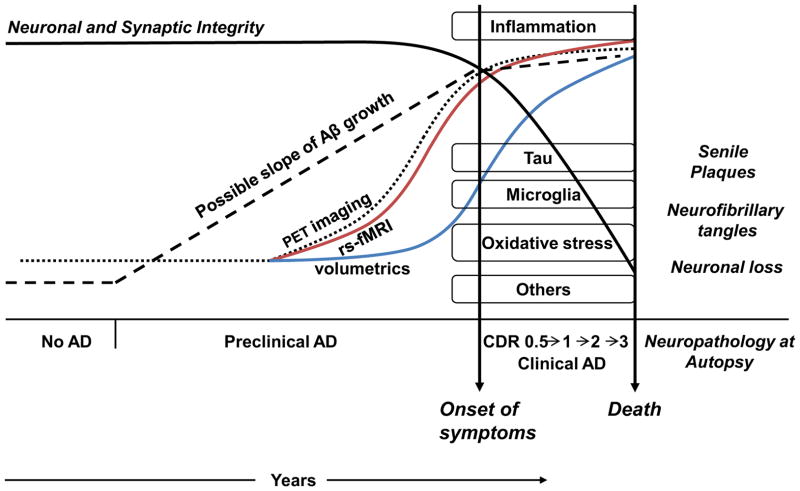
Figure 2. Timecourse from Preclinical to Clinical AD: Pathophysiology and Imaging.
Preclinical AD has been hypothesized to begin many years or decades before clinical symptoms. Progressive amyloid accumulation occurs early, with models for the kinetics of amyloid accumulation shown with different dotted lines. As yet the kinetics remain to be determined. Tau deposition, augmented by oxidative damage and inflammation, results in neuronal death. In the figure the timing and onset of tau deposition, inflammation, activated microglia, oxidative stress and other mechanisms is not meant to be precise but is simply meant to show onset during the preclinical phase. Following onset of cognitive decline clinical progression occurs resulting inevitably in death. The definitive diagnosis of AD can only be made post-mortem with autopsy showing neuropathological features of senile plaques and neurofibrillary tangles.
Amyloid accumulation is imaged with positron emission tomography (PET) scanning (dotted curve). Kinetic models for amyloid deposition remain to be determined. Following PET detection of amyloid and before structural damage, abnormalities in resting state functional connectivity can be detected on fMRI (red curve) (see text for exceptions). Progressive neurotoxicity manifests cumulatively as structural damage in imaging studies (blue curve). Following structural damage, cognitive decline produces progressive clinical deterioration.