Abstract
Background
Transfer delays for primary percutaneous coronary intervention (PPCI) may increase mortality in patients with ST-segment elevation myocardial infarction (STEMI). We examined the association between door 1 to door 2 (D1D2) time, a measure capturing the entire transfer process, and outcomes in patients undergoing inter-hospital transfer for primary PCI.
Methods and Results
We evaluated the relationship between D1D2 time and the 90 day incidence of death, shock, and heart failure in the sub-set of 2075 (36.1%) of 5745 patients who underwent inter-hospital transfer for PPCI in the APEX-AMI trial. There was no significant difference in the 90 day incidence of death, shock, and heart failure between the transferred and the non-transferred groups (10.3% vs 10.2%, p=0.89). The median difference in symptom to balloon time between the two groups was 45 minutes (229 vs 184, p<0.001). The primary outcome per 30 minute delay was higher for patients with a D1D2 time ≤ 150 minutes (HR 1.19: 95% Confidence Interval [CI], 1.06 to 1.33 p=0.004) but not for D1D2 times > 150 minutes (HR, 0.99: 95% CI, 0.96 to 1.02; p=0.496). The association between longer D1D2 time and worsening outcome was no longer statistically significant after multivariable adjustment.
Conclusion
Longer transfer times were associated with higher rate of death, shock, and heart failure among patients undergoing inter-hospital transfer from PPCI, although this difference did not persist after adjusting for baseline characteristics.
Clinical Trial Registration Information
URL: www.clincaltrials.gov, Unique Identifier: NCT00091637
Keywords: STEMI, Primary PCI, Transfer
Introduction
Early revascularization with either fibrinolysis or primary percutaneous coronary intervention (PPCI) has been shown to improve survival in patients with ST-elevation myocardial infarction (STEMI).1–3 Multiple randomized trials have demonstrated that in STEMI patients presenting to community hospitals, rapid transfer to a PPCI capable center improves outcomes compared to immediate fibrinolysis.4–7 The broad applicability of these findings has been questioned because of an average transfer delay of only 69 minutes across all trials and the low rates of rescue PCI and subsequent revascularization in the fibrinolysis arms.8 Nonetheless, regional revascularization systems of care that forego immediate fibrinolysis and transfer STEMI patients presenting to community hospitals to PPCI capable hospitals have emerged worldwide.
Observational data from the United States have shown that delays in a portion of the transfer process for primary PCI (door-in-door-out of the transfer hospital) are associated with mortality.9 Moreover, only 4–19% of transferred patients meet the guideline recommended door to balloon time of < 90 minutes and only 10–11% of patients meet transferring hospital door in to door out times of <30 minutes. 9–14 A large scale international study of how inter-hospital transfer delays for PPCI in STEMI patients presenting to a non-PPCI capable site is currently lacking. Since PCI center door-to-balloon times have improved it may be particularly important to focus on the overall transfer process from arrival at the non-PCI capable center to arrival at the PCI center.15 Accordingly, in a secondary analysis of the largest randomized controlled trial of STEMI patients undergoing PPCI, we sought to examine the outcomes associated with door 1 to door 2 (D1D2) times in patients undergoing inter-hospital transfer for PPCI. We prospectively selected D1D2 time, and not door-in-door-out or first door to balloon time, as a transfer delay measure for two reasons. First, door-in-door-out does not account for delays in transportation itself. Second, we hypothesized that most of the variability in first door to balloon time will be described by the D1D2 time, since the PCI center arrival to balloon times would be consistently short.
Methods
The Assessment of Pexelizumab in Acute Myocardial Infarction (APEX AMI) trial was a multi-center randomized double blind placebo controlled study evaluating the potential role of pexelizumab (a humanized monoclonal antibody C5 complement inhibitor) in patients with STEMI undergoing PPCI. The trial enrolled 5745 STEMI patients treated with PPCI at 296 sites in 17 countries.16, 17 Patients over the age of 18 were eligible if they presented within six hours of symptoms onset, PPCI was the planned reperfusion strategy, and had one of three high risk ECG characteristics (≥ 2 mm ST elevation in two anterior lateral leads or ≥ 2 mm ST elevation in two inferior leads coupled with ST depression in two contiguous anterior leads for a total of ≥ 8 mm or a new left bundle branch block with at least 1 mm concordant ST elevation). Patients were enrolled and randomized at percutaneous coronary intervention (PCI) centers, regardless of whether they presented directly to the PCI centers or were transferred from non-PCI centers. The Institutional Review Board of each participating hospital approved the protocol and patients were required to provide written informed consent.
Transfer Groups and Time Intervals
The overall trial population was divided into two groups: a non-transfer group comprised of patients who presented to PPCI centers and the transfer group, which comprised of patients who initially presented to non-PCI capable hospitals and underwent inter-hospital transfer to a PCI capable center. Since no treatment effect with pexelizumab was observed, patients were not stratified further according study drug assignment.
All time intervals were calculated from times entered into individual case report forms by local study personnel. Time intervals are shown in Figure 1. Symptom to presentation time was defined symptom onset to first hospital arrival; D1D2 time (for transferred patients) was defined as arrival at the first hospital to arrival at the PCI capable hospital; door-in-door-out time (for transferred patients) was defined as arrival to departure from non-PCI capable hospital; transportation time (for transferred patients) was defined as departure from non-PCI hospital to arrival at PPCI hospital; PCI center arrival to balloon time (for transferred patients) was defined as PCI center arrival to balloon inflation time; and first door to balloon time was defined as time from first hospital arrival to balloon inflation time.
Figure 1.
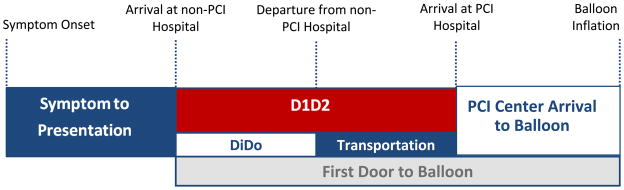
Time intervals in the transferred group.
Abbreviations: D1D2; door 1 to door 2 time; DiDo, door-in-door-out time.
Outcomes
The main outcome in the transfer group was the 90-day composite of death, shock and heart failure. Our primary analysis assessed the association between D1D2 time (as a continuous variable) in transferred patients and the 90-day composite outcome. Pre-specified secondary analyses included post-PCI TIMI flow, sum ST-segment resolution, infarct size assessed by peak CK-MB, and the individual components of the primary outcome.
In a planned analysis of the transfer group, outcomes stratified by symptom to presentation time, APEX baseline risk and D1D2 time were explored.18
Statistical Methods
Continuous variables are presented as medians with first and third quartiles and are compared between groups with Wilcoxon rank sum test. The Kruskal-Wallis test is used for comparing medians across three or more groups. Categorical variables are presented as percentages and compared across groups with the Pearson chi-squared test or the Fisher exact test when sample sizes are small. The correlation between D1D2 and door to balloon time is tested with Spearman rank correlation test (rs). A Cox proportional hazards model is used to assess the relationship between D1D2 time and the 90-day composite endpoint (death, shock, and heart failure) after multivariable adjustment. Since this model assumes that the covariates have a linear effect on the log-hazard, the Stone and Koo additive spline transformation is first applied to each covariate in an unadjusted model.19 Covariates that exhibit significant non-linearity are transformed with a linear spline using both a grid search and graphical check for the optimal knot points. Two-piece linear splines are sufficient for the non-linear covariates, age (knot at 55 years), baseline heart rate (knot at 70 bpm), D1D2 time (knot at 150 minutes), and baseline creatinine (knot at 0.9 mg/dL). Multiple imputations are performed to avoid using a complete-case analysis. Multiple imputations assume a multivariate normal distribution for the covariates. The continuous covariates are approximately normally distributed within the given range for imputed values and values for the binary baseline Q-wave covariate are imputed with no rounding. Five imputed data sets are generated with PROC MI and the final adjusted model is given using PROC MIANALYZE. The proportional hazards c-indices for each imputed model and the final model are all 0.83. The proportional hazards assumption is verified graphically by plotting the Schoenfeld residuals against log (time) for each covariate. In a planned secondary analysis, D1D2 times were stratified according to APEX risk score tertiles. This risk score uses baseline variables to predict 90- day mortality and has good discriminative properties (c=0.821).18 All analyses are performed in SAS v9.2 (SAS Institute, Cary, NC). The significance level is set at 0.05.
Results
Study Population
Among the 5745 patients in the APEX-AMI trial, 2075 (36.1%) patients were transferred from the presenting hospital for PPCI. Transfer status was not available in 3 patients. Compared to non-transferred patients, those undergoing transfer for PPCI were more likely to have prior coronary artery disease, higher heart rate and lower serum creatinine (Table 1).
Table 1.
Baseline Characteristics
| No Transfer (n=3667) | Transferred (n=2075) | p-value | |
|---|---|---|---|
| Age, median (Q1, Q3), years | 61 (52, 71) | 61 (53, 70) | 0.906 |
| Female sex, n(%) | 841 (22.9) | 483 (23.3) | 0.767 |
| Clinical History, n(%) | |||
| Diabetes | 585 (16.0) | 328 (15.8) | 0.885 |
| Hypertension | 1809 (49.3) | 1030 (49.6) | 0.823 |
| Prior MI | 468 (12.8) | 226 (10.9) | 0.037 |
| Prior PCI | 395 (10.8) | 167 (8.0) | 0.001 |
| Prior CABG | 82 (2.2) | 46 (2.2) | 0.962 |
| Prior CHF | 132 (3.6) | 76 (3.7) | 0.902 |
| Prior AF | 152 (4.1) | 86 (4.1) | 0.999 |
| Prior Stroke | 142 (3.9) | 74 (3.6) | 0.558 |
| COPD | 174 (4.7) | 108 (5.2) | 0.439 |
| Current smoker | 1567 (42.8) | 910 (44.0) | 0.378 |
| Peripheral Vascular Disease | 156 (4.3) | 90 (4.3) | 0.881 |
| High Risk Inferior (ECG), n(%) | 1527 (41.6) | 818 (39.4) | 0.100 |
| Sum ST Segment Deviation, (Q1, Q3), mm | 13.0 (9.0, 18.5) | 13.0 (9.0, 18.5) | 0.428 |
| Heart rate, (Q1, Q3), bpm | 75 (64, 86) | 76 (65, 87) | 0.012 |
| Systolic blood pressure, (Q1, Q3), mmHg | 133 (117, 150) | 132 (118, 150) | 0.994 |
| Killip > I, n(%) | 390 (10.6) | 221 (10.7) | 0.981 |
| Creatinine, (Q1, Q3), μmol/L | 90.0 (79.6, 106.1) | 88.4 (78.0, 106.1) | 0.005 |
| Time Intervals | |||
| Symptom to Presentation, (Q1, Q3), min | 101 (60, 159) | 82 (46, 139) | <0.001 |
| Door to Balloon time, (Q1, Q3), min | 76 (55, 104) | 132 (107, 167) | <0.001 |
| Door to Balloon time <90 min, n (%) | 2417 (65.9) | 386 (18.6) | <0.001 |
| Door to Balloon time <120 min, n (%) | 3096 (84.4) | 889 (42.8) | <0.001 |
| D1D2, (Q1, Q3), min | — | 84 (61, 114) | — |
| DiDo non-PCI center, (Q1, Q3), min | — | 43 (26, 70) | — |
| Transportation Time, (Q1, Q3), min | — | 35 (24, 50) | — |
| PCI Center Arrival to Balloon Time Patients, (Q1, Q3), min | 76 (55, 104) | 45 (32, 61) | <0.001 |
| Symptom to Balloon time | 184 (139, 253) | 229 (179, 297) | <0.001 |
| Weekend Presentation, n (%) | 796 (21.7) | 469 (22.6) | 0.432 |
| Weekday Evening Presentation (6pm–6am), n (%) | 669 (18.2) | 394 (19.0) | 0.465 |
| Hospital Location, n(%) | <0.001 | ||
| North American | 1406 (38.3) | 680 (32.8) | |
| Australia/New Zealand | 1204 (32.8) | 557 (26.8) | |
| West Europe | 624 (17.0) | 713 (34.4) | |
| East Europe | 433 (11.8) | 125 (6.0) | |
Abbreviations: AF, atrial fibrillation; bpm, beats per minute; CABG, coronary artery bypass grafting; CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; D1D2, time from arrival at first hospital to second hospital; DiDo, Door in to door out time at non-PCI centers; ECG, electrocardiogram; min, minutes; mm, millimeters; mmHg, millimeters mercury; n, number; MI, myocardial infarction; Q1, first quartile; Q3, third quartile; PCI, percutaneous coronary intervention.
The median symptom to presentation time was longer in the non-transferred group (101 vs 82 minutes, p<0.001). The symptom onset to balloon time (229 vs 184, p<0.001) and first door to balloon time (132 vs 76 minutes, p<0.001) times were longer in the transferred group. The percentage of patients achieving first door to balloon times less than 90 minutes was 66% in the non-transferred and and 19% in the transferred groups. First door to balloon times were highly correlated with D1D2 times in transferred patients (rs =0.816; p<0.001). In transferred patients, the median D1D2 time was 84 minutes. The median PCI center arrival to balloon time in transferred patients was significantly shorter than the non-transferred patients time (45 vs 76 minutes; p<0.001) minutes. Upon arrival at the PCI center, approximately half of the patients were treated between 30–60 minutes and 85.5% were treated in <75 minutes.
Several regional differences were observed. The largest proportion of transferred patients was in Western Europe. First door to balloon times less than 90 minutes among transferred patients was achieved in 23.9% of Western European patients, 20.8% from Australian and New Zealand, 18.5% from North America, and 14.2% from Eastern Europe.
D1D2 Time
Selected baseline characteristics stratified by D1D2 time are shown in Table 2. Patients with longer D1D2 times tended to be female, have more co-morbidities, anterior infarctions, higher heart rates, shorter symptom to presentation times, and were more likely to present on weekday evenings.
Table 2.
Patient Characteristics of Transferred Patients Stratified by D1D2 Time
| D1D2, minutes | |||||
|---|---|---|---|---|---|
| <60 (n=451) | 60–90 (n=713) | 90–120 (n=432) | >120 (n=478) | p value | |
| Age, median (Q1, Q3), years | 60 (52, 69) | 61 (54, 70) | 61 (52, 72) | 62 (53, 71) | 0.265 |
| Female sex, n(%) | 89 (19.7) | 150 (21.0) | 109 (25.2) | 135 (28.2) | 0.005 |
| Clinical History, n(%) | |||||
| Diabetes | 62 (13.7) | 98 (13.7) | 76 (17.6) | 92 (19.2) | 0.029 |
| Hypertension | 201 (44.6) | 341 (47.8) | 214 (49.5) | 273 (57.1) | 0.001 |
| Prior MI | 46 (10.2) | 68 (9.5) | 46 (10.6) | 65 (13.6) | 0.156 |
| Prior PCI | 33 (7.3) | 50 (7.0) | 42 (9.7) | 42 (8.8) | 0.341 |
| Prior CABG | 13 (2.9) | 6 (0.8) | 10 (2.3) | 17 (3.6) | 0.011 |
| Current smoker | 190 (42.3) | 337 (47.4) | 185 (42.9) | 197 (41.4) | 0.147 |
| High Risk Inferior (ECG), n(%) | 210 (46.6) | 277 (38.8) | 161 (37.3) | 169 (35.4) | 0.003 |
| Sum ST Segment Deviation, (Q1, Q3), mm | 13.0 (9.0, 19.5) | 13.5 (9.5, 19.5) | 13.0 (9.0, 18.0) | 12.0 (8.0, 17.8) | 0.002 |
| Heart rate, (Q1, Q3), bpm | 75 (64, 85) | 76 (65, 86) | 77 (65, 88) | 77 (65, 90) | 0.035 |
| Systolic blood pressure, (Q1, Q3), mmHg | 133 (120, 150) | 133 (117, 150) | 134 (118, 150) | 130 (115, 150) | 0.302 |
| Killip > I, n(%) | 41 (9.1) | 73 (10.2) | 56 (13.0) | 51 (10.7) | 0.295 |
| Creatinine, (Q1, Q3), μmol/L | 88.4 (77.0, 104.0) | 88.7 (79.0, 106.1) | 88.4 (78.0, 105.0) | 88.4 (77.0, 106.1) | 0.681 |
| Symptom Onset to D1, (Q1, Q3), min | 90 (55, 152) | 87 (50, 140) | 87 (54, 150) | 64 (30, 119) | <0.001 |
| Weekend Presentation, n (%) | 101 (22.4) | 166 (23.3) | 99 (22.9) | 103 (21.5) | 0.913 |
| Weekday Evening Presentation (6pm–6am), n (%) | 58 (12.9) | 145 (20.3) | 81 (18.8) | 110 (23.1) | 0.001 |
| Hospital Location, n(%) | <0.001 | ||||
| North American | 113 (25.1) | 219 (30.7) | 154 (35.6) | 194 (40.6) | |
| Australia/New Zealand | 33 (7.3) | 42 (5.9) | 18 (4.2) | 32 (6.7) | |
| West Europe | 158 (35.0) | 202 (28.3) | 91 (21.1) | 106 (22.2) | |
| East Europe | 147 (32.6) | 250 (35.1) | 169 (39.1) | 146 (30.5) | |
| Pre-PCI TIMI Flow | 0.269 | ||||
| 0/1 | 317 (71.7) | 503 (72.3) | 305 (72.6) | 307 (67.5) | |
| 2/3 | 125 (28.3) | 193 (27.8) | 115 (27.4) | 148 (32.5) | |
| GIIb/IIIa Use, n(%) | 284 (63.0) | 453 (63.5) | 264 (61.1) | 306 (64.0) | 0.811 |
Abbreviations: AF, atrial fibrillation; bpm, beats per minute; CABG, coronary artery bypass grafting; CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; D1, time of arrival at first hospital; D1D2, time from arrival at first hospital to second hospital; D2, time of arrival at second hospital (for transferred patients only); ECG, electrocardiogram; min, minutes; mm, millimeters; mmHg, millimeters mercury; n, number; MI, myocardial infarction; PCI, percutaneous coronary intervention; Q1, first quartile; Q3, third quartile.
Outcomes
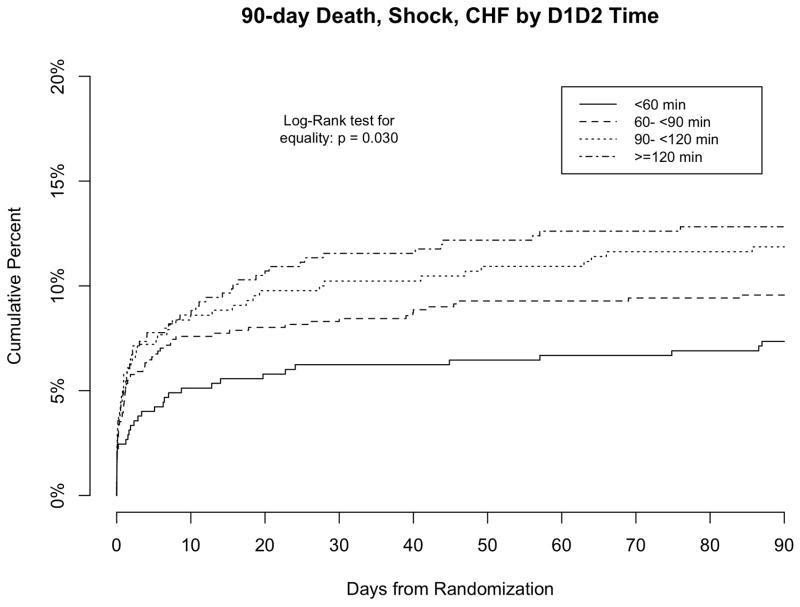
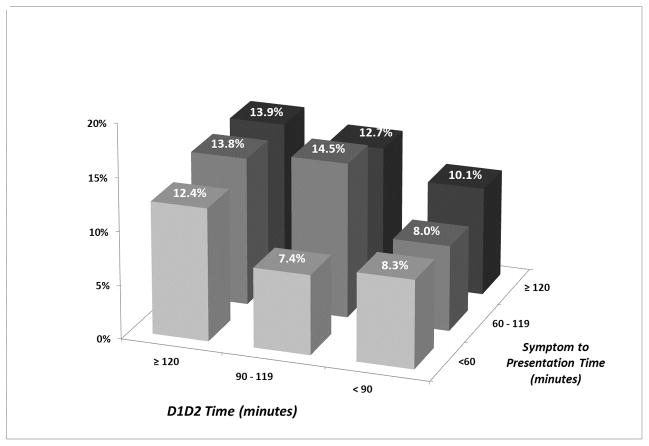
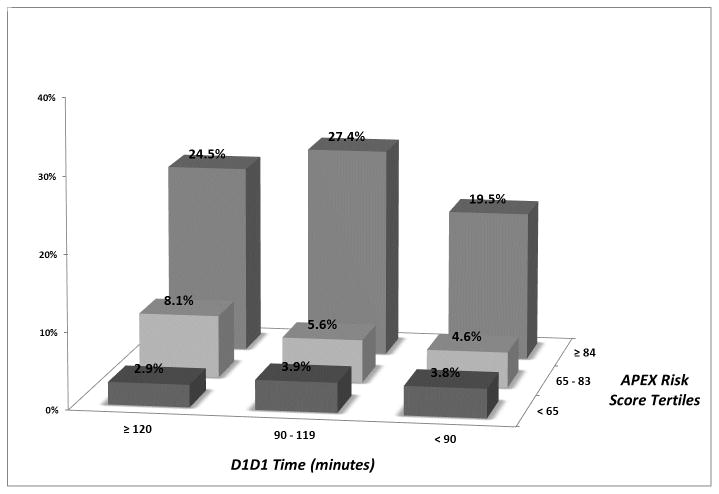
The 90 day primary outcome in the transfer and no transfer groups were 10.3% and 10.2%, respectively (p=0.89). Outcomes stratified by D1D2 times are presented in Table 3 and Figure 2. Significant nonlinearity at 150 minutes was observed between D1D2 time as a continuous variable and the primary outcome, with a less steep relationship beyond 150 minutes, thus D1D2 was analyzed as a spline in the unadjusted and adjusted model. The 90-day incidence of death, shock, and heart failure was higher for patients with a D1D2 times ≤ 150 minutes (hazard ratio (HR), 1.19 per 30 minutes: 95% Confidence Interval (CI), 1.06 to 1.33 p=0.004) but not with D1D2 times > 150 minutes (HR, 0.99: 95% CI, 0.96 to 1.02; p=0.496). A non-significant trend between heart failure and 90 day mortality was observed in patients with prolonged D1D2 times. No association was observed between D1D2 time and post-PCI TIMI flow, sum ST segment recovery, or peak CK-MB. The unadjusted primary outcome stratified by D1D2 time and symptom to presentation time (Figure 3a) and APEX risk score tertiles (Figure 3b) are shown.18 Longer D1D2 times were associated with longer symptom to presentation times (p<0.001), but no association was observed between D1D2 times and APEX risk score tertiles (p=0.176).
Table 3.
Outcomes Stratified by D1D2 Time
| Outcomes | D1D2 Time, minutes | ||||
|---|---|---|---|---|---|
| <60 (n=451) | 60–90 (n=713) | 90–120 (n=432) | >120 (n=478) | p value | |
| 90 Day Death/Shock/Heart Failure, n(%) | 33 (7.3) | 68 (9.6) | 51 (11.9) | 61 (12.8) | 0.028 |
| Death | 16 (3.6) | 30 (4.2) | 23 (5.3) | 31 (6.5) | 0.148 |
| Shock | 12 (2.7) | 24 (3.4) | 15 (3.5) | 20 (4.2) | 0.650 |
| Heart Failure | 12 (2.7) | 36 (5.0) | 28 (6.5) | 26 (5.4) | 0.058 |
| Post PCI TIMI Flow*, n(%) | 0.117 | ||||
| 0/1 | 17 (3.9) | 12 (1.7) | 9 (2.1) | 16 (3.6) | |
| 2/3 | 421 (96.1) | 680 (98.3) | 411 (97.9) | 433 (96.4) | |
| Sum ST Segment Recovery*, n(%) | 0.943 | ||||
| <30 % | 71 (17.1) | 98 (15.0) | 59 (15.2) | 70 (16.4) | |
| 30–70% | 135 (32.5) | 218 (33.3) | 123 (31.8) | 144 (33.8) | |
| >70% | 209 (50.4) | 339 (51.8) | 205 (53.0) | 212 (49.8) | |
| Peak CK-MB*, median (Q1, Q3), μg/L | 199 (84, 300) | 173 (86, 344) | 185 (77, 311) | 176 (68, 312) | 0.798 |
Endpoints not available on all patients
Abbreviations: D1D2, time from arrival at first hospital to second hospital; n, number; PCI, percutaneous coronary intervention; Q1, first quartile; Q3, third quartile.
Figure 2.
Kaplan Meier Curve of 90 day Death, Shock, and Heart Failure Stratified by D1D2 time
Figure 3.
90 day incidence of death, shock, or heart failure stratified by D1D2 time and (a) symptom to presentation time (b) APEX risk score tertiles
After multivariable adjustment, no significant association was observed between 90 day death, shock, or heart failure and either D1D2 time ≤ 150 minutes (adjusted HR, 1.07 per 30 minutes: 95% CI, 0.94 to 1.22 p=0.291) or D1D2 time > 150 minutes (adjusted HR, 0.98: 95% CI, 0.94 to 1.01; p=0.196).
Discussion
There are two important findings in this analysis of a large PPCI trial population. First, unadjusted D1D2 time was strongly associated with 90 day outcomes in patients undergoing inter-hospital transfer for PPCI, although this relationship was not significant after multivariable adjustment. Second, the difference in symptom to balloon time between transferred and non-transferred patients was only 45 minutes. This analysis may lend insights into why some observational studies, but not this analysis or analyses from other randomized studies, have shown outcome differences associated with inter-hospital transfer delays.
Delays in STEMI revascularization are associated with increased mortality; however a meta-analysis of randomized controlled trials of STEMI patients presenting community hospitals showed that foregoing immediate thrombolysis in favor of transfer to a PPCI capable center may improve outcomes.7 The generalizability of these results have been questioned given the small difference in treatment time (average 69 minutes) and the low rates of rescue PCI and subsequent revascularization in the fibrinolysis arms.8 Observational studies have reported that transfer delays are associated with higher mortality and only a minority of patients are treated within guideline recommended timeframes; first door to balloon times are met in less than 1 in 5 US patients and DIDO times are met in approximately 1 in 10.9, 10, 12, 14 This study’s finding that D1D2 time is not independently associated with 90 day death, shock, and heart failure supports the results of previous controlled studies, however these results should not be extrapolated to imply superiority of mechanical revascularization over fibrinolysis for patients presenting to non-PCI capable hospitals irrespective of transportation delays.
This analysis provides insights into the differences in outcomes associated with transfer for PPCI reported between controlled and observation studies. The difference in total ischemic time (symptom to balloon) was only 45 minutes between the transfer and non-transfer groups. This is small compared to the reported transfer delays of 48–111 minutes reported from previous controlled trials evaluating reperfusion strategies for patients presenting to non-PCI capable hospitals.8 Additionally, the transfer times achieved in this study are shorter to those in observational registry studies. In separate recent reports from the National Cardiovascular Data Registry and the Get with the Guidelines ACTION Registry, the median D1D2 time was 107 minutes and the median door-in-door-out time was 68 minutes, respectively.9, 13 Both of these measures are longer than the median D1D2 time (84 minutes) and door-in-door-out (43 minutes) achieved in this trial. This disparity highlights the fact that patients enrolled in clinical trials may not be representative of those in everyday clinical practice and the results of our study should be interpreted accordingly. We hypothesize that the APEX-AMI trial may have included study centers with superior transfer systems or geographically smaller referral networks compared to the average PPCI center. In addition, patient randomization occurred at PPCI capable centers and not at presenting hospitals, thus there is an inherent possibility that there was selective enrollment bias in favor of patients with shorter transfer times.
Our results in perspective
This study suggests that transfer of a STEMI patient for PPCI is the preferred reperfusion strategy if it can be achieved in a timely fashion. The lack of an observed difference in 90 day outcomes between the transferred and non-transferred groups likely reflects that an 84 minute D1D2 time and 45 minute difference in total ischemic time likely is not associated with a substantially worse outcome. Nevertheless, it is our opinion that these findings should not be used to support a “mechanical reperfusion only” strategy as transfer times achieved within this trial may not be achievable in all health care regions. Guidelines underscore the importance of timely reperfusion and there are calls for integrated regional PCI/fibrinolysis STEMI care systems.20, 21 Acceptable transfer delays, however, remain undefined. European Society of Cardiology guidelines recommend a first medical contact to balloon time of less than 2 hours and a recent retrospective analysis has suggested the superiority of fibrinolysis when the PCI-related delay (door to balloon – door to needle time) exceeds 120 minutes, but prospective validation of this interval is lacking.22, 23 Given the importance of timely reperfusion, regional systems of care should continue to try and minimize PPCI transfer delays until acceptable delays are prospectively defined.
D1D2 time as a measure of transfer delay
We explored D1D2 time as an inter-hospital transfer delay measure encompassing both the presenting hospital door-in-door-out time and the transportation time as a predictor of outcomes in patients transferred for PPCI. Although both door-in-door-out and door to balloon times have been associated with mortality, we feel D1D2 time is the best integrated descriptor of inter-hospital transfer delays. Door-in-door-out times only reflect presenting hospital delays and do not account for transportation times. As demonstrated in this analysis, the PCI center arrival to balloon times in transferred patients were short, likely reflecting catheterization laboratory pre-activation. Additionally, D1D2 was highly correlated with overall door to balloon time. Finally, the outcomes associated with symptom to balloon and first door to balloon times in the APEX-AMI trial, albeit not in transferred patients, have been previously published; however these metrics were not the focus of this analysis.3
Limitations
Three additional limitations merit consideration. The relationship between delay and outcome is complex, and it relates to both the effect of the delay itself, as well as the effect of measured and unmeasured confounders. Secondly, this study did not include a fibrinolysis arm thus comparison of reperfusion strategies is not possible. Finally, other studies have reported the association between treatment delays and long term mortality.24 Only intermediate term outcomes were available in this study.
Conclusions
In this analysis of the largest PPCI trial database the relatively short transfer times achieved within this trial may explain the discrepancy in the associations of inter-hospital transfer delays and outcomes reported between clinical trial and registry studies.
Acknowledgments
Funding Sources: The APEX-AMI trial, from which this work was derived, was supported by a research grant jointly funded from Procter & Gamble and Alexion Pharmaceuticals.
Footnotes
Disclosures: SVD, PW, KRW, FVdW, AWJvH: None. RDL received research grants from Bristol Myers Squibb and served as consultant/advisor for Pfizer and Boehringer Ingleheim. WDW served on data and safety monitoring boards for Boston Scientific and Boehringer Ingleheim sponsored trials. DA received research grants and speakers’ bureau payments from Eli Lilly, Astrazeneca, Daichi Sankyo, Sorin Biomedica, Boston Scientific, Pfizer; speakers’ bureau payments from Glaxaxo Smith Kline, Bristol Myers Squibb, Merc Sharpe & Dohme, Menarini; and served as consultant/advisor for Eli Lilly, Astrazeneca, Daichi Sankyo, Bristol Myers Squibb, Merc Sharpe & Dohme, Bayer. PWA and CBG received funding from Procter & Gamble Pharmaceuticals and Alexion Pharmaceuticals for the APEX-AMI trial.
References
- 1.Boersma E, Maas ACP, Deckers JW, Simoons ML. Early thrombolytic treatment in acute myocardial infarction: Reappraisal of the golden hour. Lancet. 1996;348:771–775. doi: 10.1016/S0140-6736(96)02514-7. [DOI] [PubMed] [Google Scholar]
- 2.De Luca G, Suryapranata H, Ottervanger JP, Antman EM. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction. Circulation. 2004;109:1223–1225. doi: 10.1161/01.CIR.0000121424.76486.20. [DOI] [PubMed] [Google Scholar]
- 3.Hudson MP, Armstrong PW, O’Neil WW, Stebbins AL, Weaver WD, Widimsky P, Aylward PE, Ruzyllo W, Holmes D, Mahaffey KW, Granger CB. Mortality implications of primary percutaneous coronary intervention treatment delays: Insights from the assessment of pexelizumab in acute myocardial infarction trial. Circulation: Cardiovasc Qual Outcomes. 2011;4:183–192. doi: 10.1161/CIRCOUTCOMES.110.945311. [DOI] [PubMed] [Google Scholar]
- 4.Widimský P, Groch L, Zelízko M, Aschermann M, Bednář F, Suryapranata H. Multicentre randomized trial comparing transport to primary angioplasty vs immediate thrombolysis vs combined strategy for patients with acute myocardial infarction presenting to a community hospital without a catheterization laboratory. The PRAGUE study. Eur Heart J. 2000;21:823–831. doi: 10.1053/euhj.1999.1993. [DOI] [PubMed] [Google Scholar]
- 5.Widimský P, Budešínský T, Voráč D, Groch L, Želízko M, Aschermann M, Branny M, Št’ásek J, Formánek P. Long distance transport for primary angioplasty vs immediate thrombolysis in acute myocardial infarction. Eur Heart J. 2003;24:94–104. doi: 10.1016/s0195-668x(02)00468-2. [DOI] [PubMed] [Google Scholar]
- 6.Andersen HR, Nielsen TT, Rasmussen K, Thuesen L, Kelbaek H, Thayssen P, Abildgaard U, Pedersen F, Madsen JK, Grande P, Villadsen AB, Krusell LR, Haghfelt T, Lomholt P, Husted SE, Vigholt E, Kjaergard HK, Mortensen LS. A comparison of coronary angioplasty with fibrinolytic therapy in acute myocardial infarction. N Engl J Med. 2003;349:733–742. doi: 10.1056/NEJMoa025142. [DOI] [PubMed] [Google Scholar]
- 7.Dalby M, Bouzamondo A, Lechat P, Montalescot G. Transfer for primary angioplasty versus immediate thrombolysis in acute myocardial infarction. Circulation. 2003;108:1809–1814. doi: 10.1161/01.CIR.0000091088.63921.8C. [DOI] [PubMed] [Google Scholar]
- 8.Herrmann HC. Transfer for primary angioplasty. Circulation. 2005;111:718–720. doi: 10.1161/01.CIR.0000156406.52178.C5. [DOI] [PubMed] [Google Scholar]
- 9.Wang TY, Nallamothu BK, Krumholz HM, Li S, Roe MT, Jollis JG, Jacobs AK, Holmes DR, Peterson ED, Ting HH. Association of door-in to door-out time with reperfusion delays and outcomes among patients transferred for primary percutaneous coronary intervention. JAMA. 2011;305:2540–2547. doi: 10.1001/jama.2011.862. [DOI] [PubMed] [Google Scholar]
- 10.Nallamothu BK, Bates ER, Herrin J, Wang Y, Bradley EH, Krumholz HM Investigators ftN. Times to treatment in transfer patients undergoing primary percutaneous coronary intervention in the united states. Circulation. 2005;111:761–767. doi: 10.1161/01.CIR.0000155258.44268.F8. [DOI] [PubMed] [Google Scholar]
- 11.Chakrabarti A, Krumholz HM, Wang Y, Rumsfeld JS, Nallamothu BK for the National Cardiovascular Data Registry. Time-to-reperfusion in patients undergoing interhospital transfer for primary percutaneous coronary intervention in the u.S: An analysis of 2005 and 2006 data from the national cardiovascular data registry. J Am Coll Cardiol. 2008;51:2442–2443. doi: 10.1016/j.jacc.2008.02.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roe MT, Messenger JC, Weintraub WS, Cannon CP, Fonarow GC, Dai D, Chen AY, Klein LW, Masoudi FA, McKay C, Hewitt K, Brindis RG, Peterson ED, Rumsfeld JS. Treatments, trends, and outcomes of acute myocardial infarction and percutaneous coronary intervention. J Am Coll Cardiol. 2010;56:254–263. doi: 10.1016/j.jacc.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 13.Wang TY, Peterson ED, Ou F-S, Nallamothu BK, Rumsfeld JS, Roe MT. Door-to-balloon times for patients with st-segment elevation myocardial infarction requiring interhospital transfer for primary percutaneous coronary intervention: A report from the national cardiovascular data registry. Am Heart J. 2011;161:76–83.e71. doi: 10.1016/j.ahj.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 14.Herrin J, Miller LE, Turkmani DF, Nsa W, Drye EE, Bernheim SM, Ling SM, Rapp MT, Han LF, Bratzler DW, Bradley EH, Nallamothu BK, Ting HH, Krumholz HM. National performance on door-in to door-out time among patients transferred for primary percutaneous coronary intervention. Arch Intern Med. 2011;171:1879–1886. doi: 10.1001/archinternmed.2011.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Krumholz HM, Herrin J, Miller LE, Drye EE, Ling SM, Han LF, Rapp MT, Bradley EH, Nallamothu BK, Nsa W, Bratzler DW, Curtis JP. Improvements in door-to-balloon time in the United States, 2005 to 2010/clinical perspective. Circulation. 2011;124:1038–1045. doi: 10.1161/CIRCULATIONAHA.111.044107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Armstrong PW, Adams PX, Al-Khalidi HR, Hamm C, Holmes D, O’Neill W, Todaro TG, Vahanian A, Van de Werf F, Granger CB. Assessment of pexelizumab in acute myocardial infarction (APEX AMIi): A multicenter, randomized, double-blind, parallel-group, placebo-controlled study of pexelizumab in patients with acute myocardial infarction undergoing primary percutaneous coronary intervention. Am Heart J. 2005;149:402–407. doi: 10.1016/j.ahj.2004.12.015. [DOI] [PubMed] [Google Scholar]
- 17.The APEX-AMI Investigators. Pexelizumab for acute st-elevation myocardial infarction in patients undergoing primary percutaneous coronary intervention. JAMA. 2007;297:43–51. doi: 10.1001/jama.297.1.43. [DOI] [PubMed] [Google Scholar]
- 18.Stebbins A, Mehta RH, Armstrong PW, Lee KL, Hamm C, Van de Werf F, James S, Toftegaard-Nielsen T, Seabra-Gomes R, White HD, Granger CB. Infarction for the APEX AMI Investigators. A model for predicting mortality in acute st-segment elevation myocardial infarction treated with primary percutaneous coronary intervention/clinical perspective. Circulation: Cardiovasc Interv. 2010;3:414–422. doi: 10.1161/CIRCINTERVENTIONS.109.925180. [DOI] [PubMed] [Google Scholar]
- 19.Stone CJ, Koo CY. Additive splines in statistics. Proc Stat Comp Sect Am Statist Assoc. 1985:45–48. [Google Scholar]
- 20.Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, Mullany CJ, Ornato JP, Pearle DL, Sloan MA, Smith SC, Jr, Alpert JS, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Gregoratos G, Halperin JL, Hiratzka LF, Hunt SA, Jacobs AK. Acc/aha guidelines for the management of patients with st-elevation myocardial infarction: A report of the american college of cardiology/american heart association task force on practice guidelines (committee to revise the 1999 guidelines for the management of patients with acute myocardial infarction) J Am Coll Cardiol. 2004;44:E1–E211. doi: 10.1016/j.jacc.2004.07.014. [DOI] [PubMed] [Google Scholar]
- 21.Armstrong PW, Boden WE. Reperfusion paradox in st-segment elevation myocardial infarction. Ann Intern Med. 2011;155:389–391. doi: 10.7326/0003-4819-155-6-201109200-00008. [DOI] [PubMed] [Google Scholar]
- 22.Van de Werf F, Bax J, Betriu A, Blomstrom-Lundqvist C, Crea F, Falk V, Filippatos G, Fox K, Huber K, Kastrati A, Rosengren A, Steg PG, Tubaro M, Verheugt F, Weidinger F, Weis M, Vahanian A, Camm J, De Caterina R, Dean V, Dickstein K, Funck-Brentano C, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Tendera M, Widimsky P, Zamorano JL, Reviewers D, Aguirre FV, Al-Attar N, Alegria E, Andreotti F, Benzer W, Breithardt O, Danchin N, Mario CD, Dudek D, Gulba D, Halvorsen S, Kaufmann P, Kornowski R, Lip GYH, Rutten F Guidelines ECfP. Management of acute myocardial infarction in patients presenting with persistent st-segment elevation. Eur Heart J. 2008;29:2909–2945. doi: 10.1093/eurheartj/ehn416. [DOI] [PubMed] [Google Scholar]
- 23.Pinto DS, Frederick PD, Chakrabarti AK, Kirtane AJ, Ullman E, Dejam A, Miller DP, Henry TD, Gibson CM. Benefit of transferring st-segment–elevation myocardial infarction patients for percutaneous coronary intervention compared with administration of onsite fibrinolytic declines as delays increase/clinical perspective. Circulation. 2011;124:2512–2521. doi: 10.1161/CIRCULATIONAHA.111.018549. [DOI] [PubMed] [Google Scholar]
- 24.Terkelsen CJ, Sørensen JT, Maeng M, Jensen LO, Tilsted H-H, Trautner S, Vach W, Johnsen SP, Thuesen L, Lassen JF. System delay and mortality among patients with stemi treated with primary percutaneous coronary intervention. JAMA. 2010;304:763–771. doi: 10.1001/jama.2010.1139. [DOI] [PubMed] [Google Scholar]