Abstract
Study Objective:
To determine whether adaptations to comply with Accreditation Council for Graduate Medical Education (ACGME) duty hour requirements are associated with changes in total cost and length of stay.
Design:
Retrospective, interrupted time-series cohort study using concurrent control patients.
Setting:
UCSF Benioff Children's Hospital, San Francisco, CA.
Patients:
Inpatients newborn to 18 y on the primary pediatrics medical-surgical unit. Medical patients were studied before and after an intervention, and surgical patients served as a concurrent control group.
Intervention:
Pediatrics trainees' work schedules were changed from those that relied on prolonged call shifts to those primarily based on shorter day shifts and night shifts.
Results:
We detected significant relative reductions in length of stay but not in total cost. When the analysis was limited to the subset of patients who did not receive intensive care unit care, length of stay decreased by 18% and total cost decreased by 10%. We did not detect similar changes in the control group.
Conclusions:
A trainee staffing model that included shorter shifts as consistent with current ACGME duty hour requirements was associated with reduced length of stay and total costs for patients not in the intensive care unit.
Citation:
Rosenbluth G; Fiore DM; Maselli JH; Vitinghoff E; Wilson SD; Auerbach AD. Association between adaptations to ACGME duty hour requirements, length of stay, and costs. SLEEP 2013;36(2):245–248.
Keywords: Cost of hospitalization, duty hour, length of stay, shift work, trainees
BACKGROUND
Accreditation Council for Graduate Medical Education (ACGME)-initiated duty hour reductions are intended to reduce patient harm by ensuring trainees are not overly fatigued and unable to provide optimal care. Several investigators have examined adult patient outcomes in teaching hospitals with duty hour models compliant with 2003 ACGME restrictions.1 Appropriately, much attention has been focused on the reduction in medical errors associated with reduced shift length.2 Modest improvements have been observed in intensive care unit (ICU) utilization, discharge disposition, and pharmacist intervention.3 Additionally, reduced shift length has been associated with an overall decrease in mortality in teaching hospitals with residency programs.4 Beyond clear associations between shift length and medical errors, longer hospitalizations put patients at higher risk of medication errors, which have been reported as high as 157 per 1,000 patient-days.5
New 2011 ACGME duty hour requirements limit intern shifts to fewer than 16 continuous h and other trainees to fewer than 28 h. These changes are the first major revision to 2003 guidelines, which limited trainees to an 80-h workweek and a maximum of 30 continuous h. The primary impetus for reducing shift length has been the compelling data on medical errors.2 However, less is known about how shift-based patient care may affect patient care measures such as length of stay (LOS) and total cost of hospitalization (TC).
A retrospective study6 from the era before duty hour requirements were in effect observed shorter LOS and fewer laboratory tests ordered with shift-based care. More recently, reports have suggested that use of night teams had little or no effect on LOS.3,7
Schedule adaptations have variable effects and can lead to unexpected and unintended outcomes. At least one study8 found a longer LOS after implementing a short call system. Other studies have examined the effects of adaptations to ACGME duty hour on residents' work and sleep h, with variable results. One multicenter study found no change in residents' total work h and sleep h after implementation of the 2003 duty hour requirements,9 and a separate single institution study found that after implementing a night team residents actually reported fewer sleep h.10
We investigated changes in LOS and TC on a pediatric hospitalist service after transitioning to a trainee staffing model that complied with new ACGME standards limiting duty hour by enforcing use of shorter work shifts to provide clinical coverage.
METHODS
Sites and Patients
Our study was carried out at UCSF Benioff Children's Hospital, a 175-bed tertiary care facility. We studied patients newborn to 18 y on the main inpatient medical-surgical unit. Children on the inpatient unit with nonsurgical diseases were cared for primarily on a pediatric hospitalist service (pediatric hospitalists with pediatrics trainees) or a medical subspecialty service (pediatric subspecialists with pediatrics trainees). Patients in the control group were on the pediatric surgery service (pediatric surgery attending with general surgery residents). We included patients who spent time in the ICU, although we also completed additional analyses excluding these patients as noted in the following paragraphs. Neither the medical nor the surgical teams have caps and there is no overflow or other nonteaching service.
Intervention
Our intervention was a change in pediatrics trainees' work schedule from one that relied on prolonged call shifts to one that was primarily day shift- or night shift-based. In the pre-intervention schedule general pediatrics medical patients were covered by pediatrics interns who took call every sixth night (duty hour periods up to 30 h) with cross-coverage (we define cross-coverage as coverage of patients who would be cared for during nonconsecutive shifts, and for whom residents would not participate in attending rounds). Noncall shifts were generally 10 to 11 h. Interns provided cross-coverage of patients on multiple teams at night and on afternoons when the primary interns had continuity clinic. They were supervised by senior residents who took call every 4 to 5 nights. The senior residents also provided similar cross-coverage.
In the postintervention schedule pediatrics trainees worked primarily day shifts and night shifts of 13 h, with some 24-h shifts for supervising residents on the weekends. They covered the same team for 5 to 7 consecutive days (either day shift or night shift), and their team assignment was the same when they switched from the day shift to the night shift. We increased night staffing to eliminate intern-level cross-coverage of multiple teams, and to maintain interns as the primary care providers for medical patients. Senior residents maintained supervisory responsibility for all patients. Attending coverage and pediatric ICU (backup) coverage were unchanged throughout the study period. Only the day team rounded with the attending physician.
During this time period, the pediatric surgery patients continued to be covered by a general surgery resident who took home call, and came in as needed. Additional coverage of these patients was provided by an in-house covering surgery resident.
Data Sources
We gathered data on patient factors including age, sex, diagnosis, LOS, and cost of hospitalization from our electronic medical record as well as administrative and billing databases. We reviewed data during the 12-mo period prior to the schedule change (September 15, 2007-September 15, 2008) and during the 12-mo period after the change (September 16, 2008-September 15, 2009).
We queried the database to identify the most common medical diagnoses on the pediatric medical service based on International Classification of Diseases, Ninth Edition (ICD-9) codes, and reduced this list to the 10 most common medical conditions: pneumonia, asthma, bronchiolitis, dehydration, seizure, aspiration pneumonia, acute upper respiratory infection, intussusception, urinary tract infection, and failure to thrive. All surgery patients were included.
Outcome Measures
Using multivariable gamma models (two-sided) accounting for patient factors (age, diagnosis, severity of illness, time in ICU), we retrospectively compared LOS and TC for patients 1 y before and after the schedule change. TC was not adjusted for inflation or other increases in cost of care. Severity of illness was determined using 3M all patient refined-diagnosis related groups (APR-DRG) grouper software.11 Cost was determined from internal cost accounting systems, not patient charges. We adjusted for clustering at the attending level, as well as patient age, sex, season, and diagnosis. We conducted the same analysis for the surgery patients on the same nursing unit (where there was no change in schedule) as a concurrent control group. Statistical analysis was performed using SAS, version 9.2.
This study was reviewed and approved by the UCSF Committee on Human Research with a waiver of informed consent.
RESULTS
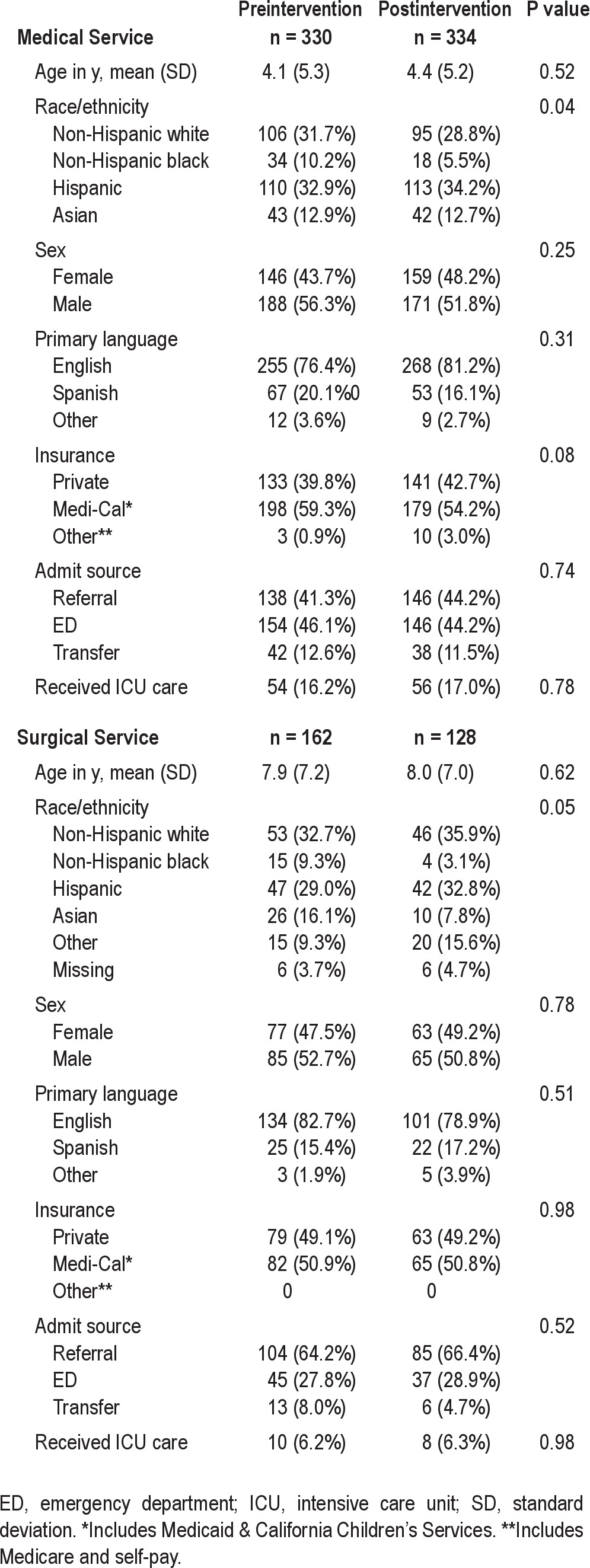
We analyzed data for 334 pediatric medical patients preintervention and 330 post-intervention. Patient characteristics were similar before and after the intervention (Table 1).
Table 1.
Patient demographics
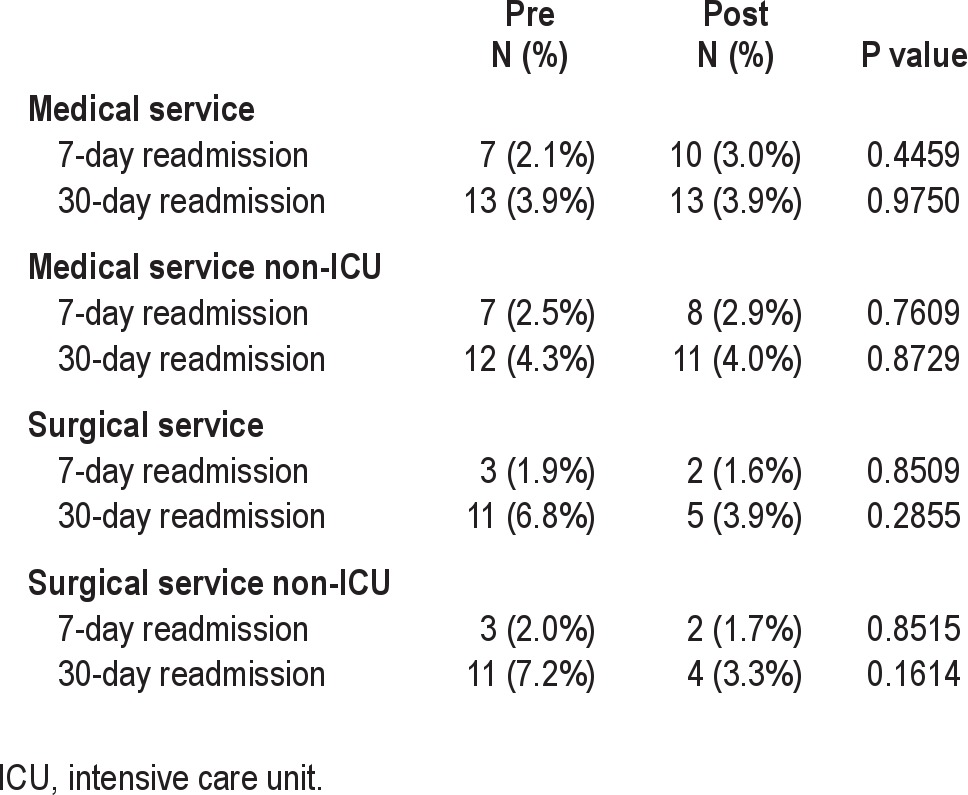
Overall for the medical patients, we saw significant reductions in LOS by 14% (adjusted relative reduction (RR) 0.86, 95% confidence interval (CI) 0.77, 0.96), but no statistically significant change in TC (Table 2). When the analysis was limited to patients who did not receive ICU care both measures were statistically significant. LOS decreased by 18% (adjusted RR 0.82, 95% CI 0.73, 0.93) and TC decreased by 10% (adjusted relative reduction 0.90, 95% CI 0.81, 0.99). The median LOS did not change (Table 2), nor did the 7-day and 30-day readmission rates (Table 3). We did not detect an effect of the schedule change on individual patient diagnosis groups.
Table 2.
Length of stay and total cost of hospitalization for all patient groups
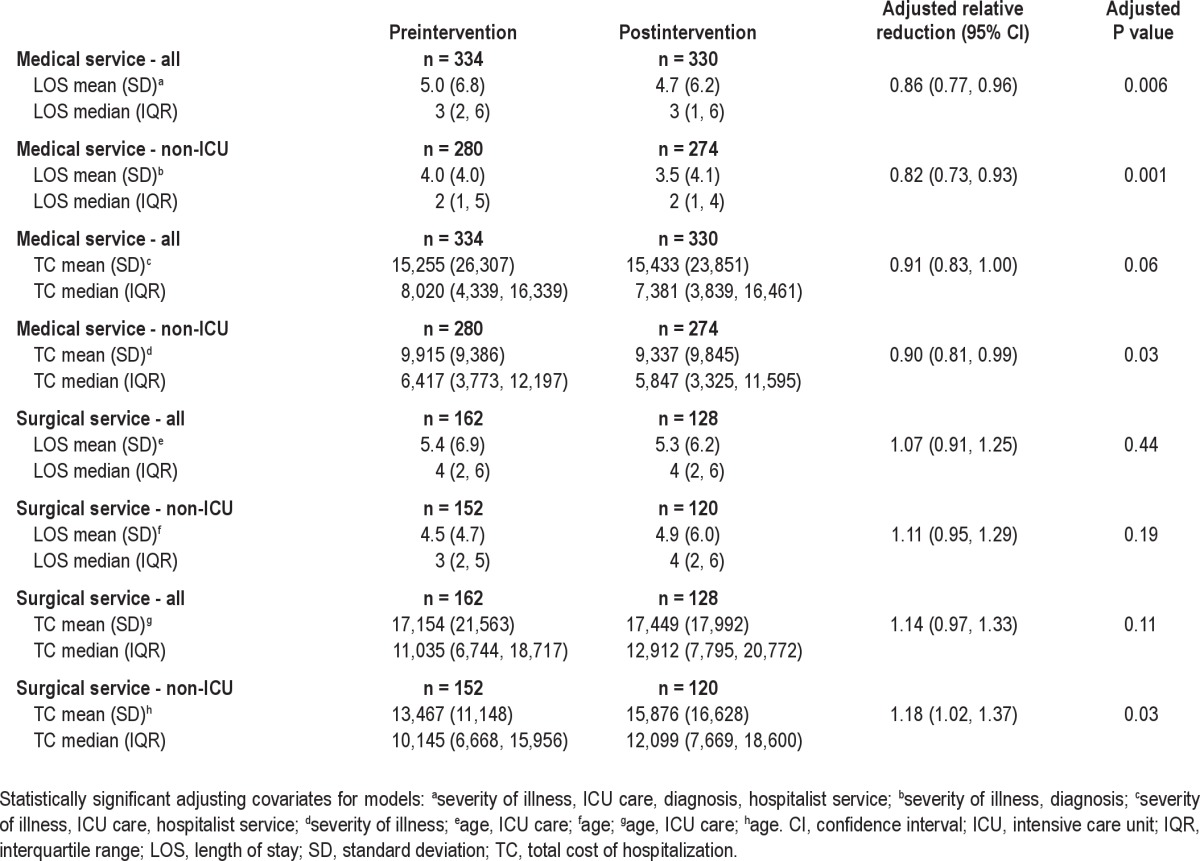
Table 3.
Readmission rates for all patient groups
The most common surgical diagnoses on the inpatient service were appendicitis, Hirschsprung disease, ileostomy creation/repair, and pectus excavatum. There was a great diversity of surgical diagnoses and procedures, which prevented us from identifying additional subsets of patients.
For non-ICU surgical patients (concurrent control group) LOS was no different (adjusted RR 1.11, 95% CI 0.95, 1.29) and TC increased (adjusted RR 1.18, 95% CI 1.02, 1.37) (Table 2). The readmission rates were also unchanged (Table 3).
DISCUSSION
A trainee staffing model with shift lengths that complied with new ACGME duty hour requirements was associated with reduced LOS and TC for non-ICU pediatric patients. This staffing model also created more consistent coverage by the members of the primary team, and eliminated traditional cross-coverage.
No significant change was noted when we included patients who spent time in the pediatric ICU, where no change in the staffing model took place and patients continued to be cared for by residents working a 4-day overnight call rotation.
Few studies have examined the effect of work h or shift changes on LOS. It is possible that our finding of shorter LOS is because residents working sequential night shifts were more likely to show up “ready to work” and therefore more likely to advance care earlier. In addition, the team at night knew some of the team from the previous night (and perhaps from the previous week on day shift) and therefore may have felt greater ownership and/or greater comfort in making clinical decisions. A resident caring for the same patients over several night shifts might be more likely to advance care, such as reducing nebulizer frequency, or advancing oral intake, in ways that speed preparation for discharge. These seemingly minor tasks might be overlooked or even ignored by a resident working a 24- to 32-h shift who was likely to be limited by fatigue and disrupted circadian cycles. These residents might have less motivation to advance care if they knew they were unlikely to care for patients after the shift.
It is also possible that reduced LOS and costs were due to more efficient care by the day teams. The daytime performance of these residents may have been more efficient after the elimination of extended-duration shifts. They also were working slightly longer shifts and so had more time to complete tasks (including facilitating discharges) before leaving for the day. Handoffs were also likely more efficient because the postintervention night teams would have already known many of the patients. In this setting, one could easily imagine the night team asking more directed questions about what would be helpful to facilitate discharge before the following night's shift.
Our findings of decreased LOS have a potential indirect effect in decreasing medical errors. The combined effects of shorter shifts and shorter LOS have the potential to lead to significant reductions in harm. Although shorter LOS has the potential to shift costs to the outpatient setting, this finding has not been conclusively demonstrated in pediatric patients.
Our research has several limitations. It is possible that unmeasured changes on our unit may have been partially responsible for our results. However, other services that cared for patients on our unit had no improvement in LOS or other outcomes. We did not measure or report ICU transfers, or other rarer adverse events, and we cannot comment on whether our new system had an effect on patient safety. Nor does our study comment on physician fatigue or career satisfaction, which would be important measures of our system's acceptability to providers. As an observational study, we are able to report only an association between our schedule change and our studied outcomes, rather than making a causal connection. Finally, as a single-site study at an academic medical center, our results may not apply to other settings.
Increased costs related to compliance with new ACGME standards are estimated by the Institute of Medicine to be as high as $1.7 billion.12 The costs will likely be directed toward additional staffing as many residency programs hire additional trainees and many hospital systems add nocturnists. Although these costs cannot be directly recouped through billing, our findings of reduced LOS and TC suggest that these costs may be partially offset by improved care efficiency.
DISCLOSURE STATEMENT
This was not an industry supported study. There was no off-label or investigational use. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
Work for this study was performed at the University of California San Francisco. Dr. Auerbach was supported by NHLBI grant K24HL098372 during the course of this study.
Footnotes
A commentary on this article appears in this issue on page 165.
REFERENCES
- 1.Levine AC, Adusumilli J, Landrigan CP. Effects of reducing or eliminating resident work shifts over 16 hours: a systematic review. Sleep. 2010;33:1043–53. doi: 10.1093/sleep/33.8.1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Landrigan CP, Rothschild JM, Cronin JW, et al. Effect of reducing interns' work hours on serious medical errors in intensive care units. N Engl J Med. 2004;351:1838–48. doi: 10.1056/NEJMoa041406. [DOI] [PubMed] [Google Scholar]
- 3.Horwitz LI, Kosiborod M, Lin Z, Krumholz HM. Changes in outcomes for internal medicine inpatients after work-hour regulations. Ann Intern Med. 2007;147:97–103. doi: 10.7326/0003-4819-147-2-200707170-00163. [DOI] [PubMed] [Google Scholar]
- 4.Shetty KD, Bhattacharya J. Changes in hospital mortality associated with residency work-hour regulations. Ann Intern Med. 2007;147:73–80. doi: 10.7326/0003-4819-147-2-200707170-00161. [DOI] [PubMed] [Google Scholar]
- 5.Kaushal R, Bates DW, Landrigan C, et al. Medication errors and adverse drug events in pediatric inpatients. JAMA. 2001;285:2114–20. doi: 10.1001/jama.285.16.2114. [DOI] [PubMed] [Google Scholar]
- 6.Gottlieb DJ, Parenti CM, Peterson CA, Lofgren RP. Effect of a change in house staff work schedule on resource utilization and patient care. Arch Intern Med. 1991;151:2065–70. [PubMed] [Google Scholar]
- 7.McCoy CP, Halvorsen AJ, Loftus CG, McDonald FS, Oxentenko AS. Effect of 16-hour duty periods on patient care and resident education. Mayo Clin Proc. 2011;86:192–6. doi: 10.4065/mcp.2010.0745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schuberth JL, Elasy TA, Butler J, et al. Effect of short call admission on length of stay and quality of care for acute decompensated heart failure. Circulation. 2008;117:2637–44. doi: 10.1161/CIRCULATIONAHA.107.740357. [DOI] [PubMed] [Google Scholar]
- 9.Landrigan CP, Fahrenkopf AM, Lewin D, et al. Effects of the accreditation council for graduate medical education duty hour limits on sleep, work hours, and safety. Pediatrics. 2008;122:250–8. doi: 10.1542/peds.2007-2306. [DOI] [PubMed] [Google Scholar]
- 10.Chua KP, Gordon MB, Sectish T, Landrigan CP. Effects of a night-team system on resident sleep and work hours. Pediatrics. 2011;128:1142–7. doi: 10.1542/peds.2011-1049. [DOI] [PubMed] [Google Scholar]
- 11.3M™ APR DRG Software. [Accessed March 12, 2012]. http://solutions.3m.com/wps/portal/3M/en_US/3M_Health_Information_Systems/HIS/Products/APRDRG_Software/
- 12.Ulmer C, Wolman D, Johns M, editors. Washington, DC: The National Academics Press; 2009. Resident Duty Hours: Enhancing Sleep, Supervision and Safety. [PubMed] [Google Scholar]


