Nilsson A., Sjöberg P. (1993). Two-year carcinogenicity study with sennosides in the rat: Emphasis on gastro-intestinal alterations. Pharmacology 47:(Suppl. 1)209–215. [DOI] [PubMed] [Google Scholar]
- Mandal G., Das A. (1980). Structure of the glucomannan isolated from the leaves of Aloe barbadensis Miller. Carbohydr. Res. 87: 249–256. [Google Scholar]
- Mapp R. K., McCarthy T. J. (1970). The assessment of purgative principles in aloes. Planta Med. 18: 361–365. [DOI] [PubMed] [Google Scholar]
- Marshall J. M. (1990). Aloe vera gel: What is the evidence? Pharm. J. 24: 360–362. [Google Scholar]
- Matsuda Y., Yokohira M., Suzuki S., Hosokawa K., Yamakawa K., Zeng Y., Ninomiya F., Saoo K., Kuno T., Imaida K. (2008). One-year chronic toxicity study of Aloe arborescens Miller var. natalensis Berger in Wistar Hannover rats. A pilot study. Food Chem. Toxicol. 46: 733–739. [DOI] [PubMed] [Google Scholar]
- Mori H., Sugie S., Niwa K., Takahashi M., Kawai K. (1985). Induction of intestinal tumours in rats by chrysazin. Br. J. Cancer 52: 781–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mori H., Yoshimi N., Iwata H., Mori Y., Hara A., Tanaka T., Kawai K. (1990). Carcinogenicity of naturally occurring 1-hydroxyanthraquinone in rats: Induction of large bowel, liver and stomach neoplasms. Carcinogenesis 11: 799–802. [DOI] [PubMed] [Google Scholar]
- Nascimbeni R., Donato F., Ghirardi M., Mariani P., Villanacci V., Salerni B. (2002). Constipation, anthranoid laxatives, melanosis coli, and colon cancer: A risk assessment using aberrant crypt foci. Cancer Epidemiol. Biomarkers Prev. 11: 753–757. [PubMed] [Google Scholar]
- Nishikawa A., Kase Y., Hayakawa T., Yanagisawa T., Kanno J., Hayashi Y. (1997). Enhancement of cell proliferation and prostaglandin biosynthesis by 1,8-dihydroxyanthraquinone in the rat large intestine. Carcinogenesis 18: 1259–1263. [DOI] [PubMed] [Google Scholar]
- Olubuyide I. O., Williamson R. C. N., Bristol J. B., Read A. E. (1984). Goblet cell hyperplasia is a feature of the adaptive response to jejunoileal bypass in rats. Gut 25: 62–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piegorsch W. W., Bailer A. J. (1997). Chapter 6. Trend testing. In Statistics for Environmental Biology and Toxicology, pp. 213–271 Chapman and Hall, London, UK. [Google Scholar]
- Pogribna M., Freeman J. P., Paine D., Boudreau M. D. (2008). Effect of Aloe vera whole leaf extract on short chain fatty acids production by Bacteroides fragilis, Bifidobacterium infantis and Eubacterium limosum . Lett. Appl. Microbiol. 46: 575–580. [DOI] [PubMed] [Google Scholar]
- Portier C. J., Bailer A. J. (1989). Testing for increased carcinogenicity using a survival-adjusted quantal response test. Fundam. Appl. Toxicol. 12: 731–737. [DOI] [PubMed] [Google Scholar]
- Prior P., Gyde S. N., Macartney J. C., Thompson H., Waterhouse J. A. H., Allan R. N. (1982). Cancer morbidity in ulcerative colitis. Gut 23: 490–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds T. (1985). The compounds in Aloë leaf exudates: A review. Bot. J. Linn. Soc. 90: 157–177. [Google Scholar]
- Ribeiro Rodrigues O., Antonangelo L., Yagi N., Minamoto H., Fernandes Schmidt A. F., Jr, Capelozzi V. L., Goldenberg S., Nascimento Saldiva P. H. (1997). Prognostic significance of argyrophilic nucleolar organizer region (AgNOR) in resected non-small cell lung cancer (NSCLC). Jpn. J. Clin. Oncol. 27: 298–304. [DOI] [PubMed] [Google Scholar]
- Saito H., Imanishi K-i., Okabe S. (1989). [Effects of aloe extracts, aloctin A, on gastric secretion and on experimental gastric lesions in rats]. Yakugaku Zasshi 109: 335–339. [DOI] [PubMed] [Google Scholar]
- Shah A. H., Qureshi S., Tariq M., Ageel A. M. (1989). Toxicity studies on six plants used in the traditional Arab system of medicine. Phytother. Res. 3: 25–29. [Google Scholar]
- Shimpo K., Chihara T., Beppu H., Ida C., Kaneko T., Nagatsu T., Kuzuya H. (2001). Inhibition of azoxymethane-induced aberrant crypt foci formation in rat colorectum by whole leaf Aloe arborescens Miller var. natalensis Berger. Phytother. Res. 15: 705–711. [DOI] [PubMed] [Google Scholar]
- Siegers C.-P., Siemers J., Baretton G. (1993a). Sennosides and aloin do not promote dimethylhydrazine-induced colorectal tumors in mice. Pharmacology 47:(Suppl. 1)205–208. [DOI] [PubMed] [Google Scholar]
- Siegers C.-P., von Hertzberg-Lottin E., Otte M., Schneider B. (1993b). Anthranoid laxative abuse–a risk for colorectal cancer? Gut 34: 1099–1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sigel J. E., Petras R. E., Lashner B. A., Fazio V. W., Goldblum J. R. (1999). Intestinal adenocarcinoma in Crohn’s disease: A report of 30 cases with a focus on coexisting dysplasia. Am. J. Surg. Pathol. 23: 651–655. [DOI] [PubMed] [Google Scholar]
- Smits-Van Prooije A. E., De Groot A. P., Dreef-Van Der Meulen H. C., Sinkeldam E. J. (1990). Chronic toxicity and carcinogenicity study of isomalt in rats and mice. Food Chem. Toxicol. 28: 243–251. [DOI] [PubMed] [Google Scholar]
- Stevens C. E., Hume I. D. (1998). Contributions of microbes in vertebrate gastrointestinal tract to production and conservation of nutrients. Physiol. Rev. 78: 393–427. [DOI] [PubMed] [Google Scholar]
- Tanaka M., Misawa E., Ito Y., Habara N., Nomaguchi K., Yamada M., Toida T., Hayasawa H., Takase M., Inagaki M., et al. (2006). Identification of five phytosterols from Aloe vera gel as anti-diabetic compounds. Biol. Pharm. Bull. 29: 1418–1422. [DOI] [PubMed] [Google Scholar]
- Tanaka T. (2009). Colorectal carcinogenesis: Review of human and experimental animal studies. J. Carcinog. 8: 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teradaira R., Shinzato M., Beppu H., Fujita K. (1993). Antigastric ulcer effects in rats of Aloe arborescens Miller var. natalensis Berger extract. Phytother. Res. 7: S34–S36. [Google Scholar]
- Til H. P., Feron V. J., Immel H. R., Vogel W. F. (1986). Chronic (89-week) feeding study with hydroxypropyl distarch phosphate, starch acetate, lactose and sodium alginate in mice. Food Chem. Toxicol. 24: 825–834. [DOI] [PubMed] [Google Scholar]
- Vaiphei K., Saha M., Sharma B. C., Bhasin D. K., Singh K. (2004). Goblet cell status in idiopathic ulcerative colitis–implication in surveillance program. Indian J. Pathol. Microbiol. 47: 16–21. [PubMed] [Google Scholar]
- van Gorkom B. A., de Vries E. G. E., Karrenbeld A., Kleibeuker J. H. (1999). Review article: Anthranoid laxatives and their potential carcinogenic effects. Aliment. Pharmacol. Ther. 13: 443–452. [DOI] [PubMed] [Google Scholar]
- Vyth A., Kamp P. E. (1979). Detection of anthraquinone laxatives in the urine. Pharm. Weekbl. 114: 456–459. [Google Scholar]
- Waller T. A., Pelley R. P., Strickland F. M. (2004). Industrial processing and quality control of Aloe barbadensis (Aloe vera) gel. In Aloes: The Genus Aloe (Reynolds T, Ed.), pp. 139–205. CRC Press, Boca Raton, FL. [Google Scholar]
- WHO-IARC (2002). Section C. Rubia tinctorum, Morinda officinalis and anthraquinones. In IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Vol. 82. Some Traditional Herbal Medicines, Some Mycotoxins, Naphthalene and Styrene, pp. 129–151 World Health Organization, International Agency for Research on Cancer, Lyon, France. [PMC free article] [PubMed] [Google Scholar]
- Willems M., van Buuren H. R., de Krijger R. (2003). Anthranoid self-medication causing rapid development of melanosis coli. Neth. J. Med. 61: 22–24. [PubMed] [Google Scholar]
- Williamson R. C. N., Davies P. W., Bristol J. B., Wells M. (1982). Intestinal adaptation and experimental carcinogenesis after partial colectomy. Increased tumour yields are confined to the anastomosis. Gut 23: 316–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaron A. (1993). Characterization of Aloe vera gel before and after autodegradation, and stabilization of the natural fresh gel. Phytother. Res. 7: S11–S13. [Google Scholar]
- Yokohira M., Matsuda Y., Suzuki S., Hosokawa K., Yamakawa K., Hashimoto N., Saoo K., Nabae K., Doi Y., Kuno T., et al. (2009). Equivocal colonic carcinogenicity of Aloe arborescens Miller var. natalensis Berger at high-dose level in a Wistar Hannover rat 2-y study. J. Food Sci. 74: T24–T30. [DOI] [PubMed] [Google Scholar]
- Zhao J., Wang J., Chen Y., Agarwal R. (1999). Anti-tumor-promoting activity of a polyphenolic fraction isolated from grape seeds in the mouse skin two-stage initiation-promotion protocol and identification of procyanidin B5-3’-gallate as the most effective antioxidant constituent. Carcinogenesis 20: 1737–1745. [DOI] [PubMed] [Google Scholar]