Abstract
Objective
There are no published empirical studies on the DSM-5 proposed Disruptive Mood Dysregulation disorder. This study will estimate prevalence, comorbidity, and correlates of this proposed disorder in the community.
Methods
Prevalence rates were estimated using data from three community studies involving 7,881 observations of 3,258 participants covering ages 2 to 17. Disruptive mood dysregulation disorder was diagnosed using items from structured psychiatric interviews.
Results
Three-month prevalence rates for meeting disruptive mood dysregulation disorder criteria ranged from 0.8% to 3.3% with the highest rate in preschoolers. These rates dropped slightly with strict application of the exclusion criterion, but were largely unaffected by application of the onset and duration criteria. Disruptive mood dysregulation disorder co-occurred with all common psychiatric disorders. The highest levels of co-occurrence were with depressive disorders (odds ratios between 9.9 and 23.5) and oppositional defiant disorder (odds ratios between 52.9 and 103.0). Sixty-two to 92% of the time disruptive mood dysregulation disorder occurred with another disorder and 32 to 68% of the time it occurred with both an emotional and a behavioral disorder. Affected children displayed elevated rates of social impairments, school suspension, service use, and poverty.
Conclusions
Disruptive mood dysregulation disorder is relatively uncommon after early childhood, frequently co-occurs with other psychiatric disorders, and meets common standards for psychiatric “caseness.” This disorder identifies children with severe levels of both emotional and behavioral dysregulation.
Keywords: Childhood, Irritability, Oppositional Defiant disorder, Mood disorders, DSM-5
Introduction
Disruptive Mood Dysregulation disorder (briefly labeled temper dysregulation disorder with dysphoria) has been proposed by the DSM-5 Childhood Disorders and Mood Disorders Work Groups to account for children with severe emotional and behavioral problems of which a prominent feature is nonepisodic (or chronic) irritability (1). Such a phenotype had been conceptualized as pediatric bipolar disorder (1, 2), but evidence from both community and clinical longitudinal studies has suggested that such irritability is associated with later unipolar, but not bipolar, mood disorders (3–5). The Work Groups adapted the “severe mood disturbance” category proposed by Leinbenluft and colleagues(6) by opting for a more descriptive name and eliminating hyperarousal as a criterial symptom. Thus the criteria for the proposed disorder include frequent (3+ weekly) severe temper outbursts combined with persistently negative mood between outbursts. These symptoms must be present for at least 12 months in multiple settings, have an onset before age 10, and the child must be at least 6 years of age. This has proven to be one of the more controversial proposals for DSM-5 (7–10).
Concerns related to this proposed diagnosis fall into two groups: 1) the potential negative consequences of adding a new childhood diagnostic category (e.g., the possibility that it might result in increased medication use with young children, or a popular backlash against pathologizing “normal” behavior); and 2) the lack of any empirical basis for this definition (7–10). The justification for disruptive mood dysregulation disorder itself states that “It can certainly be argued that it is premature to suggest the addition of the disruptive mood dysregulation disorder diagnosis to DSM-5, since the work has been done predominately by one research group in a select research setting and many questions remain unanswered”(1). But this understates the problem. All research to date has focused on severe mood dysregulation, not the proposed disruptive mood dysregulation disorder criteria. As noted above, the latter omitted the hyperarousal criterion, and also differ in terms of criteria related to the onset of symptoms (age 10 for disruptive mood dysregulation disorder as compared to age 12 for severe mood dysregulation). There are, in fact, no published empirical studies that have focused on the newly proposed criteria for disruptive mood dysregulation disorder. The goal of this analysis is to provide a review of the relative utility of the proposed criteria in community samples of children and to determine whether children meeting these criteria display a pattern of functioning indicative of psychopathology.
Methods
Participants
Table 1 provides a comparison of the three community-based samples used in this study.
Table 1.
Comparison of three community-based samples
| Duke Preschool Anxiety | Great Smoky Mountains | Caring for Children in the Community | |
|---|---|---|---|
| Total Subjects | 918 | 1420 | 920 |
| Observations | 918 | 5336 | 1627 |
| Informant | Parent only | Parent and Self-report | Parent and Self-report |
| Age | M=3.9 (SD=1.3) Range: 2 to 6 | M=13.7 (SD=2.0) Range: 9 to 17 | M=14.2 (SD=3.4) Range: 9 to 17 |
| Sex | 51.8% female | 49.2% female | 50.0% female |
| Race/Ethnicity | 62.1% white; 37.5% African American; 0.5% Other | 89.8% White; 6.4% African-American; 3.8% Native American | 41.0% White; 53.8% African-American; 5.2% Other |
| Interview | Preschool Age Psychiatric Assessment | Child and Adolescent Psychiatric Assessment | Child and Adolescent Psychiatric Assessment |
The Duke Preschool Anxiety Study
The Duke Preschool Anxiety study is a cross-sectional study of a representative sample of preschoolers (ages 2–5) attending a large primary care pediatric clinic in Central NC. 3,424 clinic attendees were screened with the parent-report anxious/depressed scale of the Child Behavior Checklist. Parents of 100% of those scoring 4 or more on the screen plus a 7.3% random sample of the rest received a diagnostic interview. Of 1125 subjects selected, parents of 918 children agree to complete interviews (81.6%). 49% of the children were female; 42% were African American, 43% were white. Data from an earlier sample recruited from this clinical setting indicated that the mean and standard deviation of scores on the total symptom scale of the Child Behavior Checklist 1½-5 were almost identical to those reported from for the national norms. (11) The majority (58%) were attending for well visits.
Great Smoky Mountains Study
The Great Smoky Mountains study is a longitudinal, representative study of children in 11 predominantly-rural counties of North Carolina (12). Three cohorts of children, ages 9, 11, and 13 years, were recruited from a pool of some 20,000 children using a two-stage sampling design. Of the 1,777 selected to participate in interviews, 1,420 interviews were completed (79.9%; see also (12)). American Indians were oversampled to constitute 25% of the sample; seven percent of the participants were African American. Annual assessments were completed on the 1420 children until age 16 for a total of 6634 assessments. The youngest cohort was not interviewed at age 13 and only half of the youngest cohort was interviewed at age 14 because of funding limitations.
Caring for Children in the Community
The Caring for Children in the Community study is a longitudinal, representative study of 920 children aged 9 to 17 from four rural counties in North Carolina (13). A random sample of 17,117 9-17-year-olds in the public schools database generated a screening sample of 4,500 youth. Of these, 3613 were contacted and agreed to complete screens (the externalizing scale of the Child Behavior Checklist). Of these families, 1302 were selected to participate in the interviews, and 920 (70.7%) interviews were completed. Fifty-four percent of the participants were African American and 50% were female. Two additional assessments were completed at 9 month intervals for participants who not yet reached age 18.
For all studies, interviews were completed by a parent figure, and by the subject if 9 years old or older. Before interviews in each study began, parent and child signed informed consent/assent forms approved by the Duke University Medical Center Institutional Review Board. All interviewers had at least bachelor's level degrees. They received one month of training and constant quality control.
Measures
Disruptive Mood Dysregulation Disorder
None of the studies was designed to assess disruptive mood dysregulation disorder. It was, however, possible to define disruptive mood dysregulation disorder because its criteria overlap entirely with those of other common disorders. The psychiatric status of all samples was assessed with the Child and Adolescent Psychiatric Assessment (14, 15) or its down-aged congener the Preschool Age Psychiatric Assessment (11). A symptom was counted as present if parent, child or both endorsed it. To minimize recall bias, the timeframe for determining the presence of psychiatric symptoms was the preceding 3 months. However, because onset dates were collected for all items, the duration criterion was determinable.
Definitions for disruptive mood dysregulation disorder criteria were identical across studies (see http://devepi.duhs.duke.edu/codebooks.html for codebook). Criterion A was defined by items assessing temper outbursts and tantrums as part of the oppositional/conduct problems section. If these behaviors were reported, the informant was then queried about the frequencies of these behaviors at home, school, and elsewhere. We could, therefore, calculate whether these behaviors occurred 3 or more times weekly (Criterion B) and whether they occurred across multiple settings (Criterion E). Frequency of losing temper in different contexts was not assessed for the first wave of the Great Smoky Mountains study, and so this wave was not included in the current analyses for this manuscript. Criterion C was assessed through items about the frequency of depressed, sad, irritable, or angry mood or low frustration threshold. Subjects were required to display these moods on more days than not. Onsets for temper outbursts and negative mood were used to establish a duration of more than 12 months (Criterion D) and onset before age 10 (Criterion G). Criterion F requires a chronological age of at least 6 years for the diagnosis to be made. Of course, nearly all participants in the preschool sample would be excluded if this criterion were applied to them. In order to be able to compare the potential presentation of disruptive mood dysregulation disorder in young children with that in older children we ignored criterion F in the preschool sample. Criteria H and I are exclusions based upon other psychiatric disorders or conditions. Criterion H refers to a manic episode in the past year. Across all samples, this was vanishingly rare and had no impact on DMDD diagnosis. The I criterion, however, would affect prevalence rates as it involves an exclusion for common mood disorders. However, in a study aiming to explore the utility of the proposed criteria, it would make little sense to exclude one of the most likely “competing” categories a priori. The effects of hierarchical rules will be examined empirically.
Psychiatric Comorbidities
Diagnostic groups included depressive disorders, anxiety disorders (generalized anxiety disorder, social phobia, separation anxiety disorder, and specific phobia), conduct disorder, ADHD, and oppositional defiant disorder. Children meeting criteria for conduct disorder were allowed to meet criteria for oppositional defiant disorder as well. For specific analyses, disorders were categorized as either emotional which included anxiety and depressive disorders or behavioral which included conduct disorder, oppositional defiant disorder and ADHD. Two-week test-retest reliabilities of interview-derived diagnoses were comparable to those of other structured interviews with kappas ranging from .36 to 1.0 (11, 14).
Impairments
Psychosocial impairment secondary to psychiatric symptomatology was assessed in areas of functioning related to life at home, at school and elsewhere (see (14), for a full description of the concept of impairment implemented in the CAPA). For this analysis, impairment variables were constructed related to social functioning between the subject and his/her parents, sibling and teachers. In addition, recent suspension from school was noted.
Sociodemographic correlates
Poverty status was coded using thresholds issued by the Census Bureau based on income and family size (16). Parental school dropout was coded if the participant's parents had not graduated from high school. Single parent was coded if the parent reported only one parental figure in the house.
Service use
Service utilization for mental health problems was identified using the Child and Adolescent Services Assessment,(17, 18) an interview for the parent and child that provides details of mental health service use during the 3 months preceding the interview. For this paper, services were categorized into five domains: specialty mental health, general medical, school, child welfare, and juvenile justice.
Analytic strategy
Participants from all samples were assigned a weight inversely proportional to their probability of selection to account for screen-stratification, so that the results from our analyses reported here represent unbiased estimates for the original populations from which the samples were drawn. Sandwich type variance corrections (19) were applied to adjust for the parameter and variance effects induced by the sampling stratification and repeated observations. Odds ratios for comorbidity analyses or associations with other variables were conducted using weighted logistic regression in the SAS procedure GENMOD.
Results
Prevalence rates
Three-month prevalence rates are provided for each criterion in Table 2. Estimates for those meeting all criteria except the exclusion criteria ranged from 0.8% to 3.3%. Rates for the full diagnosis and each criterion were highest in the preschool sample. Temper outbursts and negative mood (criteria A and C) were common across all samples. The application of frequency, duration and cross-context criteria (B, D, and E) limited the rates of those meeting full criteria. Having an onset before age 10 had little impact on final prevalence rates in the two older samples. The only sex difference in the rates of individual criteria in any of the three samples was for criterion E (multiple settings) in the Great Smoky Mountains study (3.6% in males vs. 1.9% in females, p = 0.007). There were no differences in the rates of the full diagnosis by sex in any of the three samples. In the Great Smoky Mountains study, which included multiple observations across childhood and adolescence, the cumulative prevalence by age 16 was 4.4% (SE=0.9).
Table 2.
Prevalence rates of disruptive mood dysregulation disorder and individual criteria in three community samples
| Duke Preschool Anxiety Study | Great Smoky Mountains Study | Caring for Children in the Community | ||||
|---|---|---|---|---|---|---|
| Criterion | Total N=918 | Total N=5336 | Total N=1627 | |||
| % | N | % | N | % | N | |
| A. Severe tantrums | 80.8 | 769 | 45.7 | 2465 | 49.0 | 871 |
| B. Frequency | 17.7 | 182 | 7.1 | 514 | 6.3 | 140 |
| C. Negative mood | 21.1 | 268 | 12.8 | 798 | 8.2 | 179 |
| D. Duration | 5.9 | 92 | 2.8 | 221 | 1.5 | 42 |
| E. Multiple Settings | 10.1 | 116 | 2.8 | 229 | 3.8 | 101 |
| Excluding onset criterion | -- | -- | 1.2 | 99 | 0.9 | 33 |
| Excluding duration criterion | -- | -- | 1.6 | 143 | 1.2 | 47 |
| Full criteria | 3.3 | 58 | 1.1 | 89 | 0.8 | 31 |
DMDD= Disruptive mood dysregulation disorder. Percentages are weighted and Ns are unweighted. The criterion that a subject must be at least age 6 to be diagnosed with disruptive mood dysregulation disorder was not applied. Also, the exclusion criteria was not applied, rates with application of the exclusion rate are provided in table 2.
The higher rates of severe tantrums and negative mood in the younger sample are consistent with findings from developmental psychopathology (e.g., (20)). If the frequency thresholds for tantrums and negative mood were tightened to require preschoolers to display these problems every day, then 10.3% (SE=1.8) of children would meet criterion B, 16.9% (SE=2.1) would meet criterion C, and 1.7% (SE=2.1) would meet full diagnostic criteria. This rate is still higher than in the older samples, but these thresholds also indicate a high level of emotional and behavioral dysregulation.
Comorbidity
One of the primary questions for this proposed disorder has been the degree to which it overlaps with other psychiatric disorders. Table 3 shows the rates of co-occurrence between disruptive mood dysregulation disorder and other common psychiatric disorders. Disruptive mood dysregulation disorder significantly co-occurs with all common psychiatric disorders with the exception of anxiety disorders and attention-deficit/hyperactivity disorder in one dataset, although even in these cases there was evidence of overlap. The highest levels of co-occurrence were with depressive disorders (odds ratios between 9.9 and 23.5) and oppositional defiant disorder (odds ratios between 52.9 and 103.0). Rates of disruptive mood dysregulation disorder in those without a depressive disorder provide the prevalence rate if the exclusion criterion were strictly applied. Application of this criterion reduces the rates to 2.9% (SE=0.8) in the preschool sample, 0.8% (SE=0.2) in the Great Smoky Mountains sample, and 0.8% (SE=0.2) in the Caring for Children in the Community sample.
Table 3.
Comorbidity rates between disruptive mood dysregulation disorder and other common psychiatric disorders
| Duke Preschool Anxiety Study | |||||||
|---|---|---|---|---|---|---|---|
| % Rate of DMDD in | % Rate of dx in | OR | CI | p | |||
| Comorbidity | dx | No dx. | DMDD | No DMDD | |||
| Depressive | 23.0 | 2.9 | 12.4 | 1.4 | 9.9 | 4.1–23.7 | <0.0001 |
| Anxiety | 7.5 | 1.3 | 72.9 | 30.7 | 6.1 | 1.9–19.0 | 0.002 |
| ODD | 37.7 | 1.1 | 67.7 | 3.8 | 52.9 | 17.1–163.8 | <0.0001 |
| Conduct Disorder | 9.7 | 2.8 | 22.1 | 7.0 | 3.8 | 1.5–9.3 | 0.004 |
| ADHD | 23.5 | 2.4 | 30.8 | 3.4 | 12.6 | 4.0–39.6 | <0.0001 |
| Great Smoky Mountains Study | |||||||
| Depressive | 15.6 | 0.8 | 32.7 | 2.1 | 23.5 | 9.9–56.1 | <0.0001 |
| Anxiety | 5.5 | 1.0 | 9.3 | 1.8 | 5.2 | 1.2–22.9 | 0.03 |
| ODD | 23.3 | 0.5 | 57.4 | 2.2 | 61.0 | 27.7–134.4 | <0.0001 |
| Conduct Disorder | 10.9 | 0.9 | 23.1 | 2.1 | 11.9 | 3.4–41.0 | <0.0001 |
| ADHD | 9.2 | 1.1 | 6.3 | 0.7 | 7.6 | 2.9–19.7 | <0.0001 |
| Caring for Children in the Community Study | |||||||
| Depressive | 11.8 | 0.8 | 35.8 | 3.2 | 16.3 | 6.3–42.1 | <0.0001 |
| Anxiety | 2.5 | 1.1 | 7.7 | 3.6 | 2.2 | 0.6–8.2 | 0.25 |
| ODD | 27.0 | 0.4 | 70.6 | 2.3 | 103.0 | 40.1–264.2 | <0.0001 |
| Conduct Disorder | 5.3 | 1.0 | 18.8 | 4.0 | 4.4 | 1.2–15.3 | 0.02 |
| ADHD | 4.3 | 1.1 | 9.4 | 1.8 | 2.9 | 0.4–23.3 | 0.32 |
DMDD= Disruptive mood dysregulation disorder; ODD = Oppositional defiant disorder; ADHD = Attention-deficit/hyperactivity disorder. Bolded p values are significant at p <0.05.
Seven manic episodes were reported across 6963 observations in the older samples. Only one of these cases overlapped with disruptive mood dysregulation disorder. Levels of comorbidity were similar when applying the exclusion criterion for those with mania. We also looked at the overlap with Leibenluft's Severe Mood Disturbance which has previously been studied in the Great Smoky Mountains study (5). The levels of co-occurrence were high (OR=44.5; 95% CI 18.5–107.1, p < 0.001) with 38.9% of severe mood disturbance cases meeting criteria for disruptive mood dysregulation disorder.
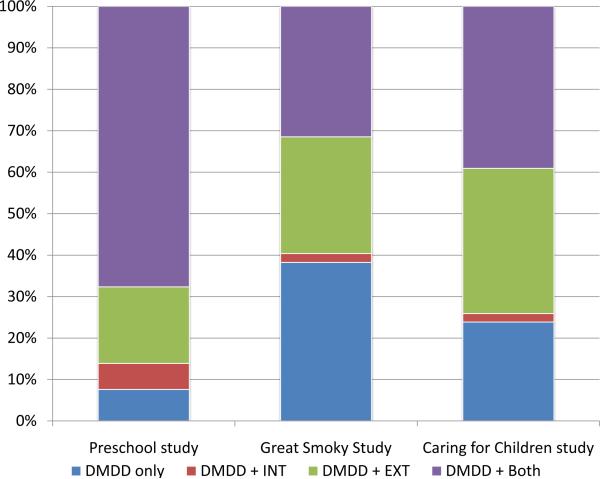
Figure 1 shows how often disruptive mood dysregulation disorder overlapped with emotional disorders (anxiety or depressive disorders), behavioral disorders (conduct, oppositional defiant or attention-deficit/hyperactivity disorder) or both. Although there were variations across samples, the most common presentation in each sample was to be comorbid with another disorder. The likelihood of disruptive mood dysregulation disorder alone ranged from 8% in the preschool sample to 38% in the Great Smoky Mountains sample. (For comparison, conduct disorder occurred alone 64% of the time and depression occurred alone 36.6% of the time in the Great Smoky Mountains Study.) The likelihood of disruptive mood dysregulation disorder occurring with both an emotional and behavioral disorder ranged from 68% in the preschool sample to 32% in the Great Smoky Mountains sample.
Figure 1.
These charts indicate the rates of individuals with disruptive mood dysregulation disorder only, disruptive mood dysregulation disorder plus emotional disorders, disruptive mood dysregulation disorder plus behavioral disorders or disruptive mood dysregulation disorder plus both emotional and behavioral disorders in the Duke Preschool Anxiety Study (A), Great Smoky Mountains Study (B), and Caring for Children in the Community study (C).
Impairment, Service use and Sociodemographic correlates
Table 3 shows the relationships between disruptive mood dysregulation disorder and impairments, service use, and sociodemograhic correlates in the studies of older children. Subjects with disruptive mood dysregulation disorder had higher levels of all social impairments and also had elevated rates of recent suspension. Rates of service use were universally elevated in affected subjects compared with those without a diagnosis. Subjects were more likely to come from impoverished families, although this was not necessarily accounted for by family structure or parental educational attainment.
Given the high degree of overlap between disruptive mood dysregulation disorder and other disorders, it is reasonable to suggest that these associations might be accounted for by such comorbidity. Analyses from table 3 were rerun in the Great Smoky Mountains Study, excluding those who met criteria for any other DSM disorders. All significant findings continued to be significant except those for impairment in relations with teacher and any service use.
Discussion
This is the first study to apply the proposed criteria for disruptive mood dysregulation disorder in community samples. The studies covered ages 2 to 18 in rural and urban communities and included large groups of European-Americans, African Americans and American Indians. Disruptive mood dysregulation disorder occurred at relatively low rates in the community, and most often occurred in combination with other psychiatric disorders. This propensity toward comorbidity extended to all common psychiatric disorders but was strongest for oppositional defiant disorder and depressive disorders. Overall, disruptive mood dysregulation disorder met the standards of psychiatric caseness tested: It was comorbid with psychiatric disorders, associated with high levels of social impairment, school suspension, all types of service use and family poverty. This does not clarify, however, its distinctiveness from existing disorders.
A few limitations should be kept in mind. First, the investigation of disruptive mood dysregulation disorder from the three studies relied exclusively upon psychiatric interviews designed to assess other disorders. Test-retest reliability data are not available for disruptive mood dysregulation disorder. None of the samples was collected to approximate a nationally representative sample of children, although all studies have employed sampling and weighting strategies to minimize selection bias. Furthermore, results from these representative community samples will likely differ from clinical samples with disruptive mood dysregulation disorder. All studies focused on a three month primary period to minimize recall bias and forgetting.
In these samples, disruptive mood dysregulation disorder was relatively uncommon in childhood and adolescence. By comparison, 3-months rates for depressive disorders were between 2 and 3% and between 2 and 5% for conduct disorder in the older samples (12, 13). This is consistent with the proposed justification for disruptive mood dysregulation disorder which described it as a “severe mood disorder”(1). It was not the case, however, that the primary symptoms were uncommon. It was only when frequency, duration and cross-context criteria were applied that a relatively uncommon phenotype was identified.
The prevalence of disruptive mood dysregulaton disorder in the preschool sample was 2-3-times that observed in the older samples. This is not surprising given the literature identifying early childhood as a peak period for temper tantrums and irritability (see table 2 in (21) for example). Developmental difference are often used to justify amended criteria and we present one example of alternative frequency thresholds for criteria B and C that could attenuate prevalence differences across development.
In the two older samples, application of the onset criterion had only a minimal effect upon the prevalence rates. Furthermore, no justification was provided by the DSM-5 work groups for why this disorder cannot be diagnosed before age 6 (1). This age criterion precludes the diagnosis for preschoolers, yet this study suggests that disruptive mood dysregulation disorder can be diagnosed in such samples and that its comorbidity patterns were generally similar to those observed in older children. The DSM-5 Task forces states that “Only by having consistent diagnoses can researchers compare different treatments for similar patients and, determine the risk factors, and causes for specific disorders, and determine their incidence and prevalence rates” (22). If this is so, then it might be preferable to eliminate this criterion to facilitate the study of severe irritability across development.
A primary concern has been whether the proposed criteria identify a distinct diagnostic entity(8). Comorbidity is common in psychiatry. In a meta-analysis of childhood comorbidity patterns, median odds ratios for comorbidity ranged from 3.0 for ADHD with anxiety to 10.7 for ADHD with conduct disorder(23) and comorbidity rates from individual studies were often much higher, yet these high levels of pairwise associations are not typically considered a threat to the validity of the diagnostic system. The observed comorbidity rates in this study were generally within the range observed for other disorder pairs with the exception of oppositional defiant disorder (odds ratio range 52.9 to 103.0). It was also the case that DMDD did sometime occur alone, particularly in the older samples.
The high levels of co-occurrence with oppositional defiant disorder, however, require further attention and belie proposed attempts to categorize disruptive mood dysregulation disorder as a mood disorder only. We believe that a provisional effort should be made to clarify the nature of this overlap prior to the publication of DSM-5. At the same time, cross-sectional comorbidity is only one consideration and evidence from longitudinal studies (including the Great Smoky Mountains study) has linked severe mood dysregulation with later mood disorders (3–5). This is exactly the same pattern that has been found for the putative behavioral disorder of oppositional defiant disorder (4, 24, 25) which so commonly co-occurs with disruptive mood dysregulation disorder. Both oppositional defiant disorder and disruptive mood dysregulation disorder should be considered disorders with mixed behavioral and emotional features.
This diagnosis does not identify an area of unmet need in the traditional sense of marking children with lower levels of service utilization. For childhood disorders, most studies have found between 35% and 45% of those with a disorder have received treatment (13, 26–28). With disruptive mood dysregulation disorder, three-month service use rates were between 45 and 61%. This does not mean, of course, that the treatment such children receive is either appropriate or even helpful. Concerns about inappropriate or untested interventions are no less a concern than the absence of treatment altogether.
Conclusion
This early look at disruptive mood dysregulation disorder suggests that it meets common standards for psychiatric “caseness” and that this disorder identifies a group of children with severe emotional and behavioral dysregulaton. Its relatively low prevalence and high levels of service utilization moderate worries about “pathologizing” normal behavior, although the core symptoms are common and its rarity comes from strict application of frequency, duration, and cross-context criteria. It is unclear which aspects of its pathophysiology are unique to disruptive mood dysregulation disorder and which are shared with the individual emotional and behavioral disorders with which it so commonly occurs. This should be a priority area of research (see for one (29) example) so that these issues can be resolved well before the advent of DSM-6.
Table 4.
Associations between disruptive mood dysregulation disorder and impairments, service use and sociodemographic variables
| Great Smoky Mountains Study | Caring for Children in the Community | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Criterion | DMDD (%) | No DMDD (%) | OR | 95%CI | p | DMDD (%) | No DMDD (%) | OR | 95%CI | p |
| Impairment | ||||||||||
| Parental relations | 57.3 | 7.0 | 17.2 | 8.2–36.1 | <0.0001 | 64.4 | 11.1 | 12.3 | 5.2–29.2 | <0.0001 |
| Sibling relations | 25.4 | 3.8 | 7.7 | 2.6–22.7 | 0.0002 | 66.2 | 6.8 | 24.3 | 10.7–55.3 | <0.0001 |
| Teacher relations | 16.5 | 2.0 | 8.5 | 2.7–26.8 | 0.0003 | 55.1 | 4.5 | 20.9 | 10.2–42.7 | <0.0001 |
| School suspension | 35.1 | 4.2 | 11.4 | 4.4–30.0 | <0.0001 | 38.3 | 8.6 | 6.0 | 2.8–12.9 | <0.0001 |
| Service use | ||||||||||
| Mental health | 31.5 | 6.0 | 6.5 | 2.6–16.3 | <0.0001 | 39.8 | 4.7 | 13.8 | 4.7–40.5 | <0.0001 |
| General Medical | 8.0 | 3.3 | 2.6 | 1.3–5.1 | 0.006 | 0.0 | 2.4 | -- | -- | -- |
| School System | 26.0 | 7.5 | 4.1 | 1.7–9.7 | 0.002 | 37.5 | 8.7 | 6.8 | 2.2–20.5 | 0.0008 |
| Child Welfare | 15.4 | 1.3 | 13.1 | 3.6–47.9 | 0.0001 | 5.8 | 0.6 | 10.2 | 1.4–75.3 | 0.02 |
| Juvenile Justice | 8.8 | 1.8 | 4.1 | 0.6–27.7 | 0.15 | 28.4 | 1.0 | 16.1 | 4.6–56.5 | <0.0001 |
| Any | 54.2 | 18.0 | 4.5 | 2.1–9.7 | 0.001 | 60.8 | 14.0 | 9.6 | 3.2–28.2 | <0.0001 |
| Sociodemographic | ||||||||||
| Impoverished | 42.9 | 19.0 | 3.0 | 1.3–6.9 | 0.01 | 66.2 | 31.9 | 4.1 | 1.6–10.4 | 0.003 |
| Single parent family | 40.0 | 23.7 | 2.2 | 1.0–4.9 | 0.05 | 26.1 | 14.7 | 2.0 | 0.8–48 | 0.12 |
| Low parent education | 19.4 | 17.3 | 1.3 | 0.5–3.2 | 0.61 | 61.8 | 42.7 | 2.1 | 0.9–4.9 | 0.09 |
DMDD= Disruptive mood dysregulation disorder; Bolded p values are significant at p <0.05.
Acknowledgements
The work presented here was supported by the National Institute of Mental Health (MH080230, MH63970, MH63671, MH48085, MH075766), the National Institute on Drug Abuse (DA/MH11301, DA011301, DA016977, DA011301), NARSAD (Early Career Award to WEC), and the William T Grant Foundation.
Footnotes
Financial Disclosures None of the authors has biomedical financial interests or potential conflicts of interest.
References
- 1.DSM-5 Childhood and Adolescent Disorders Work Group . Justification for Temper Dysregulation Disorder with Dysphoria. American Psychiatric Association; Washington, DC: 2010. [Google Scholar]
- 2.Pogge DL, et al. Diagnosis of manic episodes in adolescent inpatients: structured diagnostic procedures compared to clinical chart diagnoses. Psychiatry Research. 2001;101(1):47–54. doi: 10.1016/s0165-1781(00)00248-1. [DOI] [PubMed] [Google Scholar]
- 3.Leibenluft E, Cohen P, Gorrindo T, Brook JS, Pine DS. Chronic Versus Episodic Irritability in Youth: ACommunity-Based, Longitudinal Study of Clinical and Diagnostic Associations. Journal of Child and Adolescent Psychopharmacology. 2006;16(4):456–466. doi: 10.1089/cap.2006.16.456. [DOI] [PubMed] [Google Scholar]
- 4.Stringaris A, Cohen P, Pine DS, Leibenluft E. Adult Outcomes of Youth Irritability: A 20-Year Prospective Community-Based Study. Am J Psychiatry. 2009;166(9):1048–1054. doi: 10.1176/appi.ajp.2009.08121849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brotman MA, et al. Prevalence, Clinical Correlates, and Longitudinal Course of Severe Mood Dysregulation in Children. Biological Psychiatry. 2006;60(9):991–997. doi: 10.1016/j.biopsych.2006.08.042. [DOI] [PubMed] [Google Scholar]
- 6.Leibenluft E, Charney DS, Towbin KE, Bhangoo RK, Pine DS. Defining clinical phenotypes of juvenile mania. The American journal of psychiatry. 2003;160(3):430–437. doi: 10.1176/appi.ajp.160.3.430. [DOI] [PubMed] [Google Scholar]
- 7.Parens E, Johnston J, Carlson GA. Pediatric Mental Health Care Dysfunction Disorder? New England Journal of Medicine. 2010;362(20):1853–1855. doi: 10.1056/NEJMp1003175. [DOI] [PubMed] [Google Scholar]
- 8.Axelson D, et al. Concerns regarding the inclusion of temper dysregulation disorder with dysphoria in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Journal of Clinical Psychiatry. 2011;72(9):1257–1262. doi: 10.4088/JCP.10com06220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stringaris A. Irritability in children and adolescents: a challenge for DSM-5. European Child & Adolescent Psychiatry. 2011;20(2):61–66. doi: 10.1007/s00787-010-0150-4. [DOI] [PubMed] [Google Scholar]
- 10.Taylor E. Child Psychology and Psychiatry. John Wiley & Sons, Ltd; 2011. Diagnostic Classification: Current Dilemmas and Possible Solutions; pp. 223–228. [Google Scholar]
- 11.Egger HL, et al. The test-retest reliability of the Preschool Age Psychiatric Assessment (PAPA) Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45(5):538–549. doi: 10.1097/01.chi.0000205705.71194.b8. [DOI] [PubMed] [Google Scholar]
- 12.Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- 13.Angold A, et al. Psychiatric disorder, impairment , and service use in rural African American and White youth. Archives of General Psychiatry. 2002;59:893–901. doi: 10.1001/archpsyc.59.10.893. [DOI] [PubMed] [Google Scholar]
- 14.Angold A, et al. The Child and Adolescent Psychiatric Assessment (CAPA) Psychological Medicine. 1995;25:739–753. doi: 10.1017/s003329170003498x. [DOI] [PubMed] [Google Scholar]
- 15.Angold A, Costello E. The Child and Adolescent Psychiatric Assessment (CAPA) Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:39–48. doi: 10.1097/00004583-200001000-00015. [DOI] [PubMed] [Google Scholar]
- 16.Dalaker J, Naifah M. Poverty in the United States: 1997. U.S. Bureau of the Census, Current Population Reports: Consumer Income. 1993:60–201. [Google Scholar]
- 17.Ascher BH, Farmer EMZ, Burns BJ, Angold A. The Child and Adolescent Services Assessment (CASA): Description and psychometrics. Journal of Emotional and Behavioral Disorders. 1996;4:12–20. [Google Scholar]
- 18.Farmer EMZ, Angold A, Burns BJ, Costello EJ. Reliability of self-reported service use: Test-retest consistency of children's responses to the Child and Adolescent Services Assessment (CASA) Journal of Child and Family Studies. 1994;3(3):307–325. [Google Scholar]
- 19.Pickles A, Dunn G, Vazquez-Barquero J. Screening for stratification in two-phase (`two-stage') epidemiological surveys. Statistical Methods in Medical Research. 1995;4(1):73–89. doi: 10.1177/096228029500400106. [DOI] [PubMed] [Google Scholar]
- 20.Tremblay RE, LeMarquand D, Vitaro F. The prevention of oppositional defiant disorder and conduct disorder. In: Quay HC, Hogan AE, editors. Handbook of Disruptive Behavior Disorders. Plenum Publishers; New York: 1999. pp. 525–555. [Google Scholar]
- 21.Egger HL, Angold A. Common emotional and behavioral disorders in preschool children: Presentation, nosology, and epidemiology. Journal of Child Psychiatry and Psychology. 2006;47(3/4):313–337. doi: 10.1111/j.1469-7610.2006.01618.x. [DOI] [PubMed] [Google Scholar]
- 22.DSM-5 Task Force . Frequently asked questions. American Psychiatric Association; Washington, DC: 2010. [Google Scholar]
- 23.Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry. 1999;40:57–87. [PubMed] [Google Scholar]
- 24.Burke JD, Hipwell AE, Loeber R. Dimensions of Oppositional Defiant Disorder as Predictors of Depression and Conduct Disorder in Preadolescent Girls. Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49(5):484–492. doi: 10.1097/00004583-201005000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Copeland WE, Shanahan L, Costello EJ, Angold A. Childhood and Adolescent Psychiatric Disorders as Predictors of Young Adult Disorders. Arch Gen Psychiatry. 2009;66(7):764–772. doi: 10.1001/archgenpsychiatry.2009.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Farmer E, Burns B, Phillips S, Angold A, Costello E. Pathways into and through mental health services for children and adolescents. Psychiatric Services. 2003;54(1):60–66. doi: 10.1176/appi.ps.54.1.60. [DOI] [PubMed] [Google Scholar]
- 27.Costello EJ, Copeland W, Cowell A, Keeler G. Service Costs of Caring for Adolescents With Mental Illness in a Rural Community, 1993–2000. American Journal of Psychiatry. 2007;164(1):36. doi: 10.1176/appi.ajp.2007.164.9.A36. [DOI] [PubMed] [Google Scholar]
- 28.Leaf PJ, et al. Mental health service use in the community and schools: Results from the four-community MECA study. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35(7):889–897. doi: 10.1097/00004583-199607000-00014. [DOI] [PubMed] [Google Scholar]
- 29.Stringaris A, Zavos H, Leibenluft E, Maughan B, Ele T. Adolescent irritability: phenotypic associations and genetic links with depressed mood. American Journal of Psychiatry. 2012;169(1):47–54. doi: 10.1176/appi.ajp.2011.10101549. [DOI] [PMC free article] [PubMed] [Google Scholar]