Abstract
In recent years ultrasonography (US) has emerged as the imaging technique of choice for guiding diagnostic and therapeutic procedures including those related to the musculoskeletal system. However, the absence of ionizing radiation and the elevated safety of the method must not lead us to forget that there are precautions and contraindications to keep in mind, which are crucial to the protection of both the patient and the physician.
Among these precautions it is first of all essential to obtain the patient’s accurate clinical history including current medication, particularly if it involves drugs influencing the blood clotting, and information related to possible allergies. The patient should furthermore receive detailed information concerning the procedure (sterile precautions as well as possible side-effects of the drugs which will be injected). In addition to this, there must be a close contact between the radiologist and the patient’s general physician (GP) in order to obtain the best possible result of the procedure.
Keywords: Ultrasonography, Musculoskeletal ultrasound, Interventional ultrasound
Sommario
Negli anni recenti l’ecografia si è imposta come tecnica, spesso di elezione, per guidare interventi diagnostici e terapeutici, anche in ambito muscolo-scheletrico. L’assenza di radiazioni ionizzanti e la quasi innocuità delle procedure non devono, tuttavia, far dimenticare che esistono precauzioni da prendere e controindicazioni da conoscere, essenziali per la tutela del paziente e del medico.
Tra le precauzioni sono punti fondamentali il rigore e l’accuratezza nell’ottenimento dell’anamnesi (conoscere eventuali assunzioni di farmaci, in particolare di quelli che interagiscono con la coagulazione, o allergie del paziente), informare dettagliatamente il paziente sulla modalità di realizzazione delle procedure (effetti collaterali dei farmaci che saranno iniettati) e la sterilità.
A tutto questo deve sempre aggiungersi un corretto rapporto ecografista/medico curante che consenta di ottenere risultati ottimali.
Introduction
Thanks to the recent technological development of ultrasound (US) hardware and software, US has acquired a leading position in the diagnosis of diseases affecting the musculoskeletal system.
The main advantage of musculoskeletal US (MSUS) is that the procedure is inexpensive, non-invasive, easily available and dynamic.
In recent years, MSUS has also emerged as an excellent technique for guiding diagnostic and therapeutic procedures. The absence of ionizing radiation, the widespread availability of equipment along with the ability to monitor in real time the progress of devices such as needles, catheters, etc. are the main advantages of US guidance.
The purpose of this article is twofold: to briefly review the main indications and contraindications of interventional MSUS and to describe the precautions which should be taken during the procedure.
Indications
Indications for US-guided procedures involving lesions of the musculoskeletal system can be summarized in two main categories: diagnostic (Table 1) and therapeutic (Table 2) procedures.
Table 1.
US-guided diagnostic procedures in musculoskeletal diseases.
| Diagnostic Procedures | ||||||
|---|---|---|---|---|---|---|
| ArthrocentesisBursocentesis Tenocentesis |
Aspiration of synovial fluid:
|
Limb joints | Tendon sheaths: ankle, wrist and hand |
Synovial bursae:
|
||
| Aspiration of cysts | Mucoid cysts (periarticular, parameniscal, tendon, intramuscular, intranervous)Cysts of the skin and subcutaneous cystsOthers | Mucoid cysts of the wrist and fingers | Meniscal cysts | Spinoglenoid incision of the shoulder | Intramuscular mucoid cysts situated in the anterior or exterior compartment of the leg | Intranervous mucoid cysts of the peroneal nerve |
| Aspiration of fluid collections | AbscessHematomaLymphocele | Hematoma in muscle strain injuriesMorel-Lavallée lesion | ||||
Table 2.
Therapeutic procedures carried out under US guidance in musculoskeletal diseases.
| Therapeutic Procedures | |||||
|---|---|---|---|---|---|
| Infiltration of the synovium | Cortisonic derivative | Hyaluronic acid | Anesthetics | ||
| Tendonitis treatment | Cortisone | Needling | Blood | Polidocamol | Puncture-crushing |
| Treatment of muscle injuries | Intramuscular hematoma | Intermuscular hematoma | Fluid collection at the muscle-tendon junction | ||
| Treatment of neurological lesions | Nerve blocks | Treatment of Morton’s neuroma | Amputation neuromas | ||
| Tenotomy Fasciotomy | Dupuytren | ||||
| Foreign bodies | US-guided removal | ||||
A diagnostic procedure is aimed at obtaining a biological sample (fluid or cellular) in order to determine the etiology of the lesion.
Drainage of fluid collections is undoubtedly the most frequent indication in daily MSUS practice (Fig. 1). This procedure may be requested by the GP if the fluid collection was revealed at a clinical examination (fluid filled swelling) or it may have been identified at a US scanning. In some locations, clinical examination can identify a fluid collection, in other locations this is not possible; e.g., lesions of the hip cannot be evaluated at clinical examination as they are situated deep inside the body. Clinical examination can furthermore not differentiate joint effusion from synovial hypertrophy.
Fig. 1.
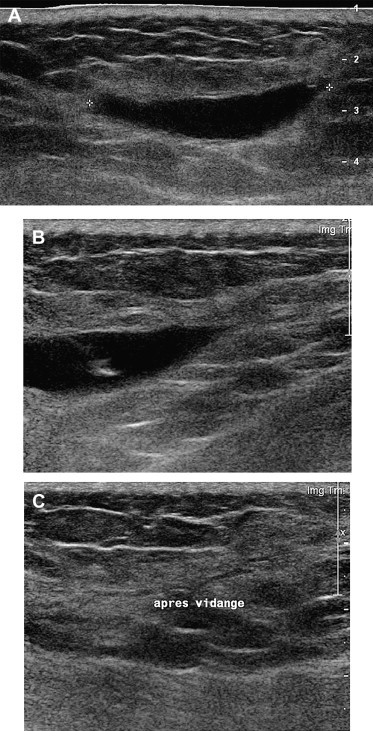
US-guided drainage of a seroma situated in the buttock (A, B): after aspiration, US demonstrates that the lesion is almost empty (C).
If the procedure was requested by the GP, the patient will already be informed about the procedure and he/she will have discussed the advantages and disadvantages of US guidance with the GP. Otherwise, it is up to the US-operator to decide if the procedure should be carried out immediately or after having discussed the possible risks with the patient and contacted the GP to get his/her consent as well as the laboratory to book the appropriate analyses.
One group of fluid-containing lesions (Table 1) affects the synovial structures (joint cavities, tendon sheaths and bursae) (Figs. 2–5).
Fig. 2.
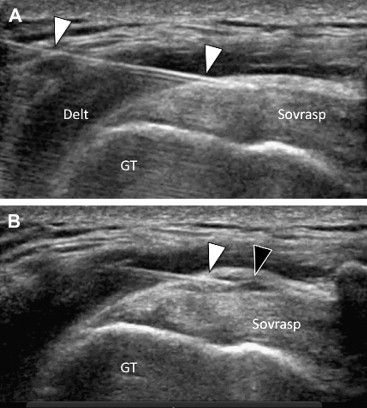
Shoulder: Lateral infiltration of cortisone and anesthetic in the subacromial bursa. A) US image, performed in the coronal oblique plane, shows the 22-Gauge needle (white arrowheads) situated between the deltoid muscle (Delt) and the supraspinatus tendon (sovrasp). The needle tip is perfectly positioned in the subacromial bursa showing wall thickening and absence of internal fluid collection. B) After US-guided injection of a few drops of solution, the injected solution is visible (black arrowhead) in the form of a small anechoic fluid collection situated inside the bursa. GT = greater tuberosity of the humerus.
Fig. 3.
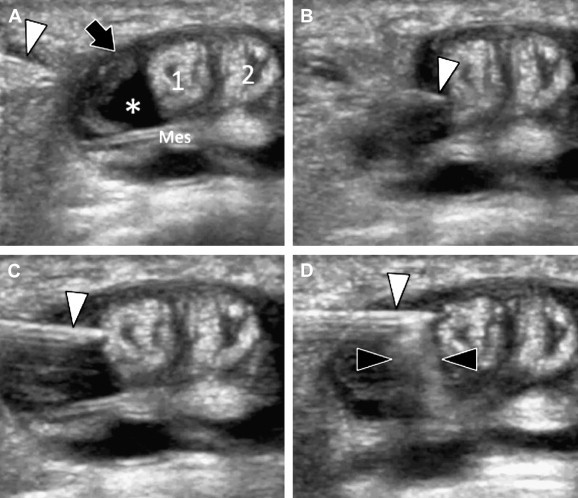
Wrist: infiltration of anesthetic and cortisone into the synovial sheath of the extensor tendons of the wrist (first compartment) for De Quervain’s disease. A) US image performed in the axial plane shows the 25-Gauge needle (white arrowhead) situated in the soft tissue and evidences hypoechoic thickening of the tendon sheath (black arrow) associated with synovial effusion (asterisk) surrounding the mesotenon (mes) and partially the two tendons (1 and 2). B,C) Sequential images showing the tip of the needle piercing the sheath and approaching the fluid collection. D) Image showing the steroid solution spreading in the synovial effusion (black arrowheads) during US-guided injection.
Fig. 4.
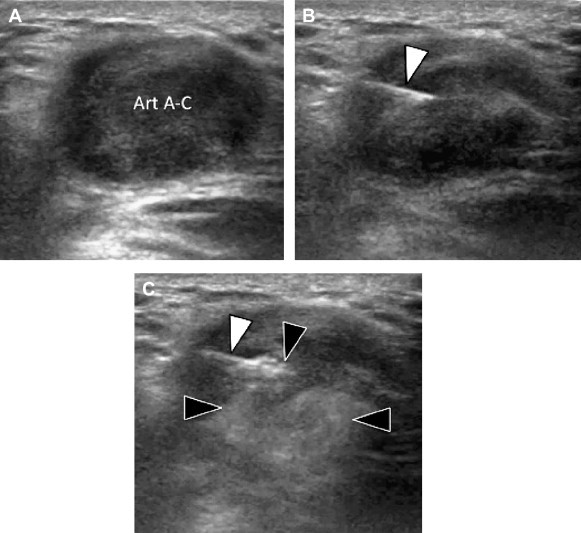
Shoulder. Infiltration of cortisone and anesthetic into the acromioclavicular articulation. A) US image performed in oblique sagittal plane shows a hypoechoic swelling of the joint. B) After US-guided introduction of a 25-Gauge needle (white arrowhead), the image shows the perfect position of the needle tip in the center of the joint. C) Image showing the steroid solution spreading in the joint (black arrowheads) during injection.
Fig. 5.
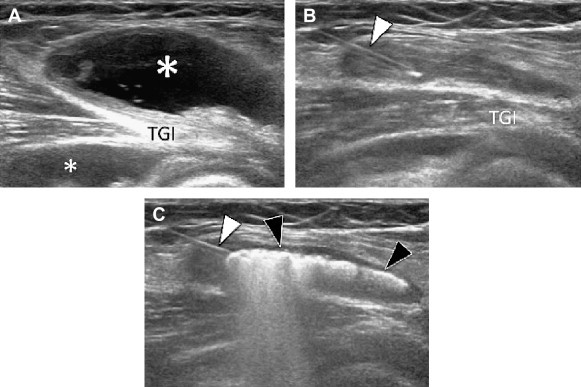
Knee. Infiltration of cortisone and anesthetic into a Baker’s cyst. A) US image performed in the sagittal plane shows the cyst (asterisk) as a hypo-anechoic mass; the deep component (small asterisk) is placed in front of the tendon of the internal twin muscle (TGI). B) Image showing the correct position of the 19-Gauge needle (white arrowhead) after nearly complete aspiration of intracystic synovial fluid. C) Image showing intracystic injection of costicosteroid solution (black arrowheads); absence of fluid in the surrounding tissues.
All synovial cavities which contain a sufficient amount of liquid can be reached under US guidance. The technique used at the procedure obviously varies according to the site of the fluid collection. Analysis of the aspired synovial fluid permits differentiation between various pathologies. The presence of uric acid crystals, calcium pyrophosphate or hydroxyapatite lead to a diagnosis of gout, chondrocalcinosis or a disease involving amorphous calcification.
A definitive diagnosis of an infectious process, evident or only suspected, cannot be made or excluded by the mere inspection of the aspirated fluid, as microscopic examination followed by culture is required.
MSUS also permits minimally invasive and safe puncture of cysts of various kinds (Fig. 6). After synovial cysts, mucoid cysts are the most frequent. At MSUS they appear as well-delimited masses, often multiloculated due to internal septations. At US, simple cysts are hypoechoic, whereas aged cysts containing thickened septations are mixed. Aspiration of a thick, viscous, gel-type liquid associated by the corresponding MSUS characteristics permits a diagnosis of the nature of the lesion. Due to the nature of their contents, mucoid cysts are aspirated using large caliber needles (18–19 Gauge); only a small amount of liquid can be aspirated, but macroscopic analysis can confirm the diagnosis. In addition to the aspiration, it is often necessary to perforate the cystic wall several times to cause rupture and reabsorption of the fluid by the surrounding tissues.
Fig. 6.
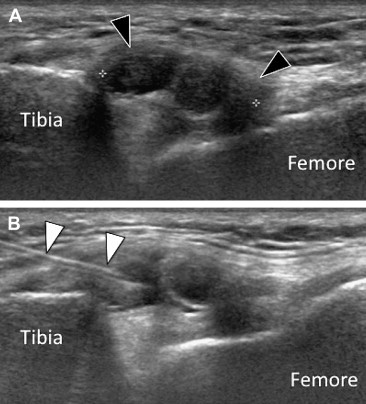
Knee. Infiltration of cortisone and anesthetic in a parameniscal cyst. A) US image performed in the coronal plane shows the cyst (black arrowheads) as a hypoechoic mass, which contains thin septa, adhering to the inner aspect of the body meniscus. B) Image showing the correct position of the 19-Gauge needle (white arrowhead) whose tip is at the center of the mucoid cyst.
US-guided aspiration of an abscess can in most cases provide diagnosis already at macroscopic examination of the aspired fluid. Laboratory tests will confirm this suspicion, identify the microorganism responsible for the infection and establish a targeted therapy.
Indications for US-guided therapeutic procedures have increased (Table 2) involving infiltration of the synovial structures, treatment of tendinopathy (Figs. 7 and 8), muscle injury, neurological damage, tenotomy, fasciotomy and removal of foreign bodies.
Fig. 7.
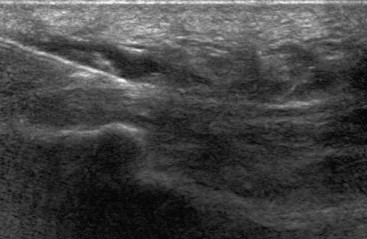
Infiltration of cortisone in a patient with plantar fasciitis. The needle is introduced under US guidance (arrows) from proximal to distal till it reaches the affected tissue which appears of increased volume and hypoechoic compared to normal tissue.
Fig. 8.
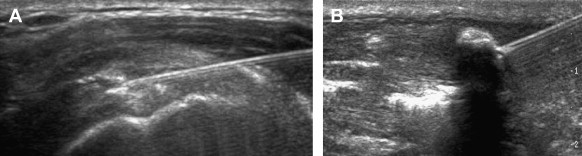
US-guided treatment of calcifications of the supraspinatus tendon (A) and Achilles tendon (B); US can in real time follow the different stages of the treatment and the therapeutic results.
The indication for drainage of muscular hematoma can vary from location to location and according to the clinicians’ beliefs and attitudes. Some sports doctors do not recommend drainage particularly in young athletes to avoid the risk of secondary infections and also because these lesions generally clear up spontaneously. Other clinicians advocate total drainage of the hematoma followed by a compression bandage to prevent recurrent hematoma, particularly in high-level athletes.
Precautions and contraindications
The remarkable frequency with which interventional procedures are carried out under US guidance and the safety of these procedures should not lead us to forget that they are still invasive and that the use of US equipment, compared to interventional procedures without US guidance, presents new risks particularly with regard to asepsis.
Before the procedure, the patient has to be fully informed about its risks and purpose as established by government regulations of medical practice which vary from nation to nation and tend to become more and more complex. This is also an opportunity for the physician to become better acquainted with the patient in order to evaluate absolute and possible contraindications [1]. It is important to keep in mind that performance of the procedure according to the protocol does not exempt the physician who carries it out from the obligation to inform the patient.
The information can be transmitted orally, but it is preferable to prepare an informed consent form that the patient must fill in, sign and return to the physician before the procedure. The form must explain the way the procedure is carried out listing possible complications and their frequency rate, and there must be a blank space where the patient can ask possible questions. The form must also contain a number of questions for the patient to answer in order to obtain the clinical history particularly in order to reveal the presence of cardiovascular diseases, diabetes, osteoporosis, hemopathologies, glaucoma or allergic diathesis. It is important to know what possible therapies the patient is undergoing particularly if he/she is receiving drugs which might alter the hemostatic mechanism.
It would be an advantage if the patient had the phone number of the physician who will carry out the procedure for any questions or in case of complications.
Asepsis is one of the key points in a successful performance of interventional procedures. Localized skin infection at the injection site is a contraindication to the procedure. In the absence of this contraindication, the disinfection of the skin is done in five steps as follows [2,3]: use of antiseptic soap, rinsing with sterile water, drying with sterile gauze, application of iodinated derivatives (or chlorhexidine if the patient is allergic to iodine), drying with sterile gauze.
Both the physician and the patient must wear masks and the physician should thoroughly disinfect his/her hands using an ethanol-water solution. Preparation of the US probe differs according to the intended use. Although it is advisable to use sterile protection, gloves and sterile gel, the procedure can be carried out without placing a sterile cover over the probe, but only if the needle does not touch the probe (“no touch” procedure) [1]. If this occurs it is necessary to sterilize the probe directly using the products recommended by the manufacturer of the equipment.
It is not necessary that all patients undergoing US-guided interventional procedures present hemostasis test, which is required only in aged and particularly fragile patients. It must be emphasized that the physician who performs the procedure must not modify a possible anticoagulant therapy without contacting the GP with whom the cost–benefit relationship must be evaluated in order to choose the best option for the patient [1,3].
It is also necessary to distinguish between the risk of bleeding and the risk of hemorrhage related to the insertion of needles, the site and the characteristics of the patient (it is obvious that a deep puncture in an aged patient will not carry the same consequences as an interphalangeal joint injection in a young patient).
Several drugs, including antiplatelet agents, aspirin, clopidogrel, nonsteroidal anti-inflammatory drugs, antidepressants, heparin and anti-vitamin-K drugs may affect the mechanism of blood coagulation, and all the appropriate precautions must be taken.
All US-guided procedures can be performed in patients treated with aspirin if the needles are 18 Gauge or less [2–4]; if larger needles are required (especially in biopsies) the GP’s consent must be obtained. It is not advisable to interrupt an aspirin therapy without contacting the GP, not even a low-dose therapy over a short period of time, as this involves an increased risk of thrombosis, particularly in patients who have an active stent [5].
Clopidogrel carries a high risk of hemorrhage, independently of the dose. A possible interruption of the therapy must always be discussed with the GP depending on the procedure to be performed [1,3]. Some nonsteroidal anti-inflammatory drugs (naproxen, pyroxicam) and antidepressant drugs such as serotonin reuptake inhibitors have an antiplatelet effect similar to that of aspirin, and the same precautions must therefore be taken. In patients receiving prophylactic low-dose heparin therapy, the procedure must be carried out according to the heparin injection schedule, whereas the procedure is contraindicated in patients who receive full-dose heparin therapy. If the procedure is expected to be of substantial benefit to the patient, the cost–benefit relationship must be evaluated with the GP [1,3]. In patients who receive anti-vitamin-K drug therapy, the procedure is contraindicated; however, if the expected benefit is important, the procedure can be carried out in agreement with the GP if the patient’s international normalized ratio (INR) is around 2 [3]. A small series of 32 patients who underwent diagnostic or therapeutic musculoskeletal procedures presented no bleeding complications [6]; however, evaluation of a larger number of patients is required to modify the present indications [1].
Other precautions are related to the drugs injected during the procedure. In all cases the expiry date of the product must be checked and the lot number must be registered. The most commonly used drugs are corticosteroids (Figs. 3,4) which are absolutely contraindicated in patients with infections, glaucoma, cataracts and some psychiatric diseases. In case of osteoporosis or severe hypertension, steroids should be avoided or used only in limited amounts [1]. Diabetes is not an absolute contraindication, although infiltration presents a risk of temporary hyperglycemia, and insulin may therefore be required. The patient should be told to check blood glucose the following day and every day for a week so that the GP can be contacted in case of significant hyperglycemia. For other drugs that are used in musculoskeletal infiltration (phenol, lidocaine or other anesthetics, radiological contrast agents, sodium hyaluronate and polidocanol), the specific precautions and contraindications related to each drug must be followed scrupulously.
In cases of acquired coagulation disorders (including thrombocytopenia due to renal failure) or congenital disorders (including hemophilia and von Willebrand disease), each patient should be evaluated in agreement with the GP [1,3].
Pregnancy is not a contraindication.
Some general guidelines are also useful: US-guided procedures should always be well-planned and they should only be performed after an accurate ethylene glycol (ETG) test.
Conclusions
Diagnostic and therapeutic interventional procedures of the musculoskeletal system are more and more common, and the indications are increasing. However, there are some contraindications and precautions which are essential for the protection of the patient and the physician.
An important point is the information that the physician gives the patient and receives from him/her; many clinical and medico-legal complications can be avoided by acquiring a thorough knowledge of the patient’s clinical history and if the patient is aware of the risks of the procedure [1]. The patient should receive a form to fill in and return to the physician before the procedure. The form should contain also a blank space, where the patient can ask possible questions, and the telephone number of the physician who carries out the procedure so that the patient can ask further questions before the procedure and, after the procedure, ask what to do in case of complications.
Asepsis is one of the key points of interventional procedures. It must be carried out with great care, and the patient’s skin must be disinfected in five steps [2,3]. To ensure maximum safety, both the physician and the patient must wear masks and the physician must disinfect his hands using an ethanol-water solution.
Blood-tests assessing possible hemostatic disorders are required only in fragile or aged patients. Various drugs can alter blood coagulation; for each of them all the necessary precautions must be taken in agreement with the patient’s GP.
Some precautions are related to the drugs injected during the procedure. In all cases the expiry date of the product must be checked and the lot number must be registered, and the precautions and contraindications specific for each product must be followed. In the presence of clotting disorders each patient should be evaluated with his/her GP. Pregnancy is not a contraindication.
In addition to the number of precautions outlined in this paper, a good and close contact with the GP is essential for the patient’s safety.
Conflict of interest statement
The authors have no conflict of interest.
References
- 1.Jacob D., Cohen M., Guerini H. Actualités en échographie de l’appareil locomoteur. Sauramps; Montpellier: 2007. Echographie interventionnelle: précautions, contre-indications, techniques, complications; pp. 219–225. [Google Scholar]
- 2.Jacob D., Cyteval C., Moinard M. Interventional sonography. J Radiol. 2005;86:1911–1923. doi: 10.1016/s0221-0363(05)81546-x. [DOI] [PubMed] [Google Scholar]
- 3.Jacob D., De Maistre E., Cohen M. Actualités en échographie de l’appareil locomoteur. Sauramps; Montpellier: 2006. Echographie interventionnelle musculo-squelettique et hémostase; pp. 63–70. [Google Scholar]
- 4.Lemaire V., Charbonnier B., Gruel Y., Goupille P., Valat J.P. Joint injections in patients on antiplatelet or anticoagulant therapy: risk mimization. Joint Bone Spine. 2002;69:8–11. doi: 10.1016/s1297-319x(01)00337-2. [DOI] [PubMed] [Google Scholar]
- 5.Ferrari E., Benhamou M., Cerboni P., Marcel B. Coronary syndromes following aspirin withdrawal: a special risk for late stent thrombosis. J Am Coll Cardiol. 2005;45(3):456–459. doi: 10.1016/j.jacc.2004.11.041. [DOI] [PubMed] [Google Scholar]
- 6.Thumboo J., O’Duffy J.D. A prospective study of the safety of joint and soft tissue aspirations and injections in patients taking warfarin sodium. Arthritis Rheum. 1998;41(4):736–739. doi: 10.1002/1529-0131(199804)41:4<736::AID-ART23>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]


