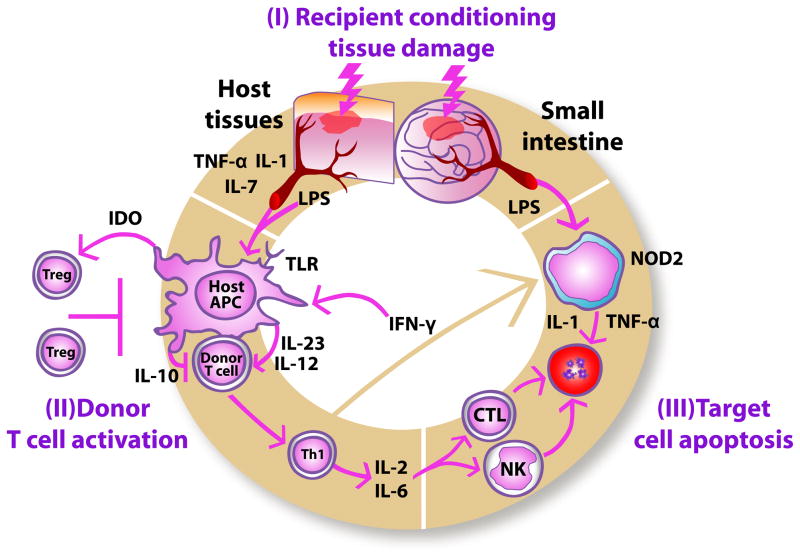
Figure 1.
Pathophysiology of acute graft-versus-host disease. During the first phase (I), recipient conditioning regimen damages patient tissues and causes release of inflammatory cytokines such as TNF-α, IL-1 and IL-7, which leads to activation of host antigen-presenting cells (APCs). In the second phase (II), host APCs activate mature donor cells through IL-12 and IL-23 to produce T helper cell type 1 (Th1) cytokines, such as IL-2, IL-6 and IFN-γ. The synthesis of inflammatory cytokines is partly inhibited by IL-10. Activated Th1 cells induce increased indoleamine 2,3-dioxygenase (IDO) secretion from host APCs through IFN-γ secretion, thus stimulating immunotolerizing Tregs. IFN-γ also stimulates mononuclear cells to secrete inflammatory cytokines, such as IL-1 and TNF-α. (III) Th1 cells promote proliferation and differentiation of activated cytotoxic T lymphocytes (CTLs) and stimulate Natural Killer (NK) cells, which, in turn, induce apoptosis. Lipopolysaccharide (LPS) and bacterial cell wall components that have leaked through the damaged intestinal mucosa stimulate mononuclear cells through interactions with NOD2 and other innate immunity proteins, thus triggering additional inflammatory cytokine production causing apoptosis.