Abstract
Purpose
The purpose of the present study was to assess whether current cancer follow-up care practices meet the needs of young adult cancer survivors in Canada.
Methods
This qualitative study used a constructivist grounded theory framework to analyze telephone interviews with cancer survivors from across Canada diagnosed between the ages of 18 and 39 years. The focus was specifically on cancer follow-up care (cfc).
Results
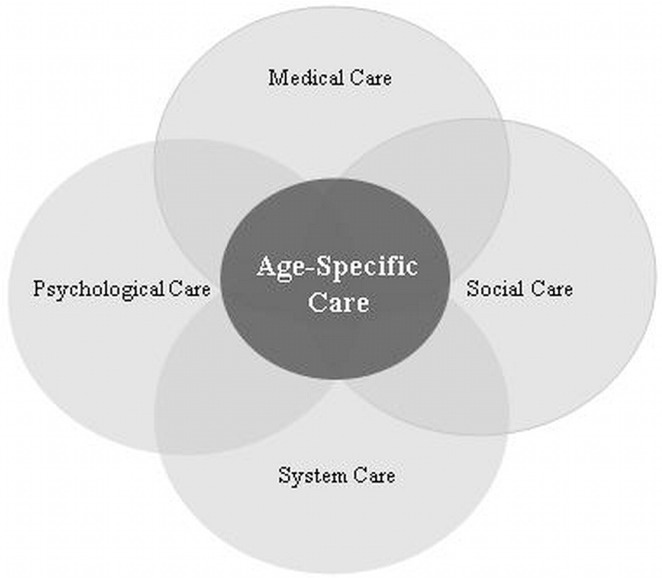
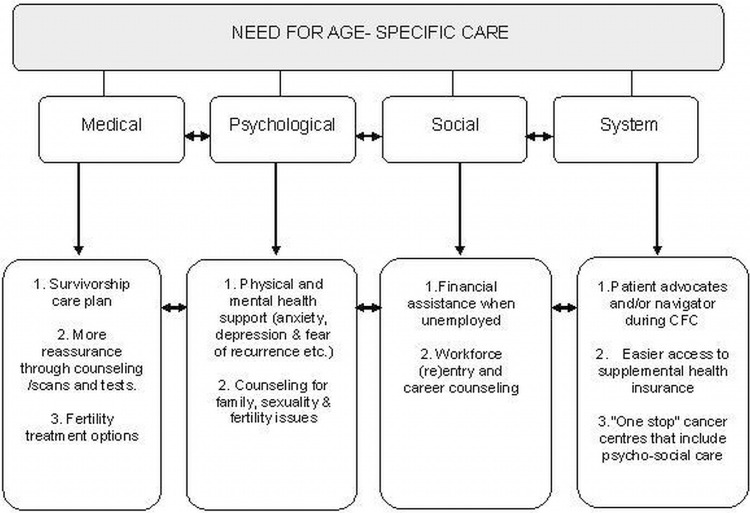
Interviews were conducted with 55 participants, and 53 interviews were used for the analysis. The overall theme that emerged from the data was the lack of age-specific cfc. Some of the subthemes that emerged were the absence or inadequacy of fertility and infertility treatment options; of psychological services such as family, couples, and sexuality counseling; of social supports such as assistance with entry or re-entry into the education system or workplace; of access to supplemental health insurance; and of survivorship care plans. Based on the data resulting from the interviews, we developed a conceptual model of young-adult cfc incorporating the major themes and subthemes that emerged from our study. The proposed model aims to ensure a more age-appropriate and comprehensive approach to cfc for this group of cancer patients.
Conclusions
Current Canadian cfc practices are inadequate and do not provide comprehensive care for young adult cancer survivors in Canada. The conceptual model presented here aims to ensure a more comprehensive approach to cfc that meets the needs of this unique cancer population and reduces further possible physical, psychological, or social cancer sequelae.
Keywords: Young adult cancer, survivorship, qualitative study, follow-up care, psychosocial issues
1. INTRODUCTION
In Canada, cancer is the major cause of early death among young adult women and the third-ranking cause of death among young men between the ages of 20 and 441. Although the mortality rate among young adults with cancer is significant, most survive to live long lives2,3. From the limited understanding available to date, it is apparent that young adults diagnosed with cancer are presented with challenges of fertility, sexuality, education, work, and relationships at a time when their peers are progressing along the road to independence, productive careers, and families4–8,a.
For researchers, the cancer journey has some distinct points along the way, as outlined by Cancer Care Ontario9; however, for patients, the distinctions are often less clear. The most important points in the cancer journey from the patient’s perspective are acute care (including diagnosis) and follow-up care5. In the present study, we focus exclusively on the survivorship phase—and particularly on the cancer follow-up care (cfc) experiences of young adult cancer survivors in Canada.
To contextualize the Canadian health care system, it is important to understand that the delivery of health care in Canada is a matter of provincial jurisdiction, and that the delivery of health care services varies greatly from region to region10. Currently, there is no comprehensive national model of cfc in Canada. In some jurisdictions, cfc includes physical (medical) and psychosocial care; in other cases, cfc includes only physical check-ups at given intervals. Many cancer centres in Canada also lack resources specific to young adults with cancer11. The lack of a comprehensive cfc approach for young adult cancer survivors may be a result of gaps in knowledge about the cfc needs of this unique age group12.
Several studies have reported on the experiences of young adult cancer patients, but most have focused on slightly different populations (children diagnosed with cancer who are now young adults); on different phases in the cancer journey (treatment); or on cancer issues in general. One such study from the United States reported that older young adults expressed a need for improved age-appropriate information and support (such as fertility options and psychological counseling) and that younger respondents wanted treatment options that least interfered with their lifestyle13. General health and wellbeing, sexuality, and a lack of social support have been cited as important issues for young adults, but are often poorly understood during cfc in this population14. Other studies provide evidence supporting the benefits of social support, counselling, and therapeutic intervention for the emotional, functional, and symptom-related adjustments associated with cancer survival15,16.
Thompson et al. conducted focus groups with young adult cancer survivors to discuss cfc and identified 3 categories of concerns: transition to follow-up care, psychosocial issues, and social issues17. Participants reported that they felt unprepared for the transition from acute treatment to follow-up care and were not sure who could best help them with the physical, emotional, and social issues that later arose from the lingering effects of treatment. Thompson et al. proposed a model of cfc that includes a transitional care plan, monitoring for recurrence and late effects, and assistance with getting back to “normal”17. Other authors have identified the need for financial assistance for young adult cancer survivors18,19.
The goals of the present study were to qualitatively document the experience of cfc by young adults in Canada and to document the gaps in cfc.
2. METHODS
2.1. Definitions
The term “young adult” is not uniquely defined in the context of cancer20. Many studies of young people with cancer have included adolescents, and many have used age ranges between 14 and 39 years. However, the upper age limit defining young adulthood has been greatly debated and ranges from 29 to 49 years20,21. A roundtable discussion with senior oncology researchers resulted in a decision on an upper age limit of 39 years22. For the present study, we set the age range at 18–39 years, focusing exclusively on young adults. The rationale for this definition is a combination of factors that are both pathophysiologic (nonepithelial vs. epithelial cancers) and psychosocial. The age of 18 marks the transition from high school student to a person who may leave home to study or work. Throughout their 30s, many young adults are searching for emotional and financial stability while trying to establish secure intimate relationships1,23. The major task for young adults between the ages of 18 and 39 is to establish independence, and this stage in life is an important context for their cfc experiences1.
Cancer follow-up care is also difficult to define. No generally accepted definition exists. To some extent, cfc is cancer-specific—for example, when focusing on early detection of a recurrence, the presentation of symptoms differs greatly depending on the cancer24. Cancer follow-up care is “not just a single event with a certain end but an enduring condition characterized by ongoing uncertainty, potentially delayed or late effects of the disease or treatment, and concurrent psycho-social issues”25. Comprehensive cancer care, according to the Canadian Strategy for Cancer Control, should include both biomedical and non-biomedical care26. Cancer follow-up care can be characterized as short- (1–3 years), medium- (up to 5 years), and long-term (5–10 years)27,28. In the present qualitative study, we focused on short- and mediumterm cfc for cancer survivors who are not palliative.
2.2. Participants
The study recruited young adults diagnosed with any kind of cancer between the ages of 18 and 39 years. Participants were required to have the ability to speak either English or French and to give consent. They received a $20 gift certificate for their participation. The recruitment strategy included posts on social networking sites (for example, Facebook), online classified websites (for example, Kijiji), newsletters and online message boards at cancer advocacy groups (for example, Young Adult Cancer Canada) and cancer-specific agencies (for example, Thyroid Cancer Canada), posters in various oncology clinics, and articles and interviews in newspapers and other media.
Once a potential participant contacted us by telephone (toll-free), e-mail, or Facebook to indicate a willingness to engage in the study, that individual was screened for eligibility according to our inclusion criteria. The screening was conducted using 5 questions asking for location, current age and age at diagnosis, sex (implied), and language of choice. A consent form was forwarded to eligible individuals, and a telephone interview date was set. Before the telephone interview commenced, the participant and the interviewer discussed the consent form to ensure that the participant was fully aware of the study procedures, risks, and benefits. The study was reviewed and approved by the research ethics boards of Dalhousie University (no. 2009–2098) and Memorial University (no. 10–46).
2.3. Data Collection
Qualitative interviews were conducted using openended questions. The first two questions were designed to make the participants feel comfortable and to elicit their stories. Question 3 asked about current cfc, and questions 4–9 asked about broad cfc issues that could be characterized as physical, psychological, relationship, and social. Questions 10 and 11 related to experiences and satisfaction with the participants’ current cfc and their recommendations for improvement. After the interview, sociodemographic information was collected to create a participant profile.
We aimed to interview a diverse sample in a homogeneous population (young adult cancer survivors) using age, location, and sex as prescreening questions. This process is called theoretical sampling29,30. Theoretical sampling was constrained by the parameters of the self-referral nature of the recruitment strategy31. Two research assistants conducted all the interviews. The interviewees and the interviewers were sex-paired. All interviews were transcribed verbatim and proofed for accuracy.
2.4. Analysis
We used a constructivist grounded theory approach to analyze the data. Constructivism is a research paradigm that rejects the notion of an objective reality, instead viewing realities as a social construct. Data are narrative constructions and may have multiple meanings. Researchers have to go beyond the “surface” of the data to find meaning and values32. Constructivist grounded theory methods are often used in health research when the voice of the participants is important33,34. Interviews were conducted and transcribed verbatim concurrently with the analysis, consistent with the constructivist grounded theory methodology. Four team members (2 co-investigators and 2 research assistants) independently read the same three transcripts [representing diversity based on age, cancer type, and residence (urban or rural)] and developed a coding scheme during a 2-day meeting. Using the constant-comparison method and continued discussions among the team members, the rest of the transcripts were each coded line-by-line by a single researcher to ensure consistency30. Throughout the coding process, the team held regular formal and informal meetings to discuss codes if new issues emerged. If need be, the coding scheme was adjusted. The coding process was facilitated through use of the qualitative data analysis program NVivo 9 (QSR International, Doncaster, Australia). The sociodemographic information was analyzed using the statistical data analysis program SPSS (version 15: SPSS, Chicago, IL, USA).
3. RESULTS
From across Canada, 67 young adult cancer survivors contacted us about the study. Of the 67, 55 participated in telephone interviews. The remaining 12 could not be reached or declined to participate after the initial contact. On average, the interviews lasted 45–90 minutes; interviews with female participants tended to be twice a long as those with male participants. After approximately 35 interviews, saturation was reached (the interviewers did not hear any new information); however, recruiting continued to ensure a diverse sample of participants based on location and sex. The mean age of the participants at diagnosis was 29 years, three quarters were female, and one quarter lived in a rural area with a population less than 10,000. Five participants (9%) self-identified as visible minorities. Just fewer than half (47%) had either thyroid or breast cancer (for more details, see Table i). Two participants did not meet the inclusion criteria: at time of diagnosis, one was older than 39 (age 44) and the other was younger than 18 (age 14). Those participants were removed from the analysis, even though their experiences were similar to those of the remaining 53 participants. Most participants were 1–5 years post diagnosis.
TABLE I.
Characteristics of the study participants
| Variable | Value |
|---|---|
| Participants (n) | 53 |
| Age | |
| Current (years) | |
| Mean | 32±6.43 |
| Range | 20–44 |
| At diagnosis (years) | |
| Mean | 29±5.93 |
| Range | 18–39 |
| <25 Years (n) | 13 |
| ≥25 Years (n) | 40 |
| Years since diagnosis [n (%)] | |
| <1 | 1 (2) |
| 1 | 17 (32) |
| 2 | 9 (17) |
| 3 | 6 (11) |
| 4 | 6 (11) |
| 5 | 8 (15) |
| >5 | 6 (11) |
| Sex [n (%)] | |
| Female | 39 (74) |
| Male | 14 (26) |
| Cancer type [n (%)] | |
| Breast | 13 (25) |
| Thyroid | 12 (23) |
| Non-Hodgkin lymphoma | 8 (15) |
| Hodgkin lymphoma | 6 (11) |
| Testicular | 4 (7) |
| Other | 10 (19) |
| Geographic location [n (%)] | |
| Eastern Canada | 34 (64) |
| Central Canada | 16 (30) |
| Western Canada | 3 (6) |
| Residence in rural areaa [n (%)] | 13 (25) |
| In a relationshipb [n (%)] | 32 (60) |
| Have children [n (%)] | 24 (45) |
| Completed postsecondary educationc | 38 (72) |
| Employment status [n (%)] | |
| Working | |
| Full-time | 22 (42) |
| Part-time/casual | 9 (17) |
| Not workingd | 10 (19) |
| ltd/government assistance | 5 (9) |
| Student (full- or part-time) | 7 (13) |
| Supplemental private health insurance (currently)e | 42 (79) |
| Annual family income | |
| <$30,000 | 7 (13) |
| $30,001–$50,000 | 7 (13) |
| $50,001–$70,000 | 7 (13) |
| $70,001+ | 23 (43) |
| Chose not to answer/did not know | 9 (17) |
Population less than 10,000.
Married or common-law partner.
Community college diploma, undergraduate or graduate university degree.
Unemployed, homemaker, unpaid sick leave.
Includes parental/spousal supplemental health insurance coverage.
ltd= long-term disability.
3.1. Themes
The overarching theme that emerged from the interviews was a desire for age-specific interventions to address the follow-up care needs of this population. In addition, four subthemes (medical, psychological, social, and system needs) were identified. Table ii provides illustrative quotes summarizing the overall theme and the subthemes.
TABLE II.
Illustrative quotations from participants of their cancer follow-up care needs
| Theme | Sample statements |
|---|---|
| Age-specific care needs | There weren’t a lot of options for young adults when I was first going through it, [and] so that’s one of my major frustrations, actually. And for a lot of people that I speak with is that they can’t find the information. It’s not easily accessible.... It’s not handed out to you at the cancer centres. It’s all older-age related, [ and] so it’s not helpful at all. |
| —Female, ovarian cancer, diagnosed at age 29 | |
| I was 19. And I’m, like, “I have to find sperm?” I’m single. I’m like, “Where am I going to get sperm?” And I didn’t like the idea of getting an anonymous—you know, that was really tough .... You could go out of province, I think, to Quebec to have just an egg frozen, but I guess it’s considered experimental, if it even works. It’s like in the tens of thousands of dollars. | |
| —Female, Hodgkin lymphoma, diagnosed at age 19 | |
| Medical care needs | When I went back, all I received was a, like, a rubdown sort of thing: check my armpits, check my groin, the areas where a lump would come back. And asked ... questions, and there was no type of medical test done.... So I wasn’t happy with that, really. |
| —Male, non-Hodgkin lymphoma, diagnosed at age 34 | |
| When they test for [blood] levels, they usually only test your tsh and t4. And that’s usually all they will test you for, but there’s another one they should test you for too. I would just feel more comfortable if they [were to] test all three, because I read so much about it, and there’s things that are ... I don’t know ... because my levels were fine before I was diagnosed, which was why they were thinking probably that I didn’t have cancer. But, obviously, there was something wrong, but it wasn’t showing. Maybe if they tested all three of them, maybe they would have seen .... I don’t know ... but I would just feel more at ease. | |
| —Female, thyroid cancer, diagnosed at age 27 | |
| Psychological care needs | Some kind of counselling around how to deal with young children when the parent is sick would have been helpful. And, also, I don’t know—something for my husband maybe, too, would have been good. Because, you know, it’s kind of a different experience when you are a young person. We’d only been married for a few years.... I think it would have been helpful for him to still have someone to talk to, you know. |
| —Female, breast cancer, diagnosed at age 36 | |
| I took a lot of, a lot of, my rage out on my girlfriend. Not physically, of course, but more emotionally. Umm, you know, I was really uncomfortable with my body. Umm, so, and like, I needed space, and during that time she needed to be close. And that, it, I was just really uncomfortable with her around. And, umm, I guess, it—it really wasn’t a whole good situation for us. Umm, I, yeah, you know, I ... we fought a lot. Umm, well it was more me doing the fighting and her just taking it, and it obviously led to our breakup, and now we don’t really have a relationship at all. | |
| —Male, testicular cancer, diagnosed at age 19 | |
| Social care needs | There should be definitely something for people that fall into the category that doesn’t get any money.... The cost of the drugs that I paid monthly after my chemo was horrendous. |
| —Female, breast cancer, diagnosed at age 34 | |
| There are those who can afford to go out and have [infertility treatment] procedures done and ... and all this, like.... And I have to say that, at that point [right after treatment], I did not have insurance or ... money, necessarily, to be able to do that. But I wish I’d been pointed out those options, and I would like there to be a fund that people can apply to, to get—to help them do that. | |
| —Female, breast cancer, diagnosed at age 32 | |
| System care needs | I think a patient navigator for one. I think, in the perfect world, that would be someone who would start right at diagnosis and take you through to the end, whatever that may be.... I don ’t know if it would be specific to each individual, but specific again to the age group. |
| —Female, cervical cancer, diagnosed at age 28 | |
| In the kind of whole ideal world is, you know, you can go to one place and have everything done.... Everything is in one department. You know, you’re not going from department to department. | |
| —Female, Hodgkin lymphoma, diagnosed at age 21 |
3.1.1. Need for Age-Specific Care
When participants were asked about their current cfc, 76% mentioned the need for age-specific cancer care. For example, an ovarian cancer survivor diagnosed at age 29 described the difficulties she had finding relevant information, saying that the resources she found were “all older-age related and not helpful at all.” Participants found that specific issues related to their stage in life were not adequately addressed.
3.1.2. Medical Care Needs
In addition to regular medical care such as physical check-ups, study participants made it clear that they would like to see
more survivorship care plans during cfc,
better access to imaging and tests to detect recurrences, and
better infertility treatment options.
Many participants felt lost after completion of their acute cancer treatment; they had no clear idea what to expect regarding cfc. Some (15%) suggested a survivorship care plan to help better coordinate care and to give survivors a sense of control over their own health. A small number of participants (11%) felt that follow-up care visits had to be more “active,” including more scans and tests.
Fertility issues are unique and important to cancer survivors in this age group. Of our participants, 29 of 39 women (74%) and 10 of 14 men (71%) mentioned fertility issues during the interviews. Of participants who discussed fertility issues, 56% were between the ages of 26 and 35 years. Fertility preservation such as sperm banking was attempted for only a few participants. The aggressive nature of some cancers and the frequency of delays in diagnosis in this age group meant that fertility preservation was not always possible before treatment. Also, many patients do not have access to fertility treatment centres in their area. Thus, infertility was a major concern for many participants.
3.1.3. Psychological Care Needs
Many cancer centres and oncology units have a psychologist on staff who is available during treatment; however, this service seems to be less accessible during cfc. Study participants reported feeling that, during their cfc, they had entered a period of uncertainty. Some struggled with depression, anxiety, fear of recurrence, and problems with sexuality and infertility.
Participants with young children faced additional challenges in terms of childcare and helping their children deal with emotions related to having a seriously sick parent. Most parents (79%) discussed the need for family counselling to help their children cope. In addition, some felt that their partners or other family members could also have benefited from counselling.
3.1.4. Social Care Needs
Although many cancer centres and oncology units have social workers on staff, participants expressed a desire for a broad set of social care needs to help deal with the enormous disruption that a cancer diagnosis brings to the lives of young adults with cancer. Work and schooling are often disrupted, because few young adults have established career patterns. Job continuation after treatment is often very difficult for survivors; many find themselves unemployed. Hence, during cfc, workforce re-entry and career counselling are important. In our study, 42% of participants were working full time; 17% were working part time or casual; 19% were not working (unemployed, on unpaid sick leave, homemakers); 9% were on long-term disability; and 13% were in school. School issues were discussed almost exclusively by participants less than 25 years of age (93%); work issues were prominent among participants older than 25 (71%). As a result of their poor participation in the workforce, many participants had experienced financial problems.
3.1.5. System Care Needs
The fourth and final subtheme that emerged from the analysis was system related:
A “one-stop” cancer centre to provide all care, including psychological and social cfc
Better access to supplemental health insurance
Patient advocates or navigators to help facilitate a more coherent and comprehensive approach to cfc
The desire for a “one-stop” cancer centre that includes psychological and social care to enable continuity of cancer care into the cfc phase of the cancer continuum was specifically mentioned by 12% of participants.
In Canada, supplemental health insurance is a private health insurance option in addition to the universal basic public health insurance (which covers hospital and physician visit costs). For participants in the workforce, the purchase of private health insurance is often a shared responsibility between employer and employee. Depending on the situation and the insurance company, many children and young adults are covered by parental private health insurance up to the age of 25. In some cases, an individual buys private health insurance outright. In our sample, 21% of survivors lacked supplemental health insurance. This subgroup had to personally pay for all of their medication and allied health care services. Also, once the diagnosis of a serious illness was made, private health insurance was more difficult to obtain.
4. DISCUSSION
It is apparent from our study that current cfc practices in Canada for young adults are inadequate. During a workshop organized by the Canadian Task Force on Adolescent and Young Adult Cancer, issues similar to the ones identified in our study were described, specifically the medical and psychological care needs; however, our findings also highlight specific social care and system care needs that are rarely discussed (if at all) in the literature35. Ramphal et al.11 described a new model of cancer care with a focus on medical care, psychosocial support, and physical environment (related to treatment). However, social and system issues were not mentioned as being important in cfc. We believe that, during cfc, social care needs and system care needs are as important as medical and psychological needs. Being unable to work or not having supplemental health insurance can have a profound impact on the cancer survivor and can lead to mental and physical morbidities in addition to those associated with cancer36. In terms of follow-up medical care needs, we recognize that some of the needs expressed by participants, such as wanting more tests or imaging, might not always be necessary or appropriate37. A paradox accompanies the desire for more testing, because such testing can often lead to increased anxiety, and it is not without risks38. At the same time, such surveillance can also reassure until the next round of testing. Perhaps the desire for tests and scans is in reality a desire for reassurance. That need could also be met by more counselling and information.
Thompson and colleagues used focus groups with young adult cancer survivors between the ages of 22 and 30 years to conduct a small qualitative study in Australia. Although their study did not focus exclusively on cfc, the study participants discussed cfc issues17. The findings from the Thompson et al. study are similar to ours, albeit less detailed. Participants in both studies described anxiety about cfc because it is less structured than active cancer treatment. Employment and education were also significant issues both in the Thompson et al. study and in our findings.
As all three of the foregoing studies demonstrated, the needs of young adult cancer survivors in countries such as Canada, the United States, and Australia are not being met in a comprehensive manner11,17.
As a result of the analysis of our data, we developed a conceptual model of cfc that is more comprehensive than the fragmented care currently provided. Figure 1 depicts the model as a schematic, and Figure 2 describes in more detail the unique age-specific cfc needs of this group. Some of the needs may be relevant to all cancer survivors regardless of age; others are unique to the young adult age group.
FIGURE 1.
Conceptual model of follow-up care in young adults with cancer.
FIGURE 2.
Specific needs of young adult cancer survivors.
We are not advocating for new cfc infrastructure for young adult cancer survivors, but we do encourage existing centres to take into consideration the unique needs of this cancer population and to include age-specific resources. In fact, the International Charter of Rights for Young People with Cancer declares that young people with cancer have a right to receive appropriate age-specific comprehensive care39. The delivery of health care in Canada is a matter of provincial jurisdiction, and it varies greatly from region to region10; however, the needs of this group of cancer survivors are similar no matter the health care jurisdiction. The participants in our study indicated that current cfc practices in Canada do not meet their needs and that a new approach is required to take their unique needs into consideration. Meeting more of the cfc needs of this population would help them transition more easily to the “normalcy” that they desire, would empower them to achieve independence, and would reduce psychological and social morbidity5.
4.1. Study Limitations
Our study is based on a theoretical sample and therefore the results cannot be generalized to all young adult cancer survivors. We acknowledge that our sample had a larger proportion of female participants and a larger representation of participants from Eastern Canada than from other parts of the country, which may have biased the results. Nonetheless, we are confident that, among young adult cancer survivors, our participants represented enough diversity of cancer type, residence (urban, rural), and geographic area that our study results are transferable to this population across Canada. As in most research studies, particularly self-referral studies such as this one, participants who experienced significant challenges might have been more inclined to participate than young adults who did not. However, we feel that we have identified deficits in current cfc in Canada, and we are confident that our conceptual model of cfc will be beneficial to many, if not all, young adult cancer survivors.
5. CONCLUSIONS AND FUTURE DIRECTIONS
The provision of age-appropriate comprehensive cfc in Canada is inadequate. A comprehensive approach to cfc can reduce the physical, psychological, and social morbidity associated with cancer. Such an approach is important for young adult cancer survivors who potentially have many productive years ahead. Hence, we propose a conceptual model of cfc based on the needs and recommendations of the participants in the present study.
6. ACKNOWLEDGMENTS
This study was supported by a grant from the Canadian Institutes of Health Research (MOP97737). We thank Krystle Hussey for her work on the project, and Dr. Sue Tatemichi for her assistance in editing the manuscript.
Footnotes
Easley J, Young Adult Cancer Canada, Retreat Yourself. Personal communication. Montreal, QC, 2006.
7. CONFLICT OF INTEREST DISCLOSURES
The authors have no financial conflicts of interest to disclose.
8. REFERENCES
- 1.Cancer Care Ontario. Cancer in Young Adults in Canada. Toronto, ON: Canadian Cancer Society; 2006. [Google Scholar]
- 2.Canadian Cancer Society’s Steering Committee. Canadian Cancer Statistics 2011. Toronto, ON: Canadian Cancer Society; 2011. [Google Scholar]
- 3.Greenberg M, Klassen A, Gafni A, McBride ML, Albritton K. Outcomes and metrics: measuring the impact of a comprehensive adolescent and young adult cancer program. Cancer. 2011;117(suppl):2342–50. doi: 10.1002/cncr.26040. [DOI] [PubMed] [Google Scholar]
- 4.Miedema BB, Easley J, Hamilton R. Young adults’ experiences with cancer: comments from patients and survivors. Can Fam Physician. 2006;52:1446–7. [PMC free article] [PubMed] [Google Scholar]
- 5.Miedema B, Hamilton R, Easley J. From “invincibility” to “normalcy”: coping strategies of young adults during the cancer journey. Palliat Support Care. 2007;5:41–9. doi: 10.1017/S147895150707006X. [DOI] [PubMed] [Google Scholar]
- 6.Miedema B. Young cancer patients face unique obstacles in being independent. The Medical Post. 2006 Oct 20;:2. [Google Scholar]
- 7.Dunn J, Steginga SK. Young women’s experience of breast cancer: defining young and identifying concerns. Psychooncology. 2000;9:137–46. doi: 10.1002/(SICI)1099-1611(200003/04)9:2<137::AID-PON442>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 8.Wang C, Burris MA, Ping XY. Chinese village women as visual anthropologists: a participatory approach to reaching policymakers. Soc Sci Med. 1996;42:1391–400. doi: 10.1016/0277-9536(95)00287-1. [DOI] [PubMed] [Google Scholar]
- 9.Cancer Care Ontario (cco) The Cancer Control Continuum [Web page] Toronto, ON: CCO; 2009. [Available at: https://www.cancercare.on.ca/pcs/careoverview/cancercontrol; cited August 29, 2012] [Google Scholar]
- 10.Sutcliffe SB. A review of Canadian health care and cancer care systems. Cancer. 2011;117(suppl):2241–4. doi: 10.1002/cncr.26053. [DOI] [PubMed] [Google Scholar]
- 11.Ramphal R, Meyer R, Schacter B, Rogers P, Pinkerton R. Active therapy and models of care for adolescents and young adults with cancer. Cancer. 2011;117(suppl):2316–22. doi: 10.1002/cncr.26048. [DOI] [PubMed] [Google Scholar]
- 12.Soliman H, Agresta SV. Current issues in adolescent and young adult cancer survivorship. Cancer Control. 2008;15:55–62. doi: 10.1177/107327480801500107. [DOI] [PubMed] [Google Scholar]
- 13.Zebrack BJ, Mills J, Weitzman TS. Health and supportive care needs of young adult cancer patients and survivors. J Cancer Surviv. 2007;1:137–45. doi: 10.1007/s11764-007-0015-0. [DOI] [PubMed] [Google Scholar]
- 14.Bloom JR, Petersen DM, Kang SH. Multi-dimensional quality of life among long-term (5+ years) adult cancer survivors. Psychooncology. 2007;16:691–706. doi: 10.1002/pon.1208. [DOI] [PubMed] [Google Scholar]
- 15.Gurevich M, Bishop S, Bower J, Malka M, Nyhof–Young J. (Dis)embodying gender and sexuality in testicular cancer. Soc Sci Med. 2004;58:1597–607. doi: 10.1016/S0277-9536(03)00371-X. [DOI] [PubMed] [Google Scholar]
- 16.Miedema B, MacDonald I, Tatemichi S. Cancer follow-up care. Patients’ perspectives. Can Fam Physician. 2003;49:890–5. [PMC free article] [PubMed] [Google Scholar]
- 17.Thompson K, Palmer S, Dyson G. Adolescents and young adults: issues in transition from active therapy into follow-up care. Eur J Oncol Nurs. 2009;13:207–12. doi: 10.1016/j.ejon.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 18.Zebrack BJ, Ganz PA, Bernaards CA, Petersen L, Abraham L. Assessing the impact of cancer: development of a new instrument for long-term survivors. Psychooncology. 2006;15:407–21. doi: 10.1002/pon.963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.D’Agostino NM, Penney A, Zebrack B. Providing developmentally appropriate psychosocial care to adolescent and young adult cancer survivors. Cancer. 2011;117:2329–34. doi: 10.1002/cncr.26043. [DOI] [PubMed] [Google Scholar]
- 20.What should the age range be for aya oncology? J Adolesc Young Adult Oncol. 2011;1:3–10. doi: 10.1089/jayao.2011.1505. [DOI] [PubMed] [Google Scholar]
- 21.Canada Cancer Society. Cancer in Adolescents and Young Adults (15–29 Years) Toronto, ON: Canadian Cancer Society; 2009. [Google Scholar]
- 22.Bleyer A, Albritton KH, Barr RD, Lewis I, Sender LS. Trailblazers in adolescent and young adult oncology. J Adolesc Young Adult Oncol. 2011;1:1–6. doi: 10.1089/jayao.2011.1500. [DOI] [PubMed] [Google Scholar]
- 23.Wu X, Groves FD, McLaughlin CC, Jemal A, Martin J, Chen VW. Cancer incidence patterns among adolescents and young adults in the United States. Cancer Cause Control. 2005;16:309–20. doi: 10.1007/s10552-004-4026-0. [DOI] [PubMed] [Google Scholar]
- 24.United States National Institutes of Health, National Cancer Institute (nci) Survivorship—Living With and Beyond Cancer [Web page] Bethesda, MD: NCI; 2006. [Available at: http://www.cancer.gov/cancertopics/coping/survivorship; cited December 6, 2012] [Google Scholar]
- 25.Zebrack BJ. Cancer survivor identity and quality of life. Cancer Pract. 2000;8:238–42. doi: 10.1046/j.1523-5394.2000.85004.x. [DOI] [PubMed] [Google Scholar]
- 26.Canadian Partnership Against Cancer (cpac) Canadian Strategy for Cancer Control, Supportive Care/Cancer Rehabilitation Workgroup Final Report. Toronto, ON: CPAC; 2002. [Google Scholar]
- 27.Ganz PA, Desmond KA, Leedham B, Rowland JH, Meyerowitz BE, Belin TR. Quality of life in long-term, disease-free survivors of breast cancer: a follow-up study. J Natl Cancer Inst. 2002;94:39–49. doi: 10.1093/jnci/94.1.39. [DOI] [PubMed] [Google Scholar]
- 28.Tan SM, Cheung KL, Willsher PC, Blamey RW, Chan SY, Robertson JF. Locally advanced primary breast cancer: medium-term results of a randomised trial of multimodal therapy versus initial hormone therapy. Eur J Cancer. 2001;37:2331–8. doi: 10.1016/S0959-8049(01)00298-2. [DOI] [PubMed] [Google Scholar]
- 29.Glaser BG, Strauss AL. The Discovery of Grounded Theory: Strategies for Qualitative Research. Chicago, IL: Aldine de Gruyter; 1967. [Google Scholar]
- 30.Charmaz K. Grounded theory: objectivist and constructivist methods. In: Denzin N, Lincoln YS, editors. Handbook of Qualitative Research. 2nd ed. Thousand Oaks, CA: Sage Publications; 2000. [Google Scholar]
- 31.Creswell JW. Qualitative Inquiry and Research Design: Choosing Among Five Traditions. Thousand Oaks, CA: Sage Publications; 1998. [Google Scholar]
- 32.Mills J, Bonner A, Francis K. The development of constructivist grounded theory. Int J Qual Meth. 2006;5:1–9. [Google Scholar]
- 33.Busby S, Witucki–Brown J. Theory development for situational awareness in multi-casualty incidents. J Emerg Nurs. 2011;37:444–52. doi: 10.1016/j.jen.2010.07.023. [DOI] [PubMed] [Google Scholar]
- 34.Hubbard G, Kidd L, Kearney N. Disrupted lives and threats to identity: the experiences of people with colorectal cancer within the first year following diagnosis. Health (London) 2010;14:131–46. doi: 10.1177/1363459309353294. [DOI] [PubMed] [Google Scholar]
- 35.Fernandes CM, Fraser GAM, Freeman CR, et al. Principles and recommendations for the provision of healthcare in Canada to adolescent and young adult-aged cancer patients and survivors. J Adolesc Young Adult Oncol. 2011;1:53–9. doi: 10.1089/jayao.2010.0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wright EP, Kiely MA, Lynch P, Cull A, Selby P. Social problems in oncology. Brit J Cancer. 2002;87:1099–104. doi: 10.1038/sj.bjc.6600642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Espasa R, Murta–Nascimento C, Bayes R, et al. The psychological impact of a false-positive screening mammogram in Barcelona. J Cancer Educ. 2012 doi: 10.1007/s13187-012-0349-9. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 38.Garcia M, Milà N, Binefa G, Borràs JM, Espinàs JA, Moreno V. False-positive results from colorectal cancer screening in Catalonia (Spain), 2000–2010. J Med Screen. 2012;19:77–82. doi: 10.1258/jms.2012.012013. [DOI] [PubMed] [Google Scholar]
- 39.Rajani S, Young AJ, McGoldrick DA, Pearce DL, Sharaf SM. The international charter of rights for young people with cancer. J Adolesc Young Adult Oncol. 2011;1:49–52. doi: 10.1089/jayao.2010.0007. [DOI] [PubMed] [Google Scholar]