Abstract
Purpose
Since early 1990s pedicle screws in thoracic spine have been used in posterior correction of adolescent idiopathic scoliosis (AIS). Long-term results are scarce. We report clinical, radiological and pulmonary function results of 48 consecutive patients with 10-year minimal follow-up.
Methods
Forty-eight consecutive patients (42 females, 6 males) with 41 Lenke 1 (lumbar modifier A = 19, B = 8, C = 14), 7 Lenke 2 (lumbar modifier A = 2, B = 4, C = 1) were operated for AIS from posterior with pedicle screw alone instrumentation. Risser stage at the time of operation was 0–3 in 24, more than 3 in 24 patients. Mean age was 15.3 years. The data were prospectively collected preoperatively, at 6 weeks, 2 years and 10 years postoperatively. Cobb angle, sagittal and coronal balance, distal adjacent disc angle and lowest fused vertebral tilt were documented at all time-points. Choice of fusion levels is described. Not every vertebra was instrumented with pedicle screws. The implant density was average one pedicle screw per vertebra or 50 %. Derotation and translation of apical vertebrae on the concave side were performed for correction. The overall outcome and the outcome of different curve types were analyzed statistically.
Results
Lowest instrumented vertebra (LIV) was distal end vertebra in two-thirds of the patients and was one below distal end vertebra in one-third of the patients. The main thoracic curve correction was 63 %, from 58° ± 12° preoperative to 21° ± 9° at 6 weeks. The Cobb angle was 23° ± 10° at 2 years and 26° ± 10° at 10 years. The apical vertebral rotation improved 35 %, the non-instrumented lumbar curves improved 47 %, the distal adjacent disc angle decreased from 6° ± 3° preoperatively to −2° ± 4° postoperatively and the last instrumented vertebral tilt decreased from 23° ± 8° preoperatively to 5° ± 5° postoperatively. All these parameters remained stable up to 10-year follow-up. The scoliosis correction was not associated with any change in the preoperative thoracic kyphosis and lumbar lordosis. The % FVC remained unchanged with 74 ± 21 % preoperatively to 74 ± 11 % at 2 years and 75 ± 10 % at 10 years. The SRS-24 score was 93 ± 18 points at 2 years and 95 ± 22 points at 10 years. There were no neurological complications, no pedicle screw-related complications.
Conclusion
Posterior correction of thoracic AIS with pedicle screw instrumentation is safe and produces a long-term stable correction and high patient satisfaction. An implant density of 50 % is sufficient to achieve these results. LIV can be the distal end vertebra or one below the distal end vertebra depending on the position of the distal end vertebra to the centre sacral line. The preoperative pulmonary function does not change on long term.
Keywords: Adolescent idiopathic scoliosis, Selective posterior correction with pedicle screw instrumentation, Choice of fusion levels, Long-term operative results, Long-term pulmonary function
Introduction
Posterior instrumentation with pedicle screw fixation (PSF) has become the current standard of care [1] for adolescent idiopathic scoliosis (AIS). The correction with PSF helps in multidimensional spinal correction [2]. Fusion length with PSF is shorter in comparison with other posterior fixation techniques [3–5]. Although good clinical and subjective outcome has been reported with all pedicle screw constructs [2, 7], long-term results with PSF are not available in the literature [1]. Only the results of 2- to 5-year follow-up have been reported [6–8]. Controversy exists on the density of implant and amount of correction, the loss of correction in Cobb angle as well as in the distal adjacent segment, the changes in thoracic kyphosis, in pulmonary function and above all on the selective fusion of thoracic curves in patients having a significant lumbar curve.
The aim of this study was to describe the instrumentation technique, choice of fusion levels and to report the clinical, radiological and pulmonary function results of selective thoracic fusion using pedicle screw alone instrumentation patients with AIS with a minimal 10-year follow-up.
Materials and methods
Data of all consecutive patients with thoracic AIS, who were operated from posterior with pedicle screw alone constructs in the same institution, with a minimal follow up of 10 years were reviewed. Data were prospectively collected. There were 48 patients (42 females and 6 males) with an average age of 15.37 (11.22–19.48) years at the time of the operation. No patient was lost to follow-up. There were 41 single thoracic curves and 7 double thoracic curves. Double major, triple major, thoracolumbar and lumbar curves were excluded from this study. According to the Lenke classification [9] there were 19 type 1A, 8 type 1B, 14 type 1C, and 2 type 2A, 4 type 2B and 1 type 2C curves. According to the King classification [10] there were 25 King II, 9 King III, 7 King IV and 7 King V curves. Risser stage [11] at the time of surgery was 0 in 3 patients, I in 3 patients, II in 6 patients, III in 12 patients, IV in 23 patients and V in 1 patient. Pulmonary function tests were done preoperatively at 2 and 10 years. Assessment of patient’s satisfaction with SRS-24 questionnaire was done at 2 and 10 years postoperatively. Radiological measurements were taken from radiographs immediately before the operation, 6 weeks, 2 years and 10 years postoperatively. Data assessment and analysis were carried out by two individuals (CS, MF) not involved in the care of the patients.
Surgical technique
All patients were operated by a single surgeon using the same operative technique. Stainless steel side-loading monoaxial pedicle screws and 6.0 mm unit rods were used in all patients. Pedicle screws were not inserted into every single vertebra. A mean of 9.48 (9–13) pedicle screws per patient and a total of 469 pedicle screws in 48 patients were used. This represented an implant density of one screw per vertebra or 50 % density. Four screws in the two most distal vertebrae for distal foundation and two screws in the most proximal vertebra for proximal foundation were routinely used. Apical screws at the concave apical region were inserted and were used for concave side derotation and translation. One or two screws proximal to the apex were used on the convex side for convex rod cantilevering (Figs. 1, 2). The concave rod was first mounted to the distal and proximal foundations. The main deformity correction was carried out by derotating the apical vertebrae individually by pulling and derotating the concave pedicle screws to the mounted concave rod. The side-loading monoaxial apical pedicle screws were essential for this reduction technique. Rod cantilevering on the convex side was performed additionally to push the convexity down. Rod derotation and direct vertebral derotation were not carried out.
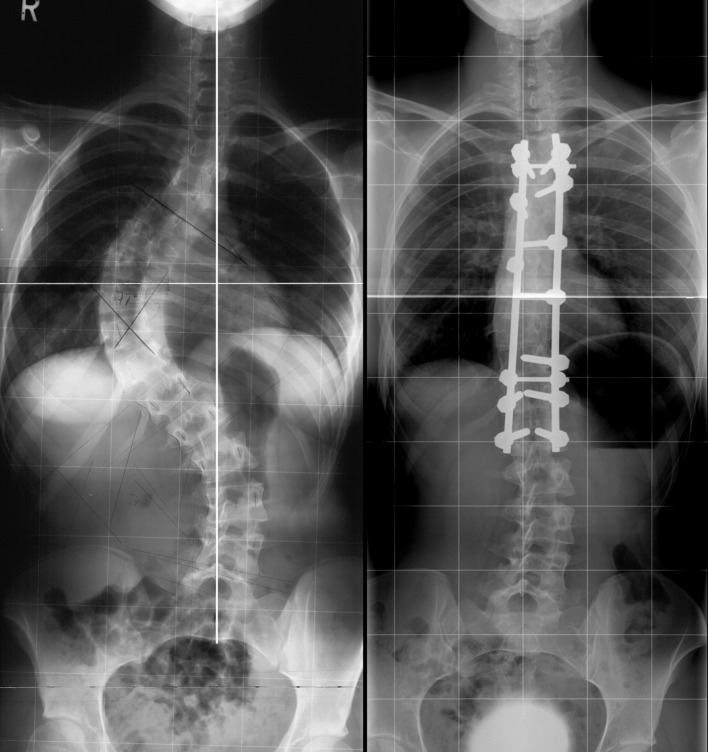
Fig. 1.
If there are two almost parallel end vertebras, the distal one which touches the centre sacral vertical line is chosen as LIV. Preoperative and 10 years postoperative radiographs
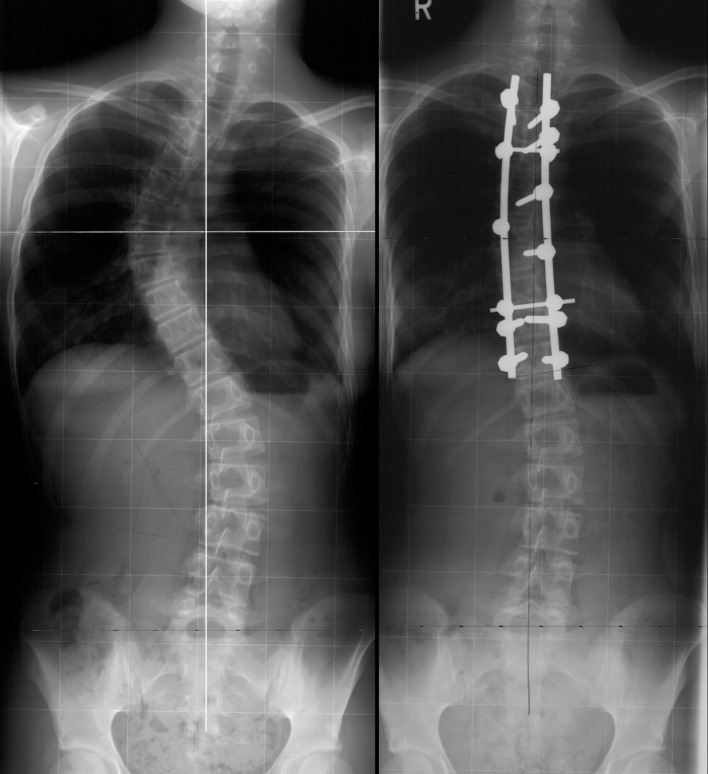
Fig. 2.
Single thoracic curve with lumbar modifier C. Distal end vertebra touches the centre sacral vertical line, and is chosen as LIV. Preoperative and 10 years postoperative radiographs
Determination of fusion levels
The distal end vertebra of the curve (EV) was chosen as the lowest instrumented vertebra (LIV) if the end vertebra touched the centre sacral vertical line (CSVL). When there were two parallel end vertebrae at the distal end of the curve, the lower one was chosen (Fig. 1). One level distal to the end vertebra was chosen if the end vertebra did not touch the CSVL (Fig. 2). The LIV was T11 in 7 patients, T12 in 20 patients, L1 in 10 patients and L2 in 11 patients.
Preoperative supine bending radiographs were used for the selection of the curve to fuse, but they did not influence the choice of the LIV.
The uppermost instrumented vertebra (UIV) was the upper end of the curve. It was T2 in all double thoracic curves. In the single thoracic curves, the UIV was either T3 or T4 in thoracic curves with the apex at T7 or T8, T4 or T5 when the apex was at T8 or T9 and was at T6 when the apex was low at T10 or T11. The UIV was T2 in 7 patients, T3 in 2 patients, T4 in 25 patients, T5 in 12 patients and T6 in 2 patients.
Radiological measurements
Radiological measurements were obtained from whole spine standing anteroposterior and lateral radiographs. Cobb angle, coronal and sagittal spinal balance, apical vertebral rotation (AVR) and apical vertebral translation (AVT), lowest instrumented vertebra tilt (LIVT), distal adjacent disc wedging (ADW), thoracic kyphosis and lumbar lordosis were measured. The coronal and sagittal balances were measured as the distance from the plumb line falling from the centre of C7 to the centre of S1 and the posterior edge of S1, respectively. AVR was measured in degrees using a Perdriolle torsionmeter. AVT was assessed by the distance of the centre of the apical vertebra to the centre sacral vertical line. LIVT was the angle between the lower endplate of the last instrumented vertebra and the horizontal line. ADW was the angle between the lower endplate of the last instrumented vertebra and the upper endplate of the distal adjacent vertebra. LIVT and ADW were defined as positive when the angulations faced the convex side of the instrumented thoracic curve. The thoracic kyphosis was measured from the upper endplate of T4 to the lower endplate of T12 and the lumbar lordosis from the upper endplate of L1 to the upper endplate of S1.
Statistical analysis
Descriptive statistical analyses report data with means, range and standard deviations (SD) where appropriate. Comparison of values at different time points were made either by a Student’s paired two-tailed t-test or a Wilcoxon matched pair test depending on the distribution of the data. Analyses for different subgroups of curves were performed by a Student’s unpaired two-tailed t-test or a Mann–Whitney test. Level of significance was set at p < 0.05. Boxplots depict means with whiskers according to ranges.
Results
Instrumented thoracic curves
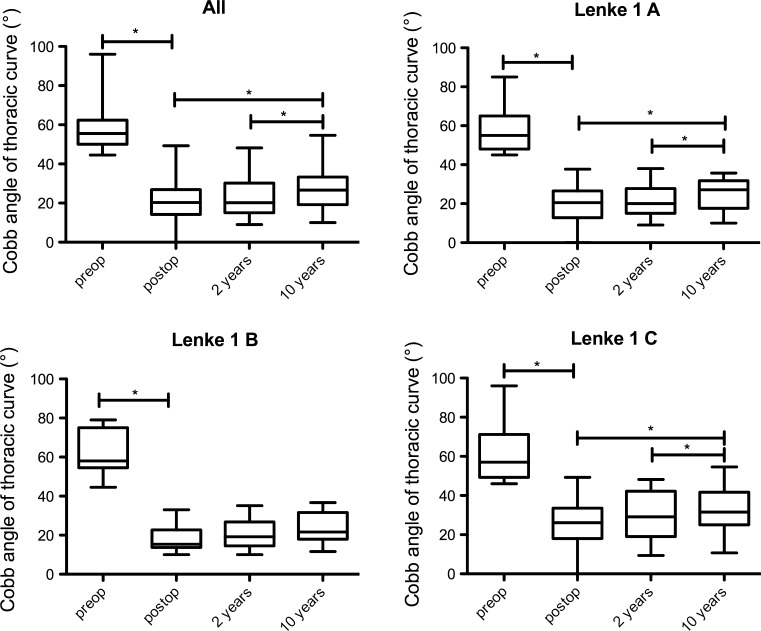
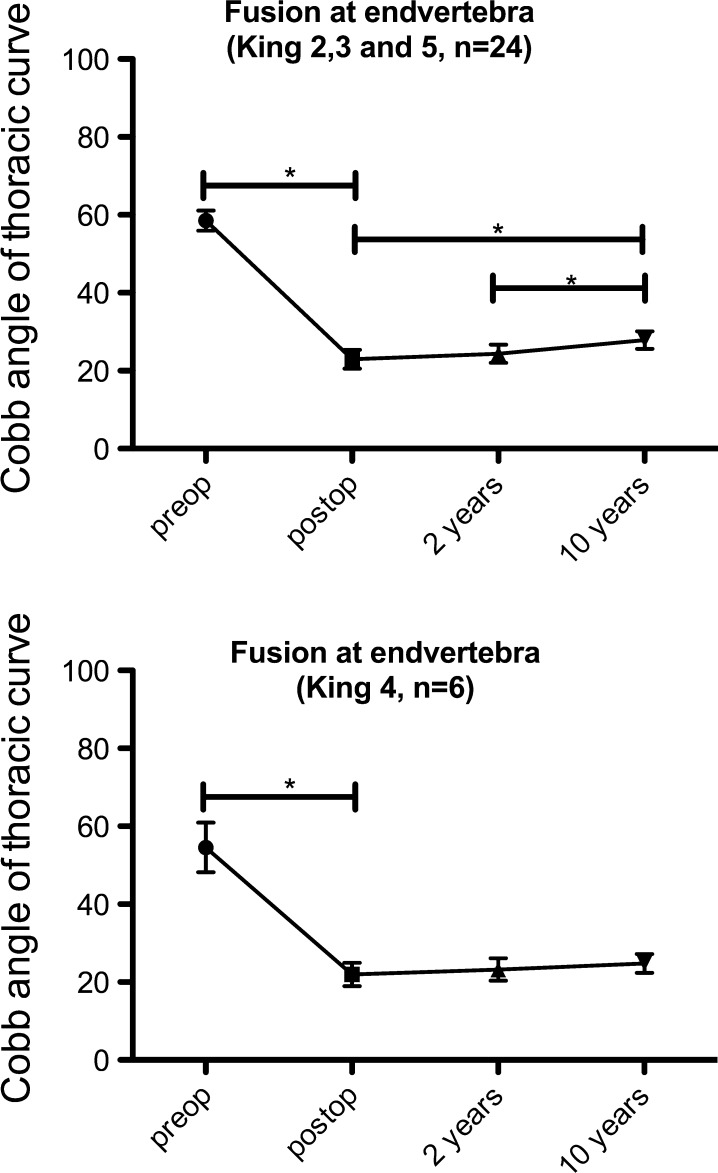
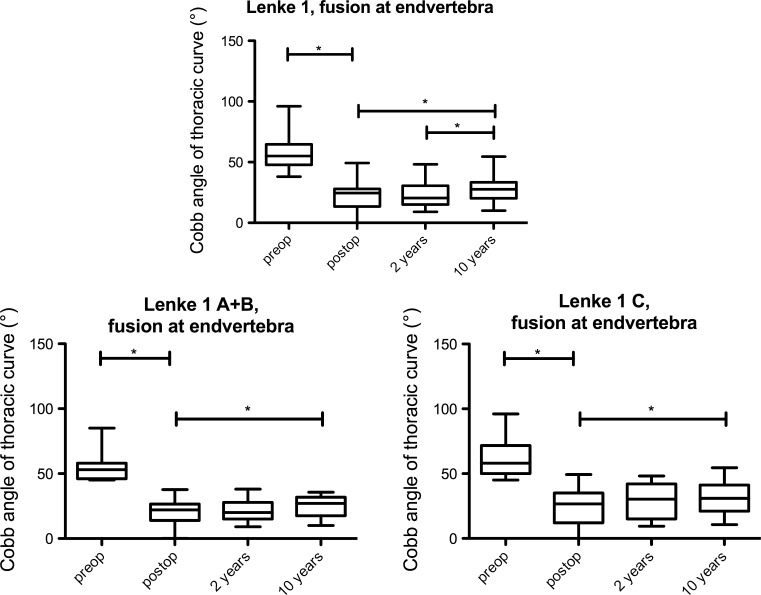
The whole group (n = 48) (Fig. 3).
Fig. 3.
Cobb angle of instrumented thoracic curves of the whole group and different lumbar curves
The main thoracic (MT) curves had a mean preoperative Cobb angle of 58° ± 12° (45°–96°) and a mean flexibility of 47 % (20–60 %). The Cobb angle of main thoracic curves was corrected to 21° ± 10° (63 % correction) (p < 0.05) initially. Cobb angle was at 23° ± 10° (p < 0.05) at 2-year (60 % correction) and 26° ± 10° at 10-year (55 % correction) follow-up (p < 0.05) (Fig. 3). There was an average loss of Cobb angle correction of 5° from 6 weeks to 10 years (p < 0.05) in the whole group.
AVR of the thoracic curves improved 35 % from 24° ± 8° preoperatively to 15° ± 8° (p < 0.05) postoperatively. This remained stable with 16° ± 9° at 2 years and 17° ± 10° at 10 years. The changes from 6 weeks to 10 years were statistically not significant.
AVT of the thoracic curves was 44 ± 20 mm preoperatively in average. It was corrected to 8 ± 10 mm (p < 0.05) postoperatively (82 % correction). AVT was 12 ± 11 mm at 2 years and 15 ± 13 (pPostop-10 years < 0.05) at 10 years. There was an average loss of 3.8 mm at 2 years (p < 0.05) and 6 mm at 10 years (p < 0.05), which resulted in 67 % correction of AVT at 10 years.
Different lumbar curves
The average postoperative correction of thoracic curves was 64 % in patients with lumbar modifier A, 67 % in patients with modifier B and 56 % in patients with modifier C. The less correction of the main thoracic curves in the patients with lumbar modifier C was explained by the presence of a significant amount of compensatory lumbar curve.
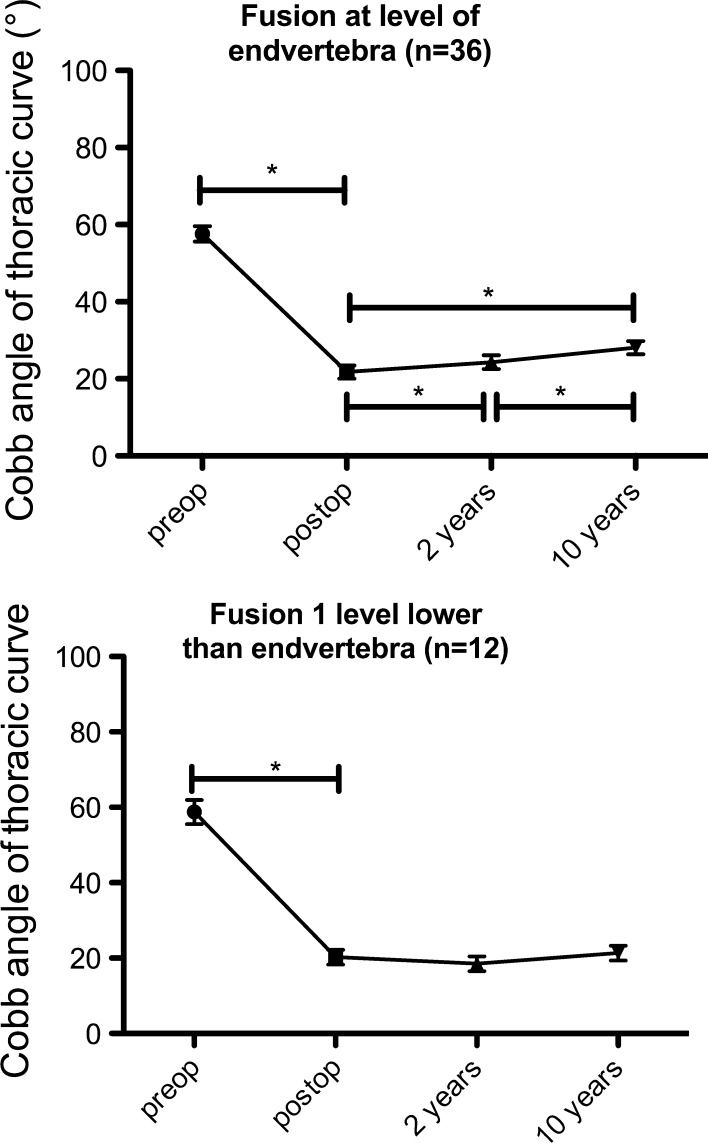
Different lowest instrumented vertebra (Fig. 4)
Fig. 4.
Cobb angle of instrumented thoracic curves in respect to different levels of last instrumented vertebra (LIV)
The patients were divided into two groups depending on the LIV. In the first group of patients (n = 36) the LIV was the end vertebra (LIV = EV) and in the second group (n = 12) the LIV was one distal to the end vertebra (LIV = EV + 1). The LIV = EV group showed a slight loss of correction in thoracic curve in comparison with the LIV = EV + 1 group (Fig. 4). The patients in the LIV = EV group had a loss of correction of 6° from postoperative 22° ± 10°–28° ± 10° (p < 0.05) whilst those in the LIV = EV + 1 group remained stable at 21° ± 7° over 10 years. In the LIV = EV group this loss of correction was similar when subdivided by the lumbar modifier A (22° ± 10° at 6 weeks to 27° ± 7° at 10 years), B (18° ± 6° to 24° ± 8°) and C (25 ± 13° to 32 ± 13°). The results of AVR and AVT did not show any significant difference between the LIV = EV and LIV = EV + 1 groups.
Long thoracic curves (King IV) (n = 7)
The long thoracic curves with L4 vertebra tilting into the curve need special consideration, even though they are type 1A according to the Lenke classification. In our series there were seven King IV patients. Six patients were fused to LIV = EV, one patient to LIV = EV + 1 in accordance with the choice of fusion levels described above. The patients with LIV = EV (n = 6) had less initial correction of 59 % when compared with the patient (n = 1) with LIV = EV + 1 who had a correction of 85 % at 6 weeks. The loss of correction in the whole group was 7 % at 10 years. AVT was 63.0 ± 21 mm preoperatively, 17.2 ± 9 mm at 6 weeks, 19.2 ± 9 mm at 2 years and 24.5 ± 6 mm at 10 years (Fig. 5).
Fig. 5.
Subdivision of the thoracic curves according to the King classification of patients where LIV is end vertebra, after exclusion of those patients with implant removal. The long thoracic type King IV curves did not show any difference compared with the other types
Patients in whom implants were removed (n = 6)
A complete implant removal was necessary in 6 patients in average 3.7 (1.1–7.9) years after the index operation due to late-onset low-grade implant-related infection caused by Propionibacterium acnes. In these patients the initial correction of 70 % (from 56° ± 6° to 17 ± 3°) was lost to 42 % with 33° ± 10° at 10 years, despite intraoperative evidence of bony fusion at the time of implant removal. The AVT increased by tendency from postoperative 5.8 ± 9.5 to 20.4 ± 16.2 mm. Although there was loss in Cobb angle correction of average 15° over the 10-year follow-up period in this patient group, the AVR remained unchanged indicating that the loss of correction after implant removal took place only in the coronal plane, not involving the rotational axial plane. This phenomenon was presumably due to gradual bending of the immature fusion mass in the coronal plane. The aetiology and modalities of treatment in patients with late implant-associated infection with P. acnes have already been reported and thoroughly discussed [12, 13].
Patients without implant removal (n = 42)
Excluding the above patients with implant removal and examining only the data of the patients who had the implant in situ to the last follow-up, the Cobb angle correction of the instrumented thoracic scoliosis was initially 63 % from 58° ± 12° to 21° ± 10°, did not change at 2 years and was 55 % at 10 years with 26° ± 10°, with a loss of correction of 4° in Cobb angle or 7 %.
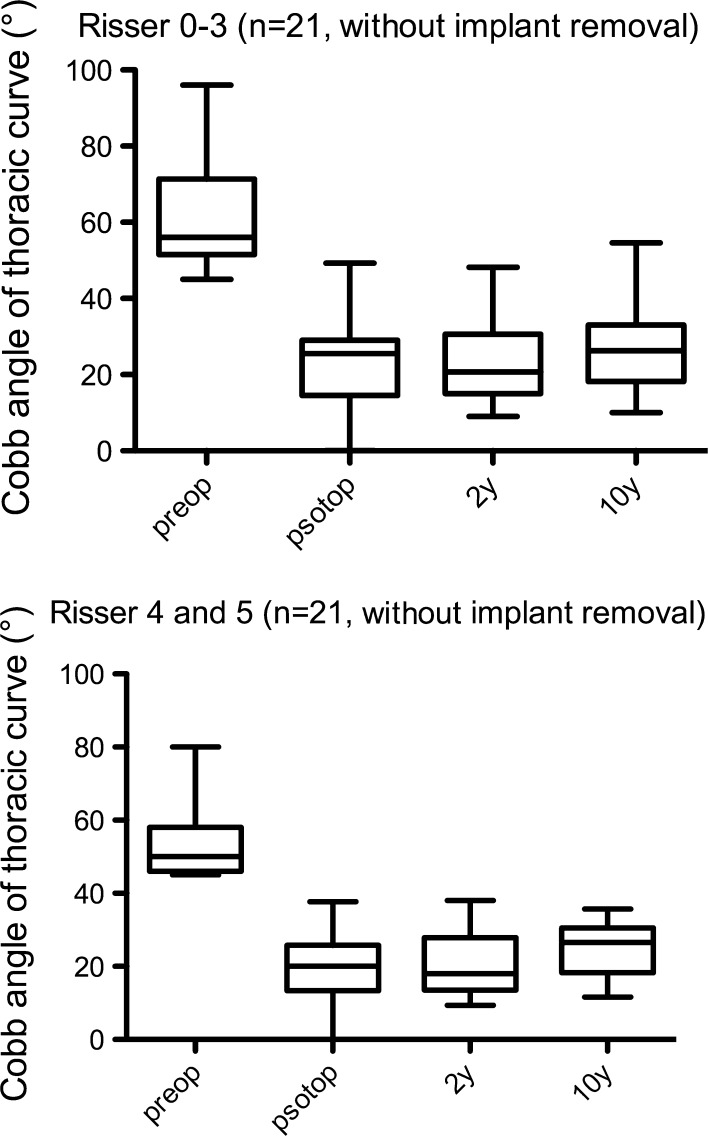
Of the 42 patients, 21 patients had Risser stage 0–III and 21 patients had Risser stage IV at the time of the index operation. There was no relevant difference in loss of correction between these two patient groups (Fig. 6).
Fig. 6.
Changes in thoracic curves depending on Risser stage at the time of operation
All the six patients in whom the implants were removed belonged to the LIV = EV group. To remove the confounding effect of implant removal in this group of patients we analysed the remaining 30 patients of the LIV = EV group. There was a minimal loss of correction from 2 to 10 years in the instrumented thoracic curves (Fig. 7).
Fig. 7.
Results of thoracic curve of patients where LIV is end vertebra, after excluding those who had implant removed (n = 30)
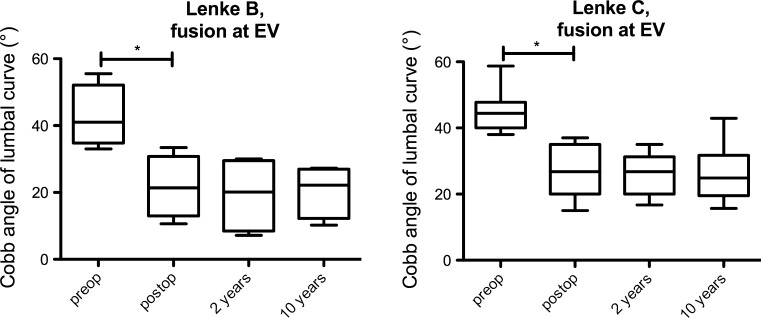
Non-instrumented lumbar curve
In King III or Lenke type 1A patients the lumbar curves were not analyzed, as the lumbar curves in such patients did not cross the midline and were produced only because of the tilt of the distal end vertebra of the thoracic curve.
In the rest of the patients (n = 48) there was a spontaneous correction of 47 % of the lumbar curves from the average preoperative 40° ± 8° (25°–59°) to 22° ± 8° at 6 weeks. There was no loss of correction of lumbar curves with 21° ± 8° at 2 years and 22° ± 8° at 10 years (p > 0.05). This was also true for the patients in LIV = EV group as well as the patients in LIV = EV + 1 group. Only three patients with lumbar modifier B and one patient with lumbar modifier C had LIV = EV + 1. All the rest of patients with lumbar B and C modifiers (n = 23) had LIV = EV. The spontaneous correction of lumbar curves in these patients is shown in Fig. 8. There was no significant loss of correction at 10 years.
Fig. 8.
Cobb angle of non-instrumented lumbar curves of patients where LIV is end vertebra subdivided by lumbar modifiers B and C, after excluding those who had implant removed (n = 23)
There was, however, some loss of correction of lumbar curves from 19° ± 2° postoperatively to 25° ± 6° at 10 years (p < 0.05) in the patients who needed implant removal (n = 6).
Spinal balance, thoracic kyphosis and lumbar lordosis (Table 1)
Table 1.
Spinal balance, Kyphosis and Lordosis
| Preoperatively | 6 weeks postop. | 2 years postop. | 10 years postop. | p (6 weeks–10 years) | |
|---|---|---|---|---|---|
| Coronal balance | 15 ± 12 mm | 12 ± 10 mm | 14 ± 10 mm | 13 ± 9 mm | 0.359 |
| Sagittal balance | 8 ± 28 mm | 11 ± 30 mm | 3 ± 26 mm | –4 ± 27 mm | <0.05 |
| Kyphosis | 28° ± 13° | 28° ± 10° | 30° ± 12° | 33° ± 11° | <0.05 |
| Lordosis | 53° ± 15° | 56° ± 12° | 55° ± 14° | 59° ± 13° | <0.05 |
The coronal balance did not change significantly immediately after the operation or over the observation time of 10 years (p > 0.05). In the sagittal plane the C7 tended to move slightly posterior during the 10-year follow-up period.
The preoperative average thoracic kyphosis of 28° ± 13° did not change initially after the operation, but thoracic kyphosis had a tendency to increase during the follow-up period with 30° ± 12° at 5 years and 33° ± 11° at 10 years (p < 0.05). The preoperative lumbar lordosis of 53° ± 15° also did not change initially, but increased to 59° ± 13° at 10 years (p < 0.05).
Lowest instrumented vertebral tilt and distal adjacent disc wedging
The lowest instrumented vertebra and the adjacent motion segment showed satisfactory and sustained correction in the whole group. Preoperative LIVT of 23° ± 8° was corrected to 5° ± 5° and did not show any relevant change with 6° ± 5° at 2 years and 7° ± 5° at 10 years (pPostop-10years = 0.016).
ADW decreased from a preoperative angle of 6° ± 3° to −2° ± 4° postoperatively and remained unchanged with −2° ± 4° at 2 years and −2° ± 4° (pPostop-10 years = 0.731) at 10 years.
Clinical rib hump
The average clinical rip hump was 12° (8°–18°) preoperatively. This improved to 8° (5°–12°) which represented a 37 % of spontaneous improvement.
Pulmonary function
The FVC % was 74 ± 20 % preoperatively and did not change postoperatively at 2 years (74 ± 11 %) or at 10 years (75 ± 10 %).
SRS-24 questionnaire
Subjective satisfaction of the patient was assessed by SRS-24 questionnaire. There were 93 ± 18 points (of maximal possible 120 points) at the 2-year and 95 ± 22 points at the 10-year follow-up in the whole group. The domain concerning pain did not change from 2 to 10 years with 28 ± 7 to 29 ± 7 points, respectively.
There was no significant difference of 10-year SRS-24 scores between the two groups of patients with the LIV = EV (96 ± 23 points) and LIV = EV + 1 (94 ± 19 points) (p = 0.660).
The patients who had the spinal implant removed for late infection also reported good subjective outcome with a score of 99 ± 15 points at 10 years.
Complications
There were no complications other than the low-grade late implant-associated infections. There were neither acute infections, nor neurological complications or pedicle-screw-related complications.
Discussion
Long-term clinical, radiological and pulmonary function results of patients with thoracic AIS corrected with pedicle screw alone implants are presented. The choice of fusion levels, in particular the choice of the LIV and the method of instrumentation are described in detail. An initial Cobb angle correction of 63 % of the instrumented thoracic curves was achieved. There was some loss of correction during the 10-year follow-up period and the correction was 55 % at 10 years. Other authors have reported some loss of correction in series of 3- to 5-year follow-up [7, 8] in agreement with the here presented results. Loss of correction, spinal balance and other parameters were not different independent of the character of lumbar compensatory curve. The correction of the thoracic curve was less in the patients with a significant lumbar curve (modifier C) in comparison with other patients with less pronounced lumbar curves (modifier A and B). Some expressed concern of decompensation in the selective thoracic fusion in the presence of a significant lumbar curve [14]. We did not see decompensation of spinal balance or loss of correction of lumbar curves in our patients with lumbar modifier C. The non-instrumented lumbar curves improved 47 % in patients with lumbar curve type B and C. Lumbar curves did not show any loss of correction even though some loss of correction in the instrumented thoracic curves was measured during 10-year follow-up. We were not able to find an explanation for this observation except the assumption of measuring errors. Our results show that the King type II or Lenke type 1 and 2 patients with a lumbar modifier C can safely be treated by selective thoracic fusion with distal fusion to EV or EV + 1. Extending the fusion to the region of lumbar compensatory curve is not necessary.
As there were only seven patients with King IV type curves, a statistical analysis was not possible. However, it seemed that the distal fusion to EV + 1 resulted in a better correction in these patients.
Although the patients in the LIV = EV group tend to have some loss of correction in comparison with those in the LIV = EV + 1 group, the difference was small and was not noticeable clinically as documented by the results of SRS-24 questionnaire. Further, this loss of correction was only in the coronal plane. There was no measurable loss in the axial plane as there was no loss in AVR. We did not perform direct vertebral rotation. Instead, we derotated the apical vertebrae individually by pulling and derotating the concave apex to the mounted concave rod. With this technique a 35 % correction of AVR was achieved without loss of correction up to 10-year follow-up. The spontaneous improvement of clinical rib hump of 37 % was achieved with this method.
There were some reports [15] concerning the changes in wedging of the adjacent disc or tilt of the last instrumented vertebra. A good correction of ADW and LIVT without loss of correction up to 10 years was achieved in our patients by means of the present method of instrumentation and the determination of the LIV. Long-term lack of changes in ADW and LIVT also suggested against any significant loss of correction in coronal plane as well as any development of significant degenerative changes in the distal adjacent discs. In summary, all other parameters remained stable except some loss of correction in Cobb angle of instrumented thoracic curves in the long term.
Some reports on all pedicle screws constructs described the use of screws on every vertebra in the fusion region [7, 8]. This is not necessary in our experience. Using only 9.48 (8–12) pedicle screws per patient, which means an implant density of 1 screw per vertebra, or a 50 % implant density, a comparable correction [7, 8] was achieved. This correction was sufficient to produce a satisfactory long-term subjective outcome.
The thoracic kyphosis was not influenced by posterior instrumentation initially after the operation with posterior pedicle screw instrumentation. This is in accordance with a previous report [6]. It tended to increase for about 5° during the 10-year follow-up period. In contrast to others [16] we did not have any proximal junctional kyphosis in our patients.
In accordance with the pertinent literature [17, 18] our patients with AIS had less than normal pulmonary function (74 % of predicted forced vital capacity) preoperatively. But contrary to K.Pehrsson et al. [17] who reported an improvement of % FVC from 67 % preoperatively to 73 % immediate postoperatively, the pulmonary function in our patients remained unchanged up to the last follow-up. In our patients the correction of thoracic scoliosis was not associated with an improvement of FVC if adjusted to age and weight. There was also no decline in pulmonary function during the 10-year follow-up period.
Other than late low-grade implant-associated infections there were no complications in our patients. There were no acute infections. In particular, there were no complications related to thoracic pedicle screws. The phenomenon of late infections in association with the use of stainless steel implants has been reported elsewhere [12, 13, 19]. Since we changed from stainless steel to titanium implants we did not see this complication up to now.
Conclusion
The correction of thoracic AIS with thoracic pedicle screw instrumentation is a safe procedure. Insertion of screws in every single vertebra is not necessary as a satisfactory multidimensional radiological correction and a high long-term patient’s satisfaction can be achieved with a low implant density of average 1 screw per vertebra (50 %). The LIV can be either the distal end vertebra or one below the distal end vertebra of the thoracic curve, depending on the position of the end vertebra to the centre sacral line. A selective thoracic curve fusion in patients with lumbar modifier C can safely be done resulting in a stable long-term correction of non-instrumented lumbar curves. The preoperative pulmonary function does not change during the 10-year follow-up period.
Conflict of interest
None of the authors has any potential conflict of interest.
References
- 1.Kepler CK, Meredith DS, Green DW, Widmann RF. Long-term outcomes after posterior spine fusion for adolescent idiopathic scoliosis. Curr Opin Pediatr. 2012;24:68–75. doi: 10.1097/MOP.0b013e32834ec982. [DOI] [PubMed] [Google Scholar]
- 2.Papin P, Labelle H, Delorme S, Aubin CE, de Guise JA, Dansereau J. Long-term three-dimensional changes of the spine after posterior spinal instrumentation and fusion in adolescent idiopathic scoliosis. Eur Spine J. 1999;8:16–21. doi: 10.1007/s005860050121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim YJ, Lenke LG, Cho SK, Bridwell KH, Sides B, Blanke K. Comparative analysis of pedicle screw versus hook instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2004;29:2040–2048. doi: 10.1097/01.brs.0000138268.12324.1a. [DOI] [PubMed] [Google Scholar]
- 4.Harrington PR. Treatment of scoliosis. Correction and internal fixation by spine instrumentation. J Bone Joint Surg Am. 1962;44-A:591–610. [PubMed] [Google Scholar]
- 5.Cotrel Y, Dubousset J. A new technic for segmental spinal osteosynthesis using the posterior approach. Rev Chir Orthop Reparatrice Appar Mot. 1984;70:489–494. [PubMed] [Google Scholar]
- 6.Min K, Waelchli B, Hahn F. Primary thoracoplasty and pedicle screw instrumentation in thoracic idiopathic scoliosis. Eur Spine J. 2005;14:777–782. doi: 10.1007/s00586-005-0977-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Suk SI, Lee SM, Chung ER, Kim JH, Kim SS. Selective thoracic fusion with segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis: more than 5-year follow-up. Spine (Phila Pa 1976) 2005;30:1602–1609. doi: 10.1097/01.brs.0000169452.50705.61. [DOI] [PubMed] [Google Scholar]
- 8.Lehman RA, Jr, Lenke LG, Keeler KA, Kim YJ, Buchowski JM, Cheh G, Kuhns CA, Bridwell KH. Operative treatment of adolescent idiopathic scoliosis with posterior pedicle screw-only constructs: minimum three-year follow-up of one hundred fourteen cases. Spine (Phila Pa 1976) 2008;33:1598–1604. doi: 10.1097/BRS.0b013e318178872a. [DOI] [PubMed] [Google Scholar]
- 9.Lenke LG, Betz RR, Harms J, Bridwell KH, Clements DH, Lowe TG, Blanke K. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am. 2001;83-A:1169–1181. [PubMed] [Google Scholar]
- 10.King HA, Moe JH, Bradford DS, Winter RB. The selection fusion levels in thoracic idiopathic scoliosis. J Bone Joint Surg Am. 1983;65:1302–1313. [PubMed] [Google Scholar]
- 11.Risser JC. The Iliac apophysis: an invaluable sign in the management of scoliosis. Clin Orthop. 1958;11:111–119. [PubMed] [Google Scholar]
- 12.Hahn F, Zbinden R, Min K. Late implant infections caused by Propionibacterium acnes in scoliosis surgery. Eur Spine J. 2005;14:783–788. doi: 10.1007/s00586-004-0854-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Farshad M, Sdzuy C, Min K (2012) Late implant removal after posterior correction of thoracic AIS with pedicle screw instrumentation—A matched case control study with 10 year follow-up. Presented in SRS 47th annual meeting, Chicago, IL, USA [DOI] [PubMed]
- 14.Lenke LG, Bridwell KH, Baldus C, Blanke K. Preventing decompensation in King type II curves treated with Cotrel–Dubousset instrumentation. Strict guidelines for selective thoracic fusion. Spine (Phila Pa 1976) 1992;17:S274–281. doi: 10.1097/00007632-199208001-00011. [DOI] [PubMed] [Google Scholar]
- 15.Erickson MA, Baulesh DM. Lowest instrumented vertebra selection in AIS. J Pediatr Orthop. 2011;31:S69–76. doi: 10.1097/BPO.0b013e318202bfcd. [DOI] [PubMed] [Google Scholar]
- 16.Kim YJ, Bridwell KH, Lenke LG, Kim J, Cho SK. Proximal junctional kyphosis in adolescent idiopathic scoliosis following segmental posterior spinal instrumentation and fusion: minimum 5-year follow-up. Spine (Phila Pa 1976) 2005;30:2045–2050. doi: 10.1097/01.brs.0000179084.45839.ad. [DOI] [PubMed] [Google Scholar]
- 17.Pehrsson K, Danielsson A, Nachemson A. Pulmonary function in adolescent idiopathic scoliosis: a 25 year follow up after surgery or start of brace treatment. Thorax. 2001;56:388–393. doi: 10.1136/thorax.56.5.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kearon C, Viviani GR, Kirkley A, Killian KJ. Factors determining pulmonary function in adolescent idiopathic thoracic scoliosis. Am Rev Respir Dis. 1993;148:288–294. doi: 10.1164/ajrccm/148.2.288. [DOI] [PubMed] [Google Scholar]
- 19.Di Silvestre M, Bakaloudis G, Lolli F, Giacomini S. Late-developing infection following posterior fusion for adolescent idiopathic scoliosis. Eur Spine J. 2011;20(Suppl 1):S121–127. doi: 10.1007/s00586-011-1754-1. [DOI] [PMC free article] [PubMed] [Google Scholar]