Abstract
Background
Aphasia is a severely disabling condition occurring in 20 to 25% of stroke patients. Most patients with aphasia due to stroke receive speech and language therapy. Methodologically sound randomised controlled trials investigating the effect of specific interventions for patients with aphasia following stroke are scarce. The currently available evidence suggests that intensive speech and language therapy is beneficial for restoration of communication, but the optimal timing of treatment is as yet unclear.
In the Rotterdam Aphasia Therapy Study-3 we aim to test the hypothesis that patients with aphasia due to stroke benefit more from early intensive cognitive-linguistic therapy than from deferred regular language therapy.
Methods/design
In a single blinded, multicentre, randomised controlled trial, 150 patients with first ever aphasia due to stroke will be randomised within two weeks after stroke to either early intensive cognitive-linguistic therapy (Group A) or deferred regular therapy (Group B). Group A will start as soon as possible, at the latest two weeks after stroke, with a four week period of one hour a day treatment with cognitive-linguistic therapy. In Group B professional speech and language therapy is deferred for four weeks. After this period, patients will follow the conventional procedure of speech and language therapy. Participants will be tested with an extensive linguistic test battery at four weeks, three months and six months after inclusion. Primary outcome measure is the difference in score between the two treatment groups on the Amsterdam-Nijmegen Everyday Language Test, a measure of everyday verbal communication, four weeks after randomisation.
Trial registration
This trial is registered in the Dutch Trial Register (http://www.trialregister.nl), NTR3271.
Keywords: Aphasia, Stroke, Cognitive-linguistic therapy, Treatment, Timing, Intensity, RCT
Background
About one fifth to a quarter of all stroke patients suffer from aphasia [1]. Aphasia after stroke is a major health problem with dramatic consequences for the quality of life of affected individuals. Communication is essential in daily life and may influence the outcome of rehabilitation [2], since different forms of therapy are usually instructed verbally. Hence, speech and language therapy (SLT) is considered very important in the acute phase after stroke.
The effectiveness of SLT has been evaluated in a variety of studies, many of which relied on small samples and were of limited methodological quality. Recently the Cochrane Collaboration has published a review of 39 trials on the efficacy of language therapy for aphasia after stroke [3]. The authors conclude that there is some evidence that SLT is more effective than no SLT for recovery of communication after stroke and that efficacy of SLT seems to be influenced by intensity of therapy. However, they emphasise that these results should be interpreted cautiously, as many studies lack proper methodology and comparison across studies is hampered by a large degree of heterogeneity regarding characteristics of the study population, applied treatment methods, timing and duration of therapy, and outcome assessments.
There are two main approaches in aphasia treatment: cognitive-linguistic therapy (CLT) and communicative or functional therapy [4]. CLT focuses on deficits in linguistic components, such as semantics (word meaning), phonology (speech sounds) and syntax (sentence level), and aims at restoring linguistic processes that are the foundation of language. Communicative therapy focuses on compensation by making use of all communicative channels; patients learn to utilise preserved verbal as well as nonverbal communicative functions. Communicative therapy is provided in a realistic everyday environment and uses gestures, communication aids, such as an icon board, role plays and the Promoting Aphasics’ Communicative Effectiveness (PACE) method [5]. CLT is mostly applied in early stages after stroke and communicative therapy later on.
Our group previously studied the efficacy of CLT, aimed at semantic and phonological processing, in comparison to communicative therapy in the acute stage of aphasia in the Rotterdam Aphasia Therapy Study (RATS) – 2 [6]. A total of 80 aphasic patients were randomised to either CLT or communicative therapy for six months, starting within three weeks after the stroke. We found no significant difference between groups on the primary outcome measure, the Amsterdam-Nijmegen Everyday Language Test, A-scale (ANELT-A) [7]. However, the majority of the secondary outcome measures on semantics and phonology were in favour of CLT. Perhaps the treatment intensity of both interventions, on average 2.1 hours per week, was insufficient to generate a significant treatment effect on top of spontaneous recovery [8-10].
Recovery of communication usually occurs shortly after stroke [11-14]. Most likely restoration of the perilesional network in the left hemisphere is the primary mechanism underlying this spontaneous recovery [15]. Therapeutic strategies to restore cerebral blood flow, such as thrombolysis, enhance spontaneous recovery. SLT is aimed at stimulating cortical networks involved in language, hence increasing blood flow to these damaged areas. CLT especially stimulates the linguistic cortical network through specific exercises for linguistic components, such as semantics, phonology and syntax [4]. Hence SLT, and in particular CLT, is thought to contribute positively to spontaneous recovery of language [14,15]. Some, therefore, claim that the focus of SL-therapists in the acute stage of aphasia, when restoration of the linguistic network is still plausible, should be on CLT [14,16].
In this respect, several clinical studies suggest that therapy provided immediately after stroke results in more beneficial effects than deferred treatment [11]. In a review article that was not restricted to randomised trials but also included studies with other designs, the authors conclude that SLT in the acute stages of aphasia following stroke is almost twice as effective as natural recovery alone [10]. This assumes the presence of a “critical period” after stroke during which the brain is more susceptible to rehabilitation. Furthermore, it implies that SLT should be initiated as soon as possible after stroke. This assumption also suggests that if SLT is initiated too late, recovery might be restricted. The length of this supposed “critical period”, however, is unclear and optimal timing of therapy remains uncertain.
A second mechanism of recovery is neural plasticity [17]. Intensive training, for instance, massed practise, is thought to trigger remodelling and consolidation of neural networks [15]. Efficacy of SLT is considered to be related to intensity [8]. In the Cochrane systematic review of randomised controlled trials on SLT for aphasic stroke patients, it was shown that efficacy of SLT positively correlated with treatment intensity, although this was related to more therapy drop-outs [3]. However, a recently published pilot study on intensive SLT in 59 acute stroke patients with aphasia suggests that early intensive SLT is feasible in the acute stage after stroke [18]. The number of drop-outs or deaths reported in the intervention group with daily therapy was not higher than in the control group with usual care therapy.
Another trial, in which 123 aphasic patients were randomised for intensive SLT (three weeks of daily SLT for 45 minutes on workdays, starting within two days after stroke) or control condition (no SLT for three weeks) in the acute stage of aphasia, showed no significant differences between groups on the primary outcome measure ANELT-A [7,19]. The authors conclude that not all patients with aphasia after stroke benefit from early intensive SLT, but it can be questioned whether therapy in this study was sufficiently intensive [8-10].
Based on the currently available evidence, we suggest an optimal regime of early initiated intensive CLT for aphasia after stroke. This regime will be studied in the Rotterdam Aphasia Therapy Study (RATS) – 3.
Objective
The objective of this study is to test the hypothesis that patients with aphasia after stroke benefit more from early initiated intensive cognitive-linguistic therapy than from deferred regular SLT.
Methods
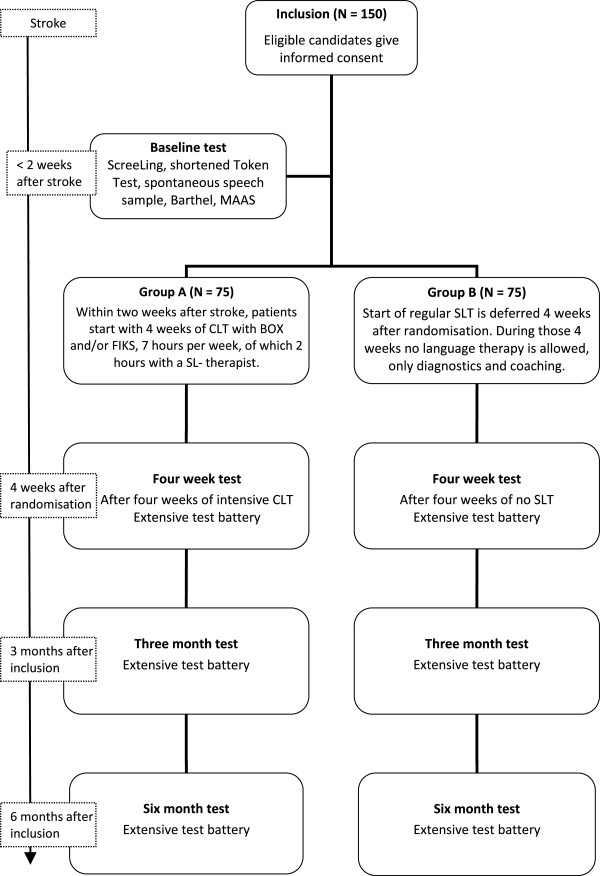
RATS-3 is a multicentre, stratified (for centre of inclusion and severity of aphasia) single-blinded randomised controlled trial with parallel groups (see Figure 1).
Figure 1.
Flow diagram of the RATS-3 study design.
Participants and recruitment
RATS-3 is coordinated by the Erasmus MC – University Medical Center Rotterdam, and over 40 hospitals, nursing homes and rehabilitation centres in The Netherlands participate. SL-therapists in participating centres are trained and supervised by the trial team.
Hospitalised patients with aphasia due to stroke are screened by the local SL-therapist for eligibility with the inclusion and exclusion criteria within two weeks after stroke (see Table 1).
Table 1.
Eligibility criteria for the Rotterdam Aphasia Therapy Study (RATS) – 3
| Inclusion criteria: | |||
|---|---|---|---|
| 1. Aphasia after stroke, determined by a neurologist or rehabilitation physician and speech and language therapist; |
|||
| 2. Within two weeks after stroke; |
|||
| 3. Testable with ScreeLing [20]; |
|||
| 4. Aphasia ascertained with shortened Token Test [21] and/or a score <5 on Goodglass Aphasia Severity Rating Scale [22]; |
|||
| 5. Age between 18 and 85 years; |
|||
| 6. Language near native Dutch; |
|||
| 7. Life expectancy of more than six months. |
|||
|
Exclusion criteria: | |||
| 1. Pre-existing aphasia; |
|||
| 2. Subarachnoid/subdural haemorrhage/hematoma; |
|||
| 3. Severe threats to success and/or feasibility of language therapy: |
|||
| a. Severe dysarthria; |
|||
| b. Premorbid dementia; |
|||
| c. Illiteracy; |
|||
| d. Severe developmental dyslexia; |
|||
| e. Severe visual perceptual disorders; |
|||
| f. Recent psychiatric history. | |||
Written informed consent is acquired by the local SL-therapist from eligible patients and/or their family. Patient information and consent forms are approved by the medical ethical committee of the Erasmus MC – University Medical Center Rotterdam. Local SL-therapists will inform the RATS-3 team of every new participant.
Baseline tests
All candidates will be tested with the ScreeLing [20], a screening instrument for aphasia. Aphasia is ascertained by the shortened version of the Token Test [21] and a sample of spontaneous speech assessed with the Goodglass Aphasia Severity Rating Scale [22]. Activities of daily life will be reported with the Barthel Index [23] and observational data on social and (neuro)psychological functioning and wellbeing will be collected with the MAAS (Multi-axial Aphasia System [24]).
Randomisation
Each participant is assigned to either Group A or Group B by restricted randomisation via stratification for severity of aphasia and centre of inclusion. The allocation sequence is computer generated and concealed in consecutively numbered, opaque, sealed envelopes. The trial coordinator randomises participants to treatment groups after severity of aphasia is assessed. A score on the Goodglass Aphasia Severity Rating Scale [22] of 0 to 2 is considered to reflect severe aphasia and a score of 3 to 5 reflects moderate to mild aphasia.
Intervention
As soon as possible after randomisation the intervention period of four weeks starts, during which Group A receives early intensive CLT and Group B receives no SLT.
Intervention group: Group A (N = 75)
Participants allocated to Group A receive intensive CLT with the treatment programs BOX [25] and/or FIKS [26]. The BOX and FIKS programs are commonly used in The Netherlands and aim at the improvement of word finding (see Table 2). BOX focuses on semantics and FIKS on phonology. Both interventions are well outlined, which ensures homogeneity of treatment in this group [6]. BOX and FIKS consist of several subparts that provide a large number of specific exercises, to treat various layers of semantic and phonological processing. Exercises can be presented visually and/or orally and require receptive and productive skills. Each subpart contains different levels of complexity, which makes these programs suitable to all types and severity levels of aphasia. Both programs are also available on computer (eBOX and eFIKS) to facilitate homework.
Table 2.
Illustration of CLT with the semantic therapy program BOX and the phonological program FIKS
| Semantic therapy program BOX Subject: word meaning Objective: consolidate the internal semantic network to improve word finding Presentation: oral, visual or by computer (eBOX) | ||||
|---|---|---|---|---|
|
Examples: |
|
|||
| Word level |
Sentence level |
|
|
|
|
Which word does not match? |
Is this sentence correct? |
|||
| Ruler |
The balloon flies in the air. |
|||
|
Musical scale |
Correct. |
|||
| Gauge |
|
|||
| Balance |
The candle is burning embittered. |
|||
| Measuring tape |
Incorrect. Please correct the sentence. |
|||
|
Phonological therapy program FIKS Subject: processing and production of speech sounds Objective: consolidate the internal phonological network and improve production of speech, to improve word finding Presentation: oral, visual or by computer (eFIKS) | ||||
|
Examples: |
|
|||
| Word level |
|
|||
|
Which word is printed here? |
tion |
trans |
la |
= translation |
|
Read it out loud please. |
ment |
ta |
tes |
= testament |
| Sentence level |
|
|||
|
Please finish the sentence with a rhyming word: |
The enthusiastic amateur cook, |
|||
| read the recipe carefully in his cooking- … | ||||
Therapy will start at the latest two weeks after stroke. However, as soon as participants are included and randomised, therapy can be started.
Recent findings on intensity of treatment [3,8] suggest that one hour of language therapy per day is sufficiently intensive to generate an effect of therapy on top of the effect of spontaneous recovery. This high intensity is uncommon in The Netherlands. Therefore SL-therapists will treat participants at least two hours a week, supplemented with homework using paper or digital versions of the therapy programs. The SL-therapists register all therapy sessions in minutes on special registration forms. These forms will be handed to the patient and/or his caretaker also for homework registration.
The trial coordinator contacts SL-therapists every week to check whether the allocated treatment is adequately applied and ask if any problems arise complying with the protocol.
Control group: Group B (N = 75)
Language therapy is deferred in Group B. Regular language therapy will start four weeks after randomisation. During these four weeks no SLT is allowed. SL-therapists, however, will be attentive to participants in Group B. They may inform the patient and his caretakers about aphasia and its consequences and provide advice to avoid severe communication distress. Additional diagnostic tests and specific observations on communicative functioning may be performed to set detailed therapy goals.
Therapy after four weeks by a SL-therapist will be arranged if the patient is discharged home. The trial coordinator will keep in contact with the patient during these four weeks. If the patient is released to a rehabilitation centre or nursing home, the coordinator will contact the SL-therapist after two weeks to evaluate whether the protocol can be followed correctly.
Follow-up measurements
Verbal communicative abilities of participants will be evaluated four weeks after randomisation, three months after inclusion and six months after inclusion, using an extensive linguistic test battery (see Table 3). Tests requiring a verbal response are recorded digitally. All SL-therapists receive a manual for the administration of the linguistic tests. Results will be scored in a booklet containing all score forms per test moment. The trial team will score all tests and report the results to the SL-therapists.
Table 3.
Linguistic test battery of RATS-3
| General communication tests | |
|---|---|
| - ANELT-A: communicative functioning in daily life [7]; | |
| - Semi-standardised interview for spontaneous speech rated with Goodglass Aphasia Severity Rating Scale [22]; | |
| - Sabadel: connected speech [27]; | |
| - ScreeLing: screening of three linguistic components: semantics, phonology and syntax [28]; | |
| - Token Test, short version: measures severity of aphasia [21]; | |
| - Boston Naming Test: identifies word finding difficulties [29]. | |
|
Specific semantic tests | |
| - Semantic Association Test, verbal version (SAT) [30]; | |
| - Comprehensive Aphasia Test, word comprehension (CAT) [31]; | |
| - Semantic Word Fluency [32]. | |
|
Specific phonological tests | |
| - Nonword repetition, PALPA [33]; | |
| - Auditory Lexical Decision, PALPA [33]; | |
| - Letter Fluency [34]. | |
|
General | |
| - Barthel Index: activities of daily life [23]; | |
| - Multi-Axial Aphasia System (MAAS) [24]; | |
| - Partner ANELT: partner’s perspective on the patient’s communicative functioning [35]; | |
| - Self evaluation of communicative functioning on a 0 to10 scale; | |
| - EuroQol: quality of life [36]; | |
| - Modified Rankin Scale: activities of daily life [37]. |
Aphasia type will be determined with the Aachen Aphasia Test (AAT, [38]) between the fourweek and threemonth test. This period after spontaneous recovery is chosen because we assume aphasia type will then be stabilised.
Sequel after the four week test
Regular language therapy will start in Group B and Group A continues with regular therapy after the fourweek test. Regular therapy in The Netherlands comprises a combination of CLT and communicative therapy and focuses mainly on therapy goals set by the patient. Regular therapy intensity is on average approximately two hours per week [39]. Registration of therapy sessions and therapy type (either CLT or communicative or a combination) will be continued, although not as meticulously as during the four weeks of intervention.
Primary outcome
The primary outcome measure in RATS-3 is the difference in the score on the ANELT-A [7] at the four week test moment (after intervention) between the two groups. CLT aims at improving linguistic skills, which theoretically results in better daily communication. The A-scale of the valid and reliable ANELT [40] measures verbal communicative ability. Participants’ verbal responses to 10 everyday communicative scenarios are scored on a five-point scale for information content.
Secondary outcomes
The difference in scores between groups at the four week test on the Semantic Association Test (SAT), verbal version [30]; Semantic Word Fluency [32], Psycholinguistic Assessment of Language Processing in Aphasia (PALPA), Nonword repetition [33]; PALPA, Auditory Lexical Decision [33]; and Letter Fluency [34] will be used as secondary outcome measures. Other secondary outcomes are differences in all test scores at three months, and differences in scores on the EuroQol (quality of life) [36] and Modified Rankin Scale (functional outcome) [37].
Tertiary outcomes
Scores on the above mentioned tests at six months after inclusion, including ANELT-A, will be used as tertiary outcome measures.
Sample size
A sample of 75 participants in each group, a total of 150 participants, is estimated to provide 84% power to detect a statistically significant difference on the primary outcome measure between groups at a 5% two-sided significance level. An inclusion period of two years is estimated to be required for recruitment.
Blinding
Due to the intervention type, therapy or no therapy, it is impossible for participants and SL-therapists to be blinded for intervention. Assessment of the primary outcome, however, will be blinded. Two experienced independent observers, who are blinded for treatment allocation and test moment, will score the primary outcome measure ANELT-A. The mean score of both independent observers will be used in the analyses. Interobserver agreement will be assessed by means of a plot of differences between scores versus their mean. The mean difference between observers will be calculated with a 95% confidence interval.
Statistical analyses
Difference in score on ANELT-A between groups will be compared with analysis of covariance (ANCOVA) with a 95% confidence interval, adjusted for baseline severity. Baseline severity is determined according to the Goodglass Aphasia Severity Rating Scale [22] in a sample of spontaneous speech.
This method will also be used for the additional linguistic tests in the secondary and tertiary outcome measures.
Ethics
The RATS-3 study protocol is approved by the independent medical ethical committee of the Erasmus MC – University Medical Center Rotterdam (MEC-2005-347), and registered in the Dutch Trial Register (NTR3271) [41].
Trial status
The trial started January 2012. We estimate that inclusion will be finished in January 2014.
Appendix
In Table 4, we publish the list of participating centres updated until August 2012. This list is not final as we are still actively recruiting centres.
Table 4.
Provisional list of participating centres and the principal local investigators*
| Hospitals | Principal Investigator |
|---|---|
| Haven Ziekenhuis, Rotterdam |
Ida Boas |
| Sint Franciscus Gasthuis, Rotterdam |
Joyce van Dalen |
| Ikazia Ziekenhuis, Rotterdam |
Mathanja Sibon |
| Maasstad Ziekenhuis, Rotterdam |
Fabiënne Stok |
| Vlietland Ziekenhuis, Schiedam |
Obbe de Roos |
| IJsselland Ziekenhuis, Capelle aan de IJssel |
Ingrid Arp |
| Reinier de Graaf Gasthuis, Delft |
Jolanda van Veldhuizen |
| MCH Westeinde, Den Haag |
Marike Kamphuis, |
| MCH Antoniushove, Leidschendam |
Christa Kerkhof |
| Haga Ziekenhuis, Den Haag |
Nienke Splinter |
| VUMC, Amsterdam |
Antoinette Keulen |
| Diaconessenhuis, Meppel |
Cock Meijs |
| Rivas, Beatrix Ziekenhuis, Gorinchem |
Wieteke Musterd |
| Amphia Ziekenhuis, Breda |
Sylvia Goosen |
|
Rehabilitation centres |
Principal investigator |
| Laurens Antonius, Binnenweg, Rotterdam |
Siri Siepel |
| Laurens Antonius, IJsselmonde, Rotterdam |
Ankerien Gerritse |
| Rijndam, Central clinic, Rotterdam |
Mieke van de Sandt |
| Rijndam, Central outpatient centre, Rotterdam |
Miranda de Waard-van Rijn |
| Rijndam, Vlietland outpatient centre, Schiedam |
Merle Paterson |
| Rijndam, De Waarden outpatient centre, Gorinchem |
Wieteke Musterd |
| Vlietland Ziekenhuis outpatient centre, Schiedam |
Obbe de Roos |
| Centrum voor Reuma en Revalidatie, Rotterdam |
Anke de Meij |
| Maasstad Ziekenhuis outpatient centre, Rotterdam |
Fabiënne Stok |
| Zonnehuis, Vlaardingen |
Suzanne van Almenkerk |
| Sophia Revalidatie, Delft |
Marjolein Zomerdijk |
| Stichting Pieter van Foreest, Delft |
Margot van Vorstenbosch |
| Sophia Revalidatie, Den Haag |
Elske van Egmond |
| Florence, Gulden Huis, Den Haag |
Charlotte Schmitz |
| Florence, Huize Westhoff, Rijswijk |
Charlotte Schmitz |
| Florence, Mariahoeve, Den Haag |
Charlotte Schmitz |
| Zonnehuis, Amstelveen |
Jan van Olsthoorn |
| Reade, Amsterdam |
Laurien Sietsma |
| De Volckaert-SBO, Oosterhout |
Marianne Slabbekoorn |
| Stichting Elisabeth, Breda |
Judith van Bree |
| Thebe Aeneas, Breda |
Cirsten van Gelder |
| De Riethorst-Stromenland, Geertruidenberg |
Cirsten van Gelder |
| Stichting Bilthuysen, De Biltse Hof, Bilthoven |
Melanie Swens |
| Zorgcombinatie Noorderboog, Reggersoord, Meppel |
Nelleke Loseman |
| Stichting Groenhuysen, Roosendaal |
Saskia Aarts |
| Avoord Zorg en Wonen, Etten-Leur |
Nancy Schuurman |
| Stichting SHDH, Janskliniek, Haarlem |
Annet Voogd |
| Stichting Afasietherapie, Amsterdam |
Marieta Gerarts |
| Rivas, Waerthove, Sliedrecht |
Wieteke Musterd |
| Rivas, Lingesteijn, Leerdam |
Wieteke Musterd |
| Rivas, Het Gasthuis, Gorinchem | Wieteke Musterd |
Abbreviations
ANELT: Amsterdam-Nijmegen everyday language test; CAT: Comprehensive aphasia test; CLT: Cognitive linguistic treatment; MAAS: Multi-axial aphasia system; PACE: Promoting Aphasics’ Communicative Effectiveness; PALPA: Psycholinguistic assessment of language production in aphasia; RATS-3: Rotterdam aphasia therapy study – 3; SAT: Semantic association test; SLT: Speech and language therapy; SL-therapist: Speech and language therapist.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
DD, PK, MJ, EV and LL conceived the study and designed this trial. LL is the principal investigator and FN is the trial coordinator. EV, MJ and FN will acquire the data, which FN will primarily analyse and interpret. LL and FN wrote the first draft of the manuscript, which was critically revised by MJ, EV, DD and PK. All authors have read and approved the final manuscript.
Authors’ information
MJ, DD, PK and EV conducted the preceding RATS-2 study in which the efficacy of impairment directed language therapy was tested in comparison to communicative therapy [6]. MJ initiated RATS-3 and started data collection. From 1 January 2012, FN has taken over the coordinating tasks of MJ.
Contributor Information
Femke Nouwens, Email: f.nouwens@erasmusmc.nl.
Diederik WJ Dippel, Email: d.dippel@erasmusmc.nl.
Marjolein de Jong-Hagelstein, Email: m.hagelstein@erasmusmc.nl.
Evy G Visch-Brink, Email: e.visch-brink@erasmusmc.nl.
Peter J Koudstaal, Email: p.j.koudstaal@erasmusmc.nl.
Lonneke M L de Lau, Email: l.delau@erasmusmc.nl.
Acknowledgements
We thank Mieke van de Sandt-Koenderman, PhD; Marion Smits, PhD and Carolina Mendez Orellana, MSc for their suggestions and collaboration. We appreciate the help of Hester Lingsma, PhD with methodological and statistical issues. We would like to thank all local SL-therapists who will actively participate in this trial. This study is financially supported by a fellowship of Hersenstichting Nederland (Dutch foundation for brain research) granted to LL.
References
- Vaartjes I, van Dis I, Visseren FLJ, Bots ML. In: Cardiovascular Diseases in The Netherlands in 2011. Facts on Lifestyle and Risk Factors. Vaartjes I, Dis I, Visseren FLJ, Bots ML, editor. Den Haag: Dutch Heart Foundation; 2011. Cardiovascular diseases in The Netherlands in women and men; pp. 7–22. [Google Scholar]
- Bowen A, Hesketh A, Patchick E, Young A, Davies L, Vail A, Long A, Watkins C, Wilkinson M, Pearl G, Lambon Ralph M, Tyrrell P. ACT NoW investigators. Clinical effectiveness, cost-effectiveness and service users’ perceptions of early, well-resourced communication therapy following a stroke: a randomised controlled trial (the ACT NoW Study) Health Technol Assess. 2012;16:1–160. doi: 10.3310/hta16260. [DOI] [PubMed] [Google Scholar]
- Brady MC, Kelly H, Godwin J, Enderby P. Speech and language therapy for aphasia following stroke. Cochrane Database Syst Rev. 2012;5:CD000425. doi: 10.1002/14651858.CD000425.pub3. [DOI] [PubMed] [Google Scholar]
- Visch-Brink EG, Wielaert S. Impairment directed therapy and/or communicative therapy for impaired functions in aquired aphasia? Stem-, Spraak- en Taalpathol. 2005;13:153–173. [Google Scholar]
- Davis GA, Wilcox MJ. Adult Aphasia Rehabilitation: Applied Pragmatics. San Diego, CA: Singular; 1985. [Google Scholar]
- de Jong-Hagelstein M, van de Sandt-Koenderman WM, Prins ND, Dippel DW, Koudstaal PJ, Visch-Brink EG. Efficacy of early cognitive-linguistic treatment and communicative treatment in aphasia after stroke: a randomised controlled trial (RATS-2) J Neurol Neurosurg Psychiatry. 2011;82:399–404. doi: 10.1136/jnnp.2010.210559. [DOI] [PubMed] [Google Scholar]
- Blomert L, Koster C, Kean ML. Amsterdam-Nijmegen Everyday Language Test. Lisse, The Netherlands: Swets & Zietlinger; 1995. [Google Scholar]
- Bhogal SK, Teasell R, Speechley M. Intensity of aphasia therapy, impact on recovery. Stroke. 2003;34:987–993. doi: 10.1161/01.STR.0000062343.64383.D0. [DOI] [PubMed] [Google Scholar]
- Cherney LR, Patterson JP, Raymer AM. Intensity of aphasia therapy: evidence and efficacy. Curr Neurol Neurosci Rep. 2011;11:560–569. doi: 10.1007/s11910-011-0227-6. [DOI] [PubMed] [Google Scholar]
- Robey RR. A meta-analysis of clinical outcomes in the treatment of aphasia. J Speech Lang Hear Res. 1998;41:172–187. doi: 10.1044/jslhr.4101.172. [DOI] [PubMed] [Google Scholar]
- Teasell R, Bitensky J, Salter K, Bayona NA. The role of timing and intensity of rehabilitation therapies. Top Stroke Rehabil. 2005;12:46–57. doi: 10.1310/ETDP-6DR4-D617-VMVF. [DOI] [PubMed] [Google Scholar]
- Saur D, Lange R, Baumgaertner A, Schraknepper V, Willmes K, Rijntjes M, Weiller C. Dynamics of language reorganization after stroke. Brain. 2006;129:1371–1384. doi: 10.1093/brain/awl090. [DOI] [PubMed] [Google Scholar]
- Pulvermuller F, Berthier ML. Aphasia therapy on a neuroscience basis. Aphasiology. 2008;22:563–599. doi: 10.1080/02687030701612213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Code C. Multifactorial processes in recovery from aphasia: developing the foundations for a multileveled framework. Brain Lang. 2001;77:25–44. doi: 10.1006/brln.2000.2420. [DOI] [PubMed] [Google Scholar]
- Berthier ML, Garcia-Casares N, Walsh SF, Nabrozidis A, Ruíz de Mier RJ, Green C, Dávila G, Gutiérrez A, Pulvermüller F. Recovery from post-stroke aphasia: lessons from brain imaging and implications for rehabilitation and biological treatments. Discov Med. 2011;12:275–289. [PubMed] [Google Scholar]
- Cicerone KD, Dahlberg C, Malec JF, Langenbahn DM, Felicetti T, Kneipp S, Ellmo W, Kalmar K, Giacino JT, Harley JP, Laatsch L, Morse PA, Catanese J. Evidence-based cognitive rehabilitation: updated review of the literature from 1998 through 2002. Arch Phys Med Rehabil. 2005;86:1681–1692. doi: 10.1016/j.apmr.2005.03.024. [DOI] [PubMed] [Google Scholar]
- Berthier ML, Pulvermuller F. Neuroscience insights improve neurorehabilitation of poststroke aphasia. Nat Rev Neurol. 2011;7:86–97. doi: 10.1038/nrneurol.2010.201. [DOI] [PubMed] [Google Scholar]
- Godecke E, Hird K, Lalor EE, Rai T, Phillips MR. Very early poststroke aphasia therapy: a pilot randomized controlled efficacy trial. Int J Stroke. 2012;7:635–644. doi: 10.1111/j.1747-4949.2011.00631.x. [DOI] [PubMed] [Google Scholar]
- Laska AC, Kahan T, Hellblom A, Murray V, von Arbin M. A randomized controlled trial on very early speech and language therapy in acute stroke patients with aphasia. Cerebrovasc Dis Extra. 2011;1:66–74. doi: 10.1159/000329835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El Hachioui H, Sandt-Koenderman MW, Dippel DW, Koudstaal PJ, Visch-Brink EG. The ScreeLing: occurrence of linguistic deficits in acute aphasia post-stroke. J Rehabil Med. 2012;44:429–435. doi: 10.2340/16501977-0955. [DOI] [PubMed] [Google Scholar]
- De Renzi E, Faglioni P. Normative data and screening power of a shortened version of the Token Test. Cortex. 1978;14:41–49. doi: 10.1016/s0010-9452(78)80006-9. [DOI] [PubMed] [Google Scholar]
- Goodglass H, Kaplan E. The Assessment of Aphasia and Related Disorders. Philadelphia, PA: Lea and Febiger; 1972. [Google Scholar]
- Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md State Med J. 1965;14:61–65. [PubMed] [Google Scholar]
- van de Sandt-Koenderman WM, van Harskamp F, Duivenvoorden HJ, Remerie SC, van der Voort-Klees YA, Wielaert SM, Ribbers GM, Visch-Brink EG. MAAS (Multi-axial Aphasia System): realistic goal setting in aphasia rehabilitation. Int J Rehabil Res. 2008;31:314–320. doi: 10.1097/MRR.0b013e3282fc0f23. [DOI] [PubMed] [Google Scholar]
- Visch-Brink EG, Bajema IM. BOX, a Semantic Therapy Program. Lisse, The Netherlands: Swets & Zeitlinger; 2001. [Google Scholar]
- Van Rijn M, Booy L, Visch-Brink EG. FIKS, a Phonological Therapy Program. Lisse, The Netherlands: Swets & Zeitlinger; 2000. [Google Scholar]
- Van Sabadel EP, Signoret JL, Pillon B. Unusual Stories for Conversation. Paris: Médecine et Sciences Internationales; 1982. [Google Scholar]
- Visch-Brink EG, Van de Sandt-Koenderman M. El Hachioui H: ScreeLing. Houten: Bohn Stafleu van Loghum; 2010. [Google Scholar]
- Kaplan E, Goodglass H, Weintraub S. Boston Naming Test. Philadelphia-Tokyo: Lippincott, Williams & Wilkins; 2001. [Google Scholar]
- Visch-Brink EG, Stronks DL, Denes G. The Semantic Association Test. Amsterdam: Harcourt Assessment B.V; 2005. [Google Scholar]
- Swinburn K, Porter G, Howard D. Comprehensive Aphasia Test. New York, NY: Psychology Press; 2004. [Google Scholar]
- Luteijn F, Barelds DPF. Groningen Intelligence Test - 2; GIT - 2. Amsterdam: Pearson Assessment and Information B.V; 2004. [Google Scholar]
- Kay J, Lesser R, Coltheart M. Psycholinguistic Assessment of Language Processing in Aphasia (PALPA) London: Lawrence Erlbaum Associates; 1992. [Google Scholar]
- Schmand B, Groenink SC, Van den Dungen M. Letter fluency: psychometric properties and Dutch standards. Tijdschr Gerontol Geriatr. 2008;39:65–77. doi: 10.1007/BF03078128. [DOI] [PubMed] [Google Scholar]
- Blomert L. Who’s the “expert”? Amateur and professional judgement of aphasic communication. Top Stroke Rehabil. 1995;2:64–71. doi: 10.1080/10749357.1995.11754081. [DOI] [PubMed] [Google Scholar]
- The EuroQol Group. EuroQol–a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988;19:604–607. doi: 10.1161/01.STR.19.5.604. [DOI] [PubMed] [Google Scholar]
- Graetz P, De Bleser R, Willmes K. Aachen Aphasia Test. Dutch version. Lisse, The Netherlands: Swets & Zeitlinger; 1991. [Google Scholar]
- NVN CBO. Dutch Guideline ‘Diagnostics, Treatment and Care for Stroke Patients’. 2009. Available from: http://www.diliguide.nl/document/230.
- Blomert L, Kean ML, Koster C, Schokker J. Amsterdam-Nijmegen everyday language test: construction, reliability and validity. Aphasiology. 1994;8:381–407. doi: 10.1080/02687039408248666. [DOI] [Google Scholar]
- Netherlands Trials Register. http://www.trialregister.nl/trialreg/index.asp.