Figure 1.
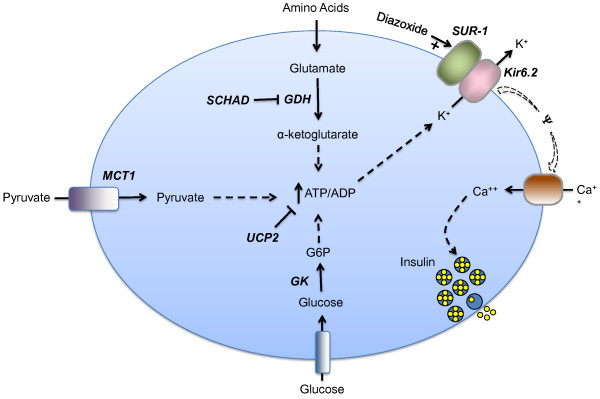
Genetic defects in the beta cell leading to hyperinsulinism. In the pancreatic beta cell, ATP production from fuel metabolism leads to inhibition and closure of ATP-sensitive potassium channels, which triggers membrane depolarization and opening of voltage-dependent calcium channels. The resulting increase in cytosolic calcium triggers insulin secretion. Defects in this pathway can result in hyperinsulinism. The known protein defects are depicted in bold italics. Five are inactivating mutations: SUR-1 (sulfonylurea receptor), Kir6.2 (potassium channel), SCHAD (short-chain 3-OH acyl-CoA dehydrogenase), UCP2 (uncoupling protein 2), HNF-4α (hepatic nuclear transcription factor 4α), and HNF-1α (hepatic nuclear transcription factor 1α). The last 2 are transcription factors and are not depicted in the figure. Three are activating mutations: GK (glucokinase), GDH (glutamate dehydrogenase), MCT-1 (monocarboxylate transporter 1). Positive effects are shown by a plus arrow; negative effects by a minus arrow. Dashed arrows denote multiple steps in a pathway. G6P = glucose-6-phosphate, ATP = adenosine triphosphate, ADP = adenosine diphosphate.
