Abstract
Background
Studies have suggested that patient contact time for internal medicine residents is decreasing and being replaced with computer-related activities, yet objective data regarding computer use by residents are lacking.
Objective
The aim of this study was to objectively measure time use by internal medicine residents while on duty in the hospital setting using real-time, voice-capture technology.
Methods
First- and third-year categoric internal medicine residents participated (n = 25) during a 3-month period in 2010 while rotating on general internal medicine rotations. Portable speech-recognition technology was used to record residents' activities. The residents were prompted every 15 minutes from an earpiece and asked to categorize the activity they had been doing since the last prompt, choosing from a predetermined list of 15 activities.
Results
Of the 1008 duty-time responses, 493 (49%) were classified as computer-related activities, whereas 341 (34%) were classified as direct patient care, 110 (11%) were classified as noncomputer-related education, and 64 (6%) were classified as other activities. Of resident reported computer-use time, 70% was spent on patient notes and order entry.
Conclusions
The results of our study suggest that computer use is the predominant activity for internal medicine residents while in the inpatient setting. Work redesign because of duty hour regulations should consider how to free up residents' time from computer-based activities to allow residents to engage in more direct patient care and noncomputer-based learning.
Introduction
There is ongoing concern that residents spend less time in direct patient care activities and increasing time on documentation using electronic medical records and other electronic modules for patient care and reimbursement.1–3 A 2010 national survey4 completed by more than 16 000 internal medicine (IM) residents revealed that 68% spent more than 4 hours daily on clinical documentation while in the inpatient setting, compared with only 39% who spent this same amount of time in direct patient care. However, much of the reported data regarding how residents spend their time in the hospital is based on subjective observation and survey responses. Handheld devices have been used to capture information within the workplace by residents, but these studies did not focus on on-call activities.5,6 Given changes in duty hour requirements,7 it is imperative that time use be scrutinized to maximize patient contact and education.
It is difficult to obtain objective data on how residents allocate their time because of residents' busy schedules, which limit their time to complete objective, time-in-motion studies; hand-washing and isolation procedures, which make the use of electronic sensor systems challenging; and finally, variability of residents' on-call practices, which makes measurement a technical challenge. Our goal was to objectively determine how time was used by residents while on duty in the hospital using real-time, voice-capture technology to overcome the aforementioned barriers.
Methods
Setting and Participants
The Mayo Clinic Internal Medicine Residency has 48 categoric residents in each of 3 sequential years of training. During the study period, between February and April 2010, 63 residents were assigned to the general IM services. Participation was voluntary; 25 of 63 residents (40%) agreed to participate, of whom 64% (16 of 25) were men. Written consent was obtained from residents, and a tutorial was provided by study personnel before the equipment was used. The study was approved by the Mayo Clinic Institutional Review Board.
Data Collection
Residents carried a voice-capture technology device (VoiceViewer; Bannockburn, IL). The device was equipped with an earpiece microphone worn continuously during the recording time. Every 15 minutes, the system prompted the resident through the earpiece asking, “What are you doing now?” The resident had 10 seconds to verbally respond using one of 15 predetermined prompts (table). These prompts were determined after a pilot project with 10 residents who used the technology; initial prompts were modified based on feedback. More than one prompt could be entered if time was divided between activities. Responses were recorded and time-stamped by the device. Residents were asked to wear the device for 3 days, including a precall day, an on-call day, and a postcall day, with the device removed when leaving duty or resting on call.
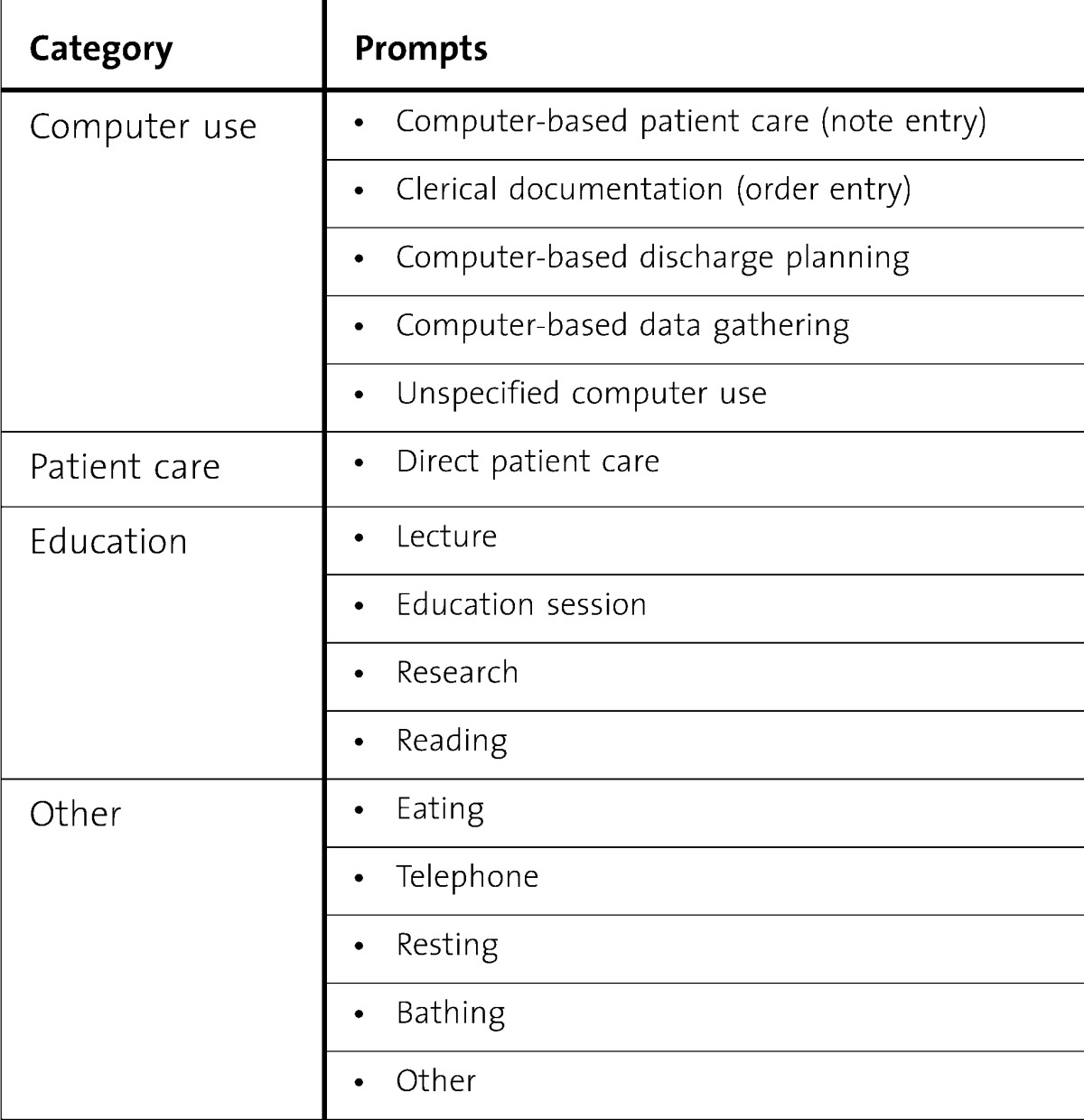
TABLE.
Fifteen Prompts According to Category
Data Analysis
Time-stamped audio files were stored, and each audio clip was analyzed by a trained researcher to allow accurate categorization. Ten percent of files (random allocation) were also analyzed by an independent, blinded investigator to verify accuracy.
Results
A session was defined as the time a resident wore the voice-capture device continuously. There were 60 sessions recorded by 25 residents; the average session length was 11 hours. A total of 1008 audio clips were analyzed, totaling 252 duty hours. Of the 2547 responses, 1539 (60%) were blank, with blank responses distributed throughout duty periods and across residents, with a slight increase during evening hours (figure 1). The 15 predetermined prompts were allocated into 4 categories (figure 2). The 1008 duty-time responses were classified as follows: 493 (49%) were computer-related; 341 (34%) were direct patient care-related; 110 (11%) were noncomputer-related education; and 64 (6%) were other. The various activities classified as computer use are shown in figure 3. Computer use related to patient care and clinical documentation (patient notes and order entry) accounted for 70% (346/493) of computer use time; computer-based discharge planning (dismissal summaries and prescriptions) was 8% (37/493); and electronic data gathering (reviewing the medical record) was 5% (26/493). Unspecified computer use made up the remainder of time (17%, 84/493), and included reading e-mail and general Internet use.
FIGURE 1.
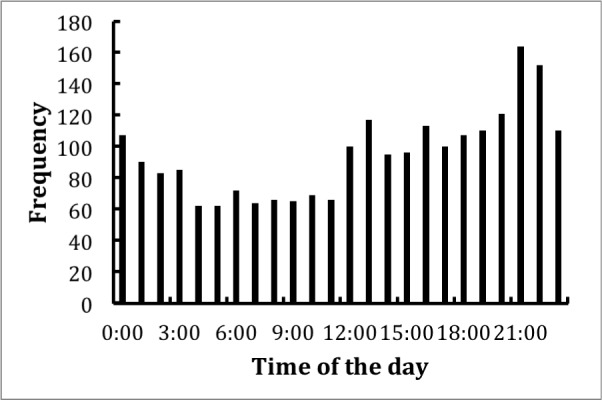
Distribution of Blank Responses Throughout the Recording Periods
FIGURE 2.
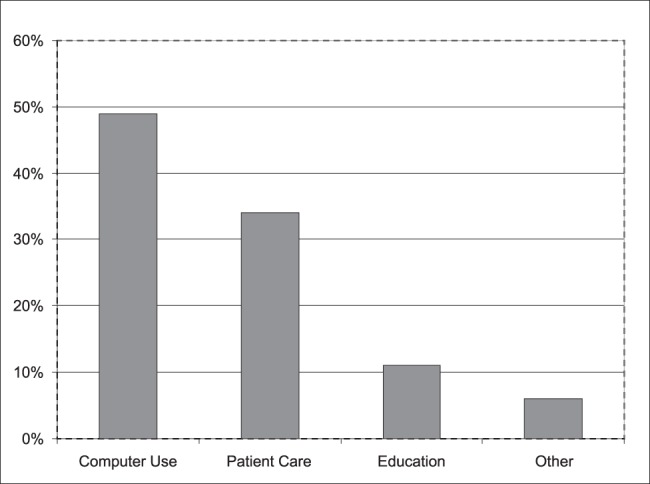
Percentage of Time Internal Medicine Residents Spent on Various Inpatient Activities
FIGURE 3.
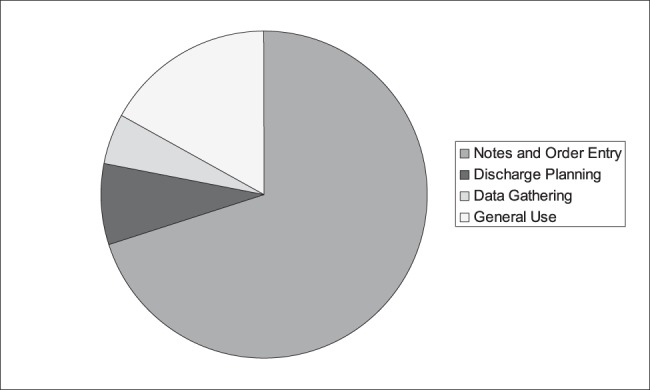
Breakdown of Computer Use Time by Internal Medicine Residents in the Inpatient Setting
Discussion
Our major finding was that IM residents spent half their time on duty using a computer while on inpatient rotations. Most of computer-use time was associated with patient care, which included typing notes and order entry. Approximately one-third of residents' time was spent in direct face-to-face patient care. These objective findings substantiate prior subjective reports, such as the large national study4 of IM residents, where more than two-thirds of residents reported spending in excess of 4 hours per day on documentation.
Alromaihi et al8 similarly attempted to objectively categorize time spent by IM residents in the inpatient setting with personal digital assistants, noting 43% of residents' time was spent on the computer (compared with 49% in our study) and 20% time in direct patient contact (compared with 34% in our study). However, their study used a hybrid electronic-paper medical record system, and multitasking could not be captured. Our institution uses a comprehensive electronic medical system, which may account for increased computer use by our residents. The novel use of voice-capture technology allowed our residents to categorize more than one activity during the preceding time interval, thereby enabling multitasking.
Federal efforts are in place to provide incentives to hospitals to incorporate electronic health record systems.9 A 2008 survey10 found only 1.5% of US hospitals had comprehensive electronic medical records (EMRs). Additionally, the use of an EMR is now required by the Residency Review Committee for IM,11 so it is likely that residents will spend increasing time at a computer given these mandates. Possible benefits of the EMR on training include increased efficiency in gathering medical information, safer order entry, and the ability to access interactive online programs.12 However, EMRs have been shown to have negative consequences on teacher-learner interactions, workflow,13 and note quality, the latter because of the “cut and paste” function.14 Lack of trainee feedback on clinical documentation is also a concern; one academic medical center found that 16% of all electronic notes were unread.15
The potential adverse effects of excessive computer use on residents should not be ignored. The prevalence of neck, wrist, and shoulder pain is notable in computer users, and is significantly higher with increased use.16,17 Additionally, an association between computer mouse use of greater than 20 hours weekly and carpal tunnel syndrome has been found.18 Finally, visual-display terminal work of 6 or more hours daily can negatively affect total sleep duration and cause excessive daytime sleepiness.19
In light of recent duty hour changes, training programs should use the findings of this and similar studies to create initiatives to decrease computer use time to optimize patient contact and education. The use of dictation services, electronic note systems, and voice recognition software could be employed to reduce computer use time.
Our study has several limitations. First, it was conducted at a single institution with a comprehensive EMR, limiting generalizability. Second, there were a large number of blank survey responses, and is it not possible to assess whether there was an equal distribution of activities that were not categorized. Additionally, residents were not allowed to wear the voice-capture devices in patient rooms with isolation practices. Finally, the designation of an activity into one or more of 15 preselected prompts is a reflection of how the resident categorized an activity; whether residents routinely labeled certain activities into more than one category is unknown.
Conclusions
Through the use of voice-capture technology, we were able to objectively demonstrate that computer use accounts for approximately half of IM residents' time in the inpatient setting. We hope that this study will precipitate a reevaluation of how resident time in the hospital setting can be used most appropriately.
Footnotes
All authors are at Mayo Clinic. Amy S. Oxentenko, MD, is a Consultant, Fellowship Director, and Vice Chair for Education in Gastroenterology and Hepatology, and is an Associate Professor of Medicine; at the time of writing, Chinmay U. Manohar, MS, was a Research Assistant in Endocrinology; he is now Senior Fellow, Medical Device Center, University of Minnesota; Christopher P. McCoy, MD, is a Senior Associate Consultant and Instructor of Medicine in Hospital Internal Medicine; at the time of writing, William K. Bighorse, BA, was a Research Assistant in Endocrinology; he is now Field Interviewer for the National Health and Alcohol Study in Seneca Falls, NY; Furman S. McDonald, MD, MPH, is a Consultant in General and Hospital Internal Medicine, Associate Chair for Residency Programs, Internal Medicine Residency Program Director, and an Associate Professor of Medicine; at the time of writing, Joseph C. Kolars, MD, was an Emeritus Internal Medicine Residency Program Director and Consultant and Professor of Medicine in Gastroenterology and Hepatology; he is now the Senior Associate Dean for Education and Global Initiatives at the University of Michigan Medical School; and James A. Levine, MD, PhD, is a Consultant and Professor of Medicine in Endocrinology.
Funding: This study was supported in part by the Mayo Clinic Internal Medicine Residency Office of Educational Innovations as part of the Accreditation Council for Graduate Medical Education Educational Innovations Project. Funding for the project was also provided by grants DK56650, DK63226, DK66270, and DK50456 (Minnesota Obesity Center); RR-0585 (United States Public Health Service); the Mayo Foundation; and, in part, VoiceViewer to Dr Levine.
References
- 1.Moore SS, Nettleman MD, Beyer S, Chalasani K, Fairbanks RJ, Goyal M, et al. How residents spend their nights on call. Acad Med. 2000;75(10):1021–1024. doi: 10.1097/00001888-200010000-00020. [DOI] [PubMed] [Google Scholar]
- 2.Lurie N, Rank B, Parenti C, Woolley T, Snoke W. How do house officers spend their nights? a time study of internal medicine house staff on call. N Engl J Med. 1989;320(25):1673–1677. doi: 10.1056/NEJM198906223202507. [DOI] [PubMed] [Google Scholar]
- 3.Boex JR, Leahy PJ. Understanding residents' work: moving beyond counting hours to assessing educational value. Acad Med. 2003;78(9):939–944. doi: 10.1097/00001888-200309000-00022. [DOI] [PubMed] [Google Scholar]
- 4.Oxentenko AS, West CP, Popkave C, Weinberger SE, Kolars JC. Time spent on clinical documentation: a survey of internal medicine residents and program directors. Arch Intern Med. 2010;170(4):377–380. doi: 10.1001/archinternmed.2009.534. [DOI] [PubMed] [Google Scholar]
- 5.Tejani N, Dresselhaus TR, Weinger MB. Development of a hand-held computer platform for real-time behavioral assessment of physicians and nurses. J Biomed Inform. 2010;43(1):75–80. doi: 10.1016/j.jbi.2009.08.011. [DOI] [PubMed] [Google Scholar]
- 6.Stucky ER, Dresselhaus TR, Dollarhide A, Shively M, Maynard G, Jain S, et al. Intern to attending: assessing stress among physicians. Acad Med. 2009;84(2):251–257. doi: 10.1097/ACM.0b013e3181938aad. [DOI] [PubMed] [Google Scholar]
- 7.Nasca TJ, Day SH, Amis ES., Jr ACGME Duty Hour Task Force. The new recommendations on duty hours from the ACGME Task Force. N Engl J Med. 2010;363(2):e3. doi: 10.1056/NEJMsb1005800. doi:10.1056/NEJMsb1005800. [DOI] [PubMed] [Google Scholar]
- 8.Alromaihi D, Godfrey A, Dimoski T, Gunnels P, Scher E, Baker-Genaw K. Internal medicine residents' time study: paperwork versus patient care. J Grad Med Educ. 2011;3(4):550–553. doi: 10.4300/JGME-D-11-00057.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jha AK. Meaningful use of electronic health records: the road ahead. JAMA. 2010;304(15):1709–1710. doi: 10.1001/jama.2010.1497. [DOI] [PubMed] [Google Scholar]
- 10.Jha AK, DesRoches CM, Campbell EG, Donelan K, Rao SR, Ferris TG, et al. Use of electronic health records in U.S. hospitals. N Engl J Med. 2009;360(16):1628–1638. doi: 10.1056/NEJMsa0900592. [DOI] [PubMed] [Google Scholar]
- 11.Accreditation Council for Graduate Medical Education. ACGME Program Requirements for Graduate Medical Education in Internal Medicine. http://acgme.org/acWebsite/downloads/RRC_progReq/140_internal_medicine_07012009.pdf. Page 3, item I.A.2.k. Accessed January 16, 2012. [Google Scholar]
- 12.Doll JA, Arora V. Time spent on clinical documentation: is technology a help or a hindrance. Arch Intern Med. 2010;170(14):1276. doi: 10.1001/archinternmed.2010.228. [DOI] [PubMed] [Google Scholar]
- 13.Schenarts PJ, Schenarts KD. Educational impact of the electronic medical record. J Surg Educ. 2012;69(1):105–112. doi: 10.1016/j.jsurg.2011.10.008. [DOI] [PubMed] [Google Scholar]
- 14.Hirschtick RE. A piece of my mind: copy-and-paste. JAMA. 2006;295(20):2335–2336. doi: 10.1001/jama.295.20.2335. [DOI] [PubMed] [Google Scholar]
- 15.Hripcsak G, Vawdrey DK, Fred MR, Bostwick SB. Use of electronic clinical documentation: time spent and team interactions. J Am Med Inform Assoc. 2001;18(2):112–117. doi: 10.1136/jamia.2010.008441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lorusso A, Bruno S, L'Abbate N. Musculoskeletal disorders among university student computer users [in Italian] Med Lav. 2009;100(1):29–34. [PubMed] [Google Scholar]
- 17.Zejda JE, Bugajska J, Kowalska M, Krzych L, Mieszkowska M, Brozek G, et al. Upper extremities, neck and back symptoms in office employees working at computer stations [in Polish] Med Pr. 2009;60(5):359–367. [PubMed] [Google Scholar]
- 18.Andersen JH, Thomsen JF, Overgaard E, Lassen CF, Brandt LP, Vilstrup I, et al. Computer use and carpal tunnel syndrome: a 1-year follow-up study. JAMA. 2003;289(22):2963–2969. doi: 10.1001/jama.289.22.2963. [DOI] [PubMed] [Google Scholar]
- 19.Yoshioka E, Saijo Y, Fukui T, Kawaharada M, Kishi R. Association between duration of daily visual display terminal work and insomnia among local government clerks in Japan. Am J Ind Med. 2008;51(2):148–156. doi: 10.1002/ajim.20543. [DOI] [PubMed] [Google Scholar]


