Abstract
Objective
Burn injury deformities and obesity have been associated with social integration difficulty and body image dissatisfaction. However, the combined effects of obesity and burn injury in social integration difficulty and body image dissatisfaction are unknown.
Methods
Adolescent and young adults burn injury survivors were categorized as normal weight (n=47) or overweight and obese (n=21). Burn-related and anthropometric information was obtained from patients' medical records, while validated questionnaires were used to assess the main outcomes and possible confounders. Analysis of covariance and multiple linear regressions were performed to evaluate the objectives of this study.
Results
Obese and overweight burn injury survivors did not experience increased body image dissatisfaction (12 ± 4.3 vs 13.1 ± 4.4, p = 0.57) or social integration difficulty (17.5 ± 6.9 vs 15.5 ± 5.7, p=0.16) compared to normal weight burn injury survivors. Weight status was not a significant predictor of social integration difficulty or body image dissatisfaction (p=0.19 and p=0.24, respectively). However, mobility limitations predicted greater social integration difficulty (p=0.005) and body image dissatisfaction (p<0.001), while higher weight status at burn was a borderline significant predictor of body image dissatisfaction (p=0.05).
Conclusions
Obese and overweight adolescents and young adults, who sustained a major burn injury as children, do not experience greater social integration difficulty and body image dissatisfaction compared to normal weight burn injury survivors. Mobility limitations and higher weight status at burn are likely more important factors affecting the long-term social integration difficulty and body image dissatisfaction of these young people.
Keywords: Obesity, burn, social integration, body image dissatisfaction
Introduction
Advances in medical care have dramatically increased the survival rate of severely burned persons.1 Nonetheless, burn injury survivors suffer from permanent body deformities such as scar tissue formation, mobility limitations, impaired skin integrity and amputations.2,3 Moreover, in response to the thermal injury, they experience dramatic weight loss, which abates over time. 4Long-term data on the weight status of pediatric burn injury survivors as compared to healthy individuals are not available. Body image is a major determinant of the perception of self (“self-perception”),5 as individuals tend to define themselves in response to the information they receive from interaction with the environment and self-observation.6
Burn injury survivors, especially those with facial burn injuries 7, report worse quality of life compared to healthy individuals 8. Moreover, they tend to suffer from higher body image dissatisfaction, decreased social integration and higher perceived stigmatization from their social environment 9-13. Specific behaviors encountered from their social environment include avoidance, staring, and unfriendly conduct 9-13. Age 8,14, time post-burn 8,15, sex 8,16,17, and injury severity 7,18 have been associated with body image satisfaction and social integration among burn injury survivors.
Similarly, obese individuals experience social marginalization, inequity, weight discrimination and prejudice in a variety of public settings due to the prevalent negative assumptions about their attributions and the causes of obesity.19,20 Laziness, immorality, lack of personal hygiene and self-control,21 and low intellect 22 are characteristics frequently misattributed to obese individuals. The experienced weight discrimination has been associated with negative psychosocial outcomes such as low body satisfaction, emotional eating, and other adverse mental health outcomes.23
The purpose of this study was to investigate whether overweight/obese adolescent and young adult burn injury survivors experience higher body image dissatisfaction and worse social integration compared to normal weight burn injury survivors. To the best of our knowledge, this is the first study to investigate the relationship of weight status on body image and social integration in burn injury survivors.
Methods
Sample
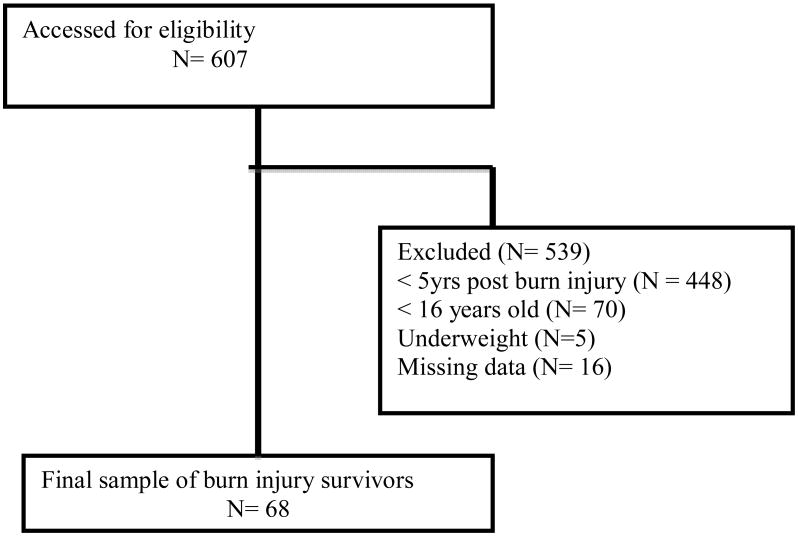
The current study was part of two larger cohort studies designed to investigate the long-term psychosocial impact of burn injury. Study sample consisted of 68 adolescent and young adult (16 to 30 years) survivors of pediatric burns who received acute treatment at a pediatric hospital specializing in burns (Figure 1). This institution serves children and adolescents of low socioeconomic status (SES) in financial need at no cost, both from the US and abroad (mostly Mexico). Data were collected in conjunction with the following studies: Burn Model System Five and Ten Year Long-Term Follow-Up of a National Sample of Major Burn Injuries (LTF-NDS) (IRB# 11-356) and Burn Center Data Bank Study (IRB# 11-435). Approval was obtained from the University of Texas Medical Branch Institutional Review Board. Written consent was obtained from all participants 18 years and older. For participants younger than 18, both their written assent and written consent from their parents or guardians were obtained. Inclusion criteria included patients admitted with ≥ 20% total burn surface area (TBSA) burns, electrical high voltage burns, and individuals younger than 18 years at the time of injury, who were at least 16 years old at follow-up, and for whom follow-up occurred at least five years after their burn. Exclusion criteria included being admitted to the hospital for non-burn injury related reasons, being underweight, not speaking either English or Spanish, and having missing data. Underweight individuals at the time of the interview were excluded from the study sample, as being underweight/ cachectic is also a type of disfigurement that it is stigmatized and associated with poor health.24 All questionnaires were self-administered. Validated Spanish versions of the questionnaires were provided for Spanish-speaking participants.
Figure 1. Study diagram.
Measures
Perceived Burn Specific Health
The brief version of the Burn Specific Heath Scale (BSHS-B) was used to evaluate the physical and emotional well being of participants.25 This 40-item questionnaire assesses nine domains: simple abilities, heat sensitivity, hand function, treatment regimens, work, body image, affect, interpersonal relationships and sexuality.25 In prior studies, the Cronbach's alpha coefficient of reliability for the subscales ranged from 0.75 to 0.93. 25,26 In our sample, the Cronbach alpha of the body image domain was 0.92. Examples of specific items include “I would rather be alone than with my family,” “I am not interested doing things with my friends, ” or “I have no one to talk about my problems with.” Response options ranged from 0 (“all the time/great difficulty”) to 4 (“never/no difficulty”). Items were summed to obtain subscale scores and a total score.
Well- Being
The Short Form (SF)-12® Health Survey, version 2 was used to evaluate the overall well being (functional health and mental health) of participants.27 This abbreviated form of the Short Form (SF)-36® Health Survey includes 12 questions on physical functioning, limitations because of physical problems, pain, general health perception, energy/fatigue, social functioning, and limitations because of social and mental health problems. The SF-12 is a reliable measure of physical and mental health status, yielding results comparable to the original questionnaire.27 In our sample, the Cronbach's alpha for SF-12 was 0.85. Specific questions include “How does your health now limit you in climbing several flights or stairs,” “How much of the time were you limited in the kind of work or other activities you could do,” “During the past 4 weeks how much did pain interfere with your normal work (outside home and house work),” and “How much of the time during the past 4 weeks have you felt downhearted and depressed.” The total score ranges from 12 to 56, with higher scores indicating greater well-being.
Social Intergration
The World Health Organization Disability Assessment Schedule II (WHODAS II) was used to assess participants' social integration and mobility limitations. Social integration was defined as the existence of the same rights and opportunities for all members of the social group. 28 WHODAS II is a standardized questionnaire used to assess health and disability.29 It has proven to be valid, sensitive, and reliable across cultures. Previous factor analysis of the WHODAS II form 2 subscales indicated that Domains 4 and 6 of Section 3 can be used to assess difficulty getting along with people and with participating in social activities. The scores from Domain 4 and 6 were summed to assess the social integration difficulty of participants, while Domain 2 was used to evaluate mobility limitations (difficulty getting around). Response options range from 1 (“none”) to 5 (“extreme”). Answers are then summed to obtain a total social integration subscale score. In prior research, the Cronbach's alpha for those with physical disabilities was 0.97, while for domains for Domains 4 and 6 it is 0.92 and 0.94, respectively. In our sample, the Cronbach's alpha values for Domains 3, 4 and 6 were 0.81, 0.82 and 0.84 respectively.
Weight Status
For this study, we assessed participants' weight status at burn and the time of the interview using anthropometric information obtained from participants' electronic medical record. Weight status at burn was used as a surrogate marker of pre-burn weight status. Trained clinical staff members conducted all measurements at admission and at follow-up. Weight was measure with an ST Scale-Tronix Model 5102 409 (Scale-Tronix White Plains, NY), while height was measured with a stadiometer, PE-WM-BASE (Perspective Enterprises, Portage, MI). Participants with limb amputations were weighed without their prostheses and their weights adjusted retrospectively for the missing limb.30 Participants' body mass index (BMI) was calculated using the following formula: BMI= weight (kg)/ height2 (m2). World Health Organization (WHO) criteria were used to classify subjects older than 20 years as underweight (BMI < 18.4), normal weight (BMI 18.5-24.9), overweight (BMI 25 - 29.9), or obese (BMI > 30). Furthermore, the BMI of participants younger than 20 was classified using the age and gender-specific BMI international cut-off values as established by Cole et al31,32. Participant percentile BMI was calculated according to the age- and sex-specific BMI growth charts developed by the Centers for Disease Control and Prevention33.
Other Variables
Clinical information and other burn-related data obtained from the medical record included etiology of burn injury, TBSA, specific part of body affected, amputations, age at burn injury, years post burn, and physical disability. TBSA was assessed using the “rule of nines” method during excisional surgery.34 Socio-demographic data obtained included age, sex, and ethnicity.
Statistical Analysis
All continuous variables are presented as mean ± standard deviation (SD), and all categorical variables are presented as absolute and relative frequencies. Descriptive statistics, chi-square tests of association, and analysis of covariance (ANCOVA) were performed to evaluate differences in social integration, body image, and well being across the four weight status categories. We also performed multiple linear regressions to evaluate possible predictors of body image dissatisfaction and social integration. Data analysis was performed using the PASW Statistics 18, Release Version 18.0.0 (SPSS Inc., 2010, Chicago, IL).
Results
The mean age of participants was 18.6 ± 4.2 years. The mean BMI for normal weight participants was 21.7 ±1.7 and for overweight/obese participants was 29.5 ± 5.7 (p<0.001). As shown in Table 1, the majority of subjects were male (67.6%) and Hispanic (89.7%). Overall, 69.2% of the sample was normal weight and 30.8% was overweight or obese. Overweight individuals were slightly older than normal weight individuals (19.5 ± 0.5 vs 18.2 ± 3 years, p=0.04).
Table 1.
Subject characteristics of adolescent and young adult burn injury survivors.
| Parameters | Total (n = 68) | Normal weight (n = 47) | Overweight/obese (n = 21) | p-value |
|---|---|---|---|---|
| Age (yrs) | 18.6 ± 4.2 | 18.2 ± 3 | 19.5 ± 0.5 | 0.04 |
| Sex | ||||
| Male | 46 (67.6%) | 30 (63.8 %) | 16 (72.6 %) | |
| Female | 22 (32.4%) | 17 (36.2%) | 5 (23.8%) | 0.31 |
| Ethnicity | ||||
| Hispanic | 61 (89.7%) | 44 (93.6%) | 17 (81.0 %) | |
| Non-Hispanic | 7 (10.3%) | 3 (6.4%) | 4 (19 %) | 0.35 |
| BMI | 24 ± 4.9 | 21.7 ±1.7 | 29.5 ±5.7 | <0.001 |
| BMI percentile | 61.4 ± 26.2 | 49.2 ±21.4 | 90.1 ± 6.9 | <0.001 |
BMI: Body Mass Index
Table 2 reflects the burn related characteristics of the study sample. Fire or flame was the primary cause of burn injury. For about 81% of participants, the burn injury affected the head and neck area. The mean TBSA was 56.1 ± 5.6%, while 15.4% of participants had an amputation. The mean age at burn was 10.7 ± 4.4 years, while the mean time post burn was 7.9 ± 3.9 years. Normal weight children were slightly younger than overweight/obese at time of the burn injury (9.9 ± 4 vs 12.3 ± 4.3 years, p=0.04).
Table 2. Burn related characteristics of adolescent and young adult burn injury survivors.
| Parameters | Total (n= 68) | Normal weight (n= 47) | Overweight/obese (n=21) | p-value |
|---|---|---|---|---|
| Etiology | ||||
| Flame/ Fire | 52 (76.5%) | 34 (72.3%) | 18 (85.7%) | |
| Scald/Grease | 5 (7.3 %) | 4 (8.6 %) | 1 (4.8%) | |
| Electricity | 10 (14.7%) | 8 (17%) | 2 (9.5 %) | 0.69 |
| TBSA (%) | 56.1 ± 5.7 | 58.4 ± 8.1 | 50.9 ± 8.8 | 0.54 |
| Age at burn (yrs) | 10.7 ± 4.4 | 9.9 ± 4 | 12.3 ± 4.3 | 0.04 |
| Years post-burn | 7.9 ± 3.9 | 8.4 ± 0.6 | 6.8 ± 0.6 | 0.125 |
| Amputation | 10 (15.4 %) | 8 (17.8%) | 2 (10%) | 0.42 |
| Burn Site | ||||
| Head/Neck | 55 (80.9 %) | 38 (80.9%) | 17 (81 %) | 0.78 |
| Trunk | 62 (91.2 %) | 43 (91.5%) | 19 (90.5%) | 0.37 |
| Perineum | 21 (30.9%) | 13 (27.7%) | 8 (38.1%) | 0.76 |
| Arm | 64 (94.1%) | 43 (91.5%) | 21 (100 %) | 0.47 |
| Hand | 54 (79.43%) | 36 (76.6%) | 18 (85.7%) | 0.33 |
| Leg | 58 (85.3%) | 42 (89.3 %) | 16 (76.2 %) | 0.24 |
| Foot | 31 (45.5%) | 19 (40.4%) | 12 (57.1%) | 0.57 |
TBSA: Total burn surface area
Participants reported mild body image dissatisfaction (according to BSHS-B) and mild difficulty in participating in society and getting along with others (WHODAS II; Table 3). Overweight/obese participants did not report statistically significant body image dissatisfaction, difficulty getting along with people, difficulty participating in society and social integration difficulty, after adjustment for sex, age at burn, weight status at burn, well-being, amputation, head and neck injury and mobility limitations. Unadjusted means also showed no statistically significant differences between the two groups.
Table 3. Adjusted means scores of social integration and body image from adolescent and young adult burn injury survivors.
| Total (n = 68) | Normal Weight (n = 47) | Overweight or obese (n = 21) | P-value | ||
|---|---|---|---|---|---|
| Body Image Dissatisfaction a | Crude | 12.1 ± 4.4 | 11.8 ± 4.4 | 12.7 ± 4.4 | 0.55 |
| Adjusted | 12.4 ± 4.2 | 12 ± 4.3 | 13.1 ± 4.4 | 0.57 | |
| Difficulty Getting along with People b | Crude | 8 ± 3.3 | 8.4 ± 3.5 | 7 ± 2.5 | 0.21 |
| Adjusted | 7.6 ± 3.2 | 7.8 ± 3.5 | 7.0 ± 2.2 | 0.21 | |
| Difficulty Participating in Society c | Crude | 8.7 ± 4.0 | 8.8 ± 4.2 | 8.4 ± 3.7 | 0.7 |
| Adjusted | 8.6 ± 3.7 | 9 ± 4.1 | 7.9 ± 2.9 | 0.58 | |
| Difficulty in Social Integration d | Crude | 16.9 ± 6.6 | 17.5 ± 6.9 | 15.5 ± 5.7 | 0.32 |
| Adjusted | 16.4 ± 6.4 | 17.2 ± 6.9 | 14.9 ± 5.1 | 0.16 |
Adjusted for sex, age at burn, weight status at burn, well-being, amputation, head and neck burn injury, and mobility limitation.
Total score of the Burn Specific Heath Scale-Brief, Body Image Section. Possible score range: 0 -16.
Total score of the WHO-DAS II, Section 3, Domain 4. Possible score range: 5 - 25
Total score of the WHO-DAS II, Section 3, Domain 6. Possible score range: 5 - 25
Total score of the WHO-DAS II, Section 3, Domains 4 and 6. Possible score range: 10 - 50
To examine the predictors of social integration, we conducted a multiple regression controlling for weight status, weight status at burn, head neck injury, well-being, and mobility limitation. As shown in Table 4, social integration difficulty was not associated with currently being overweight/obese after controlling for weight status at burn, head neck injury, well-being, and mobility limitations. However, mobility limitations were associated with greater difficulty in participating in society (p<0.001).
Table 4. Multiple linear regression model: Predictors of social integration difficulty a among adolescent and young adult burn injury survivors.
| Beta coefficients | p-value | |
|---|---|---|
| Overweight/Obese | - 0.15 | 0.24 |
| Well-being b | 0.05 | 0.73 |
| Head Neck Burn Injury | 0.05 | 0.69 |
| Mobility limitation c | 0.57 | <0.001 |
| Weight status at burnd | 0.16 | 0.22 |
Total score of the WHO-DAS II, Section 3, Domains 4 and 6.
Total score of the Short Form (SF)-12® Health Survey version 2
Total score of the WHO-DAS II, Section 3, Domain 2
A second multiple logistic regression was performed to assess for possible predictors of body image dissatisfaction. After controlling for the same factors listed above, body image dissatisfaction was also not associated with being overweight or obese (Table 5). However, mobility limitations were associated with body image dissatisfaction (p=0.005), while weight status at burn was an additional predictor of body image dissatisfaction.
Table 5. Multiple linear regression model: Predictors of body image dissatisfaction a among adolescent and young adult burn injury survivors.
| Beta coefficients | p-value | |
|---|---|---|
| Sex | 0.025 | 0.84 |
| Age at burn | -0.062 | 0.63 |
| Overweight/Obese | 0.18 | 0.19 |
| TBSA | 0.032 | 0.80 |
| Mobility limitation b | -0.37 | 0.005 |
| Weight status at burnc | -0.268 | 0.05 |
Total score of the Burn Specific Heath Scale-Brief, Body Image Section.
Total score of the WHO-DAS II, Section 3, Domain 2
Discussion
Contrary to our initial hypothesis, we found no association between overweight/obesity and social integration and body image in long term burn injury survivors. However, mobility limitations were associated with higher body image dissatisfaction and social integration difficulty, while weight status at burn was associated with greater difficulty with higher body image dissatisfaction,.
The current findings are surprising given previous research among non-disfigured individuals, which found obesity associated with greater body image dissatisfaction,35 social marginalization, inequity, and prejudice.19,20 Instead, we found that obesity/overweight is not associated with body image dissatisfaction and difficulty with social integration in long-term burn injury survivors. Interestingly, higher weight status at burn was associated with greater body image dissatisfaction. This may be due to the fact that individuals facing life threatening conditions may become more resilient and develop positive coping mechanisms such as better communication skills, greater self-determination and a focus on getting the maximal pleasure from daily living. 36 Alternatively, the limitations and disfigurement of experiencing a traumatic physical injury may outweigh any concerns of the individual about weight. Regardless of the reason, it appears that weight status at the time of burn may no longer be a major determinant of body image for such persons. Participants with high weight status at burn may have pre-existing body image dissatisfaction, which persisted after burn injury.
Mobility limitations were associated with greater body image dissatisfaction and social integration difficulty. Previous research conducted in burn survivors two months post burn37 and patients with amputations 38 also support the notion that physical function difficulties are associated with body image dissatisfaction. Likewise, improved physical functioning has been previously associated with early social reintegration in adolescent burn injury survivors. 39 Individuals with mobility limitations cannot easily participate in social events and return to their pre-burn activities.
Several factors may limit the generalizability of our results. First, the small study sample consisted mostly of males and Hispanics. In addition, pre-burn psychopathology and family environment were not assessed, as data on these factors were not available. Weight status at burn, used as a marker of pre-burn weight status, may have been skewed by acute fluid shifts related to the burn injury. Although we did not have data on the SES of participants, the vast majority were of low SES. This fact may have also biased our results, as those with low SES may be less prejudiced against obese and overweight individuals.40 Moreover, the SF-12 used has not been validated for pediatric burn injury survivors. Finally, the body image domain of the BSHS-B, used to assess body image satisfaction, may not have been sensitive enough to discern differences in body image dissatisfaction related to weight status.
However, this study has numerous strengths. To the best of our knowledge, this is the first study to investigate the effect of weight status on body image and social integration in burn injury survivors, or indeed, children with any form of physical disfigurement. In addition, the availability of data on long-term burn injury survivors strengthens the significance of our findings. Finally, all information was collected using validated questionnaires and medical record information, which is a relatively reliable approach.
In conclusion, contrary to our initial hypothesis, we found that overweight and obesity are not associated with negative long-term body image and social integration among pediatric burn injury survivors. On the other hand, mobility difficulty was a significant determinant of body image satisfaction and community integration, while weight status at burn was a predictor of body image dissatisfaction. Once their medical status is stable, rehabilitation should be a priority for all pediatric burn injury survivors. In addition, body image concerns should be addressed in individuals with high weight status at burn. As a result, an interdisciplinary approach is needed to ensure the optimal long-term psychosocial adjustment of pediatric burn injury survivors. Further research is needed to investigate longitudinally the proposed hypothesis in a larger sample, as burn injury survivors may undergo changes during the adjustment period.
Acknowledgments
We also thank Deborah Benjamin, Wes Benjamin, Maria Cantu, Mario Celis, Kathryn Epperson, Eric Henry, Holly Goode, Kara Hougen, Joanna Huddleston, Mary Kelly, Xuyang Liang, Marc Nicolai, Sylvia Ojeda, Cathy Reed, Lisa Richardson, Lucile Robles, Pam Stevens, Sierra Tinney, and Judith Underbrink for their assistance in obtaining the study measurements.
Sources of Support: This study was supported by grants from the National Institute for Disabilities and Rehabilitation Research (H133A070026 and H133A70019), the National Institutes of Health (P50-GM60338, R01-HD049471, and T32-GM8256), and Shriners Hospitals for Children (84080, 8741, 9145, 8760, and 71008).
Footnotes
Conflicts of Interest: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Wolf SE, Rose JK, Desai MH, Mileski JP, Barrow RE, Herndon DN. Mortality determinants in massive pediatric burns. An analysis of 103 children with > or = 80% TBSA burns (> or = 70% full-thickness) Ann Surg. 1997;225(5):554–565. doi: 10.1097/00000658-199705000-00012. discussion 565-559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Costa BA, Engrav LH, Holavanahalli R, et al. Impairment after burns: a two-center, prospective report. Burns. 2003;29(7):671–675. doi: 10.1016/s0305-4179(03)00153-0. [DOI] [PubMed] [Google Scholar]
- 3.Thomas CR, Brazeal BA, Rosenberg L, Robert RS, Blakeney PE, Meyer WJ. Phantom limb pain in pediatric burn survivors. Burns. 2003;29(2):139–142. doi: 10.1016/s0305-4179(02)00281-4. [DOI] [PubMed] [Google Scholar]
- 4.Przkora R, Herndon DN, Jeschke MG. The factor age and the recovery of severely burned children. Burns. 2008 Feb;34(1):41–44. doi: 10.1016/j.burns.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 5.Knudson-Cooper MS. Adjustment to visible stigma: the case of the severely burned. Soc Sci Med Med Anthropol. 1981;15B(1):31–44. doi: 10.1016/0160-7987(81)90007-7. [DOI] [PubMed] [Google Scholar]
- 6.Hazel M. Self-schemata and processing information about the self. Journal of personality and social psychology. 1977;35(2) [Google Scholar]
- 7.Stubbs TK, James LE, Daugherty MB, et al. Psychosocial impact of childhood face burns: a multicenter, prospective, longitudinal study of 390 children and adolescents. Burns. 2011 May;37(3):387–394. doi: 10.1016/j.burns.2010.12.013. [DOI] [PubMed] [Google Scholar]
- 8.Rosenberg M, Blakeney P, Robert R, Thomas C, Holzer C, 3rd, Meyer W., 3rd Quality of life of young adults who survived pediatric burns. J Burn Care Res. 2006 Nov-Dec;27(6):773–778. doi: 10.1097/01.BCR.0000245477.10083.BC. [DOI] [PubMed] [Google Scholar]
- 9.Macgregor FC. Facial disfigurement: problems and management of social interaction and implications for mental health. Aesthetic Plast Surg. 1990;14(4):249–257. doi: 10.1007/BF01578358. [DOI] [PubMed] [Google Scholar]
- 10.Fauerbach JA, Lawrence JW, Schmidt CW, Jr, Munster AM, Costa PT., Jr Personality predictors of injury-related posttraumatic stress disorder. J Nerv Ment Dis. 2000;188(8):510–517. doi: 10.1097/00005053-200008000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Lawrence JW, Fauerbach JA, Heinberg LJ, Doctor M, Thombs BD. The reliability and validity of the Perceived Stigmatization Questionnaire (PSQ) and the Social Comfort Questionnaire (SCQ) among an adult burn survivor sample. Psychol Assess. 2006;18(1):106–111. doi: 10.1037/1040-3590.18.1.106. [DOI] [PubMed] [Google Scholar]
- 12.Lawrence JW, Fauerbach JA, Thombs BD. A test of the moderating role of importance of appearance in the relationship between perceived scar severity and body-esteem among adult burn survivors. Body Image. 2006;3(2):101–111. doi: 10.1016/j.bodyim.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 13.Thombs BD, Notes LD, Lawrence JW, Magyar-Russell G, Bresnick MG, Fauerbach JA. From survival to socialization: a longitudinal study of body image in survivors of severe burn injury. J Psychosom Res. 2008;64(2):205–212. doi: 10.1016/j.jpsychores.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 14.Lawrence JW, Rosenberg L, Mason S, Fauerbach JA. Comparing parent and child perceptions of stigmatizing behavior experienced by children with burn scars. Body Image. 2011 Jan;8(1):70–73. doi: 10.1016/j.bodyim.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 15.Byrne C, Love B, Browne G, Brown B, Roberts J, Streiner D. The social competence of children following burn injury: a study of resilience. J Burn Care Rehabil. 1986;7(3):247–252. doi: 10.1097/00004630-198605000-00011. [DOI] [PubMed] [Google Scholar]
- 16.Salvador-Sanza JF, Sanchez-Paya J, Rodriguez-Marin J. Quality of life of the Spanish burn patient. Burns. 1999 Nov;25(7):593–598. doi: 10.1016/s0305-4179(99)00054-6. [DOI] [PubMed] [Google Scholar]
- 17.Russell W, Holzer CE, 3rd, Robert RS, Thomas C, Blakeney P, Meyer WJ., 3rd Differences in behavioral perceptions between young adult burn survivors and cross-informants. J Burn Care Res. 2008 Sep-Oct;29(5):750–755. doi: 10.1097/BCR.0b013e3181848192. [DOI] [PubMed] [Google Scholar]
- 18.Wiechman SA, Ptacek JT, Patterson DR, Gibran NS, Engrav LE, Heimbach DM. Rates, trends, and severity of depression after burn injuries. J Burn Care Rehabil. 2001 Nov-Dec;22(6):417–424. doi: 10.1097/00004630-200111000-00012. [DOI] [PubMed] [Google Scholar]
- 19.Dejong W. The stigma of obesity: the consequences of naive assumptions concerning the causes of physical deviance. J Health Soc Behav. 1980 Mar;21(1):75–87. [PubMed] [Google Scholar]
- 20.Sarwer DB, Fabricatore AN, Eisenberg MH, Sywulak LA, Wadden TA. Self-reported stigmatization among candidates for bariatric surgery. Obesity (Silver Spring) 2008;16(2):S75–79. doi: 10.1038/oby.2008.450. [DOI] [PubMed] [Google Scholar]
- 21.Puhl RM, Heuer CA. Obesity stigma: important considerations for public health. Am J Public Health. 2010;100(6):1019–1028. doi: 10.2105/AJPH.2009.159491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Latner JD, Simmonds M, Rosewall JK, Stunkard AJ. Assessment of obesity stigmatization in children and adolescents: modernizing a standard measure. Obesity (Silver Spring) 2007;15(12):3078–3085. doi: 10.1038/oby.2007.366. [DOI] [PubMed] [Google Scholar]
- 23.Farrow CV, Tarrant M. Weight-based discrimination, body dissatisfaction and emotional eating: the role of perceived social consensus. Psychol Health. 2009;24(9):1021–1034. doi: 10.1080/08870440802311348. [DOI] [PubMed] [Google Scholar]
- 24.Hopkinson J, Corner J. Helping patients with advanced cancer live with concerns about eating: a challenge for palliative care professionals. J Pain Symptom Manage. 2006;31(4):293–305. doi: 10.1016/j.jpainsymman.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 25.Kildal M, Andersson G, Fugl-Meyer AR, Lannerstam K, Gerdin B. Development of a brief version of the Burn Specific Health Scale (BSHA-B) J Trauma. 2001;51(4):740–746. doi: 10.1097/00005373-200110000-00020. [DOI] [PubMed] [Google Scholar]
- 26.Kildal M, Andersson G, Gerdin B. Health status in swedish burn patients. Assessment utilising three variants of the Burn Specific Health scale. Burns. 2002;28(7):639–645. doi: 10.1016/s0305-4179(02)00111-0. [DOI] [PubMed] [Google Scholar]
- 27.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 28.United Nations Research Institute for Social Development. Social Integration: Approaches and Issues; UNRISD Briefing Paper No. 1; 1994. [Google Scholar]
- 29.Üstün TB, Kostanjsek N, Chatterji S, Rehm S. [Accessed July 9, 2011];Measuring Health and Disability Manual for WHO Disability Assessment Schedule WHODAS 2.0. 2010 http://whqlibdoc.who.int/publications/2010/9789241547598_eng.pdf.
- 30.Osterkamp LK. Current perspective on assessment of human body proportions of relevance to amputees. J Am Diet Assoc. 1995;95(2):215–218. doi: 10.1016/S0002-8223(95)00050-X. [DOI] [PubMed] [Google Scholar]
- 31.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320(7244):1240–1243. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cole TJ, Flegal KM, Nicholls D, Jackson AA. Body mass index cut offs to define thinness in children and adolescents: international survey. BMJ. 2007;335(7612):194. doi: 10.1136/bmj.39238.399444.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention, National Center for Health Statistics. [Accessed June 2, 2012];Growth Charts. http://www.cdc.gov/growthcharts/
- 34.Stylianos S, Eichelberger MR. Pediatric trauma. Prevention strategies. Pediatr Clin North Am. 1993;40(6):1359–1368. doi: 10.1016/s0031-3955(16)38666-7. [DOI] [PubMed] [Google Scholar]
- 35.Paxton SJ, Wertheim EH, Gibbons K, Szmukler GI, Hillier L, Petrovich JL. Body image satisfaction, dieting beliefs, and weight loss behaviors in adolescent girls and boys. Journal of Youth and Adolescence. 1991;20(3) doi: 10.1007/BF01537402. [DOI] [PubMed] [Google Scholar]
- 36.Palmer L, Erickson S, Shaffer T, Koopman C, Amylon M, Steiner H. Themes arising in group therapy for adolescents with cancer and their parents. Int J Rehabil Health. 2000;5(1):43–54. [Google Scholar]
- 37.Fauerbach JA, Heinberg LJ, Lawrence JW, et al. Effect of early body image dissatisfaction on subsequent psychological and physical adjustment after disfiguring injury. Psychosom Med. 2000;62(4):576–582. doi: 10.1097/00006842-200007000-00017. [DOI] [PubMed] [Google Scholar]
- 38.Rybarczyk B, Nyenhuis DL, Nicholas JJ, Cash SM, Kaiser J. Body Image, Perceived Social Stigma, and the Prediction of Psychosocial Adjustment to Leg Amputation. Rehabilitation Psychology. 1995;40(2):95–110. [Google Scholar]
- 39.Sheridan RL, Hinson MI, Liang MH, et al. Long-term outcome of children surviving massive burns. JAMA. 2000;283(1):69–73. doi: 10.1001/jama.283.1.69. [DOI] [PubMed] [Google Scholar]
- 40.Hansson LM, Karnehed N, Tynelius P, Rasmussen F. Prejudice against obesity among 10-year-olds: a nationwide population-based study. Acta Paediatr. 2009;98(7):1176–1182. doi: 10.1111/j.1651-2227.2009.01305.x. [DOI] [PubMed] [Google Scholar]