Abstract
Objective
To determine continuing medical education (CME) course participants' use of social media (SM) and their attitudes about the value of SM for enhancing CME education and to examine associations between participants' characteristics and attitudes toward SM.
Participants and Methods
We conducted a cross-sectional survey and validation study of 539 participants at a Mayo Clinic Internal Medicine CME course in November 2011. The Social Media Use and Perception Instrument (SMUPI) consisted of 10 items (5-point Likert scales) and categorical response options. The main outcome measures were psychometric characteristics of the SMUPI scale, course participants' use of SM, and their attitudes regarding the importance of SM for enhancing CME.
Results
Of 539 CME course participants, 327 (61%) responded to the SMUPI survey. Most respondents (291 [89%]) reported using SM, with the most common types being YouTube (189 of the 327 participants [58%]) and Facebook (163 of 327 [50%]). Factor analysis revealed a 2-dimensional assessment of course participants' attitudes. Internal consistency reliability (Cronbach α) was excellent for factor 1 (0.94), factor 2 (0.89), and overall (0.94). The CME course participants' favorable attitudes toward SM were associated with younger age (20-29 years, mean score 3.13; 30-39 years, 3.40; 40-49 years, 3.39; 50-59 years, 3.18; 60-69 years, 2.93; and ≥70 years, 2.92; P=.02), using SM frequently (never, mean score 2.49; less than once monthly, 2.75; once monthly, 3.21; weekly, 3.31; and daily, 3.81; P<.0001), and professional degree (PhD, mean score 3.00; MD, 3.05; DO, 3.35; PA, 3.42; and NP, 3.50; P=.01).
Conclusion
We describe the first validated measure of CME course participants' use of and attitudes toward SM. Our results suggest that CME course directors should guide SM strategies toward more youthful, technology-savvy CME participants and that SM will become increasingly worthwhile in CME as younger learners continue to enter the profession.
Abbreviations and Acronyms: CME, continuing medical education; SM, social media; SMUPI, Social Media Use and Perception Instrument
Social media (SM) (eg, Facebook, Twitter, and YouTube) consists of Internet- and mobile device–based technologies that enhance interactivity among individuals and organizations. The strengths of SM include wide accessibility and personalized user profiles that allow the targeting of specific audiences for entertainment, marketing, and education. Facebook has more than 500 million users, 50% of whom access their accounts daily. Although SM is considered a phenomenon of the millennial generation (also called Generation Y [those born between approximately 1980 and 2000), more than 30% of Facebookers are over age 35, and users older than 50 years are the fastest growing cohort.1 Remarkably, nearly 70% of all Internet users have Facebook accounts, and during 20 minutes of Facebook use globally, more than 1 million links are shared and nearly 3 million messages are sent. Similar statistics exist for YouTube; as of 2011, there were approximately 500 million unique visitors and 3 billion hours spent on YouTube per month among all users combined.2 Social media websites can reach large populations and have been widely used for business-related purposes. Recent marketing research by the University of Massachusetts Dartmouth found that corporate and academic utilization of SM is substantial, with 20% of Fortune 500 companies, 45% of Inc. 500 companies, 50% of US colleges and universities, and 100% of the top US charities using SM.3-5
Social media has the potential to enhance continuing medical education (CME). Web-based learning in medical education has already been established and validated during recent years, although the advantage of Web-based learning over conventional teaching methods remains unclear.6-8 The popularity of SM among medical learners and faculty physicians has generated studies about the implications regarding professionalism associated with this new technology.9-14 A recent report by the Robert Wood Johnson Foundation highlighted potential professionalism issues regarding the use of SM among health care professionals, including breaches of the patient-physician relationship and patient confidentiality.15 This concern for professionalism has led the American Medical Association and numerous US medical schools to publish guidelines on the appropriate use of SM by health care professionals.9,16 However, while the use of SM in medicine is widespread, its utility for enhancing learning remains poorly understood.
An estimated 45% to 90% of medical students, residents, and fellows use SM.10,11,17,18 Recent surveys revealed that 67% of practicing physicians use Facebook19 and 48% use Twitter.20 Although many studies have described students' attitudes about the professional use of SM in medicine,17,18,21,22 few have examined physicians' attitudes on the use of SM for academic purposes. For instance, a recent survey of medical students and practicing physicians demonstrated a high awareness of existing SM tools for medical education but showed a lack of knowledge regarding the use of these technologies for learning.23
The potential application of SM to CME has been recognized.24,25 However, we are unaware of published research on the use of SM to deliver CME knowledge content to practicing physicians or studies on physicians' attitudes regarding the use of SM to market CME activities. Our objective was to conduct a cross-sectional survey of US physicians attending a Mayo Clinic Internal Medicine CME course to determine their use of SM and evaluate their attitudes regarding the value of SM for enhancing CME.
Participants and Methods
Study Design and Participants
We conducted a cross-sectional survey and validation study that included all 539 participants at the Mayo Clinic 2011 Clinical Reviews course. Clinical Reviews is an annual week-long course accredited by the Mayo School of Continuous Professional Development that provides 22.5 hours of CME credit. The format consists of 20- to 30-minute podium presentations. Presenters are encouraged to use clinical cases and the audience response system whenever possible. Faculty members from the Mayo Clinic College of Medicine are selected by the course directors to give one or two presentations. Participants at Clinical Reviews typically represent health care professionals from the midwestern United States. All course participants were asked to voluntarily complete the Social Media Use and Perception Instrument (SMUPI) during a break between speaker sessions. A water bottle with a Mayo Clinic logo was offered on survey completion. This study was deemed exempt by the Mayo Clinic Institutional Review Board.
Survey Instrument Development
The SMUPI was designed to determine CME participants' general knowledge and use of SM and to evaluate their attitudes regarding the value of SM for enhancing CME use and marketing. Content for this instrument was derived from the existing literature,10,11,17,18,20-22,26-28 discussions with 3 college-age students of the millennial generation and an SM consultant, and input from Mayo physicians with experience in scale design, validation,29-36 and CME assessment. The initial iteration generated 19 items, 9 of which were initially chosen and further refined. Further iterations included a 10th item, “Social media will be increasingly utilized for CME in the future.” The final version was agreed on by 4 of the authors (A.T.W., N.P.S., C.M.W., and T.J.B.) and consisted of 10 items structured on 5-point scales (1 = strongly disagree, 2 = disagree, 3 = neutral, 4 = agree, and 5 = strongly agree) along with categorical response options for demographic variables (individual Likert scale items in Table 1).
TABLE 1.
SMUPI Mean Scores, Factor Loadings, and Internal Consistency Reliabilitya
| Item loading |
||||
|---|---|---|---|---|
| Item | Mean score (SD) | Factor 1b | Factor 2c | Cronbach αd |
| Factor 1: Value of SM to course participants | 0.94 | |||
| 1. I would use SM to gain CME knowledge | 2.96 (1.17) | .684 | .563 | |
| 2. I would use SM to enhance my medical education | 3.10 (1.15) | .699 | .526 | |
| 3. SM would be useful for learning about CME courses | 3.15 (1.09) | .675 | .459 | |
| 4. I would be interested in SM for information about CME opportunities | 3.26 (1.23) | .877 | .297 | |
| 5. I would like to have CME courses advertised to me by SM | 3.01 (1.22) | .813 | .314 | |
| Factor 2: Value of SM to CME course directors | 0.89 | |||
| 6. CME courses should use SM to enhance learning | 3.12 (0.96) | .518 | .607 | |
| 7. SM is a professional way to assess CME content | 3.02 (0.99) | .401 | .747 | |
| 8. SM is an ethical way to engage CME participants | 3.28 (0.90) | .256 | .765 | |
| 9. SM is an appropriate resource for CME | 3.21 (0.96) | .344 | .794 | |
| Overall (all 9 items) | 0.94 | |||
| 10. SM will be increasingly utilized for CME in the futuree | 3.74 (0.94) | . . . | . . . | |
CME = continuing medical education; SM = social media; SMUPI = Social Media Use and Perception Instrument.
Factor 1 contains 5 items (1-5) representing the value of SM to CME course participants.
Factor 2 contains 4 items (6-9) representing the value of SM to CME course directors.
Cronbach α reflects internal consistency reliability of items comprising each factor and overall (ie, all items combined).
This item was eliminated from the statistical analyses because of ambiguous item loading.
Statistical Analyses
Factor analysis was performed on scores from the 10 Likert-scaled survey items. Factors were extracted using the minimal proportion criteria. Items with factor loadings of 0.60 or more were retained.37 Interrater reliability for individual items was calculated using intraclass correlation coefficients with 95% CIs. Intraclass correlations were interpreted as follows: coefficients less than 0.4, poor; 0.4 to 0.75, fair to good; and greater than 0.75, excellent.38 Internal consistency reliability for items comprising each factor and overall were calculated using Cronbach coefficient α, in which α>0.7 is considered acceptable.37
The SMUPI scores were reported as means and SDs for the 10 instrument items. Participant characteristics, which were treated as categorical variables, were the following: age (20-29, 30-39, 40-49, 50-59, 60-69, and ≥70 years), sex, geographic region (western, northeastern, midwestern, and southern United States and Canada), practice type (academic, private-urban, private-rural, and resident or fellow in training), degree (MD/MBBS, DO, NP, PA, PharmD, and PhD), medical specialty (internal medicine, internal medicine subspecialty, family medicine, surgery, emergency medicine, and pediatrics), types of SM use (categories listed in Table 1), frequency of SM use (never, less than once a month, monthly, weekly, and daily), purpose of SM use (personal, CME, general education, and professional), and means of learning about the CME courses (SM, mail brochure, e-mail brochure, journal/newspaper ad, another Mayo CME course, word of mouth, previous attendance, Internet search, and other). Associations between SMUPI scores and CME participant–related variables were determined using the Kruskal-Wallis test. Statistical significance was set at P<.05. Statistical analyses were conducted using SAS version 9.2 (SAS Institute Inc).
Results
Factor analysis revealed a 2-dimensional assessment of CME course participants' attitudes, with factor 1 representing the value of SM to course participants (items 1-5) and factor 2 representing the value of SM to CME course directors (items 6-9). One item was eliminated due to an ambiguous item loading. Overall, the extracted factors accounted for 100% of the shared variance among the original variables. Internal consistency reliability (Cronbach α) was excellent for factor 1 (0.94), factor 2 (0.89), and overall (0.94). Regarding survey responses, participants expressed the most agreement with items stating that SM would be useful for disseminating information about CME opportunities, that the use of SM in CME is ethical, and that SM will be increasingly utilized for CME in the future (Table 1).
The survey was completed by 327 of the 539 CME participants, yielding a response rate of 61% (some respondents did not answer all questions, however). The majority of the participants were male (193 of 321 [60%]) and older than 50 years (215 of 323 [67%]). Most participants were from the midwestern United States (307 of 321 [96%]), but participants also represented the western, northwestern, and southern United States and Canada. Of the 308 respondents who specified practice type, 149 (48%) were in private-rural practice, 88 (29%) were in private-urban practice, 65 (21%) were in academics, and 6 (2%) were residents/fellows in training (Table 2).
TABLE 2.
Associations Between SMUPI Scores and CME Participant Characteristicsa
| Participant characteristicb | No. (%) of respondents | Mean (SD) assessment score | P valuec |
|---|---|---|---|
| Age (y) (n=323) | .02 | ||
| 20-29 | 10 (3.10) | 3.13 (0.94) | |
| 30-39 | 45 (13.93) | 3.40 (0.73) | |
| 40-49 | 53 (16.41) | 3.39 (0.95) | |
| 50-59 | 112 (34.67) | 3.18 (0.86) | |
| 60-69 | 78 (24.15) | 2.93 (0.99) | |
| ≥70 | 25 (7.74) | 2.92 (0.73) | |
| Sex (n=321) | .10 | ||
| Male | 193 (60.12) | 3.11 (0.89) | |
| Female | 128 (39.88) | 3.26 (0.89) | |
| Geographic region (n=321) | .39 | ||
| Western US | 3 (0.93) | 2.96 (1.17) | |
| Northeastern US | 2 (0.62) | 3.44 (0) | |
| Midwestern US | 307 (95.64) | 3.18 (0.88) | |
| Southern US | 2 (0.62) | 1.89 (0.94) | |
| Canada | 7 (2.18) | 3.32 (1.29) | |
| Type of practice (n=308) | .34 | ||
| Academic | 65 (21.10) | 3.27 (0.89) | |
| Private-urban | 88 (28.57) | 3.20 (0.99) | |
| Private-rural | 149 (48.38) | 3.09 (0.84) | |
| Resident/fellow | 6 (1.95) | 3.30 (1.38) | |
| Degree (n=324) | .01 | ||
| MD/MBBS | 230 (70.99) | 3.05 (0.90) | |
| DO | 21 (6.48) | 3.35 (0.91) | |
| NP | 44 (13.58) | 3.50 (0.80) | |
| PA | 28 (8.64) | 3.42 (0.83) | |
| PharmD | 0 (0) | NA | |
| PhD | 1 (0.31) | 3.00 (NA) | |
| Medical specialty (n=321) | .26 | ||
| Internal medicine | 34 (10.59) | 2.94 (1.03) | |
| IM subspecialty | 17 (5.30) | 3.31 (1.13) | |
| Family medicine | 241 (75.08) | 3.19 (0.87) | |
| Surgical specialty | 17 (5.30) | 3.46 (1.02) | |
| Anesthesia | 7 (2.18) | 2.90 (0.53) | |
| Emergency medicine | 4 (1.25) | 2.81 (0.19) | |
| Pediatrics | 1 (0.31) | 2.67 (NA) | |
| Frequency of SM use (n=322) | <.0001 | ||
| Never | 54 (16.77) | 2.49 (0.75) | |
| Less than once monthly | 74 (22.98) | 2.75 (0.78) | |
| Monthly | 36 (11.18) | 3.21 (0.85) | |
| Weekly | 72 (22.36) | 3.31 (0.75) | |
| Daily | 86 (26.71) | 3.81 (0.72) | |
| Purpose of SM use (n=386)d | . . . | ||
| Personal | 251 (65.03) | 3.31 (0.86) | |
| CME | 21 (5.44) | 4.21 (0.73) | |
| General education | 64 (16.58) | 3.78 (0.67) | |
| Professional | 50 (12.95) | 3.97 (0.71) |
CME = continuing medical education; IM = internal medicine; NA = not applicable; SM = social media; SMUPI = Social Media Use and Perception Instrument; US = United States.
The total number of study participants for each of the variables including age, sex, geographic region, type of practice, degree, medical specialty, and frequency of SM use do not equal the total number of study participants (327) because not all participants responded to all of the questions for each of these variables.
Associations between overall SMUPI scores and participant-related variables were determined using the Kruskal-Wallis test. P values are not provided for “Purpose of SM use” because data for this category were not mutually exclusive.
The total number of study participants for “Purpose of SM use” is greater than the number of study participants (327) because the participants could select more than one category of SM use. Percentages are based on the total number of responses (386).
Nearly all participants reported having used at least one type of SM (291 of 327 [89%]), and very few (54 of 322 [17%]) reported never using SM. Most of the 327 participants utilized SM for personal use (251 [77%]); others used SM for general education (64 [20%[), CME purposes (21 [6%]), and other professional use (50 [15%]) (Table 2).
Among the 327 participants who responded to the survey, the most common SM tools were YouTube (189 [58%]), Facebook (163 [50%]), and Skype (142 [43%]) (Figure). The types of SM that were rarely or never used were Doximity (5 [2%]), Sermo (4 [1%]), and Second Life (4 [1%]). The following types of SM were used less than 1% of the time: fring, SlideShare, foursquare, Digg, Friendster, reddit, and tumblr.
FIGURE.
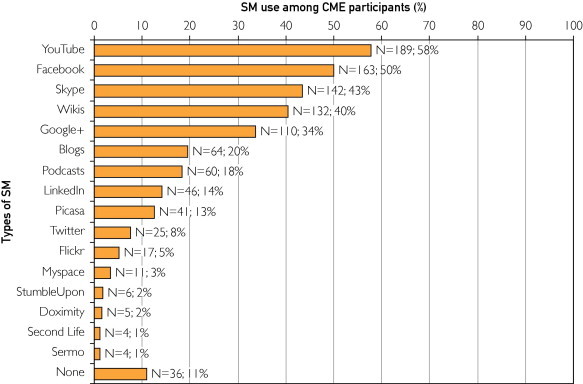
Types of social media (SM) used by 327 CME course participants. The percentages do not total 100% because participants could select more than one type of SM. CME = continuing medical education.
The CME course participants' favorable attitudes toward SM were associated with characteristics of younger age (20-29 years, mean score of 3.13; 30-39 years, 3.40; 40-49 years, 3.39; 50-59 years, 3.18; 60-69 years, 2.93; and ≥70 years, 2.92; P=.02), using SM frequently (never, mean score of 2.49; less than once monthly, 2.75; once monthly, 3.21; weekly, 3.31; and daily, 3.81; P<.0001), and professional degree (PhD, mean score of 3.00; MD, 3.05; DO, 3.35; PA, 3.42; and NP, 3.50; P=.01). There were no significant associations between participants' attitudes toward SM and participant sex, geographic region, type of practice, or medical specialty (Table 2).
Discussion
We describe the first validated measure of CME participants' attitudes regarding personal use of SM and the value of SM for CME. The vast majority of CME participants utilized SM for personal reasons and/or education. The most common types of SM used by CME participants were YouTube, Facebook, and Skype. Participants' favorable attitudes toward SM utilization for CME were associated with younger age and frequency of SM use. These findings have important implications for CME course directors and future research on using SM to enhance CME.
The CME course participants in this study reported using SM frequently. Notably, SM use represents a high behavior-level outcome, which is not commonly reported in education research.39 Additionally, CME course participants expressed some agreement that use of SM for CME is ethical, desirable for distributing CME content, and likely to increase over time; however, course participants older than age 50 were less likely to view SM as a professional medium of communication. A recent pilot study revealed that only 24% of CME professionals had a formal strategic plan for incorporating SM into their CME courses and that 67% had no plans to incorporate SM in the future.40 Given the overall popularity of SM use among CME participants and the significantly negative association between SMUPI scores and participant age, it appears that CME course directors should consider adopting a strategy of targeting CME marketing and educational content to CME participants, especially younger ones, through the use of SM.
Our findings regarding type and frequency of SM use are similar to those of other studies among health care professionals including nurses, pharmacists, medical students, residents, fellows, and practicing physicians.10-12,17-20,41-43 As in previous studies,23,43 we found that CME participants use SM for personal, more than for professional or educational, purposes. Nonetheless, the desirability of SM for educational use has been recognized.23,41 Potential barriers to using SM for education include inadequate knowledge about how to access electronic information, lack of educational content in SM compared with other forms of media, poor quality control, and limited time to access SM for learning.23
Our results suggest that clinicians with DO, NP, or PA degrees view SM more favorably than do those with MD or PhD degrees. Several studies indicated that nurses and physician assistants may be more likely than physicians to use SM for professional reasons. According to recent surveys, 65% of nurses reported using SM in their professions,41 whereas 60% of physicians were interested in using SM at work.44 Another survey revealed that only 3% of physicians and 10% of physicians in training used SM for professional reasons.45 An additional investigation showed that 21% of physicians used SM, compared with 36% of physician assistants.46 Alternatively, the varying opinions toward SM among CME participants with different professional degrees in our study might have been due to participant age; the average age of DOs, NPs, and PAs was 31 years and that of MDs was 40 years, whereas the single PhD was in the sixth decade of life.
Many experts have examined SM regarding what constitutes professional use and the prevalence of unprofessional behavior.12,17,18,21,22,27 Related to this issue, health care professionals have been wary of SM because of concerns about maintaining patient confidentiality and anecdotes of physicians and nurses who have been terminated for inappropriate Facebook posts.47,48 Therefore, health care organizations, medical schools, and professional societies such as the American Medical Association have issued guidelines on the appropriate use of SM, including suggestions for separating personal and professional content online.16 Similarly, the Alliance for Continuing Medical Education has provided standards for the appropriate use of SM.49 Our experiences as CME course directors have revealed that incorporating SM into large-scale CME offerings can be accomplished without difficulty and at exceedingly low risk. Indeed, we have yet to experience any incidents in which SM has compromised the integrity of our CME courses, presenters, or participants.
Although we are unaware of any research describing the use of SM for marketing in CME, it is noteworthy that industry studies have revealed that more than 90% of marketers utilize SM to sell their products.50,51 Based on industry standards and the current study findings, it would seem advantageous for CME course directors to take full advantage of SM for the promotion of their courses.
Our method for measuring CME participants' attitudes about SM is supported by validity evidence, which includes the categories of content, internal structure, response process, criteria, and consequences.31,52 In this study, content evidence was supported by survey items from previous literature on SM and CME and input by experts in education. Internal structure evidence was supported by factor analysis that showed a 2-dimensional assessment of CME participants' attitudes regarding the use of SM in CME and excellent reliability. Criterion evidence was supported by associations between attitude scores and other variables including CME participants' ages and frequencies of SM use. Notably, previous literature reviews revealed that content, internal structure, and relationships to other variables are the most commonly reported validity evidence categories in medical education studies.30
Our study has some limitations. The majority of the respondents resided in the Midwest, and there was only limited representation from other regions of the United States and Canada. Most of the participants were family and internal medicine physicians, with only a minority of the participants practicing in surgical specialties or internal medicine subspecialties. Although findings from this study should be generalized to other settings with caution, we found no compelling evidence that the results would have been strongly influenced by variations in geographic or practice distributions. Furthermore, the demographic characteristics of our study sample, including CME participant practice type, medical specialty, and educational degree, are similar to those reported in large systematic reviews of CME.53-55 Our collection of demographic variables could have been more robust to include questions regarding issues such as socioeconomic status and broadband access availability, but as noted previously, the demographic profile of our sample appears to be similar to that of participants in other published CME studies. Lastly, we acknowledge that survey nonresponders may have had different attitudes than responders regarding SM. However, the response rate in this study was favorable compared with that typically seen in physician surveys.56,57
Conclusion
To our knowledge, this study represents the first validated measure of CME participants' attitudes regarding personal use of SM and the value of SM for attaining CME. Our findings indicate that the most fruitful categories of SM for CME use and marketing may be Facebook, YouTube, and Skype. The identified association between positive attitudes on using SM in CME with younger age and increased frequency of SM use suggests that CME course directors might want to direct SM learning strategies toward more youthful, technology-savvy CME physicians and that the utilization of SM in CME will become increasingly worthwhile as junior physicians enter the profession. More research on developing methods, including SM interventions, for enhancing CME is needed.
Footnotes
Financial Support: Drs Wang and Sandhu received a Continuing Medical Education Research Award from the Mayo Clinic Department of Internal Medicine.
Supplemental Online Material
Author Interview Video
References
- 1.Facebook statistics, stats & facts for 2011. http://www.digitalbuzzblog.com/facebook-statistics-stats-facts-2011/ Digital Buzz Blog website. Published January 18, 2011. Accessed July 6, 2012.
- 2.Elliott A.-M. 10 Fascinating YouTube facts that may surprise you. http://mashable.com/2011/02/19/youtube-facts/ Mashable Social Media website. Published February 19, 2011. Accessed July 6, 2012.
- 3.The 2010 Inc. 500 Update: Most blog, friend and tweet but some industries still shun social media. http://www.umassd.edu/cmr/studiesandresearch/industriesstillshunsocialmedia/ UMass Dartmouth website. Accessed July 6, 2012.
- 4.Social media usage now ubiquitous among US top charities, ahead of all other sectors. http://www.umassd.edu/cmr/studiesandresearch/socialmediatopcharities/ UMass Dartmouth website. Accessed July 6, 2012.
- 5.Social media and college admissions: higher-ed beats business in adoption of new tools for third year. http://www.umassd.edu/media/umassdartmouth/cmr/studiesandresearch/socialmediaadmissions.pdf UMass Dartmouth website. Accessed July 6, 2012.
- 6.Cook D.A., Garside S., Levinson A.J., Dupras D.M., Montori V.M. What do we mean by web-based learning?: A systematic review of the variability of interventions. Med Educ. 2010;44(8):765–774. doi: 10.1111/j.1365-2923.2010.03723.x. [DOI] [PubMed] [Google Scholar]
- 7.Cook D.A., Dupras D.M., Thompson W.G., Pankratz V.S. Web-based learning in residents' continuity clinics: a randomized, controlled trial. Acad Med. 2005;80(1):90–97. doi: 10.1097/00001888-200501000-00022. [DOI] [PubMed] [Google Scholar]
- 8.Cook D.A., Levinson A.J., Garside S., Dupras D.M., Erwin P.J., Montori V.M. Internet-based learning in the health professions: a meta-analysis. JAMA. 2008;300(10):1181–1196. doi: 10.1001/jama.300.10.1181. [DOI] [PubMed] [Google Scholar]
- 9.Kind T., Genrich G., Sodhi A., Chretien K.C. Social media policies in place in US medical schools. Med Educ Online. 2010;15:5324. doi: 10.3402/meo.v15i0.5324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thompson L.A., Dawson K., Ferdig R. The intersection of online social networking with medical professionalism. J Gen Intern Med. 2008;23(7):954–957. doi: 10.1007/s11606-008-0538-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sandars J, Homer M, Pell G, Crocker T. Web 2.0 and social software: the medical student way of e-learning [published online ahead of print June 18, 2010]. Med Teach. [DOI] [PubMed]
- 12.Chretien K.C., Farnan J.M., Greysen S.R., Kind T. To friend or not to friend?: Social networking and faculty perceptions of online professionalism. Acad Med. 2011;86(12):1545–1550. doi: 10.1097/ACM.0b013e3182356128. [DOI] [PubMed] [Google Scholar]
- 13.Chretien K. Should I be “friends” with my patients on social networking web sites? Am Fam Physician. 2011;84(1):105. 108. [PubMed] [Google Scholar]
- 14.Chretien K.C., Greysen S.R., Chretien J.P., Kind T. Online posting of unprofessional content by medical students. JAMA. 2009;302(12):1309–1315. doi: 10.1001/jama.2009.1387. [DOI] [PubMed] [Google Scholar]
- 15.Are social media threatening medical professionalism? http://www.rwjf.org/humancapital/product.jsp?id=71546 Robert Wood Johnson Foundation website. Published December 6, 2010. Accessed July 6, 2012.
- 16.New AMA policy helps guide physicians' use of social media. http://www.ama-assn.org/ama/pub/news/news/social-media-policy.page AMA website. Published November 8, 2010. Accessed July 6, 2012.
- 17.Garner J., O'Sullivan H. Facebook and the professional behaviours of undergraduate medical students. Clin Teach. 2010;7(2):112–115. doi: 10.1111/j.1743-498X.2010.00356.x. [DOI] [PubMed] [Google Scholar]
- 18.Moubarak G., Guiot A., Benhamou Y., Benhamou A., Hariri S. Facebook activity of residents and fellows and its impact on the doctor-patient relationship. J Med Ethics. 2011;37(2):101–104. doi: 10.1136/jme.2010.036293. [DOI] [PubMed] [Google Scholar]
- 19.Physicians on Facebook. http://www.mdsearch.com/physician-careers/physicians-on-facebook MDSearch.com website. Accessed July 6, 2012.
- 20.Chretien K.C., Azar J., Kind T. Physicians on Twitter. JAMA. 2011;305(6):566–568. doi: 10.1001/jama.2011.68. [DOI] [PubMed] [Google Scholar]
- 21.Lee K.L., Ho M.J. Online social networking versus medical professionalism. Med Educ. 2011;45(5):523. doi: 10.1111/j.1365-2923.2011.03978.x. [DOI] [PubMed] [Google Scholar]
- 22.Cain J., Scott D.R., Akers P. Pharmacy students' Facebook activity and opinions regarding accountability and e-professionalism. Am J Pharm Educ. 2009;73(6):104. doi: 10.5688/aj7306104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sandars J., Schroter S. Web 2.0 technologies for undergraduate and postgraduate medical education: an online survey. Postgrad Med J. 2007;83(986):759–762. doi: 10.1136/pgmj.2007.063123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sullivan T. Continuing medical education embracing social media? http://www.policymed.com/2010/09/continuing-medical-education-embracing-social-media.html Policy and Medicine website. Published September 24, 2010. Accessed July 6, 2012.
- 25.Aase L. Opening keynote: Social Media Summit. http://socialmedia.mayoclinic.org/tag/lee-aase/ Mayo Clinic Center for Social Media website. Published October 18, 2011. Accessed July 6, 2012.
- 26.MacDonald J., Sohn S., Ellis P. Privacy, professionalism and Facebook: a dilemma for young doctors. Med Educ. 2010;44(8):805–813. doi: 10.1111/j.1365-2923.2010.03720.x. [DOI] [PubMed] [Google Scholar]
- 27.Metzger A.H., Finley K.N., Ulbrich T.R., McAuley J.W. Pharmacy faculty members' perspectives on the student/faculty relationship in online social networks. Am J Pharm Educ. 2010;74(10):188. doi: 10.5688/aj7410188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Peluchette J., Karl K. Social networking profiles: an examination of student attitudes regarding use and appropriateness of content. Cyberpsychol Behav. 2008;11(1):95–97. doi: 10.1089/cpb.2007.9927. [DOI] [PubMed] [Google Scholar]
- 29.Beckman T.J., Cook D.A. Developing scholarly projects in education: a primer for medical teachers. Med Teach. 2007;29(2-3):210–218. doi: 10.1080/01421590701291469. [DOI] [PubMed] [Google Scholar]
- 30.Beckman T.J., Cook D.A., Mandrekar J.N. What is the validity evidence for assessments of clinical teaching? J Gen Intern Med. 2005;20(12):1159–1164. doi: 10.1111/j.1525-1497.2005.0258.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cook D.A., Beckman T.J. Current concepts in validity and reliability for psychometric instruments: theory and application. Am J Med. 2006;119(2) doi: 10.1016/j.amjmed.2005.10.036. 166.e7-116. [DOI] [PubMed] [Google Scholar]
- 32.Beckman T.J., Mandrekar J.N. The interpersonal, cognitive and efficiency domains of clinical teaching: construct validity of a multi-dimensional scale. Med Educ. 2005;39(12):1221–1229. doi: 10.1111/j.1365-2929.2005.02336.x. [DOI] [PubMed] [Google Scholar]
- 33.Reed D.A., West C.P., Mueller P.S., Ficalora R.D., Engstler G.J., Beckman T.J. Behaviors of highly professional resident physicians. JAMA. 2008;300(11):1326–1333. doi: 10.1001/jama.300.11.1326. [DOI] [PubMed] [Google Scholar]
- 34.Beckman T.J., Ghosh A.K., Cook D.A., Erwin P.J., Mandrekar J.N. How reliable are assessments of clinical teaching?: A review of the published instruments. J Gen Intern Med. 2004;19(9):971–977. doi: 10.1111/j.1525-1497.2004.40066.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Beckman T.J., Lee M.C., Mandrekar J.N. A comparison of clinical teaching evaluations by resident and peer physicians. Med Teach. 2004;26(4):321–325. doi: 10.1080/01421590410001678984. [DOI] [PubMed] [Google Scholar]
- 36.Beckman T.J., Lee M.C., Rohren C.H., Pankratz V.S. Evaluating an instrument for the peer review of inpatient teaching. Med Teach. 2003;25(2):131–135. doi: 10.1080/0142159031000092508. [DOI] [PubMed] [Google Scholar]
- 37.DeVellis R.F. Sage; Newbury Park, CA: 1991. Scale Development : Theory and Applications. [Google Scholar]
- 38.Landis J.R., Koch G.G. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- 39.Reed D.A., Cook D.A., Beckman T.J., Levine R.B., Kern D.E., Wright S.M. Association between funding and quality of published medical education research. JAMA. 2007;298(9):1002–1009. doi: 10.1001/jama.298.9.1002. [DOI] [PubMed] [Google Scholar]
- 40.Lundberg J. Social media in continuing medical education: a pilot survey of CME professionals. Presented at: 2010 Alliance for CME Annual Meeting: MECCA Section. New Orleans, LA; January 27, 2010.
- 41.New study highlights social media use among nurses; comprehensive report also sheds light on social media behaviors of physicians. http://www.prweb.com/releases/Nicholson_Kovac/Healthcare_Study/prweb3646144.htm PRWeb website. Published February 24, 2010. Updated October 5, 2012. Accessed July 6, 2012.
- 42.Most health workers use social media for professional purposes. http://www.ihealthbeat.org/articles/2011/9/12/most-health-workers-use-social-media-for-professional-purposes.aspx iHealthBeat website. Published September 12, 2011. Accessed July 6, 2012.
- 43.Alkhateeb F.M., Clauson K.A., Latif D.A. Pharmacist use of social media. Int J Pharm Pract. 2011;19(2):140–142. doi: 10.1111/j.2042-7174.2010.00087.x. [DOI] [PubMed] [Google Scholar]
- 44.Keckley P.H., Hoffmann M. Social networks in health care: communication, collaboration and insights. https://www.deloitte.com/view/en_US/us/industries/US-federal-government/center-for-health-solutions/disruptive-innovations/2fbc755f3c1b9210VgnVCM100000ba42f00aRCRD.htm Deloitte website. Updated August 27, 2012. Accessed July 6, 2012.
- 45.Bosslet G.T., Torke A.M., Hickman S.E., Terry C.L., Helft P.R. The patient-doctor relationship and online social networks: results of a national survey. J Gen Intern Med. 2011;26(10):1168–1174. doi: 10.1007/s11606-011-1761-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.District of Columbia Board of Medicine Physician & Physician Assistant Workforce Capacity Report: A Summary of Findings From the Physician and Physician Assistant 2010 Workforce Survey in the District of Columbia, 9/2011. http://www.hwic.org/experts/details.php?id=1724 HWIC website. Published September 30, 2011. Updated July 19, 2012. Accessed July 6, 2012.
- 47.Associated Press. April 18, 2011. Doctor busted for patient info spill on Facebook.http://www.msnbc.msn.com/id/42652527/ns/technology_and_science-security/t/doctor-busted-patient-info-spill-facebook/ NBC News website. Accessed July 6, 2012. [Google Scholar]
- 48.Hennessy-Fiske M. When Facebook goes to the hospital, patients may suffer. http://articles.latimes.com/2010/aug/08/local/la-me-facebook-20100809 Los Angeles Times website. Published August 8, 2010. Accessed July 6, 2012.
- 49.Social media guidelines of the Alliance for CME http://www.acehp.org/iMIS15/aCME/PDFs/Social_Media_Guidelines.pdf?hkey=83739c03-3623-4b9d-83f5-bb8cc2ce3c37 Alliance for CME website. Updated January 2011. Accessed July 6, 2012.
- 50.Study finds 90% of marketers use social media for professional purposes. http://www.btobonline.com/article/20101117/FREE/101119922 BtoB website. Published November 17, 2010. Accessed October 9, 2012.
- 51.Stelzner M.A. 2011 Social Media Marketing Industry Report: How Marketers Are Using Social Media to Grow Their Businesses. http://www.socialmediaexaminer.com/SocialMediaMarketingReport2011.pdf Social Media Examiner website. Published April 2011. Accessed July 6, 2012.
- 52.Downing S.M. Validity: on meaningful interpretation of assessment data. Med Educ. 2003;37(9):830–837. doi: 10.1046/j.1365-2923.2003.01594.x. [DOI] [PubMed] [Google Scholar]
- 53.Davis D.A., Thomson M.A., Oxman A.D., Haynes R.B. Changing physician performance: a systematic review of the effect of continuing medical education strategies. JAMA. 1995;274(9):700–705. doi: 10.1001/jama.274.9.700. [DOI] [PubMed] [Google Scholar]
- 54.Davis D.A., O'Brien M.A., Freemantle N., Wolf F.M., Mazmanian P., Taylor-Vaisey A. Impact of formal continuing medical education: do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes? JAMA. 1999;282(9);):867–874. doi: 10.1001/jama.282.9.867. [DOI] [PubMed] [Google Scholar]
- 55.Forsetlund L., Bjørndal A., Rashidian A. Continuing education meetings and workshops: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2009;(2) doi: 10.1002/14651858.CD003030.pub2. CD003030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Asch D.A., Jedrziewski M.K., Christakis N.A. Response rates to mail surveys published in medical journals. J Clin Epidemiol. 1997;50(10):1129–1136. doi: 10.1016/s0895-4356(97)00126-1. [DOI] [PubMed] [Google Scholar]
- 57.Kellerman S.E., Herold J. Physician response to surveys: a review of the literature. Am J Prev Med. 2001;20(1):61–67. doi: 10.1016/s0749-3797(00)00258-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Author Interview Video


