Abstract
The discovery of somatic mutations in the JAK-STAT signaling pathway was a major breakthrough in our understanding of the molecular pathogenesis of the myeloproliferative neoplasms (MPNs) polycythemia vera, essential thrombocytosis, and primary myelofibrosis. This finding led to the development of small molecule inhibitors targeting Janus kinase (JAK) 2 and other JAK family members. Currently, there are a number of research and clinical trials ongoing with JAK inhibitors. While the appeal of inhibiting JAK2 is clear, studies to date suggest that JAK2 inhibitor monotherapy might not be sufficient to cause reductions in disease allele burden in MPN patients. There is compelling evidence that JAK inhibitors are improving symptoms and therefore quality of life for patients. It will be important to investigate the efficacy of JAK inhibitors in preclinical and clinical studies to better understand their effects, while at the same time pursuing alternative therapies which might offer benefit to MPN patients alone and in combination with JAK inhibitors.
Keywords: JAK kinases, myeloproliferative disorder, JAK inhibitor, essential thrombocytosis, polycythemia vera, myelofibrosis
Background
MPNs and JAK2V617F
Myeloproliferative neoplasms (MPNs) are clonal hematopoietic stem cell disorders that are characterized by dysregulated myeloid proliferation, with aberrant expansion of different myeloid lineages [Levine and Gilliland, 2008]. The most common MPNs are polycythemia vera (PV), essential thrombocytosis (ET), primary myelofibrosis (PMF), and chronic myeloid leukemia (CML). The pathogenesis and therapy of CML has been discussed extensively elsewhere and will not be discussed in this review. The different MPNs were originally classified as a set of phenotypically related MPNs by William Dameshek in 1951 [Dameshek, 1951], but a common pathogenetic event which unified PV, ET, and PMF was not discovered until 2005.
PV and ET most commonly present as increased numbers of cells in one or more myeloid lineages; in contrast PMF most commonly presents with cytopenias, bone marrow fibrosis, and marked extramedullary hematopoiesis. Although PV and ET are associated with less clinical sequelae at presentation than PMF, these MPNs are still associated with increased morbidity and mortality, most commonly thrombosis, bleeding, progressive bone marrow failure, and leukemic transformation. In addition, PV and ET can progress to myelofibrosis (MF), and all three MPN can progress to acute myeloid leukemia (AML; see Figure 1); importantly progression to acute leukemia following an MPN is associated with a dismal outcome.
Figure 1.
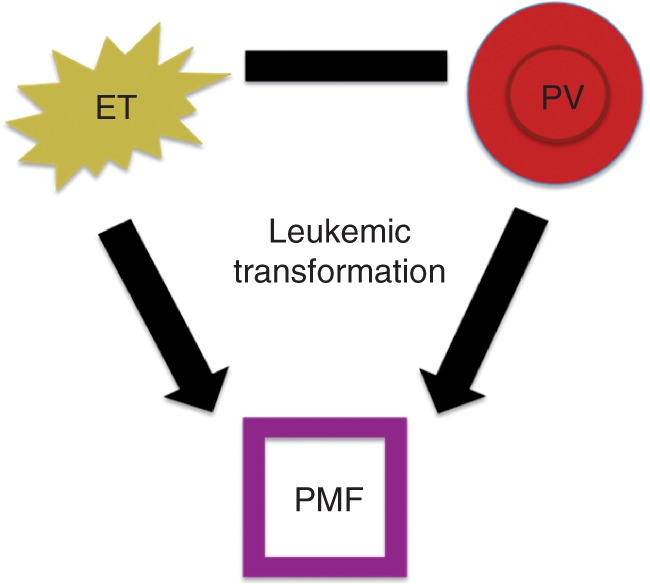
Relationship of Philadelphia-negative myeloproliferative neoplasms. ET, essential thrombocytosis; PV, polycythemia vera; PMF, primary myelofibrosis.
Discovery of JAK2V617F mutations
In 2005, four groups simultaneously identified the somatic JAK2V617F mutation in the majority of MPN patients [Baxter et al. 2005; James et al. 2005; Kralovics et al. 2005; Levine et al. 2005]. The Janus kinase (JAK) family of genes consists of four nonreceptor tyrosine kinases: JAK1, JAK2, JAK3, and TYK2. They contain seven JAK homology domains which are numbered from carboxy to amino-terminus. The somatic mutation from guanine to thymidine results in a valine to phenylalanine substitution at position 617 in the JAK2 pseudokinase (JH2) domain; expression of the JAK2V617F mutant kinase leads to constitutive activation of the JAK2 gene and subsequent activation of signal transducers and activators of transcription (STAT) proteins and to hematopoietic transformation in vitro (as assessed by transformation to cytokine-independent growth). Mutational studies using sensitive, allele-specific assays demonstrate that ∼95% of PV patients are positive for the VF mutation, while ∼50% of ET and PMF patients are positive. The presence of the identical disease allele in three related, but phenotypically distinct myeloid neoplasms, suggests there are additional factors involved in MPN pathogenesis to allow for three distinct phenotypes. However, the genetic linking of three distinct disease entities with one common somatic disease allele unifies these diseases and credentials JAK2 as a therapeutic target in MPN patients.
Role of additional mutations in the JAK-STAT pathway in MPN pathogenesis
Subsequent to the discovery of the JAK2V617F allele, investigators searched for alternate disease alleles in JAK2V617F-negative MPN. This led to the discovery of additional mutations in the JAK/STAT pathway in MPN patients. A subset of patients with JAK2V617F-negative PV or erythrocytosis were found to have somatic mutations in exon 12 of the JAK2 gene [Scott et al. 2007]. A number of different mutations within this exon have been discovered to date [Pietra et al. 2008]. These patients predominately have erythroid expansion without any associated thrombocytosis or leukocytosis and to date these mutations have not been identified in ET or PMF. In contrast, somatic mutations in the MPL gene have been identified in 5-10% of ET/PMF patients [Pardanani et al. 2006; Pikman et al. 2006]. The most common MPL mutation results in lysine or leucine being substituted for tryptophan at position 515, although additional somatic mutations at codons 515 and 505 have subsequently been identified. Expression of mutant MPL alleles in vitro leads to constitutive activation of JAK2 and the JAK-STAT pathway, and in vivo expression of mutant MPL alleles results in marked thrombocytosis, extramedullary hematopoiesis, and MF. Taken together, these data demonstrate that activation of the JAK-STAT pathway is a common pathogenetic event in JAK2V617F-negative MPN.
Treatment of MPNs and development of JAK inhibitors
Classically, PV is treated with therapeutic phlebotomy [Pearson and Wetherley-Mein, 1978]. However, patients with a higher risk of developing disease-related complications require additional treatment. This includes patients who are considered higher risk due to age (>65 years old), and those with a history of prior thrombotic events [Marchioli et al. 2005]. For patients who require cytostatic therapy, hydroxyurea is commonly used, although there is no evidence that it prolongs survival or results in marked reduction in JAK2 mutant allele burden [Larsen et al. 2009]. In contrast, recent studies have shown that treatment with pegylated interferon can result in clinical responses, including complete clinical and molecular responses [Quintas-Cardama et al. 2009; Kiladjian et al. 2008].
Asymptomatic ET patients at low risk of thrombosis are generally observed without therapy with the exception of antiplatelet therapy with aspirin. High-risk ET patients who have increased incidence of thrombosis or bleeding (those over 60 years old or with prior thrombotic events, or with a platelet count over 1500 × 109/1, respectively) [Besses et al. 1999; Ruggeri et al. 1998] are treated with hydroxyurea, anagrelide, or pegylated interferon, most commonly using hydroxyurea as the first-line agent in patients with risk factors for thrombosis [Harrison et al. 2005]. The only current treatment for PMF which can modify disease outcome is allogeneic stem cell transplantation [Deeg et al. 2003]. In contrast there are many treatments used to alleviate PMF symptoms, such as red cell transfusions for anemia, steroids, and splenectomy for abdominal pain and hypersplenism. However, these therapies also have their own risks, and the survival of patients with PMF is poor compared with MPN or age-matched controls. After the discovery of the JAK2V617F mutation, however, the possibility of more precise therapy became apparent, and initial trials of JAK2 inhibitors enrolled PMF and post-PV/ET MF patients given the need for novel therapies for these disease subsets.
The role of somatic alterations that activate tyrosine kinase signaling pathways has been well described. Small molecule inhibitors targeting abnormal tyrosine kinases have therefore been evaluated for the treatment of a spectrum of neoplastic disease, and in many cases have resulted in dramatic improvements in outcomes for patients with kinase-dependent malignancies. The development of imatinib and second-generation ABL kinase inhibitors has dramatically altered the treatment of CML, and similar agents have been developed for other mutant tyrosine kinases [Druker et al. 2001]. For example, drugs which inhibit FLT3, Src, and JAK2 are currently being evaluated in late-stage clinical trials.
JAK inhibitors for MPNs
Like BCR-ABL inhibitors, the first generation of JAK inhibitors are ATP-competitive compounds that interfere with the kinase (JH1) domain function [Lucet et al. 2006]. Multiple studies have shown, both in vitro and in vivo, that JAK inhibitors inhibit the growth and signaling of JAK2V617F mutant cells. Based on these preclinical studies, various JAK inhibitors are currently being tested in clinical trials at all phases of study. Table 1 lists the JAK inhibitors currently being tested in clinical trials as listed by the NIH clinical trials registry.
Table 1.
JAK inhibitors currently in use in clinical trials.
| Drug compound | Selectivity | Trial phase | Diseases enrolled |
|---|---|---|---|
| AZD1480 | JAK2 | I/II | PMF, post-PV/ET-MF |
| CEP701 | JAK2 | I/II | PMF, PV, ET, AML |
| CYT387 | JAK1/JAK2 | I/II | PMF, post-PV/ET-MF |
| INCB018424 | JAK1/JAK2 | I/II/III | AML, ALL, MDS, CML, PMF, PV |
| SB1518 | JAK2 | I/II | AML, CML, CMML, MDS, PMF, Lymphoma |
| TG101348 | JAK2 | I/II | PMF |
| LY2784544 | JAK2 | I | PMF, PV, ET |
PMF, primary myelofibrosis; PV, polycythemia vera; ET, essential thrombocytosis; AML, acute myeloid leukemia; MDS, myelodysplastic syndrome; CML, chronic myeloid leukemia; CMML, chronic myelomonocytic leukemia; MF, myelofibrosis.
INCB018424
INCB018424 is an oral, selective JAK1 and JAK2 inhibitor developed by Incyte. In vitro enzymatic assays showed an IC50 value of 3.3nM for JAK1 and 2.8nM for JAK2 for INCB018424 [Quintas-Cardama et al. 2010]. Studies in Ba/F3 EpoR JAK2V617F cells (an isogenic cell line expressing the VF mutation and overexpressing the erythropoietin receptor) and HEL cells (a human erythroleukemia cell line homozygous for the same JAK2 mutation) demonstrated that INCB018424 treatment inhibited cell growth and JAK-STAT signaling. Studies of INCB018424 in JAK2V617F+ primary cells similarly showed nanomolar activity of INCB018424 at doses lower than those which inhibited the proliferation of normal hematopoietic progenitor cells. In a murine model of JAK2V617F mutant disease (where animals developed splenomegaly and death in a few weeks), INCB018424 treatment was associated with improved survival and in a decrease in spleen weights compared with vehicle-treated animals. The treated mice showed a decreased amount of JAK2V617F expression compared with vehicle by quantitative polymerase chain reaction (PCR), and treatment with INCB018424 decreased phospho-STAT3 levels to that of normal animals when compared with the vehicle arm. Compared with vehicle, there was no difference seen in hematologic parameters with INCB018424. A decrease in circulating cytokines was also seen in the treatment arm as compared with vehicle (although not to the level of naïve animals).
A phase I-II trial of INCB018424 has been conducted in patients with JAK2V617F (+) or (-) PMF and in patients with post-PV or post-ET MF [Verstovsek et al. 2010]. A total of 153 patients were enrolled on the trial and were treated for a median of 14.7 months (75% of patients remained on treatment at the time of publication). Initial starting dose was 25 mg twice daily, with escalation to 50 mg twice daily as tolerated, and once daily dosing was also evaluated. The maximum tolerated dose (MTD) was determined to be 25 mg bid, or 100 mg once per day. The phase II portion utilized multiple dosing schedules, with the majority of patients beginning at 15 mg twice per day followed by patient-specific dosing. (Patients who started at 25 mg twice daily had the best response, but 60% needed to be dose-reduced for thrombocytopenia.) A total of 61 of 140 patients with enlarged spleens at the time of entry into the study had a reduction in palpable spleen size of ≥50%. The response was maintained after 12 months of therapy in over 70% of these patients. Twenty eight patients in the 15 and 25 mg twice-daily dosing groups were transfusion dependent at the time of enrollment, and after a median of 12 weeks of therapy, 14% were transfusion independent (for a median of 20 months). However, 23% of previously transfusion-independent patients enrolled developed a new-onset anemia during therapy. Ten patients had decreases in their elevated platelet counts at 3 months, and seven patients had persistently normal platelet counts for at least 1 year.
Importantly, the majority of patients receiving 10, 15, or 25 mg two times per day had greater than 50% improvement in symptoms (such as itching, bone pain, and abdominal pain); this lasted through 6 months of therapy. The median weight gain after 1 year in these patient groups was 6.6, 9.4, and 7.1 kg, respectively. In addition, the improvement in systemic symptoms and reduced cachexia was associated with changes in systemic inflammation. Specifically, pro-inflammatory cytokines (which are classically elevated in PMF patients) were markedly reduced in a substantial proportion of patients treated with the INCB018424 25 mg twice-daily dose. Effects on JAK2V617F allele burden were also looked at, and in 34 patients who were evaluated the mean maximal suppression of the mutant allele was only 13% from baseline after 12 month-long cycles of treatment with INCB018424. Phase III studies are being carried out in PMF, and additional phase I/II studies are being done in PV/ET and in other malignant contexts including acute leukemia.
CEP-701 (Lestaurtinib)
CEP-701 is an oral tyrosine kinase inhibitor that is known to inhibit FLT3, and was found on a multikinase screen to also inhibit JAK2. The in vitro kinase screen showed an IC50 concentration of 1 nM for JAK2 [Hexner et al. 2008]. Treatment of HEL cells with CEP-701 showed inhibition of phosphorylation of JAK2, and its downstream effectors STAT3 and STAT5. CEP-701 treatment impaired growth of HEL xenograft tumors versus controls. Most importantly, treatment of cultured primary erythroid cells from ET and PMF patients showed significant inhibition of growth and downstream signaling compared with vehicle treatment.
As with INCB018424, a phase II trial of CEP-701 in PMF and post-PV and post-ET MF was completed and results were published recently [Santos et al. 2010]. A total of 22 patients were enrolled on the study, and received a dose of 80 mg two times per day. They were evaluated every 3 months, and patients were followed for a median of 16.5 months. Six patients had a response under the category of clinical improvement as per the International Working Group on Myelofibrosis Research and Treatment (IWG-MRT). Signs of clinical improvement included decreased spleen size, transfusion independence, and improvement in hematologic parameters. None of the responders had improvement in bone marrow fibrosis. Median duration of these responses was 14 months. In contrast to Incyte, which was associated with a low frequency of nonhematopoietic toxicities, a number of patients experienced toxicity, with the most severe effects being gastrointestinal-related symptoms. A decrease in signaling of phospho-STAT3 was seen in responders; however cytokine levels were not improved and there was no significant decrease in JAK2V617F allele burden in the responders.
CYT387
Like CEP-701, CYT387 is a multikinase inhibitor with activity within the JAK family similar to that seen for INCB018424. In an in vitro single-point screening assay, JAK1 and JAK2 were shown to be among a small group of kinases with an IC50 for CYT387 below 100 nM. Specifically, CYT387 was found to have an IC50 of 11 nM for JAK1 and 18 nM for JAK2 [Pardanani et al. 2009b]. Studies in cell lines have shown an IC50 in Ba/F3 EpoR JAK2V617F cells of 500 nM. Treatment with CYT387 was shown to inhibit signaling of downstream effectors in JAK2-mutant hematopoietic cells. CYT387 was evaluated in an in vivo model of JAK2V617F mutant disease using the murine bone marrow transplantation strategy [Tyner et al. 2010]. Mice were treated with either 25 or 50 mg/kg orally, twice daily. Mice receiving 50 mg/kg two times per day had significant improvements in their blood counts, and both groups had significant decreases in spleen size. Bone marrow fibrosis was improved in the highest dose group. Elevated cytokine levels were improved in the treatment group for a number of different cytokines. In the 50 mg/kg dosing group, the JAK2V617F/GFP-positive population was significantly reduced but not eliminated. CYT387 is currently being tested in a phase I/II trial for PMF and secondary MF following PV or ET. Recent data from the phase I trial was presented at the 2010 ASH Annual Meeting. MTD was determined to be 300 mg/day. Limited grade 3 toxicities were seen with no grade 4 toxicities reported. The anemia response rate was found to be 63% overall, and almost all patients had an improvement in splenomegaly and some of their constitutional symptoms. Effect on JAK2V617F allele burden among the 81% of patients who were JAK2 positive is being evaluated over time [Pardanani et al. 2010b].
TG101348
TG101348 is an oral kinase inhibitor that has been found to selectively inhibit JAK2 over the other JAK family kinases. It has greater selectivity for JAK2 than other JAK kinase inhibitors in clinical development. TG101348 demonstrates nanomolar efficacy in vitro in proliferation [Lasho et al. 2008] and signaling assays [Wernig et al. 2008]. The murine JAK2V617F bone marrow model was used to assess the efficacy of TG101348, and mice were treated (for 42 days) with either 60 or 120 mg/kg twice daily. Survival in the higher treatment group was greater than in placebo. These animals had a reduction in hematocrit of ∼18%, and both groups had significant reductions in spleen weights. Erythropoietin-independent erythroid colony formation (EEC) is a feature of JAK2V617F mutant MPN. Treatment of cells from PV patients with 300 or 600nM of TG101348, in the presence of erythropoietin, led to a large reduction in BFU-E formation. Without erythropoietin, the formation of BFU-E was almost completely blocked. A phase I study in PMF and secondary myelofibrosis has been done and preliminary analysis demonstrates the MTD to be 680 mg [Pardanani et al. 2009a]. Long-term data was published recently, with median cumulative exposure to the drug being 380 days. As treatment progressed, more patients showed response in spleen size (increasing from 42% in the first six cycles of treatment to 65% treated beyond six cycles). Of patients with leukocytosis and thrombocytosis at baseline, over 50% showed normalization of counts at the end of 6 and 12 cycles (with 57% having normal white blood cell (WBC) count and 88% having normal platelet counts after 12 cycles). Improvement in constitutional symptoms was seen in most patients, and reduction in JAK2 allele burden was seen in a subset of patients on this trial [Pardanani et al. 2011].
Additional JAK2 inhibitors
AZD1480 is a recently characterized JAK2 inhibitor that has shown efficacy in a spectrum of tumor models [Hedvat et al. 2009]. It is currently being tested in a phase I/II study for primary and secondary myelofibrosis. SB1518 is a JAK2 inhibitor (that also has activity against FLT3) that is being used in phase I/II trials in MPN patients as well as in patients with other hematologic malignancies [Wanner et al. 2010]. LY2784544 is a JAK2 inhibitor being tested in a phase I trial in MPN patients.
Other novel agents for MPNs
Histone deacetylase inhibitors
Histone deacetylase (HDAC) proteins are vital contributors to chromatin structure and subsequently gene expression. Acetylation of histone proteins promotes a closed chromatin structure and suppresses gene expression. HDAC expression and activity has been evaluated in PMF patients [Grana and Marchiolo, 1967]. CD34+ cells were taken from PMF patients and were subjected to a HDAC activity assay. PMF patients showed significantly higher levels of deacetylated protein than other MPN patients or normal controls.
A number of HDAC inhibitors are being tested in MPN patients. ITF2357 (Givinostat) is a class I and II HDAC inhibitor that showed efficacy in vitro in JAK2-mutant cell lines and MPN patient samples [Guerini et al. 2008]. A phase II study of ITF2357 for JAK2V617F-positive patients was completed [Pardanani et al. 2010c]. Twenty nine patients were enrolled for a 24-week treatment period: 18 patients were able to complete the study. (Discontinuation reasons included disease progression, grade 2 thrombocytopenia, and a non-drug-related adverse psychiatric event.) Over half of the patients had some degree of clinical response, with more frequent responses in PV/ET patients than in MF patients. A separate phase II trial is currently recruiting participants to evaluate IT2357 in combination with hydroxyurea in PV patients. A phase I study was recently completed with another HDAC inhibitor, MS-275 (Entinostat), in all hematologic cancers. MK-0683 is a third HDAC inhibitor being evaluated in patients with PV and ET. LBH-589 has been studied preclinically both alone and in combination with a JAK2 inhibitor in MPN model systems and is being investigated in a phase II trial for patients with MF [Lasho et al. 2010]. SAHA (Vorinostat, Zolinza) is a HDAC inhibitor being looked at in combination with Decitabine (Dacogen), which is a DNA methyltransferase inhibitor. These drugs are being evaluated at the phase I level in MPNs.
HSP90 inhibitors
HSP90 is a molecular chaperone that is involved with various client proteins and has been shown to be upregulated in cancer [Schoof et al. 2009]. HSP90 has been shown to interact with JAK2 [Shang and Tomasi, 2006], and recently it was shown that an HSP90 inhibitor, PU-H71, could lead to degradation of JAK2 protein levels, inhibition of JAK-STAT signaling, and marked reductions in aberrant myeloproliferation in murine MPN models without appreciable effects on normal hematopoietic progenitors [Marubayashi et al. 2010]. STA-9090 is an HSP90 inhibitor that is currently being assessed in a phase I trial for MPN and other hematological malignancies. Two additional HSP90 inhibitors, IPI-493 and SNX-5422 Mesylate, are also in phase I trials for patients with hematological malignancies including MPNs.
Additional agents
Kinase inhibitors designed to target other molecules have been used in trials for MPN patients. Erlotinib (Tarceva), an EGFR inhibitor, is being used in a phase II trial for PV patients. Imatinib (Gleevec) is being looked at in phase II for PV. BMS-354825 (Dasatinib) is a BCR-ABL and Src kinase inhibitor; it was recently evaluated in a phase II trial for PV patients. TAK-901 is an Aurora kinase B inhibitor that is being studied in a phase I for various advanced hematological malignancies (including PV and MF).
CC-4047 (Pomalidomide) is a thalidomide derivative that is being studied in two trials, in both primary and secondary MF, alone and in combination with prednisone. Bevacizumab (Avastin) is a VEGF-A inhibitor and acts as an anti-angiogenic agent. It is being evaluated in a phase II for MF patients. Arsenic trioxide is being studied at the phase I level in MF. Plitidepsin (Aplidin) is a marine-derived biologic that has various anticancer properties, such as initiation of the JNK pathway [Pardanani et al. 2010a], caspase activation, and induction of G1 arrest [Ramakrishnan et al. 2010].
Are we hitting the target/future directions?
As the main class of agents in study for targeting MPN, JAK inhibitors have provided a great deal of hope and potential for many researchers and patients. In preclinical and clinical studies, JAK inhibitors can mitigate many of the sequelae of myeloproliferation, including extramedullary hematopoiesis and constitutional symptoms. However, the mechanism by which these benefits are achieved, and whether these clinical benefits are all due to JAK2 inhibition, has not been delineated conclusively. Nonetheless, the clinical benefit to date represents an important achievement in the therapeutic development of targeted agents for MPN patients who clearly do benefit from this class of agents.
Despite the positive clinical improvement seen with these agents, the lack of pathologic, complete hematologic, or significant (>1 log fold) molecular responses raises questions as to whether these agents, at the doses given are able to potently inhibit JAK2, or if the lack of optimal efficacy reflects incomplete dependence on JAK2 by the MPN clone. Importantly, it has not been shown for any of the above therapies whether in vivo treatment lead to maximal inhibition of JAK2 kinase activity in vivo itself (and not just inhibition of downstream targets), and if the side effects observed with these agents are due to JAK2 inhibition or due to off-target effects. In addition, work by Mullally and colleagues using a newly generated JAK2V617F conditional knock-in mouse has shown that treatment with a JAK2 inhibitor, while leading to clinical improvement, did not eradicate the disease-initiating stem cell population. Purified LSK cells from inhibitor treated mice were able to induce disease in secondary recipients. Importantly, prolonged treatment of these secondary recipients still did not prevent propagation of disease with unfractionated bone marrow transplanted into tertiary recipients [Mullally et al. 2010]. Finally, and most importantly, the efficacy of combining JAK2 inhibitors with other novel therapies has not yet been assessed, and may provide a hope for improved efficacy and outcomes for MPN patients compared to JAK inhibitor monotherapy. We predict much insight will come from current and future preclinical and clinical trials in the MPN field.
Footnotes
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
None declared.
References
- Baxter E.J., Scott L.M., Campbell P.J., East C., Fourouclas N., Swanton S., et al. (2005) Acquired mutation of the tyrosine kinase JAK2 in human myeloproliferative disorders. Lancet 365: 1054–1061 [DOI] [PubMed] [Google Scholar]
- Besses C., Cervantes F., Pereira A., Florensa L., Sole F., Hernandez-Boluda J.C., et al. (1999) Major vascular complications in essential thrombocythemia: A study of the predictive factors in a series of 148 patients. Leukemia 13: 150–154 [DOI] [PubMed] [Google Scholar]
- Dameshek W. (1951) Some speculations on the myeloproliferative syndromes. Blood 6: 372–375 [PubMed] [Google Scholar]
- Deeg H.J., Gooley T.A., Flowers M.E., Sale G.E., Slattery J.T., Anasetti C., et al. (2003) Allogeneic hematopoietic stem cell transplantation for myelofibrosis. Blood 102: 3912–3918 [DOI] [PubMed] [Google Scholar]
- Druker B.J., Sawyers C.L., Kantarjian H., Resta D.J., Reese S.F., Ford J.M., et al. (2001) Activity of a specific inhibitor of the BCR-ABL tyrosine kinase in the blast crisis of chronic myeloid leukemia and acute lymphoblastic leukemia with the Philadelphia chromosome. N Engl J Med 344: 1038–1042 [DOI] [PubMed] [Google Scholar]
- Grana A., Marchiolo B. (1967) [Contribution to the study of the clearance of I-131 in skin grafts]. Minerva Dermatol 42: 83–85 [PubMed] [Google Scholar]
- Guerini V., Barbui V., Spinelli O., Salvi A., Dellacasa C., Carobbio A., et al. (2008) The histone deacetylase inhibitor ITF2357 selectively targets cells bearing mutated JAK2(V617F). Leukemia 22: 740–747 [DOI] [PubMed] [Google Scholar]
- Harrison C.N., Campbell P.J., Buck G., Wheatley K., East C.L., Bareford D., et al. (2005) Hydroxyurea compared with anagrelide in high-risk essential thrombocythemia. N Engl J Med 353: 33–45 [DOI] [PubMed] [Google Scholar]
- Hedvat M., Huszar D., Herrmann A., Gozgit J.M., Schroeder A., Sheehy A., et al. (2009) The JAK2 inhibitor AZD1480 potently blocks Stat3 signaling and oncogenesis in solid tumors. Cancer Cell 16: 487–497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hexner E.O., Serdikoff C., Jan M., Swider C.R., Robinson C., Yang S., et al. (2008) Lestaurtinib (CEP701) is a JAK2 inhibitor that suppresses JAK2/STAT5 signaling and the proliferation of primary erythroid cells from patients with myeloproliferative disorders. Blood 111: 5663–5671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- James C., Ugo V., Le Couedic J.P., Staerk J., Delhommeau F., Lacout C., et al. (2005) A unique clonal JAK2 mutation leading to constitutive signalling causes polycythaemia vera. Nature 434: 1144–1148 [DOI] [PubMed] [Google Scholar]
- Kiladjian J.J., Cassinat B., Chevret S., Tourlure P., Cambier N., Roussel M., et al. (2008) Pegylated interferon alpha-2a induces complete hematological and molecular responses with low toxicity in polycythemia vera. Blood, in press. [DOI] [PubMed] [Google Scholar]
- Kralovics R., Passamonti F., Buser A.S., Teo S.S., Tiedt R., Passweg J.R., et al. (2005) A gain-of-function mutation of JAK2 in myeloproliferative disorders. N Engl J Med 352: 1779–1790 [DOI] [PubMed] [Google Scholar]
- Larsen T.S., Pallisgaard N., de Stricker K., Moller M.B., Hasselbalch H.C. (2009) Limited efficacy of hydroxyurea in lowering of the JAK2 V617F allele burden. Hematology 14: 11–15 [DOI] [PubMed] [Google Scholar]
- Lasho T.L., Pardanani A., Tefferi A. (2010) LNK mutations in JAK2 mutation-negative erythrocytosis. N Engl J Med 363: 1189–1190 [DOI] [PubMed] [Google Scholar]
- Lasho T.L., Tefferi A., Hood J.D., Verstovsek S., Gilliland D.G., Pardanani A. (2008) TG101348, a JAK2-selective antagonist, inhibits primary hematopoietic cells derived from myeloproliferative disorder patients with JAK2V617F, MPLW515K or JAK2 exon 12 mutations as well as mutation negative patients. Leukemia 22: 1790–1792 [DOI] [PubMed] [Google Scholar]
- Levine R.L., Gilliland D.G. (2008) Myeloproliferative disorders. Blood 112: 2190–2198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine R.L., Wadleigh M., Cools J., Ebert B.L., Wernig G., Huntly B.J., et al. (2005) Activating mutation in the tyrosine kinase JAK2 in polycythemia vera, essential thrombocythemia, and myeloid metaplasia with myelofibrosis. Cancer Cell 7: 387–397 [DOI] [PubMed] [Google Scholar]
- Lucet I.S., Fantino E., Styles M., Bamert R., Patel O., Broughton S.E., et al. (2006) The structural basis of Janus kinase 2 inhibition by a potent and specific pan-Janus kinase inhibitor. Blood 107: 176–183 [DOI] [PubMed] [Google Scholar]
- Marchioli R., Finazzi G., Landolfi R., Kutti J., Gisslinger H., Patrono C., et al. (2005) Vascular and neoplastic risk in a large cohort of patients with polycythemia vera. J Clin Oncol 23: 2224–2232 [DOI] [PubMed] [Google Scholar]
- Marubayashi S., Koppikar P., Taldone T., Abdel-Wahab O., West N., Bhagwat N., et al. (2010) HSP90 is a therapeutic target in JAK2-dependent myeloproliferative neoplasms in mice and humans. J Clin Invest 120: 3578–3593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullally A., Lane S.W., Ball B., Megerdichian C., Okabe R., Al-Shahrour F., et al. (2010) Physiological Jak2V617F expression causes a lethal myeloproliferative neoplasm with differential effects on hematopoietic stem and progenitor cells. Cancer Cell 17: 584–596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pardanani A., Brown P., Neben-Wittich M., Tobin R., Tefferi A. (2010a) Effective management of accelerated phase myelofibrosis with low-dose splenic radiotherapy. Am J Hematol 85: 715–716 [DOI] [PubMed] [Google Scholar]
- Pardanani A., George G., Lasho T., Hogan W.J., Litzow M.R., Begna K., et al. (2010b) A phase I/II study of CYT387, an oral JAK-1/2 inhibitor, in myelofibrosis: Significant response rates in anemia, splenomegaly, and constitutional symptoms. Blood 116, abstract 460. [Google Scholar]
- Pardanani A., Gotleib J., Jamieson C., Cortes J., Talpaz M., Stone R., et al. (2009a) A phase I evaluation of TG101348, a selective JAK2 inhibitor, in myelofibrosis: clinical response is accompanied by significant reduction in JAK2V617F allele burden. Blood-American Society of Hematology Annual Meeting, in press.
- Pardanani A., Gotlib J.R., Jamieson C., Cortes J.E., Talpaz M., Stone R.M., et al. (2011) Safety and efficacy of TG101348, a selective JAK2 inhibitor, in myelofibrosis. J Clin Oncol, in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pardanani A., Lasho T., Smith G., Burns C.J., Fantino E., Tefferi A. (2009b) CYT387, a selective JAK1/JAK2 inhibitor: In vitro assessment of kinase selectivity and preclinical studies using cell lines and primary cells from polycythemia vera patients. Leukemia 23: 1441–1445 [DOI] [PubMed] [Google Scholar]
- Pardanani A., Vannucchi A.M., Passamonti F., Cervantes F., Barbui T., Tefferi A. (2010c) JAK inhibitor therapy for myelofibrosis: Critical assessment of value and limitations. Leukemia, in press. [DOI] [PubMed]
- Pardanani A.D., Levine R.L., Lasho T., Pikman Y., Mesa R.A., Wadleigh M., et al. (2006) MPL515 mutations in myeloproliferative and other myeloid disorders: A study of 1182 patients. Blood 108: 3472–3476 [DOI] [PubMed] [Google Scholar]
- Pearson T.C., Wetherley-Mein G. (1978) Vascular occlusive episodes and venous haematocrit in primary proliferative polycythaemia. Lancet 2: 1219–1222 [DOI] [PubMed] [Google Scholar]
- Pietra D., Li S., Brisci A., Passamonti F., Rumi E., Theocharides A., et al. (2008) Somatic mutations of JAK2 exon 12 in patients with JAK2 (V617F)-negative myeloproliferative disorders. Blood 111: 1686–1689 [DOI] [PubMed] [Google Scholar]
- Pikman Y., Lee B.H., Mercher T., McDowell E., Ebert B.L., Gozo M., et al. (2006) MPLW515L is a novel somatic activating mutation in myelofibrosis with myeloid metaplasia. PLoS Med 3: e270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quintas-Cardama A., Kantarjian H., Manshouri T., Luthra R., Estrov Z., Pierce S., et al. (2009) Pegylated interferon alfa-2a yields high rates of hematologic and molecular response in patients with advanced essential thrombocythemia and polycythemia vera. J Clin Oncol 27: 5418–5424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quintas-Cardama A., Vaddi K., Liu P., Manshouri T., Li J., Scherle P.A., et al. (2010) Preclinical characterization of the selective JAK1/2 inhibitor INCB018424: Therapeutic implications for the treatment of myeloproliferative neoplasms. Blood 115: 3109–3117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramakrishnan V., Kimlinger T., Haug J., Timm M., Wellik L., Halling T., et al. (2010) TG101209, a novel JAK2 inhibitor, has significant in vitro activity in multiple myeloma and displays preferential cytotoxicity for CD45+ myeloma cells. Am J Hematol 85: 675–686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruggeri M., Finazzi G., Tosetto A., Riva S., Rodeghiero F., Barbui T. (1998) No treatment for low-risk thrombocythaemia: Results from a prospective study. Br J Haematol 103: 772–777 [DOI] [PubMed] [Google Scholar]
- Santos F.P., Kantarjian H.M., Jain N., Manshouri T., Thomas D.A., Garcia-Manero G., et al. (2010) Phase 2 study of CEP-701, an orally available JAK2 inhibitor, in patients with primary or post-polycythemia vera/essential thrombocythemia myelofibrosis. Blood 115: 1131–1136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoof N., von Bonin F., Trumper L., Kube D. (2009) HSP90 is essential for JAK-STAT signaling in classical Hodgkin lymphoma cells. Cell Commun Signal 7: 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott L.M., Tong W., Levine R.L., Scott M.A., Beer P.A., Stratton M.R., et al. (2007) JAK2 exon 12 mutations in polycythemia vera and idiopathic erythrocytosis. N Engl J Med 356: 459–468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shang L., Tomasi T.B. (2006) The heat shock protein 90-CDC37 chaperone complex is required for signaling by types I and II interferons. J Biol Chem 281: 1876–1884 [DOI] [PubMed] [Google Scholar]
- Tyner J.W., Bumm T.G., Deininger J., Wood L., Aichberger K.J., Loriaux M.M., et al. (2010) CYT387, a novel JAK2 inhibitor, induces hematologic responses and normalizes inflammatory cytokines in murine myeloproliferative neoplasms. Blood 115: 5232–5240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verstovsek S., Kantarjian H., Mesa R.A., Pardanani A.D., Cortes-Franco J., Thomas D.A., et al. (2010) Safety and efficacy of INCB018424, a JAK1 and JAK2 inhibitor, in myelofibrosis. N Engl J Med 363: 1117–1127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wanner S.P., Guimaraes J.B., Pires W., La Guardia R.B., Haibara A.S., Marubayashi U., et al. (2010) Physical exercise-induced cardiovascular adjustments are modulated by muscarinic cholinoceptors within the ventromedial hypothalamic nucleus. Physiol Res 59: 165–175 [DOI] [PubMed] [Google Scholar]
- Wernig G., Kharas M.G., Okabe R., Moore S.A., Leeman D.S., Cullen D.E., et al. (2008) Efficacy of TG101348, a selective JAK2 inhibitor, in treatment of a murine model of JAK2V617F-induced polycythemia vera. Cancer Cell 13:S 311–320 [DOI] [PubMed] [Google Scholar]


