Abstract
Secondary to leaflet injury, which is a well-known technical mistake, aortic regurgitation can occur during mitral valve replacement or repair. In most cases, the left or the non-coronary cusps are affected. For the first time, we report the case of a patient who had severe aortic regurgitation due to right coronary cusp perforation after mitral valve replacement. This complication was not identified until reoperation. Had transoesophageal echocardiography (TOE) been used during the first procedure, a delayed reoperation could have been avoided. During mitral surgery, every aortic cusp is at risk and peroperative TOE should be a mandatory procedure.
Keywords: Aortic valve injury, Mitral valve surgery, Complication
INTRODUCTION
De novo aortic regurgitation after mitral valve surgery is a rarely reported kind of surgical damage. Classically, aortic regurgitation results from either the perforation or entrapment of an aortic valve cusp by direct stitching or indirectly from aortic annulus distortion caused by sutures retaining the mitral valve [1, 2]. In these cases, the non-coronary and left coronary cusps are affected [1, 2]. Here, we report a right coronary cusp tear after a mitral valve replacement.
CASE REPORT
A 60-year old man who had suffered from symptomatic mitral valve regurgitation due to a huge excess of tissue associated with a complete prolapse of all segments of the mitral valve was treated with mechanical valve replacement in April 2010 at another small case-volume institution. The early postoperative period had been marked by prolonged ventilation, acute renal impairment and complete heart block, necessitating implantation of a pacemaker. Before discharge, a transthoracic echocardiography showed moderate aortic regurgitation. The patient was discharged, but his status progressively deteriorated into functional Class III of the New York Heart Association. In November 2011, surgery was indicated and preoperative workup revealed a well functioning mitral valve prosthesis, severe aortic regurgitation with an altered 45% left ventricular ejection fraction and a mildly dilated left ventricle. On transoesophageal echocardiography (TOE), the right coronary cusp was noticed as being restrictive (Fig. 1). Additionally, the patient demonstrated pulmonary hypertension at 60 mmHg with a Grade III tricuspid insufficiency and a 42-mm diameter annulus dilatation. The angiocoronarography demonstrated an absence of coronary lesions. The supra aortic angiography showed aortic regurgitation of Grade III–IV and the absence of aortic enlargement. Calculated additive EuroSCORE was 10. Intraoperatively, the aortic valve was tricuspid, without calcification. There was a fibrous band crossing the left outflow tract from the prosthetic mitral annulus to the right coronary cusp (Fig. 2) associated with a perforation of about 1 cm² in the right coronary cusp. During the surgical procedure, the valvular apparatus was resected and the fibrous band was cut. The wall of the aorta in the sinus area appeared very thin, but there was no root dilatation or coronary ostia displacement. A 22 aortic mechanical bileaflet was implanted in the supra annular position, and a 34 tricuspid annuloplasty was added. Shortly after unclamping of the aorta, a strong bleeding in the posterior aspect of the aorta led to a bailout Bentall procedure for the aortic annulus tearing at the level of the left non-coronary commissure. Weaning of bypass was not possible without central extracorporeal membrane oxygenation. The patient died of multiorgan failure after 36 h of assistance.
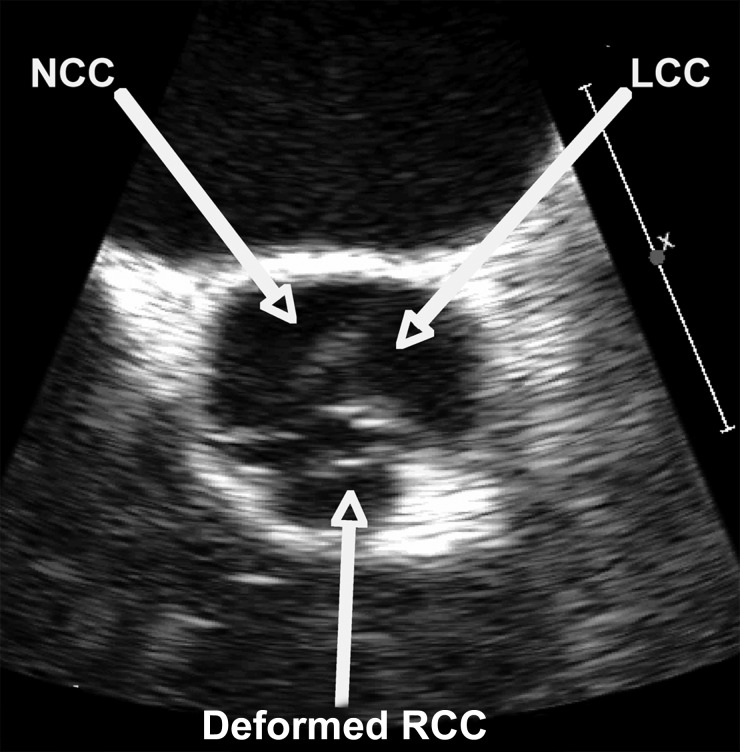
Figure 1:
Preoperative transoesophageal echocardiography (TOE), short-axis view, 59° showing a deformed restrictive right coronary cusp (RCC). LCC: left coronary cusp; NCC: non-coronary cusp.
Figure 2:
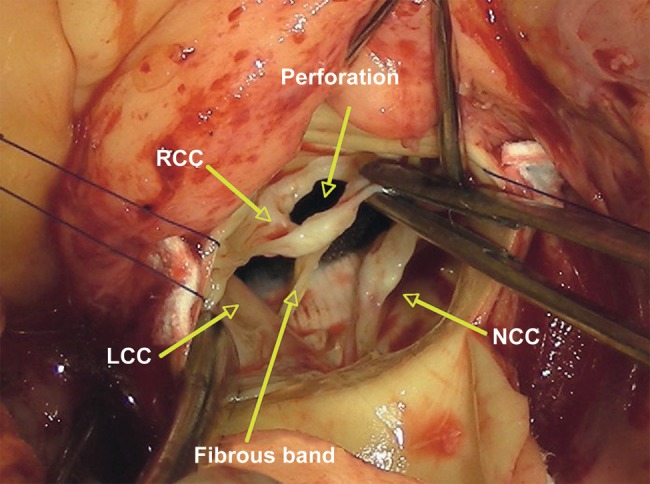
Peroperative view showing the perforation of right coronary cusp (RCC) and the fibrous band binding the mitral mechanical prosthesis annulus to the RCC. LCC: left coronary cusp; NCC: non-coronary cusp.
DISCUSSION
Suture-related injury to the aortic valve should always be considered and excluded when surgical corrections of adjacent cardiac structures are performed. We report, here, to our knowledge for the first time, a patient who had severe aortic regurgitation after mitral valve replacement caused by a perforation of the right coronary cusp. During mitral surgery, great care is mandatory when stitching at the base of the anterior leaflet. Manoeuvres such as pushing the aortic root from outside towards the mitral valve to improve exposure must not be used as this increases the risk of aortic valve injury. During this procedure, a stitch had tackled the right coronary cusp (RCC). The resulting aortic insufficiency had not been recognized as aortic cusp-related as no TOE had been performed. Nevertheless, TOE has been notified as a Class IIa recommendation during mitral replacement and allows the detection of technical problems such as paravalvular regurgitation, abnormal leaflet motion or tethering of a cusp of the aortic valve with a suture placed in the mitral annulus [3]. The American Society of Anesthesiologists and the Society of Cardiovascular Anesthesiologists have stated that for adult patients without contraindications, TOE should be used in all open-heart (e.g. valvular) procedures [4]. In this case, the entrapment of the RCC was not suspected until the TOE was performed before the redo procedure.
To avoid such a how-not-to-do-it case when referring a patient for mitral insufficiency, one has to take into account local resources, particularly in the case of procedures such as complex valve repair, and not hesitate to transfer the patient to a more specialized centre [5]. Finally, one should keep in mind that, during mitral surgery, every aortic cusp is at risk, thus making peroperative TOE a mandatory procedure.
Conflict of interest: none declared.
REFERENCES
- 1.Hill AC, Bansal RC, Razzouk AJ, Liu M, Bailey LL, Gundry SR. Echocardiographic recognition of iatrogenic aortic valve leaflet perforation. Ann Thorac Surg. 1997;64:684–9. doi: 10.1016/s0003-4975(97)00524-9. doi:10.1016/S0003-4975(97)00524-9. [DOI] [PubMed] [Google Scholar]
- 2.Ducharme A, Courval JF, Dore A, Leclerc Y, Tardif JC. Severe aortic regurgitation immediately after mitral valve annuloplasty. Ann Thorac Surg. 1999;67:1487–9. doi: 10.1016/s0003-4975(99)00230-1. doi:10.1016/S0003-4975(99)00230-1. [DOI] [PubMed] [Google Scholar]
- 3.Bonow RO, Carabello BA, Chatterjee K, de Leon AC, Jr, Faxon DP, Freed MD, et al. Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2008;118:e523–661. doi: 10.1161/CIRCULATIONAHA.108.190748. doi:10.1161/CIRCULATIONAHA.108.190748. [DOI] [PubMed] [Google Scholar]
- 4.American Society of Anesthesiologists and Society of Cardiovascular Anesthesiologists Task Force on Transesophageal Echocardiography. Practice guidelines for perioperative transesophageal echocardiography. An updated report by the American Society of Anesthesiologists and the Society of Cardiovascular Anesthesiologists Task Force on Transesophageal Echocardiography. Anesthesiology. 2010;112:1084–96. doi: 10.1097/ALN.0b013e3181c51e90. doi: [DOI] [PubMed] [Google Scholar]
- 5.Vahanian A, Alfieri O, Andreotti F, Antunes MJ, Barón-Esquivias G, Baumgartner H, et al. Guidelines on the management of valvular heart disease (version 2012): The Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) Eur J Cardiothorac Surg. 2012;42:S1–44. doi: 10.1093/ejcts/ezs455. doi:10.1093/ejcts/ezs455. [DOI] [PubMed] [Google Scholar]