Abstract
The cortisol awakening response (CAR) is a normative rise in cortisol levels across the 30 minutes post awakening. Both the levels and the degree of change in cortisol across this time period are sensitive to the perceived challenges of the day and are thought to prepare the individual to meet these tasks. However, working parents of young children may be under unique strains at this time as they attempt to simultaneously care for their children while also preparing themselves for the workday ahead. In these analyses we examined the contributions of both work and parenting stress on maternal cortisol levels and awakening responses, and how these relationships differed on workdays compared to non-workdays. To do this, saliva samples were collected from 56 working mothers (25% single) with a child between the ages of 2 and 4 years old (mode = 2 children), at awakening and 30-minutes post awakening. Samples were collected on four consecutive days—two non-workdays followed by two workdays. Analyses revealed mothers reporting higher levels of parenting stress had higher average AM cortisol on workdays compared to non-workdays. Further, mothers reporting a combination of high job strain and high parenting stress had significantly higher cortisol levels, and steeper CAR increases on workdays compared to non-workdays. Findings are discussed by integrating knowledge from the fields of parenting stress, work-family, and stress physiology.
Keywords: cortisol awakening response, parenting stress, job strain, mothers
Introduction
Our understanding of biosocial interactions within the family context has rapidly advanced with the ability to examine physiological processes in naturalistic and family salient settings (e.g., Booth, Carver, & Granger, 2000). In particular, for dual-earner families who spend a large portion of their waking hours apart, evening reunions have revealed an intersection of work and family, as well as behavior and biology (e.g., Campos, Graesch, Repetti, Bradbury, & Ochs, 2009; Saxbe, Repetti, & Nishina, 2008). Interestingly, morning departures, which also contain unique behavioral and physiological processes, have received little attention in biosocial examinations of family functioning. Workday mornings create a “collision” of two worlds, as mothers of young children are charged with caring for, and attending to, their children while also mentally and physically preparing themselves for the workday ahead. In addition, the distinct physiological processes that occur at the start of the day increase the relevance of examining families in the morning. In particular, cortisol levels increase dramatically in response to awakening, and individual differences in morning cortisol levels and degree of change across the morning have unique associations with indices of behavior and health (for review, see Fries, Dettenborn, & Kirschbaum, 2009). Surprisingly, to the best of our knowledge, no study has examined how work stress, parenting stress, and morning stress physiology interact. To fill this knowledge gap, the combined contributions of work and parenting stress on morning cortisol levels and awakening responses in working mothers of preschool-aged children were examined.
Cortisol and the cortisol awakening response
The hypothalamic-pituitary-adrenal (HPA) axis is a primary component of the psychobiology of the stress response. Cortisol, the end product of the HPA axis, functions to increase the availability of glucose, thus preparing the body to face perceived challenges (Nelson, 2011). Cortisol production and secretion follow a distinct rhythm across the day marked by a rise in the morning and a decline across the afternoon. The sharp burst of cortisol in the first hour post-awakening (i.e., the cortisol awakening response or CAR) is, in part, caused by a shift in activity in the suprachiasmatic nucleus (SCN). During sleep, the SCN inhibits HPA axis activity; however, upon awakening the SCN stimulates HPA activity resulting in an increase in cortisol (for review, see Clow, Hucklebridge, Stalder, Evans, & Thorn, 2010). Previous studies have found cortisol levels to rise roughly 50 – 75% within the first 30 to 45 minutes after awakening (e.g., Wilhelm et al., 2007). Approximately 75% of healthy subjects exhibit a CAR (Wüst, Federenko, Hellhammer, & Kirschbaum, 2000), with the degree of the rise being relatively stable across consecutive days (Pruessner et al., 1997).
An emerging literature has linked morning cortisol levels and the CAR to perceived stress, and long-term mental and physical health. However, these studies have produced mixed results regarding the direction of the effect between psychological stress and the CAR. For example, increased CARs have been found in individuals reporting higher social stress, worrying, and job demands (Kunz-Ebrecht et al., 2004; Wüst et al., 2000), while blunted CARs have been associated with depression and chronic exposure to economic strain (Huber et al., 2006; Ranjit et al., 2005). Likewise, morning cortisol levels have been found to be positively related to general life stress and posttraumatic stress syndrome (Chida et al., 2009), but attenuated in women with chronic fatigue syndrome (Nater et al., 2008). Altogether it appears that morning cortisol and well-being follow an inverted-U function, with high and low levels, and steep and flat inclines, related to worse health outcomes (for review, see Fries et al., 2009).
Work stress and stress physiology
Work environments characterized by high levels of demand and low levels of control (i.e., job strain), are known to be detrimental to employee health and well-being (Theorell & Karasek, 1996). Theoretical and empirical evidence suggest activation of the HPA axis across the day may provide a link between stressful work environments and health outcomes (e.g., McEwen, 1998). Physiological examinations have found workdays to be associated with steeper CARs, with negative perceptions of the upcoming workday mediating the accentuated cortisol response (e.g., Pruessner et al., 1999). Further, steeper CAR inclines on workdays have been found in individuals reporting higher job strain and lower perceived job control (Karlson et al., 2011; Maina, Palmas, Bovenzi, & Filon, 2009). However, the behavioral and physiological responses to stress and work may function differently for women and mothers (Taylor, Klein, Lewis, Gruenewald, Gurung, & Updegraff, 2000).
Employment affords many women mental and physical health benefits (for review, see Repetti et al., 1989), yet working mothers tend to be under unique strains, attempting to balance both work and family demands (e.g., Walker & Best, 1991). Specifically, working mothers pay the price of lost sleep, reduced leisure time, and feeling overloaded and stressed by their multiple roles (e.g., Presser, 1995). Thus, working mothers may represent a population at high risk of dysregulated stress physiology. Interestingly, compared to men, women have been found to exhibit higher morning cortisol levels and CARs (Maina et al., 2009; Steptoe, Cropley, Griffith, & Kirschbaum, 2000) as well as steeper awakening response inclines on workdays (Kunz-Ebrecht et al., 2004). These gender differences are posited to stem from workload imbalances at home (Kunz-Ebrecht et al., 2004), and preliminary evidence supports this notion. In particular, having a dependent child, high levels of family strain (Luecken et al., 1997), and increased time devoted to household chores (Saxbe, Repetti, & Graesch, 2011), have all been related to higher cortisol levels on workdays. Taken together, this evidence suggests stressors at work may be accentuated by those at home, interactively contributing to women’s physiological profiles.
Parenting stress and stress physiology
Parenting a young child can be a challenge (Brame, Nagin, & Temblay, 2001), causing frustrations and irritations that have the potential to occur on a daily basis (Crnic & Greenberg, 1990). While some degree of parenting stress is normative, chronic negative perceptions of parenting and stressors revolving around parenting have been negatively related to parental life satisfaction, psychological well-being, and marital quality (Crnic & Booth, 1991; Lavee, Sharlin, & Katz, 1996). Thus, there is reason to believe that parenting stress is more than skin deep, and has the potential to impact physiology (Adam & Gunnar, 2001).
While no studies have examined the relationship between normative parenting stressors and maternal morning cortisol, findings from the caregiving literature highlight the potential for this relationship. Studies have shown caregivers of chronically ill adults exhibit higher awakening cortisol levels (de Vugt et al., 2005) and steeper awakening responses (Wahbeh, Kishiyama, Zajdel, & Oken, 2008) than non-caregivers. Parents of children with disabilities also show physiological dysregulation, exhibiting lower overall cortisol levels across the day (Barker, Greenberg, Seltzer, & Almeida, 2012; Seltzer et al., 2010) and less pronounced afternoon declines (Seltzer et al., 2009). A primary aim of this study is to examine whether these physiological processes occur in normative parenting situations.
Work, family, and stress physiology
To the best of our knowledge, no studies have examined work, parenting, and stress physiology; however, recent studies have connected work, marital relationships, and stress physiology. Specifically, marital problems have been found to potentiate the link between work stress and wives’ physiological arousal (Slatcher, Robles, Repetti, & Fellows, 2010) and reduced end of day cortisol recovery (Saxbe, Repetti, & Nishina, 2008). These studies corroborate sociological examinations of the interactions between work and family, and create a foundation for studies such as this one, exploring work, parenting, and physiological processes. Despite the dearth in literature, we predict that parenting stress will be related to working mothers’ physiology above and beyond the contribution of job strain. Because previous examinations with morning cortisol have found caregiving stress to be related to higher levels and slopes, we predict high parenting stress to be related to higher morning cortisol levels and steeper CARs, after controlling for job strain. We will also examine workday as a moderator, and predict parenting stress will have a more profound effect on workdays, when mothers must meet the demands of work and family, compared to non-workdays. Lastly, we will expand upon the existing research and examine the combination of job strain and parenting stress across work and non-workdays. Existing research has consistently found negative work environments to be related to higher cortisol levels and greater CARs. Thus, we hypothesize that mothers who perceive high levels of stress in both their work and parenting role will have the highest morning cortisol levels and steepest awakening response inclines on workdays.
Method
Participants
Fifty-six working mothers of preschool-aged children were recruited through fliers posted in local child care centers and public places for participation in the study. Eligibility criteria required that mothers were employed outside the home, were the biological mother of a child between the ages of 2 and 4, and were free of chronic illness. Pregnant mothers were excluded regardless of trimester. Fifty-two percent (51.8%) of the sample worked 40 hours per week or more (M = 35.11 hr, SD = 9.69, range: 11 – 60 hours/week), 94.6% worked 20 hours or more, and the remaining (n = 3) worked under 20 hours.
Mothers ranged in age from 22 to 43 years (M = 31.13 years, SD = 4.82), and the majority (75%) were married at the time of this study. Mothers had between one and four children under the age of 18 living in the home (mode = 2 children), with the target child (35.7% male) being on average 3.47 years of age (SD = .92). The majority of mothers (80.4%) were non-Hispanic white and 62.5% had at least a Bachelor’s degree. Approximately fifty percent (51.7%) of the mothers reported their combined annual household income at or below $59,999.
Procedure
Participants selected locations to meet individually with research assistants to review the study protocol and learn saliva collection techniques at the time of consent. Participants collected saliva twice a day (immediately upon waking and again 30 min later) for four consecutive days (two non-workdays followed by two workdays). On each morning that saliva was collected, participants filled out questionnaires designed to assess compliance with the saliva samplings. During the days of collection, participants also filled out a series of questionnaires assessing demographic information, the work environment, and perceptions of parenting. Families were compensated 100 dollars after returning the questionnaires and saliva samples.
Measures
Job strain
Participants filled out an 18-item self-report scale consisting of three main components of the job strain model: Job Demands, Job Control, and Skill Discretion (Karasek & Theorell, 1990). The Job Demands subscale provided a measure of perceptions of work-related demands and was comprised of four items (e.g., “Do you have to work very intensely?”). Fourteen items assessed Job Control, measuring the extent to which respondents feel they have control over what happens in the work place (e.g., “Do you have a choice in deciding how you do your job?”). Finally, Skill Discretion was measured by six items and yielded an assessment of perceptions of the use of skills and the ability to learn new and interesting things in one’s work (e.g., “Do you have the possibility of learning new things through your work?”). Respondents were asked to identify the frequency with which these situations occur in the workplace on a Likert-type scale, ranging from often to never. Internal consistency for the three subscales was .63, .88, and.75, respectively. Following Steptoe et al. (2000), a composite variable was created to index perceptions of Job Strain, calculated by the following equation: Job Strain = (Job Demands)/(Job Control + Skill Discretion). Higher scores indicate greater job strain.
Parenting stress
Parenting stress was assessed using a composite of the Parenting Daily Hassles questionnaire and the Parenting Stress Index-Short Form. The Parenting Daily Hassles questionnaire (PDH; Crnic & Greenberg, 1990) is a 20-item self-report measure of the frequency and intensity of minor everyday events that occur in the context of parenting and in parent-child interactions. Parents were asked to report on a Likert-type scale both the frequency (‘1’ = never to ‘5’ = constantly) and how much of a hassle they experience (‘1’ = no hassle to ‘5’ = big hassle) with items such as: “The kids demand that you entertain or play with them.” Mean scores were computed with higher scores indicating greater frequency or intensity of events, respectively; internal consistency was high for both Frequency (α = .82) and Intensity (α = .83). Previous literature has found this measure to be reliable (α = .90) and to exhibit strong concurrent validity (Crnic & Greenberg, 1990). The Parenting Stress Index-Short Form (PSI-SF; Abidin, 1995) is a 36-item self-report questionnaire measuring responses on a 5-point Likert scale (ranging from strongly agree to strongly disagree). For the current analyses, the Parental Distress and Parent-Child Dysfunctional Interaction subscales were used. The Parental Distress (12 items) subscale measures distress occurring as a result of personal characteristics (for example, depression) or from perceived life limitations resulting from caring for children (e.g., “I feel myself giving up more of my life to meet my children’s needs than I ever expected”). The Parent-Child Dysfunctional Interaction (12 items) subscale yields a measure of the degree to which parents are dissatisfied with parent-child interactions and find their children unacceptable (e.g., “When I do things for my child, I get the feeling that my efforts are not appreciated very much”). Items were reverse coded with mean scores reflecting greater parental distress or parent-child dysfunctional interactions. The PSI-SF is a valid measure of parenting perceptions (Haskett et al., 2006) and consistent with previous research (McBride et al., 2002), internal consistency coefficients were .81 and .85, respectively. Subscales from the PDH and the PSI-SF were standardized and summed to create a single measure of the experience of parenting stress. Inter-correlations between the subscales ranged from .23 – .64 (ps = .10 – .001).
The psychobiology of stress
Participants collected two saliva samples, one upon awakening and one 30 min post awakening, on two consecutive non-workdays followed by two consecutive workdays. Research assistants called participants the night before their first collections to remind them to begin the following morning. At this time they were reminded not to eat, drink, or smoke before collecting their second sample; however, to increase hydration, they were asked to drink a glass of water 10 min before their second collection. Participants were asked to collect their first sample immediately at awakening, right upon opening their eyes, and before getting out of bed.
Participants expressed saliva through a short straw into a 1.8 mL cryogenic vial and were instructed to immediately store the sample in the freezer. Samples were transported on ice to Purdue University and then frozen at −80 °C until assayed. Samples were assayed for salivary cortisol using a highly sensitive enzyme immunoassay (Salimetrics, State College, PA). The test used 25µL of saliva (for singlet determinations), had a range of sensitivity from 0.007 to 1.8 g/dL, and had average intra- and inter-assay coefficients of variation of less than 10% and 15%, respectively. All samples were assayed in duplicate and the average of the duplicates was used in all analyses. Cortisol values were natural log transformed to correct for skewness.
Saliva Collection Questionnaire
On each morning of their saliva collections participants filled out a questionnaire designed to assess compliance with collection procedures. Participants were asked questions about the night before and the morning of each collection (e.g., “how many hours did you sleep,” “what time did you wake up,” “what time did you go to bed”) and what time they collected each sample. Following Broderick et al. (2004), a 15 minute “compliance window” was employed. First morning samples that were collected within 15 min of awakening, and second samples collected between 15 and 45 min post awakening, were considered compliant. Non-compliant samples (n = 7) were not included in the analyses. Time between first and second collections ranged from 20 to 45 min.
Out of the 448 samples collected, 11% were missing. This resulted in 35 of the 56 participants having cortisol values for all eight collection points. Fourteen participants were missing one sample, two were missing two samples, and five were missing three samples or more. Missing cortisol samples were due to poor quality of sample or insufficient amount of saliva, preventing assay. Samples with a coefficient of variation larger than 20 were removed. Full information maximum likelihood was used for all models, which has been shown to produce unbiased parameter estimates and standard errors in models with missing data.
Analytical strategy
To assess the effect of parenting on morning cortisol levels and slopes, all analyses were run with average morning cortisol and CAR as dependent variables. Average AM cortisol was computed by averaging the awakening and the 30 min post samples. CAR was computed by a change score subtracting awakening cortisol levels from the cortisol levels at 30 min post awakening. Mothers needed values for both the awakening and 30 min post sample to calculate the average cortisol levels and CARs. First, descriptives of AM cortisol levels and CARs will be provided along with behavioral and physiological differences between work and non-workdays. The main analyses employ a series of mixed models (Bryk & Raudenbush, 1992) examining AM cortisol levels and CARs on work and non-workdays, in relation to job strain and parenting stress. At Level 1 we modeled the within-person workday/non-workday association with cortisol, while at Level 2 we introduced our between-person variables (i.e., job strain, parenting stress, and interactions). Subsequent models also included interactions. For CAR, the modeling of Level 1 and Level 2 equations was identical to the levels model, apart from the dependent variable and covariates.
| Level 1: |
| Level 2: |
All modeling was carried out using Proc MIXED in SAS 9.2 (SAS Institute, 2008); all variables were standardized and the number of children under the age of 5 living in the household was controlled for in all analyses. Following Kunz-Ebrecht et al (2003) analyses and discussion focus on fixed effects. Dawson and Richter’s (2006) method was employed to plot interaction effects. See Table 1 for a correlation matrix of relevant variables.
Table 1.
Job Strain and Parenting Stress among Working Mothers: Descriptive Statistics and Correlations of Key Variables (N = 56).
| Variables | M | SD | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|---|
| 1. Job Strain | .07 | .02 | — | |||
| 2. Parenting Stress | .06 | 3.04 | .11 | — | ||
| 3. AM Cortisol Levels | .82 | .71 | −.15* | .04 | — | |
| 4. CAR | .06 | .83 | .05 | .06 | .14+ | — |
Note. Job Strain and Parenting Stress centered at their respective means for main analyses.
p < .10.
p < .05.
Results
Preliminary and descriptive analyses
Cortisol
Intercept only models for both AM cortisol levels and CAR revealed that 47.1% of the variability in AM cortisol levels and 13.5% of the variation in CAR is due to between person differences. Furthermore, the standard error of the variance in the intercepts was significant for AM cortisol levels (p < .001) and CAR (p < .01), indicating there is significant variance around the parameter estimate that may be explained by additional predictors.
On average, mother’s cortisol levels increased roughly 60% from waking (M = .37 ug/dL, SD = .23) to 30 min post (M = .44 ug/dL, SD = .32) controlling for wake time, β = .16, p < .01 (range: −0.77 ug/dL to 1.14 ug/dL). Maternal age, number of hours slept, bed time, medication use, amount of time elapsed between awakening and the first sample, amount of time elapsed between the first and second samples, report of health status, household income, marital status, and smoking status were examined as potential control variables. Wake time, β = −.11, p < .001, and household income, β = .11, p = .04, were related to AM cortisol levels; earlier wake times and higher income were related to higher average AM cortisol. No potential control variables were related to CAR. Wake time and income were controlled for in all AM cortisol models. Lastly, higher AM cortisol levels were related to steeper awakening responses, β = .16, p = .04.
Comparing workdays to non-workdays
Mothers slept for significantly less time on nights before work (M = 7 hr 40 min, SD = 1 hr 13 min), than nights before a non-workday (M = 8 hr 24 min, SD = 1 hr 59 min), β = −.75, p < .001, waking up about an hour earlier on workdays (M = 6:44, SD = 0:53) than non-workdays (M = 7:50, SD = 1:13). Women had higher AM cortisol levels, β = .15, p = .04, and steeper CARs, β = .10, p = .006 on workdays (levels: M = .44 ug/dL, SD = .20; CAR: M = .11 ug/dL, SD = .26) compared to non-workdays (levels: M = .37 ug/dL, SD = .24; CAR: M = .01 ug/dL, SD = .19). However, the relationship between workday and cortisol levels was no longer significant after controlling for wake time. None of the potential control variables interacted with workday to predict AM cortisol or CAR. Compliance did not differ on work compared to non-workdays, χ2(1) = .34, ns.
Main analyses
Controlling for job strain, do parenting stressors predict AM cortisol levels or awakening responses?
A mixed model (see Table 2 and 3, Model 1) was used to examine maternal report of parenting stressors as a predictor of average AM cortisol levels and awakening responses across the four collection days. Neither job strain nor parenting stress were related to AM cortisol levels or CAR.
Table 2.
Mixed Models Predicting AM Cortisol Levels from Parenting Stress and Examining Workday (Model 2) and Job Strain as Moderators (Model 3; N = 56)
| Model | Null | 1 | 2 | 3 |
|---|---|---|---|---|
| Fixed Effects | Estimate (SE) | Estimate (SE) | Estimate (SE) | Estimate (SE) |
| Intercept | −1.03 (.04)*** | −1.27 (.18) | −1.26 (.18) | −1.21 (.18) |
| #Children <5 | −.13 (.08) | −.13 (.08) | −.14 (.07) | |
| Wake Time | −.08 (.03)* | .10 (.03)* | −.10 (.03)* | |
| Incomea | .11 (.04)** | .11 (.04)** | .10 (.03)** | |
| Workdayb | .08 (.08) | .06 (.07) | .03 (.07) | |
| Job Strain | −.01 (.05) | −.01 (.05) | .01 (.05) | |
| Parenting Stress | .02 (.05) | −.03 (.05) | −.01 (.05) | |
| Parenting X Workday | .14 (.07)* | .23 (.07)** | ||
| Parenting X Job Strain | .07 (.06) | |||
| Job Strain X Workday | .19 (.06)** | |||
| 3-Way Interactionc | .20 (.08)* | |||
Note.
Household income.
Workday: 0 = non-workday, 1 = workday.
Job Strain X Parenting Stress X Workday.
p < .10.
p < .05.
p < .01.
p < .001.
Table 3.
Mixed Models Predicting CAR from Parenting Stress and Examining Workday (Model 2) and Job Strain as Moderators (Model 3; N = 56)
| Model | Null | 1 | 2 | 3 |
|---|---|---|---|---|
| Fixed Effects | Estimate (SE) | Estimate (SE) | Estimate (SE) | Estimate (SE) |
| Intercept | .06 (.02)** | .02 (.05) | .02 (.05) | .03 (.02) |
| #Children <5 | −.01 (.03) | −.01 (.03) | −.01 (.03) | |
| Workdaya | .10 (.04)** | .10 (.04)** | .07 (.04)** | |
| Job Strain | .01 (.02) | .01 (.02) | .02 (.02) | |
| Parenting Stress | .01 (.02) | .01 (.02) | −.01 (.02) | |
| Parenting X Workday | .01 (.04) | .04 (.04) | ||
| Parenting X Job Strain | −.03 (.03) | |||
| Job Strain X Workday | −.05 (.04) | |||
| 3-Way Interactionb | .12 (.04)** | |||
Note.
Workday: 0 = non-workday, 1 = workday.
Job Strain X Parenting Stress X Workday.
p < .10.
p < .05.
p < .01.
p < .001.
Does workday moderate the relationship between parenting stressors and AM cortisol levels or awakening responses?
To examine whether the relationship between parenting stress and morning cortisol levels and awakening responses across the four days depends on workday, a workday by parenting stress interaction was added to the model (see Table 2 and 3, Model 2). Parenting stress and workday interacted to predict maternal cortisol levels, revealing mothers with high parenting stress have higher cortisol levels on workdays than non-workdays. However, mothers reporting lower levels of parenting stress do not experience this workday difference. Parenting stress and workday did not interact to predict CAR.
Does job strain moderate the relationship between parenting stress and maternal cortisol levels or awakening responses across work and non-workdays?
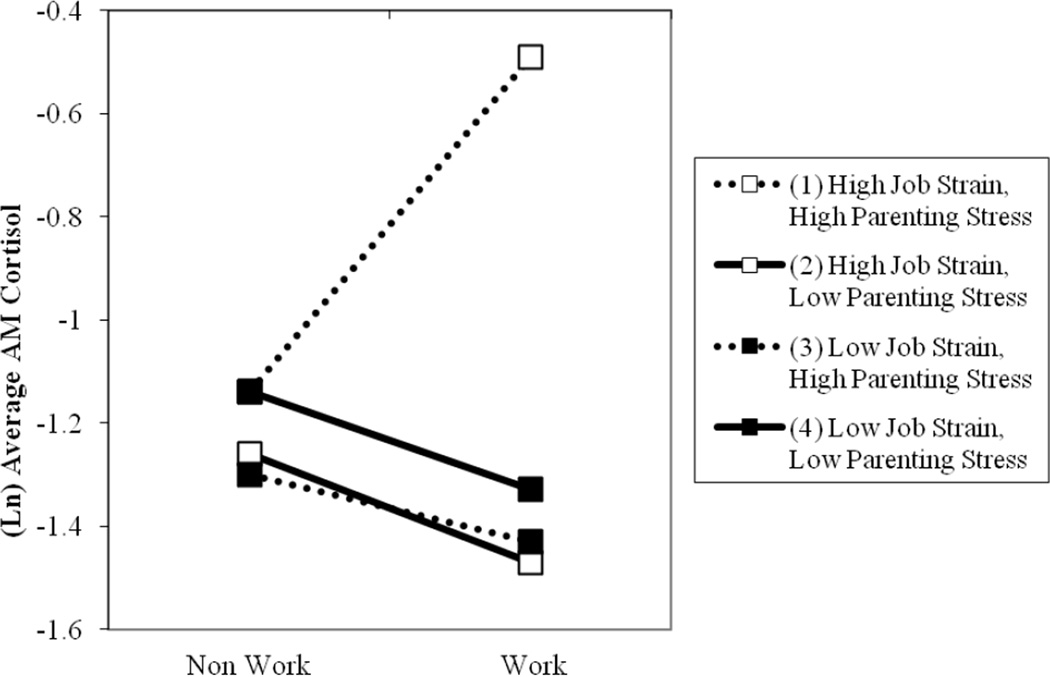
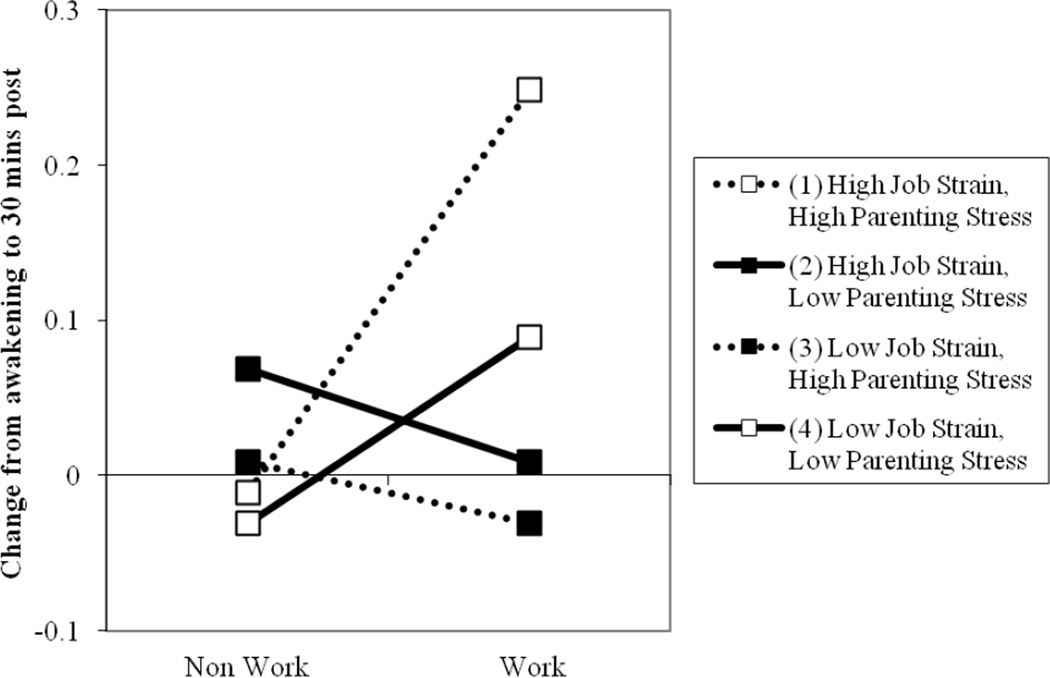
Finally, the third model (see Table 2 and 3) examined the three-way interaction between parenting stress, job strain, and workday. This interaction significantly predicted mother’s average AM cortisol levels (see Figure 1) and CARs (see Figure 2). Plots of simple slopes suggest significantly higher cortisol levels and steeper inclines in CAR on workdays compared to non-workdays in mothers reporting high levels of parenting stress and job strain. Mothers reporting either high parenting stress or high job stress did not appear to have higher AM cortisol levels or steeper CARs on work compared to non-work days. Interestingly, mothers with both low parenting stress and low job strain appear to have moderately steeper CARs on workdays compared to non-workdays.
Figure 1.
Mothers reporting a combination of high parenting stress and high job strain have higher cortisol levels on workdays compared to non-workdays. Plots suggest no other group exhibits a workday/non-work day difference in AM cortisol levels.
Figure 2.
Mothers reporting a combination of high parenting stress and high job strain have higher cortisol awakening responses on workdays compared to non-workdays. Mothers reporting a combination of low parenting stress and low job strain also have higher cortisol awakening responses on workdays compared to non-workdays Plots suggest other groups do not exhibit a workday/non-work day difference in CARs.
Follow-up analyses
To better understand the relationship between cortisol (AM levels and CAR) and the stress variables, analyses were re-examined within workday. Interactions between job strain and parenting stress were significant for AM levels, β = .27, p < .001, and CAR, β = .08, p = .04, but only on workdays. The interaction of job strain and parenting stress was not related to non-workday AM cortisol levels, β = .07, ns, or CAR, β = −.03, ns.
Discussion
The purpose of this analysis was to examine the unique and combined contributions of parenting and work stress on maternal stress physiology on work and non-workdays. Psychological and sociological explorations of working mothers have highlighted the strain on personal time and energy mothers feel when juggling the demands of paid work and family obligations (Hochschild & Machung, 2003). Further, physiological examinations have noted women exhibit a workday/non-workday difference in morning cortisol, with higher cortisol on workday mornings (e.g., Kunz-Ebrecht et al., 2004). The current analysis extends and integrates these two related fields of research. While the workday difference in stress physiology was confirmed, subsequent analyses suggested this difference may only occur in mothers with high parenting stress and job strain. In particular, mothers reporting high parenting stress exhibit higher AM cortisol levels on workdays compared to non-workdays. Additionally, job strain moderated this relationship, showing that while the majority of mothers do not show a workday difference in cortisol, mothers reporting high levels of parenting stress and job strain exhibit higher AM cortisol levels and steeper CARs on workdays. These findings are discussed by integrating knowledge from the fields of parenting stress, work-family, and stress physiology.
Contemporary families value closeness and cohesion, striving towards family life marked by high quality, warm relationships among parents and children (e.g., Coontz, 2005; Tubbs, Roy, & Burton, 2005). However, family time often does not meet these idealized expectations (Tubbs et al., 2005) and parent-child relationships often include some degree of conflict (Crouter & Bumpus, 2001). Parenting requires constant adaptation to the changing demands of the child, and coping with the daily stressors of child rearing (Deater-Deckard, 2004). These challenges might make parenting stress particularly detrimental to maternal well-being. Interestingly, the current study did not find support for a main effect of parenting stress on either AM cortisol levels or CAR, indicating that parenting stress alone was not enough to physiologically arouse mothers in the current sample. Past studies finding highly stressed parents to exhibit dysregulated cortisol rhythms have focused on parents with a disabled or chronically ill child (e.g., Seltzer et al., 2010). Studies of parents of ill children have also shown these parents to be under higher levels of stress than parents of typical children (Byrne et al., 2010). Thus, it could be that parenting stress must be outside the normative range to have independent physiological repercussions.
However, our findings suggest that when normative parenting stress is combined with stress from another domain of life, the multiplicative effects of both stressors might strain physiological resources. This phenomenon has been highlighted by past authors, and researchers have been urged to examine the cumulative exposure of multiple stressors (e.g., Deater-Deckard, Dodge, Bates, & Pettit, 1998; Sameroff, 2000) in an attempt to understand the link between physiological stress, and mental and physical health (McEwen, 1998). Indeed, our analyses revealed that mothers reporting high parenting stress and high job strain had higher cortisol levels and steeper CAR inclines on work compared to non-work days. On days when mothers are working, the unique burden of caring for preschool-aged children (Crnic & Booth, 1991) may be accentuated by the perceived challenges of the work day (Crouter & Bumpus, 2001). Work demands have been shown to limit parent’s time available for family matters, as well as deplete their psychosocial resources (e.g., Repetti & Wood, 1997). Thus, perceptions of work challenges when simultaneously performing morning childcare routines, seems to increase HPA activation in mothers with high levels of parenting stress. Importantly, repeated over-activation of the HPA axis may place these mothers at risk for exhaustion, cardiovascular problems, or other mental or physical health problems (e.g., Bellingrath, Weigl, & Kudielka, 2009; McEwen, 1998). However, our analysis gives hope that the burden of high work and family stress only exerts a physiological toll on workdays, with physiological recovery on non-workdays.
Past studies have shown steeper CARs on workdays compared to non-workdays to be normative (e.g., Kunz-Ebrecht et al., 2004) and due to higher levels of worrying and workload on these days (Pruessner et al., 2003; Scholtz et al., 2004). However, in this analysis, mothers reporting low levels of both parenting stress and job strain also exhibited this normative, steeper CAR on workdays. Interestingly, mothers reporting either high parenting stress or job strain (but not both) do not appear to have greater HPA activation, showing no change in average cortisol levels or awakening responses from non-work to workdays. It is not clear why this would occur. Potentially, this “hypoarousal” is also a pathological profile, suggesting mothers’ attenuated responses are insufficient to meet the demands of their upcoming day (Susman, 2006). Likewise, low stress in one domain may create a cross-domain buffering effect. However, if this were the case, we would expect to see mothers with high stress in only one domain to exhibit physiological profiles similar to mothers reporting low stress in both domains. At least for the mothers reporting high parenting stress, it could be that non-workdays are just as full of worry and work as workdays, inhibiting CAR recovery on these days. Importantly, neither of the stress measures employed captured the duration of exposure to the stressor, which may have helped to disentangle the various profiles exhibited in the workday and stress interactions
The heightened stress physiology in stressed mothers may have important ramifications for children. Taylor and colleagues (2000) have proposed a stress response paradigm specific to females and mothers highlighting the unique obligations of a mother. Specifically, in order to effectively calm and soothe a distressed child, mothers may need to suppress their own heightened stress physiology. However, this paradigm is conceptualized around maternal responses to stressors found outside of the mother-child relationship (e.g., predators, threats to mother or offspring survival). The present analyses support the notion that to some mothers, children are a physiological and psychological stressor (Brame, Nagin, & Tremblay, 2001). The mothers in this sample that report high levels of stress in both their work and family lives may find that this high level of stress and physiological activation interferes with their ability to sensitively respond to their child’s needs. Indeed, stress has long been described as a major determinate of parenting behavior (e.g., Belsky, 1984), with highly stressed mothers using harsher and more punitive parenting strategies (e.g., Baker, Heller, & Henker, 2000). Further, recent studies have begun to show parental stress physiology to be an important correlate of parenting behavior (e.g., Martorell & Bugental, 2006). Thus, the present findings raise the possibility that heightened stress physiology may be a mechanism by which parenting stress affects parenting behavior and subsequent child development.
Limitations and future directions
Due to the small sample size and homogeneous nature of the participants, particularly with respect to socioeconomic status and race/ethnicity, this analysis was a preliminary investigation into the physiological profiles of working mothers of young children. Financial resources play a large role in the types of stress an individual faces and their ability to cope with these stressors (e.g., Folkman & Lazarus, 1980). Importantly, parenting stress has been found to be greater in low-income populations (for review, see McLoyd, 1990). Thus, the middle class status of this sample may be masking some of the effects of parenting stress on stress physiology, preventing a true examination of the role of income in the relationship between parenting stress and stress physiology. As a preliminary report, this analysis offers a glimpse into the physiological strains of working mothers and offers a foundation for future research. Future studies should strive to collect more information regarding the activities of mothers in the first 30 min of their morning. Anecdotally, many of the mothers described a rushed and hectic morning to get their children and themselves ready for daycare and work, a feeling that has been noted previously (Mattingly & Bianchi, 2003). A clearer understanding of morning routines may also help uncover intra-individual differences in physiology in relation to psychological and behavioral processes. Further, compliance was assessed through self-report of collection times. Past studies have shown mixed results with this methodology. For example, a recent exploration using a nationally representative sample found self-report to be highly correlated (r = .90) to electronic time stamp (Almeida et al., 2009); however some researchers have questioned its use (Broderick et al., 2004). Future studies should attempt to incorporate objective measures of compliance (e.g., electronic time stamps).
While gender roles in today’s society are less pronounced than in previous decades, certain societal norms still perpetuate gender divisions of labor and create an interesting venue for physiological examination. Mothers tend to be responsible for roughly twice as much of the household chores as men (Stafford, 2008) and the bulk of child care responsibilities (Darling-Fisher & Tiedje, 1990) regardless of maternal employment status. Work-family researchers have long recognized the role strain and conflict (e.g., Goode, 1960) and lower psychological well-being (Coverman, 1989) that arises when roles pose excessive demands. The present analyses provide a potential mechanism by which stressors in multiple life domains impact maternal health and well-being. Specifically, combinations of work and family stressors may create challenges beyond a mother’s coping abilities, and facilitate frequent HPA activation. In the long term, these physiological profiles are known to lead to the development of mental and physical disease (McEwen, 1998). Fortunately, policy change has the potential to positively impact this societal issue. Recent studies have found longer paternal leaves may increase long term paternal involvement (Nepomnyaschy & Waldfogel, 2007), potentially reducing maternal role strain. Similarly, flexible work arrangements seem to benefit both companies and families, increasing the number of hours worked (Hill, Hawkins, Ferris, & Weitzman, 2001) and the perception of a healthy work and family balance (Galinsky, Bond, & Friedman, 1993). The current findings highlight the importance of creating family friendly policies to reduce the mental, physical, and physiological burden of juggling work and family, especially for mothers with young children.
Acknowledgments
We would like to thank the many families who took time out of their busy schedules to participate in this project. We would also like to thank Rebecca Jarvis-Caruthers, Uma Senguttuvan, Elizabeth Langston, and Shilpa Parakh, whose invaluable help made this study possible. The first author was supported by a grant from the National Institute of Child Health and Human Development (R21 HD066269-01A1). The second author was supported by an assistantship from the Agricultural Research Program, Purdue University.
References
- Abidin RR. Parenting Stress Index professional manual. (3rd Edition) Odessa, FL: Professional Assessment Resources; 1995. [Google Scholar]
- Adam EK, Gunnar MR. Relationship functioning and home and work demands predict individual differences in diurnal cortisol patterns in women. Psychoneuroendocrinology. 2001;26:189–208. doi: 10.1016/s0306-4530(00)00045-7. [DOI] [PubMed] [Google Scholar]
- Almeida DM, McGonagle K, King H. Assessing daily stress processes in social surveys by combining stressor exposure and salivary cortisol. Biodemography and Social Biology. 2009;55(2):219–237. doi: 10.1080/19485560903382338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker BL, Heller TL, Henker B. Expressed emotion, parenting stress, and adjustment in mothers of young children with behavior problems. Journal of Child Psychology and Psychiatry. 2000;41:907–915. [PubMed] [Google Scholar]
- Barker ET, Greenberg JS, Seltzer M, Almeida DM. Daily stress and cortisol patterns in parents of adult children with a serious mental illness. Health Psychology. 2012;31(1):130–134. doi: 10.1037/a0025325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellingrath S, Weigl T, Kudielka BM. Chronic work stress and exhaustion is associated with higher allostastic load in female school teachers. Stress: The International Journal on the Biology of Stress. 2009;12(1):37–48. doi: 10.1080/10253890802042041. [DOI] [PubMed] [Google Scholar]
- Belsky J. The determinants of parenting: A process model. Child Development. 1984;55:83–96. doi: 10.1111/j.1467-8624.1984.tb00275.x. [DOI] [PubMed] [Google Scholar]
- Brame B, Nagin DS, Tremblay RE. Developmental trajectories of physical aggression from school entry to late adolescence. Journal of Child Psychology and Psychiatry. 2001;42:503–512. [PubMed] [Google Scholar]
- Broderick JE, Arnold D, Kudielka BM, Kirschbaum C. Salivary cortisol sampling compliance: comparison of patients and healthy volunteers. Psychoneuroendocrinology. 2004;29:636–650. doi: 10.1016/S0306-4530(03)00093-3. [DOI] [PubMed] [Google Scholar]
- Bryk AS, Raudenbush SW. Hierachical linear models. Newbury Park, CA: Sage; 1992. [Google Scholar]
- Byrne MB, Hurley DA, Daly LL, Cunningham CG. Health status of caregivers of children with cerebral palsy. Child: care, health, and development. 2010;36(5):696–702. doi: 10.1111/j.1365-2214.2009.01047.x. [DOI] [PubMed] [Google Scholar]
- Campos B, Graesch AP, Repetti R, Bradbury T, Ochs E. Opportunity for interaction? A naturalistic observation study of dual-earner families after work and school. Journal of Family Psychology. 2009;23(6):798–807. doi: 10.1037/a0015824. [DOI] [PubMed] [Google Scholar]
- Chida Y, Steptoe A. Cortisol awakening response and psychosocial factors: A systematic review and meta-analysis. Biological Psychology. 2009;80:265–278. doi: 10.1016/j.biopsycho.2008.10.004. [DOI] [PubMed] [Google Scholar]
- Clow A, Hucklebridge F, Stalder T, Evans P, Thorn L. The cortisol awakening response: more than a measure of HPA axis function. Neuroscience and Biobehavioral Reviews, special issue: Psychophysiological Biomarkers of Health. 2010;35:97–103. doi: 10.1016/j.neubiorev.2009.12.011. [DOI] [PubMed] [Google Scholar]
- Coontz S. The evolution of matrimony: The changing social context of marriage. Annals of the American Psychotherapy Assn. 2005;8(4):30–33. Retrieved from http://www.annalsofpsychotherapy.com/ [Google Scholar]
- Coverman S. Role overload, role conflict, and stress: Addressing consequences of multiple role demands. Social Forces. 1989;67:965–983. [Google Scholar]
- Crnic KA, Greenberg MT. Minor parenting stresses with young children. Child Development. 1990;61:1628–1637. doi: 10.1111/j.1467-8624.1990.tb02889.x. [DOI] [PubMed] [Google Scholar]
- Crnic KA, Booth CL. Mothers and fathers perceptions of daily hassles of parenting across early childhood. Journal of Marriage and Family. 1991;53:1042–1050. [Google Scholar]
- Crouter AC, Bumpus MF. Linking parents' work stress to children's and adolescents' psychological adjustment. Current Directions in Psychological Science. 2001;10:156–160. [Google Scholar]
- Darling-Fisher CS, Tiedje LB. The impact of maternal employment characteristics on fathers' participation in child care. Family Relations. 1990;39:20–26. [Google Scholar]
- Dawson JF, Richter AW. Probing three-way interactions in moderated multiple regression: Development and application of a slope difference test. Journal of Applied Psychology. 2006;91(4):917–926. doi: 10.1037/0021-9010.91.4.917. [DOI] [PubMed] [Google Scholar]
- Deater-Deckard K. Parenting stress. New Haven, CT: Yale University Press; 2004. [Google Scholar]
- Deater-Deckard K, Dodge KA, Bates JE, Pettit GS. Multiple risk factors in the development of externalizing behavior problems: Group and individual differences. Development and Psychopathology. 1998;10(3):469–493. doi: 10.1017/s0954579498001709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Vugt ME, Nicolson NA, Aalten P, Lousberg R, Jolle J, Verhey FRJ. Behavioral problems in dementia patients and salivary cortisol patterns in caregivers. J Neuropsychiatry Clin. Neurosci. 2005;17:201–207. doi: 10.1176/jnp.17.2.201. [DOI] [PubMed] [Google Scholar]
- Folkman S, Lazarus RS. An analysis of coping in a middle-aged community sample. Journal of Health and Social Behavior. 1980;21(3):219–239. [PubMed] [Google Scholar]
- Fries E, Dettenborn L, Kirschbaum C. The cortisol awakening response (CAR): Facts and future directions. International Journal of Psychophysiology. 2009;72:67–73. doi: 10.1016/j.ijpsycho.2008.03.014. [DOI] [PubMed] [Google Scholar]
- Galinsky E, Bond JT, Friedman DE. The changing workforce: Results of the national study. New York: Families and Work Institute; 1993. [Google Scholar]
- Goode WJ. A theory of role strain. American Sociological Review. 1960;25(4):483–496. [Google Scholar]
- Haskett ME, Ahern LS, Ward CS, Allaire JC. Factor structure and validity of the parenting stress index-short form. Journal of Clinical Child & Adolescent Psychology. 2006;35(2):302–312. doi: 10.1207/s15374424jccp3502_14. [DOI] [PubMed] [Google Scholar]
- Hill EJ, Hawkins AJ, Ferris M, Weitzman M. Finding an extra day a week: The positive influence of perceived job flexibility on work and family life balance. Family Relations. 2001;50:49–58. [Google Scholar]
- Hochschild AR, Machung A. The second shift: Working parents and the revolution at home. 2nd ed. New York: Penguin Books; 2003. [Google Scholar]
- Karasek RA, Theorell T. Healthy Work. New York: Basic Books; 1990. [Google Scholar]
- Karlson BK, Frida E, Hansen AM, Garde AH, Ørbæk P. Cortisol variability and self-reports in the measurement of work-related stress. Stress & Health. 2011;27(2):e11–e24. doi: 10.1002/smi.1330. [DOI] [PubMed] [Google Scholar]
- Kunz-Ebrecht SR, Kirschbaum C, Marmot M, Steptoe A. Differences in cortisol awakening response on workdays and weekends in women and men from the Whitehall II cohort. Psychoneuroendocrinology. 2004;29:516–528. doi: 10.1016/s0306-4530(03)00072-6. [DOI] [PubMed] [Google Scholar]
- Lavee Y, Sharlin S, Katz R. The effect of parenting stress on marital quality. Journal of Family Issues. 1996;17:114–135. [Google Scholar]
- Luecken LJ, Suarez EC, Kuhn CM, Barefoot JC, Blumenthal JA, Siegler IC, Williams RB. Stress in employed women: Impact of marital status and children at home on neurohormone output and home strain. Psychosomatic Medicine. 1997;59:352–359. doi: 10.1097/00006842-199707000-00003. Retrieved from http://www.psychosomaticmedicine.org. [DOI] [PubMed] [Google Scholar]
- Maina G, Palmas A, Bovenzi M, Filon FL. Salivary cortisol and psychosocial hazards at work. American Journal of Industrial Medicine. 2009;52(3):251–260. doi: 10.1002/ajim.20659. [DOI] [PubMed] [Google Scholar]
- Martorell GA, Bugental DB. Maternal variations in stress reactivity: Implications for harsh parenting practices with very young children. Journal of Family Psychology. 2006;20:641–647. doi: 10.1037/0893-3200.20.4.641. [DOI] [PubMed] [Google Scholar]
- Mattingly MJ, Bianchi SM. Gender differences in the quantity and quality of free time: The U.S. experience. Social Forces. 2003;81(3):999–1030. [Google Scholar]
- McBride BA, Schoppe SJ, Rane TR. Child characteristics, parenting stress, and parental involvement: Fathers versus mothers. Journal of Marriage and Family. 2002;64(4):998–1011. [Google Scholar]
- McEwen BS. Stress, adaptation, and disease: Allostasis and allostatic load. Ann N Y Acad Sci. 1998;840:33–44. doi: 10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- McLoyd VC. The impact of economic hardship on black families and children: Psychological distress, parenting, and socioemotional development. Child Development. 1990;61(2):311. doi: 10.1111/j.1467-8624.1990.tb02781.x. [DOI] [PubMed] [Google Scholar]
- Nater UM, Maloney E, Boneva RS, Gurbaxani BM, Lin JM, Jones JF, Heim C. Attenuated morning salivary cortisol concentrations in a population-based study of persons with chronic fatigue syndrome and well controls. Journal of Clinical Endocrinology and Metabolism. 2008;93(3):703–709. doi: 10.1210/jc.2007-1747. [DOI] [PubMed] [Google Scholar]
- Nelson RJ. An Introduction to Behavioral Endocrinology. Sunderland, MA: Sinauer Associates, Inc.; 2011. [Google Scholar]
- Nepomnyaschy L, Waldfogel J. Paternity leave and fathers’ involvement with their young children. Community, Work & Family. 2007;10(4):427–453. [Google Scholar]
- Presser HB. Job, family, and gender: Determinants of nonstandard work schedules among employed americans in 1991. Demography. 1995;32(4):577–598. [PubMed] [Google Scholar]
- Pruessner JC, Wolf OT, Hellhammer DH, Buske-Kirschbaum A, von Auer K, Jobst S, Kirschbaum C. Free cortisol levels after awakening: A reliable biological marker for the assessment of adrenocortical activity. Life Sci. 1997;61:2539–2549. doi: 10.1016/s0024-3205(97)01008-4. [DOI] [PubMed] [Google Scholar]
- Pruessner JC, Hellhammer DH, Kirschbaum C. Burnout, perceived stress, and cortisol responses to awakening. Psychosomatic Medicine. 1999;61:197–204. doi: 10.1097/00006842-199903000-00012. Retrieved from http://www.psychosomaticmedicine.org. [DOI] [PubMed] [Google Scholar]
- Pruessner M, Hellhammer DH, Pruessner JC, Lupien SJ. Self-reported depressive symptoms and stress levels in healthy young men: Associations with the cortisol response to awakening. Psychosomatic Medicine. 2003;65(1):92. doi: 10.1097/01.psy.0000040950.22044.10. [DOI] [PubMed] [Google Scholar]
- Ranjit N, Young EA, Kaplan G. Material hardship alters the diurnal rhythm of salivary cortisol. International Journal of Epidemiology. 2005;34(5):1138–1143. doi: 10.1093/ije/dyi120. [DOI] [PubMed] [Google Scholar]
- Repetti RL, Matthews KA, Waldron I. Employment and women's health: Effects of paid employment on women's mental and physical health. American Psychologist. 1989;44:1394–1401. [Google Scholar]
- Repetti RL, Wood J. Effects of daily stress at work on mothers' interactions with preschoolers. Journal Of Family Psychology. 1997;11(1):90–108. [Google Scholar]
- Sameroff AJ. Ecological perspectives on developmental risk. In: Osofsky JD, Fitzgerald HE, editors. WAIMH handbook of infant mental health: Vol. 4. infant mental health in groups at high risk. New York: Wiley; 2000. [Google Scholar]
- Saxbe DE, Repetti RL, Graesch AP. Time spent in housework and leisure: Links with parents' physiological recovery from work. Journal of Family Psychology. 2011;25:271–281. doi: 10.1037/a0023048. [DOI] [PubMed] [Google Scholar]
- Saxbe DE, Repetti RL, Nishina A. Marital satisfaction, recovery from work, and diurnal cortisol among men and women. Health Psychology. 2008;27:15–25. doi: 10.1037/0278-6133.27.1.15. [DOI] [PubMed] [Google Scholar]
- Scholtz W, Hellhammer J, Schulz P, Stone AA. Perceived work overload and chronic worrying predict weekend-weekday differences in the cortisol awakening response. Psychosom. Med. 2004;66:207–214. doi: 10.1097/01.psy.0000116715.78238.56. [DOI] [PubMed] [Google Scholar]
- Seltzer MM, Almeida DM, Greenberg JS, Savla J, Stawski RS, Hong J, Taylor JL. Psychosocial and biological markers of daily lives of midlife parents of children with disabilities. Journal of Health and Social Behavior. 2009;50:1–15. doi: 10.1177/002214650905000101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seltzer MM, Greenberg JS, Hong J, Smith LE, Almeida DM, Coe C, Stawski RS. Maternal cortisol levels and behavior problems in adolescents and adults with ASD. Journal of Autism and Developmental Disorders. 2010;40:457–469. doi: 10.1007/s10803-009-0887-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slatcher RB, Robles TF, Repetti RL, Fellows MD. Momentary work worries, marital disclosure, and salivary cortisol among parents of young children. Psychosomatic Medicine. 2010;72:887–896. doi: 10.1097/PSY.0b013e3181f60fcc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stafford F. Chore wars: Men, women, and housework [Press Release] 2008 Retrieved from http://www.nsf.gov/discoveries/disc_summ.jsp?cntn_id=111458.
- Steptoe A, Cropley M, Griffith J, Kirschbaum C. Job strain and anger expression predict early morning elevations in salivary cortisol. Psychosomatic Medicine. 2000;62:286–292. doi: 10.1097/00006842-200003000-00022. Retrieved from http://www.psychosomaticmedicine.org. [DOI] [PubMed] [Google Scholar]
- Susman EJ. Psychobiology of persistent antisocial behavior: Stress, early vulnerabilities and the attenuation hypothesis. Neuroscience & Biobehavioral Reviews. 2006;30(3):376–389. doi: 10.1016/j.neubiorev.2005.08.002. [DOI] [PubMed] [Google Scholar]
- Taylor SE, Klein LC, Lewis BP, Gruenewald TL, Gurung RAR, Updegraff JA. Biobehavioral responses to stress in females: Tend-and-befriend, not fight-or-flight. Psychological Review. 2000;107:411–429. doi: 10.1037/0033-295x.107.3.411. [DOI] [PubMed] [Google Scholar]
- Theorell T, Karasek RA. Current issues relating to psychosocial job strain and cardiovascular disease research. Journal of Occupational Health Psychology. 1996;1:9–26. doi: 10.1037//1076-8998.1.1.9. [DOI] [PubMed] [Google Scholar]
- Tubbs CY, Roy KM, Burton LM. Family ties: Constructing family time in low-income families. Family Process. 2005;44(1):77–91. doi: 10.1111/j.1545-5300.2005.00043.x. [DOI] [PubMed] [Google Scholar]
- Wahbeh H, Kishiyama SS, Zajdel D, Oken BS. Salivary cortisol awakening response in mild Alzheimer disease, caregivers, and noncaregivers. Alzheimer Disease & Associated Disorders. 2008;22:181–183. doi: 10.1097/WAD.0b013e31815a9dff. [DOI] [PubMed] [Google Scholar]
- Walker LO, Best MA. Well being of mothers with infant children: A preliminary comparison of employed women and homemakers. Women & Health. 1991;17:71–89. doi: 10.1300/J013v17n01_05. [DOI] [PubMed] [Google Scholar]
- Wilhelm I, Born J, Kudielka BM, Schlotz W, Wüst S. Is the cortisol awakening rise a response to awakening? Psychoneuroendocrinology. 2007;32:358–366. doi: 10.1016/j.psyneuen.2007.01.008. [DOI] [PubMed] [Google Scholar]
- Wüst S, Federenko I, Hellhammer DH, Kirschbaum C. Genetic factors, perceived chronic stress, and the free cortisol response to awakening. Psychoneuroendocrinology. 2000;25:707–720. doi: 10.1016/s0306-4530(00)00021-4. [DOI] [PubMed] [Google Scholar]