Abstract
Objectives
We assessed public views about the acceptability of and need for sexually transmitted disease (STD) and sexual health-related educational messaging in local campaigns.
Methods
A 28-item state-added module was included in the 2008 New York Behavioral Risk Factor Surveillance System survey (n=3,751). Respondents rated acceptability of venues/dissemination channels and messaging and agreement with attitudinal/need statements. Additional data were analyzed from a separate state survey with individual county samples (n=36,257). We conducted univariate, bivariate, and multivariable modeling analyses.
Results
Each venue was acceptable to more than three-quarters of respondents (range: 79% for billboards to 95% for teaching STD prevention in high school). All message areas were acceptable to at least 85% of respondents (acceptability rating range: 85% to 97%). More than 70% agreed that there is a need for more open discussion about STDs. Bivariate analyses identified areas where messaging tailored to specific subgroups may be helpful (e.g., 26% of white people, 44% of African Americans, and 45% of Hispanic people agreed with the statement, “I need ideas about how to talk to my partner about protection from STDs”). Little geographic variation was seen. Results of multivariable modeling on opposition showed limited interaction effects.
Conclusion
These data provide key information about current community norms and reflect the public's approval for hearing and seeing more about sexual health and STDs in a range of public forums.
In New York State (NYS), sexually transmitted diseases (STDs) represent more than two-thirds of reported communicable disease, with the highest rates found in adolescents and young adults.1 Previous state-level behavioral surveillance found that (1) many New Yorkers greatly underestimated the level of STDs in their community, (2) a high number had rarely or never been asked about their sexual history during routine check-ups, and (3) important STD-related knowledge gaps exist.2 Given these trends, the Bureau of STD Prevention and Epidemiology at the New York State Department of Health (NYSDOH) AIDS Institute identified increased public awareness about STD prevention as a priority goal. In a 2006 telephone survey, 96% of New York respondents felt that public health services were an important priority for New York, with preventing the spread of infectious diseases (e.g., tuberculosis, measles, flu, and acquired immunodeficiency syndrome [AIDS]) as the most important role of public health (99%).3 However, the acceptability of STD-related and sexual health educational messaging in terms of community norms has not been examined.
It is a common perception that sexual health issues represent a sensitive topic about which people do not want to hear or talk. The 1997 Institute of Medicine report on STDs, entitled “The Hidden Epidemic,” indicated that STDs are hidden from public view at least partly because Americans do not address sexual health issues openly.4 Limited research has been conducted on public attitudes toward open discussion about STDs at the community level, especially regarding perceptions of the need for public discourse on STDs and which messages are acceptable for public venues. One exception is in the area of topics that Americans feel should be taught as part of sex education in schools. An in-depth National Public Radio/Kaiser/Kennedy School survey of American parents and school principals found strong support for sex education in schools.5 More recent polls, including one in NYS, found a high level of support for comprehensive sex education in school settings.6–11 Yet, local opponents, even when representing a minority view, have successfully used social and political communications to challenge implementation in numerous local communities.12 Beyond the limited focus of research about school settings, few studies have looked at either the acceptability of using other community venues or the norms for STD education in the general population.
Results of research meta-analyses of press coverage of STD-related topics document that messaging related to STDs is most frequently presented in a stigma frame.13,14 In addition, numerous examples exist of press coverage of STD-related or sexual health campaigns, including coverage of media campaigns where sexual health content was rejected for placement by advertisers or even pulled after posting.15–19 To aid in effective prevention planning, it is critical to better understand what approaches are acceptable to the public in terms of messages and venues for local education campaigns. The NYSDOH Bureau of STD Prevention and Epidemiology conducted this assessment to obtain key information needed to appropriately tailor its STD prevention efforts to community needs and communication preferences.
METHODS
Data sources included two statewide surveys. In 2008, NYSDOH included a Behavioral Risk Factor Surveillance System (BRFSS) state-added module with 28 questions exploring public knowledge and attitudes related to local STD educational campaigns. BRFSS is a Centers for Disease Control and Prevention (CDC)-supported annual telephone survey with core questions administered by all states. State health departments may fund state-specific questions about risk behaviors and preventive health practices when jurisdiction-level information is needed. The cross-sectional telephone survey (data collection occurred from January–-December 2008) used disproportionate stratified random sampling with weighting that allows generalization of data to each state's population. The STD module was administered to a statewide representative sample of the noninstitutionalized adult (aged 18 years and older) population.
As shown in Table 1, final demographic variables used for the analysis included gender, five levels of age, three racial/ethnic groups (white, African American, and Hispanic), three education levels, six levels of annual household income, marital status (single or married/member of unmarried couple), and region (New York City [NYC] and NYS excluding NYC). Due to limited numbers, respondents from five additional race categories (Asian, Native Hawaiian/other Pacific Islander, American Indian/Alaska native, other race, and multiracial) were included only in the univariate analyses.
Table 1.
Demographic characteristics of study sample: NYS BRFSS 2008 state-added modulea
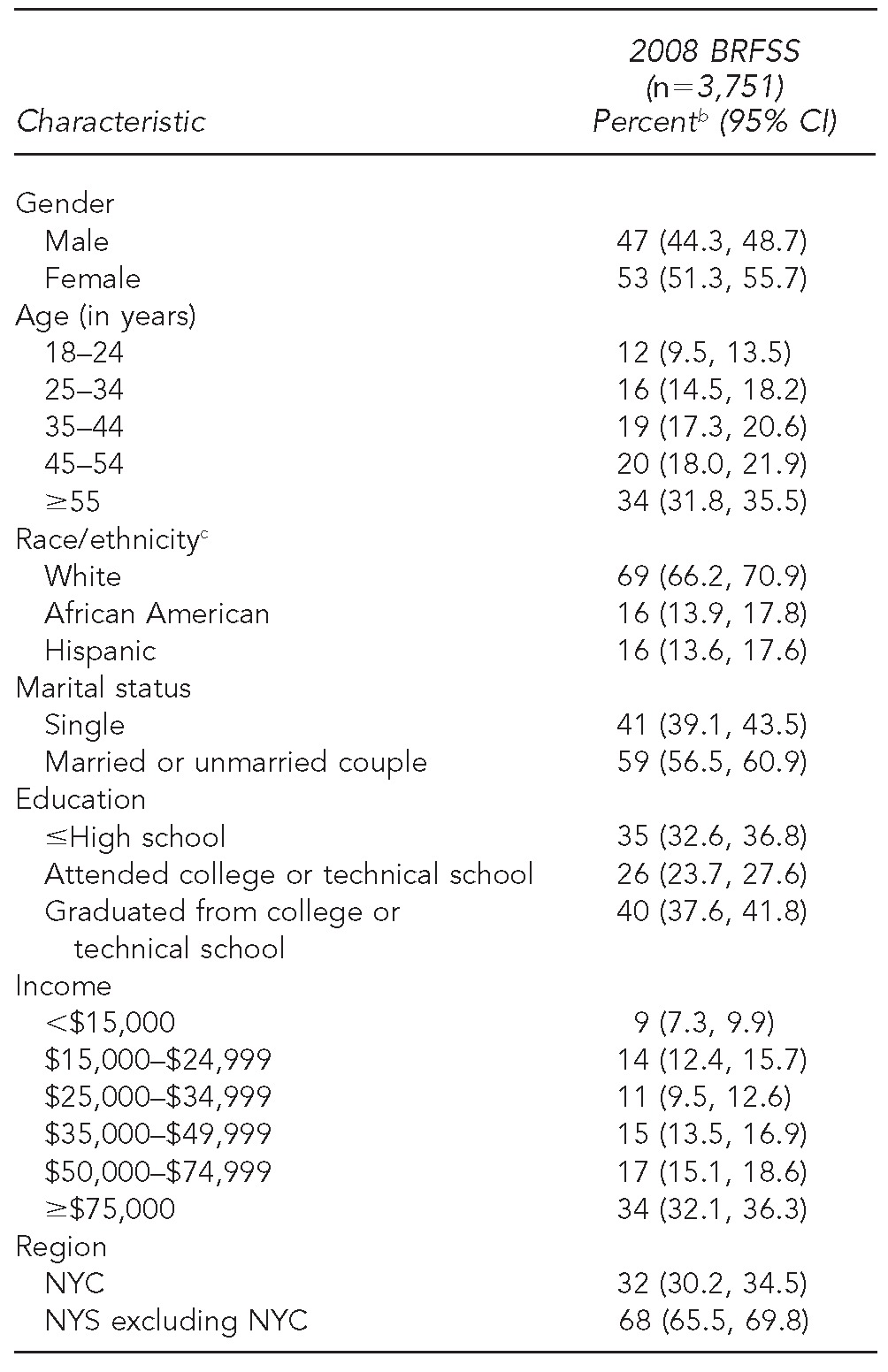
aThe NYS BRFSS is administered annually to a statewide representative sample of noninstitutionalized adults aged 18 years and older. In 2008, it included a 28-item module assessing public knowledge and attitudes related to local sexually transmitted disease educational campaigns.
bPercentages may not total 100% due to rounding.
cN shown for race/ethnicity = 3,532 (219 respondents from five additional racial/ethnic categories—Asian, Native Hawaiian/other Pacific Islander, American Indian/Alaska native, other race, and multiracial—were included only in the univariate analyses).
NYS = New York State
BRFSS = Behavioral Risk Factor Surveillance System
CI = confidence interval
NYC = New York City
Nineteen questions were included on the state-specific module examining the acceptability of specific venues/dissemination channels and messages for an STD campaign. These questions were prefaced by an introductory statement to transition from the prior topic of the survey: “The next set of questions is about people's knowledge and attitudes regarding sexually transmitted diseases or STDs. As you may know, sexually transmitted diseases are diseases that can be passed from person to person by having sex. They include diseases such as gonorrhea, chlamydia, syphilis, herpes, HIV, and others. There are many choices about how best to get the word out about STDs in any community. We'd like to know how and where the public feels education on STD prevention and STD risk should be offered.”
Respondents were specifically asked how acceptable it was to use each of eight specific venues in their county: television, radio, newspaper, transit ads, billboards, middle school, high school, and public places where brochures may be displayed (Table 2). The interviewer next asked about respondents' views on 11 specific messages that have been used in STD education campaigns in other places, and how acceptable it would be to include this type of information in a local publicity campaign reaching adolescents and adults in their county. Message content ranged from less explicit (e.g., “information on the level and rates of STDs here in your county”) to more explicit (e.g., “ideas on how to ask a partner or spouse to start using condoms” or “the increased STD risks for men who have sex with men”). Response options for both venue and message acceptability used a five-point Likert scale (1 = not acceptable, 2 = rarely acceptable, 3 = somewhat acceptable, 4 = acceptable, and 5 = very acceptable).
Table 2.
Acceptability of specific STD educational campaign venues and messages to New York State residents aged >18 years: BRFSS 2008a
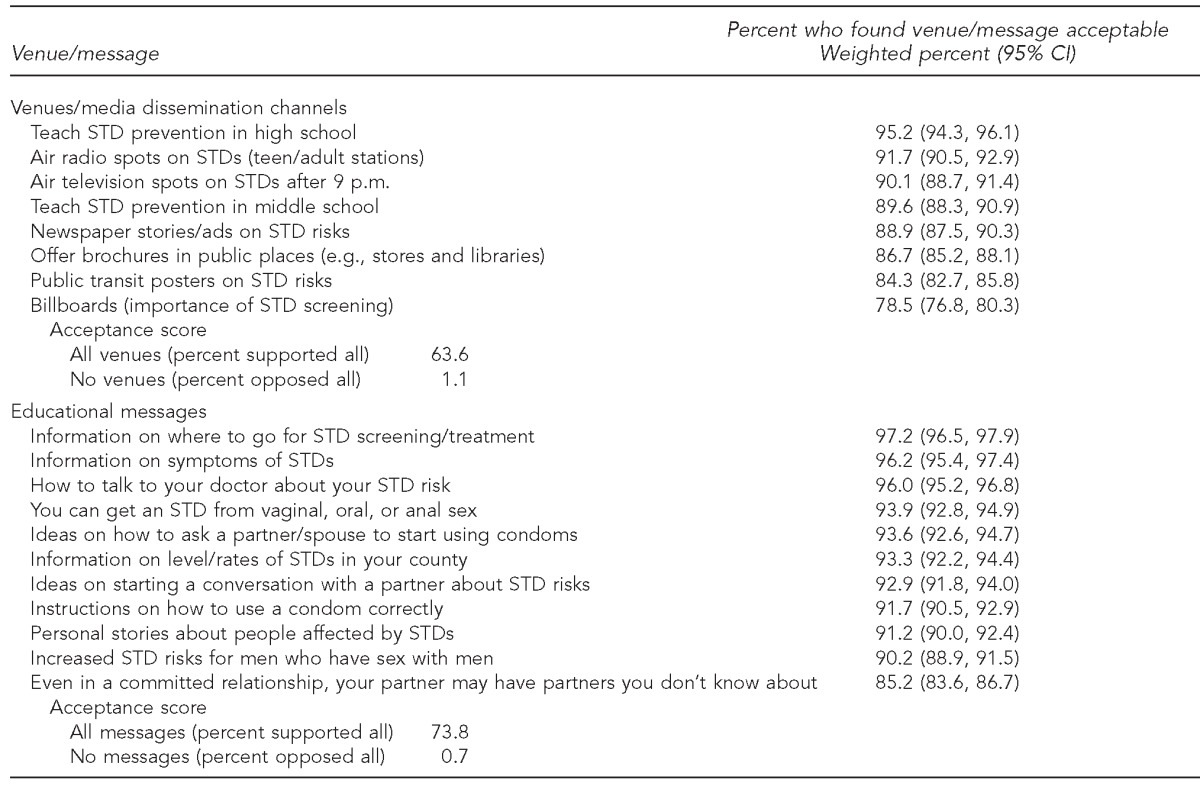
aN ranged from 3,582 (6,445,551 weighted frequency) to 3,678 (6,648,180 weighted frequency), depending on the question.
STD = sexually transmitted disease
BRFSS = Behavioral Risk Factor Surveillance System
An additional seven questions examined the perceived need for STD education. It was prefaced by the statement: “People have different comfort levels and beliefs about how and where an issue like sexually transmitted diseases—STDs—should be talked about.” Respondents were asked how much they agreed or disagreed with each statement, using a five-point Likert scale (1 = completely disagree, 2 = somewhat disagree, 3 = neither agree nor disagree, 4 = somewhat agree, and 5 = completely agree). This section included four questions on perceived community need (e.g., “There needs to be more open discussion in our community about the risks and problem of STDs”) and three questions related to personal need/comfort (e.g., “I need some ideas about how to talk with my sex partner about protection from STDs”) (Table 3). Finally, two awareness/knowledge questions were included. The first question was, “How many people in your community who are your age do you think have had an STD?” Respondents selected from four answer options (hardly any [0–1 out of 10], a few [2–3 out of 10], about half [4–6 out of 10], and all or almost all [9–10 out of 10]). The second question, “Having another STD increases your chances of being infected with HIV,” could be answered with true, false, or don't know.
Table 3.
Knowledge, attitudes, and perceived needs related to STD education among New York State residents aged >18 years: BRFSS 2008a
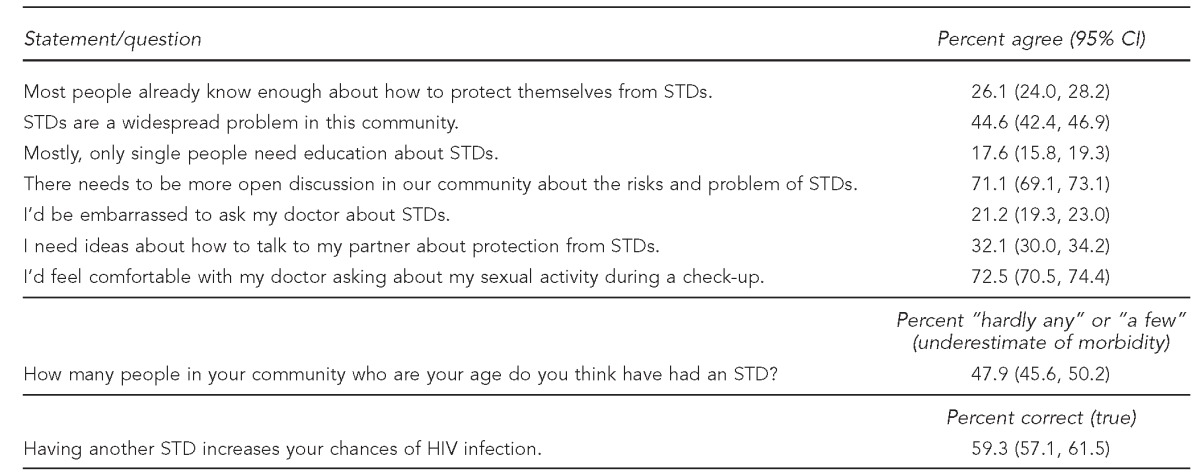
aN ranged from 3,492 (6,308,926 weighted frequency) to 3,557 (6,396,857 weighted frequency) depending on the question.
STD = sexually transmitted disease
BRFSS = Behavioral Risk Factor Surveillance System
CI = confidence interval
HIV = human immunodeficiency virus
In addition to the aforementioned questions included on the 2008 NYS BRFSS, a question was included on the Expanded BRFSS (data collection occurred from July 2008 to June 2009) to fully understand geographic variation (especially rural vs. urban) within the state in support of STD education campaigns. The Expanded BRFSS is a separate NYS survey conducted approximately every five years to augment the annual BRFSS by including 58 separate county-level samples—57 upstate counties plus five NYC counties in a single unit—with approximately 650 interviews conducted in each county. Respondents were asked, “How acceptable is it to you to see and hear public discussion about STD risks in your local media (e.g., TV, radio, and newspaper) and other public forums in your county?” We used the same five-point Likert acceptability scale from the 2008 annual BRFSS.
For the 2008 BRFSS, CDC's National Center for Chronic Disease Prevention and Health Promotion's Behavioral Surveillance Branch provided the final edited and weighted data file back to NYSDOH, to ensure that uniform criteria for post-stratification weighting were used across data collected by different jurisdictions. Further analyses were performed using SAS® version 9.2 using sampling weights and strata appropriate for the survey design.20
Univariate analyses for the 2008 BRFSS described the proportion of respondents who found each venue and message acceptable and who agreed with each perceived need statement. For the Expanded BRFSS, acceptance of public discussion of STDs within each county was analyzed. On both surveys, for items using the acceptability scale, responses in the three highest acceptance categories (somewhat acceptable, acceptable, and very acceptable) were collapsed (and coded as 1) and the two lowest acceptance categories (rarely acceptable and not acceptable) were collapsed (and coded as 0). The decision to code the middle category as part of the acceptable responses was made after reviewing the distribution of responses. This category was the smallest of the acceptable options for every question (ranging from 5%–18%), and because it was read to respondents as somewhat acceptable, it was grouped with the other two acceptable options. For the perceived need items, agree or strongly agree responses were combined, and disagree, strongly disagree, and neither agree nor disagree responses were combined. Acceptance scores were created by summing the number of acceptable venues and by summing the number of acceptable messages from the 2008 BRFSS to examine the score distributions.
Bivariate analyses examined the relationship between demographic factors and acceptability ratings of individual venues and messages and the attitudes/perceived need questions using prevalence ratios and 95% confidence intervals (CIs).
We performed multivariable logistic regression using the SAS Survey Logistic Procedure. The relationship between demographic factors and opposition (e.g., those opposing at least one venue and those opposing at least one message) was modeled against age (18–34 years vs. ≥35 years), gender, income (<$35,000 vs. ≥ $35,000), education (college graduate vs. other), region, and marital status. This relationship was also modeled for those who agreed that, “I would be embarrassed to ask my doctor about STDs.” The final models included only those predictors of p<0.05.
RESULTS
The 2008 BRFSS survey containing the sexual health module was administered to 3,751 respondents statewide. The refusal rate (i.e., the proportion of eligible respondents who refused to complete an interview or terminated prior to the partial interview threshold) was 19%. The response rate (i.e., the number of complete and partial interviews in the numerator and an estimate of the number of eligible units in the sample in the denominator) was 40%.
Table 2 presents findings on the acceptability of specific STD education campaign venues and message content. Each venue was acceptable to more than three-quarters of all respondents, with the acceptability level for specific venues ranging from 79% (for billboards) to 95% (for teaching STD prevention in high school). Each of the 11 message areas was acceptable to at least 85% of respondents, with the acceptability level for individual messages ranging from 85% (for “even in a committed relationship, your partner may have partners you don't know about”) to 97% (for “information on where to go for STD screening/treatment”). More explicit messages were rated similarly to what would be considered fairly standard message areas (e.g., “information on levels/rates of STDs in your county”). More explicit message areas included “ideas on how to ask a partner/spouse to start using condoms,” “ideas on starting a conversation with your partner about STD risks,” and “instructions on how to use a condom correctly.” The percentages of respondents that found all venues (63.6%) and all messages (73.8%) acceptable as well as no venues (1.1%) and no messages (0.7%) acceptable are also shown. There was little consistency in which venues and messages were rejected across respondents.
Table 3 shows the findings on selected knowledge, attitudes, and perceived needs related to STD education. There was a strong perceived need at the community level for education, with only 26.1% agreeing that “most people already know enough about how to protect themselves from STDs” and 17.6% indicating that “.. . only single people need education about STDs.” The majority of respondents (71.1%) agreed that “there needs to be more open discussion in our community about the risks and problems of STDs” (9.4% disagreed, 15.9% were neutral, 2.5% answered “don't know/not sure,” and 1.0% did not respond). The background rates for ever having had an STD were underestimated, with almost half (47.9%) saying that “hardly any” or “only a few” people in the community in their same age have had an STD. In terms of comfort in discussing sexual health issues with their doctor, 21.2% of respondents said they would be embarrassed to ask their doctor about STDs, and most (72.5%) indicated they would be comfortable with their doctor asking about sexual activity during a check-up.
Bivariate analyses on individual items found significant differences among subgroups, particularly for messages and specific attitudes/perceived needs. Given the large sample size and the high overall level of acceptability/agreement, a number of these differences were statistically significant for all six covariates. Most differences seen were not particularly meaningful, often reflecting differences of only a few percentage points. However, several of the statistically significant findings are notable. For example, while overall less than half of the sample (44.6%) agreed that “STDs are a widespread problem in this community” (Table 3), there were significant differences by race/ethnicity (37% for white people, 62% for African Americans, and 58% for Hispanic people, data not shown). While one-third (32.1%) of respondents overall agreed that “I need ideas about how to talk to my partner about protection from STDs” (Table 3), only 26% of white people agreed, compared with 44% of African Americans and 45% of Hispanic people (data not shown). The lowest income group (where 59% agreed) differed significantly from the highest income group (where 22% agreed) on this item. Income and education were particularly significant for additional measures, including “I'd be embarrassed to ask my doctor about STDs (e.g., 39% in the lowest income group vs. 15% in the highest income group agreed with this statement, data not shown).
Results of multivariable modeling on opposition showed no significant interaction effects among demographic groups. For venues, white people (odds ratio [OR] = 1.6, 95% CI 1.2, 2.1) were more likely and college graduates (OR=0.73, 95% CI 0.6, 0.9) were less likely to oppose one or more venues. For messages, only gender was significant (OR=0.7, 95% CI 0.5, 0.8), with females being less likely than males to oppose one or more messages. Younger respondents aged 18–34 years were more likely to feel embarrassed to ask their doctor about STDs (OR=1.4, 95% CI 1.0, 2.1) than those aged ≥ 35 years. White people (OR=0.7, 95% CI 0.5, 0.9) and college graduates (OR=0.6, 95% CI 0.5, 0.8) were least likely to be embarrassed to ask their doctor about STDs (data not shown).
Finally, the Expanded BRFSS question was completed by 36,257 respondents statewide. The refusal and response rates varied by county (range: 16%–24% refusal rate; 34%–53% response rate). The proportion of respondents in individual counties who thought it was at least somewhat acceptable to see and hear public discussion about STD risks in local media (e.g., television, radio, or newspaper) and other public forums in the county ranged from 80% to 96% (median: 90%; interquartile range 88%, 93%). Statewide, acceptability was 90% (95% CI 88.2%, 91.3%). Mean acceptability was 88.4% for the 26 counties in NYS designated as rural by the Health Resources and Services Administration Office of Rural Health Policy (all data not shown).
DISCUSSION
In the area of sexual health, it is not uncommon for health departments sponsoring STD-related education campaigns to hear from a small number of highly vocal critics who strongly object to messaging in those campaigns. Having clear survey data on broader community attitudes among the state's citizens provides a context for understanding how representative those opponents are of citizens' views. While achieving full public consensus on any issue is unrealistic, it is interesting to consider what level of opposition is significant enough to lead to a decision not to air specific messaging or to use specific dissemination channels/venues. Further discussion is needed regarding where one draws the line for public discourse related to sexual health campaigns. In the case of these survey data, a large majority of the citizenry was in support of such campaigns.
Survey results identified several areas where perceived need for STD education (e.g., those wanting ideas on how to start a conversation with their partner about STDs) was higher for specific subgroups. In addition, those at higher risk of STDs (e.g., people <35 years of age) were more likely to feel embarrassed to ask their doctor about STDs. The sophistication of media channels today allows for tailoring health information, so these details are useful in prioritizing and tailoring prevention efforts.
NYS has continued to include new state-added sexual behavior questions on its BRFSS to aid in prevention planning. For example, the 2012 cycle includes the question, “Starting at what age do you think parents should begin to talk with their child about sexuality and ways to prevent (teen) pregnancy and sexually transmitted diseases?,” and the previous cycle includes a question on whether respondents “support or oppose a government information program to promote safe sex practices, such as the use of condoms.” It may be useful for other states to conduct this type of assessment to better understand the level of support for public health campaigns among their own citizenry. There may well be key regional differences in social norms related to discussing STDs or sexual health, with findings that may differ significantly from the NYS survey.
Limitations
There were important limitations to the findings. Coverage bias (e.g., no cell phone sample for this specific section of the survey) and nonresponse bias are important considerations in survey research, especially with the falling response rates in telephone surveys. Recent studies have found that the relationship between nonresponse rates and actual nonresponse bias is complex, and it is not possible to establish the degree of potential bias in these specific data.21,22 In terms of survey scope, we tested acceptability of general areas of message content, and additional research would be needed to confirm the acceptability of detailed messages (including testing both graphics and words) that are proposed for a specific campaign. The fact that we did not directly ask if such a campaign was needed, only what would be acceptable components, was also a limitation. The BRFSS also did not collect information on factors such as political affiliation, religiosity, or other social values, which other researchers23 have identified as impacting policy preferences related to sex education, and which might have moderated some of the differences seen (e.g., by race/ethnicity) if they had been able to be included in the analyses. Finally, social media channels were not included in the list of venues/dissemination channels tested. Acceptability of these channels for STD-related messaging has, however, been included in a subsequent BRFSS.
CONCLUSION
Across NYS communities, more than 70% of respondents agreed that there should be more open discussion about STDs. A wide range of message content, including more explicit risk information, was found acceptable by a large majority of respondents. These data provide key information about actual community norms concerning acceptable messaging and the public's interest in seeing and hearing more about STD prevention in a range of local public forums. Data can be a critical tool in gaining the support of government stakeholders (e.g., health department leadership, public affairs, and elected officials) for campaigns related to STD prevention and reducing institutional barriers to public education.
Footnotes
The authors thank the Behavioral Risk Factor Surveillance System Unit at the Bureau of Chronic Disease Evaluation and Research, Division of Chronic Disease Prevention, New York State Department of Health (NYSDOH) for management and technical oversight of the administration of both surveys that served as the data collection source for this article. The authors also thank Dr. David Strogatz for statistical consultation. Both study protocols were approved by the NYSDOH Institutional Review Board.
This behavioral surveillance project was supported by the Comprehensive Sexually Transmitted Disease Prevention Systems Projects grant #H25/CCH204318 from the Centers for Disease Control and Prevention (CDC). The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of CDC.
REFERENCES
- 1.New York State Department of Health. 2010. [cited 2012 Aug 29]. 2010 communicable disease annual reports: New York statewide reported cases by disease and county—2010. Available from URL: http://www.health.ny.gov/statistics/diseases/communicable/ [Google Scholar]
- 2.Thomas RP, Bekan-Homawoo B, Coles FB. BRFSS: STD-related behavioral surveillance in New York State. Poster session presented at the National STD Prevention Conference; 2008 Mar 10-13; Chicago. [Google Scholar]
- 3.Research' America. New York residents speak out on public health. 2006. [cited 2012 Sep 10]. Available from: URL: http://www.hanys .org/upload/NYPHreportFINAL.pdf.
- 4.Eng TR, Butler WT, editors. Washington: National Academy Press; 1997. The hidden epidemic: confronting sexually transmitted diseases. [PubMed] [Google Scholar]
- 5.National Public Radio. Sex education in America: an NPR/Kaiser/Kennedy School poll. 2004. Feb 24, [cited 2012 Sep 10]. Available from: URL: http://www.npr.org/templates/story/story.php?storyId=1622610.
- 6.Bleakley A, Hennessy M, Fishbein M. Public opinion on sex education in US schools. Arch Pediatr Adolesc Med. 2006;160:1151–6. doi: 10.1001/archpedi.160.11.1151. [DOI] [PubMed] [Google Scholar]
- 7.Ito KE, Gizlice Z, Owen-O'Dowd J, Foust E, Leone PA, Miller WC. Parent opinion of sexuality education in a state with mandated abstinence education: does policy match parental preference? J Adolesc Health. 2006;39:634–41. doi: 10.1016/j.jadohealth.2006.04.022. [DOI] [PubMed] [Google Scholar]
- 2.Tortolero SR, Johnson K, Peskin M, Cuccaro PM, Markham C, Hernandez BF, et al. Dispelling the myth: what parents really think about sex education in schools. J Appl Res Children. 2011;2(2) [Google Scholar]
- 9.Eisenberg ME, Bernat DH, Bearinger LH, Resnick MD. Support for comprehensive sexuality education: perspectives from parents of school-age youth. J Adolesc Health. 2008;42:352–9. doi: 10.1016/j.jadohealth.2007.09.019. [DOI] [PubMed] [Google Scholar]
- 10.Martinez G, Abma J, Copen C. NCHS Data Brief No. 44. Hyattsville (MD): National Center for Health Statistics; 2010. [cited 2012 Sep 10]. Educating teenagers about sex in the United States. Also available from: URL: http://www.cdc.gov/nchs/data/databriefs/db44.htm. [PubMed] [Google Scholar]
- 2.ReadMedia. Poll shows 84% of New Yorkers support sex education for youth. [cited 2012 Sep 10];2009 Oct 1; Available from: URL: http://readme.readmedia.com/Poll-Shows-85-of-New-Yorkers-Support-Sex-Education-for-Youth/959314. [Google Scholar]
- 12.Irvine JM. Emotional scripts of sex panics. Sex Res Soc Policy. 2006;3:82–94. [Google Scholar]
- 13.Smith R. Media depictions of health topics: challenge and stigma formats. J Health Commun. 2007;12:233–49. doi: 10.1080/10810730701266273. [DOI] [PubMed] [Google Scholar]
- 14.Yoo JH, Jang S. An attributional analysis of stigma associated with sexually transmitted diseases and its relationship with communication efficacy. Glob J Health Sci. 2012;4:15–26. doi: 10.5539/gjhs.v4n4p15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kennedy R. Health ads in bus shelters are pulled after complaints. New York Times. 2001 Jun 27; [Google Scholar]
- 16.McAndrew M. Syracuse Post Standard. New York: Centro won't allow ad naming sexual diseases; 2003. Mar 18, [Google Scholar]
- 17.Chong J-R. Anti-syphilis TV message finds few takers. Los Angeles Times. 2004. Dec 2, [cited 2012 Sep 10]. Available from: URL: http://articles.latimes.com/2004/dec/02/local/me-syphilis2.
- 18.Newman AA. Pigs with cellphones, but no condoms. New York Times. 2007. Jun 18, [cited 2012 Sep 10]. Available from: URL: http://www .nytimes.com/2007/06/18/business/media/18adcol.html.
- 19.CBS Local News. Billboard with giant inflated condom moved after Van Nuys mom complains. 2012. Apr 26, [cited 2012 Sep 10]. Available from: URL: http://losangeles.cbslocal.com/2012/04/26/billboard-with-giant-inflated-condom-moved-after-van-nuys-mom-complains.
- 20.SAS Institute, Inc. SAS®: Version 9.2. Cary (NC): SAS Institute, Inc; 2008. [Google Scholar]
- 21.Schneider KL, Clark MA, Rakowski W, Lapane KL. Evaluating the impact of non-response bias in the Behavioral Risk Factor Surveillance System (BRFSS) J Epidemiol Community Health. 2012;66:290–5. doi: 10.1136/jech.2009.103861. [DOI] [PubMed] [Google Scholar]
- 22.Groves RM. Nonresponse rates and nonresponse bias in household surveys. Public Opin Q. 2006;70:646–75. [Google Scholar]
- 23.Bleakley A, Hennessy M, Fishbein M. Predicting preferences for types of sex education in US schools. Sex Res Soc Policy. 2010;7:50–7. [Google Scholar]


