Abstract
Therapist perspectives regarding delivery of evidence-based practice (EBP) strategies are needed to understand the feasibility of implementation in routine service settings. This qualitative study examined the perspectives of 13 therapists receiving training and delivering a package of EBPs to children with autism spectrum disorders (ASD) in community mental health clinics. Therapists perceived the training and intervention delivery as effective at improving their clinical skills, the psychotherapy process, and child and family outcomes. Results expand parent pilot study findings, and add to the literature on training community providers and limited research on training providers to deliver EBPs to children with ASD.
Keywords: therapist perspectives, evidence-based practice, autism spectrum disorders, community mental health clinics, challenging behaviors
Community mental health (CMH) providers’ perspectives of evidence-based practice (EBP) strategies are an important contextual factor influencing the use of EBPs in CMH settings (Aarons, 2004; Aarons, Hurlburt, & Horwitz, 2011; Baumann, Kolko, Collins, & Herschell, 2006; Garland, Hurlburt, & Hawley, 2006). However, studies examining CMH providers’ perspectives of EBPs, generally, and EBP manuals in particular, have yield mixed results (Aarons, 2004; Addis & Krasnow, 2000; Baumann et al., 2006; Essock, Goldman, Van Tosh, Anthony, Appell, Bond et al., 2003; Sheehan, Walrath, & Holden, 2007). Although many CMH providers indicate that they use research to inform their practice (Addis & Krasnow, 2000; Kazdin, Siegel, & Bass, 1990; Stewart & Chambless, 2007), many report negative attitudes toward EBPs and manualized approaches. Specifically, CMH providers cite restriction of clinical skills and autonomy, limited flexibility, and a lack of “fit” with the complex and diverse community patient samples who they serve as reasons for their negative perspectives (Addis & Krasnow, 2000; Baumann et al., 2006; Essock et al., 2003; Nelson, Steele, & Mize, 2006). CMH providers’ perceptions of the value of EBPs have been found to predict their use of EBPs (Casper, 2007). Given these, often negative, perspectives of EBPs, it is not surprising that evidence-based treatment strategies have been found to be used with relatively low intensity (Garland, Brookman-Frazee, Hurlburt, Accurso, Zoffness, Haine-Schlagel et al., 2010), and that delivery of EBPs in CMH service settings is challenging.
In addition to the growing literature regarding provider perspectives on EBPs in CMH service settings generally, there has been a small body of research examining CMH therapist perspectives of serving specific populations in CMH service settings. For example, there has been increased recognition of the importance of examining routine care provided to children with autism spectrum disorders (ASD) (Brookman-Frazee, Taylor, & Garland, 2010b; Brookman-Frazee, Drahota, Stadnick, & Palinkas, 2012b). These children represent a growing population with complex clinical needs (Brookman-Frazee, Baker-Ericzen, Stahmer, Mandell, Haine, & Hough, 2009a). The Centers for Disease Control and Prevention (CDC) estimate that approximately one in 88 children have an ASD (CDC, 2012), which are a set of neurobiologically-based disorders characterized by social and communicative difficulties, and exhibition of restricted, stereotyped patterns of behavior or interests (American Psychiatric Association, 2000). The CMH system plays a particularly important role in caring for school-age children with ASD for treatment of behavioral and co-occurring psychiatric problems associated with ASD. Children with ASD represent approximately 10–14% of children in psychiatrically referred populations (Joshi, Petty, Wozniak, Henin, Fried, Galdo, et al., 2010; Sverd, Dubey, Schweitzer, & Ninan, 2003) and an average of 21% of CMH therapists’ caseloads (Brookman-Frazee et al., 2012b).
Research on the characteristics of children with ASD in CMH settings indicates that these youth typically have milder forms of ASD (i.e., pervasive developmental disorder-not otherwise specified [PDD-NOS] or Asperger’s Disorder rather than Autistic Disorder), and have a significantly greater number of co-occurring non-ASD disorders compared to youth with non-ASD diagnoses (Joshi et al., 2010). Further, the primary presenting problem for children with ASD in CMH clinics, regardless of co-occurring psychiatric disorders, is challenging behaviors (Brookman-Frazee, Baker-Ericzen, Stadnick, & Taylor, 2011; Brookman-Frazee et al., 2012b; Mandell, Walrath, Manteuffel, Sgro, & Pinto-Martin, 2005). This is not surprising given the high prevalence of co-occurring challenging behaviors for children with ASD (Matson, Wilkins, & Macken, 2009; Matson, Mahan, Hess, Fodstad, & Neal, 2010) and the association between challenging behaviors and presentation of other psychiatric conditions (Wood & Gadow, 2010; Kim, Szatmari, Bryson Streiner & Wilson, 2000). Due to the clinical complexity of children with ASD, the common occurrence of challenging behaviors associated with an ASD diagnosis, and data suggesting that CMH clinics serve many children with ASD, ensuring that the CMH system is equipped to provide effective EBP care for this population is of particular importance.
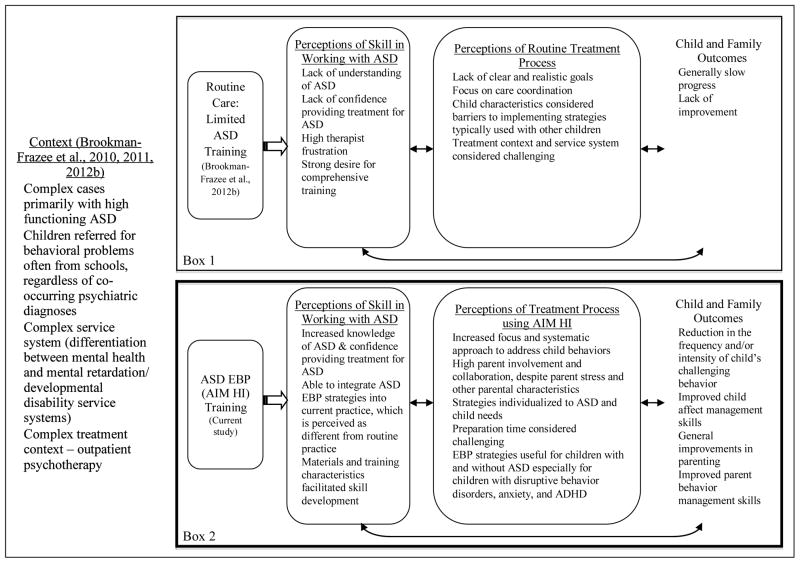
Unfortunately, research examining routine CMH care suggests that there are gaps between EBPs and CMH services (Brookman-Frazee et al., 2010b) for children with ASD. One reason is that therapists in CMH clinics are typically generalists (i.e., not specializing in treatment of a particular mental health or developmental disorder) and have insufficient specialized knowledge about ASD to effectively treat this population, particularly those who present with challenging behaviors (Brookman-Frazee et al., 2011, 2012b). Data from a recent mixed-methods study examined the perspectives of 100 CMH therapists regarding their experiences providing routine care to school age children with ASD. Themes related to therapists’ experiences providing care to children with ASD are summarized in Box 1 of Figure 1. Specifically, these CMH therapists reported that they have limited training in ASD, lack an understanding of ASD and confidence providing treatment to children with ASD, and are highly frustrated serving this population (Brookman-Frazee et al., 2012b). Therapists described the therapy process as challenging due to lack of clear and realistic treatment goals, child characteristics (e.g., complex clinical presentation) that were perceived as barriers to implementing typical treatment strategies, considerable time spent on care coordination, and the constraints of the CMH setting itself (e.g., competing time demands, limited therapeutic time). Further, therapists described the slow rate of child progress and lack of improvement. Despite this, CMH therapists reported that they had a strong desire for comprehensive training to better serve the children with ASD on their caseload. These data underscore the need for understanding the training needs of CMH therapists and how to tailor interventions to suit the CMH context in order to improve care for children with ASD.
Figure 1.
Integrating themes about therapist perspectives on serving children with ASD.
Implementing existing EBPs for ASD (Lord & Bishop, 2010; National Standards Report, 2009) in CMH clinics can facilitate efforts to improve care. Although there is empirical support for child skills training and parent-mediated interventions based on principles of applied behavior analysis and cognitive behavioral therapy methods, EBP strategies for challenging behaviors in children with ASD are typically “focal intervention practices” (Lord & Bishop, 2010). These practices are not packaged as comprehensive protocols readily adopted for use in mental health clinics because they likely do not meet the complex clinical needs of school-age children with ASD receiving treatment in CMH settings (Brookman-Frazee et al., 2010b). Additionally, existing treatment protocols and training models were not designed for delivery within CMH clinics (i.e., providers with limited ASD experience, traditional one hour per week model). Thus, CMH therapists have few options for selecting readily “implementable” EBPs to treat children with ASD.
To address this lack of readily “implementable” EBPs for children with ASD presenting with challenging behaviors in CMH settings, An Individualized Mental Health Intervention for Children with ASD (AIM HI) (Brookman-Frazee & Drahota, 2010a) was developed. AIM HI is a package of parent-mediated and child-focused EBP strategies, based on the principles of applied behavior analysis, designed to reduce challenging behaviors in children with ASD ages five to 13 served in CMH settings. The AIM HI clinical intervention protocol and corresponding therapist training model were developed through a research-community partnership approach in which community stakeholders (organizational leaders, clinicians, and parents) partnered with ASD intervention experts to integrate findings from a comprehensive mixed-methods needs assessment (Brookman-Frazee et al., 2011, 2012b) and existing EBP strategies for this population (National Standards Report, 2009). AIM HI was developed based on the clinical needs of children with ASD and the training needs of the therapists who serve them in CMH settings (see Box 1 of Figure 1). The individual components of AIM HI (e.g., functional behavior assessment, use of antecedent and consequence-based strategies, skill modeling, direct skill practice with feedback, environmental modifications for ASD) are classified as “well established” by the National Autism Center’s National Standards Project (National Standards Report, 2009) and the National Professional Development Center on ASD (Odom, Collet-Klingenberg, Rogers, & Hatton, 2010) based on independent rigorous scientific merit reviews.
Additionally, quantitative data from a recent pilot study (Brookman-Frazee, Drahota, & Stadnick, 2012a) support the feasibility of training therapists to deliver AIM HI in CMH clinics. Specifically, therapists participated in ongoing AIM HI training, were able to deliver the intervention with fidelity, and perceived the intervention as useful. Meaningful reductions in child challenging behaviors occurred over five months of AIM HI delivery, providing promising support for the implementation of the AIM HI intervention in CMH settings. Further, mixed methods data collected from primary caregiver participants who received AIM HI with their child support the acceptability of AIM HI as an intervention for children with ASD and their families (Stadnick, Drahota, & Brookman-Frazee, 2012).
As AIM HI was developed very differently than other EBP protocols through ongoing CMH therapist feedback and needs assessment, CMH therapists’ perspectives toward AIM HI may be more favorable than their perspectives towards other EBPs and manualized interventions. Therefore, the purposes of the current qualitative study are to build on previous qualitative research examining therapist perspectives of routine care for children with ASD (Brookman-Frazee et al., 2012b), and complement and expand the quantitative outcomes data collected from the larger pilot study of AIM HI, which focused on the feasibility of AIM HI in this context, therapists’ fidelity to the intervention manual, and child- and parent-related outcomes (Brookman-Frazee et al., 2012a). For the current study, qualitative methods were used to gather in-depth information on the perspectives of therapists regarding their experiences receiving training in and delivering AIM HI to child clients with ASD in CMH clinics.
Methods
Design
Data for the current study were drawn from a broader pilot study of the AIM HI clinical intervention and corresponding therapist training protocol. To date, the primary results of this pilot study including quantitative data on the feasibility, acceptance, and fidelity of CMH therapists’ use of AIM HI, preliminary child and family outcomes (Brookman-Frazee et al., 2012a), and qualitative data on parent perspective of the intervention (Stadnick et al., 2012) have been reported. The current study further extends this research by using qualitative methods to examine the perspectives of CMH therapists who participated in the pilot study.
In order to capture the richness and potential diversity of therapists’ perceptions about their experiences with the AIM HI training and delivery, the current study used qualitative interviews coded for emergent themes using a coding, consensus, and comparison methodology (Willms et al., 1990), described below. Qualitative interviews with pilot study therapists occurred after they were trained and delivered the AIM HI intervention to a child and caregiver over five months. Qualitative methods, such as the individual interviews used in the current study, are particularly appropriate for gathering participants’ in-depth, subjective experiences (Marshall & Rossman, 2006).
Participants
Participants in the current qualitative study included all 13 therapists who participated in the AIM HI pilot study. Note that this sample size is considered sufficient to reach theoretical saturation in qualitative studies of this nature (Guest, Bunce, & Johnson, 2006). The therapist/family dyads participating in the pilot study were from three CMH clinics within one organization in a large, geographically diverse county within California. This organization is the largest contractor for publicly funded, clinic-based outpatient care for children in one of the most populated counties in the United States. These clinics serve racially/ethnically and diagnostically diverse children and their families. None of the clinics specialized in treatment of children with ASD or in EBPs for other disorders before or during the study period.
AIM HI pilot study therapist participants
During August to September 2009, all therapists from the three participating clinics were recruited through weekly treatment team/supervision meetings. Of the 74 therapists present during the recruitment meetings, 76% (n = 56) agreed to be contacted about the study. Therapists were eligible if she/he: (a) was employed as staff or a trainee at one of the participating clinics; (b) was employed at that clinic for at least the next nine months; and (c) had an eligible client on their current caseload (see client inclusion criteria below) who, with their parent/caregiver was willing to participate in the AIM HI pilot study. Pilot study therapists received an honorarium ($100) for agreeing to participate in the study. Fourteen therapists who met the eligibility criteria by the end of October 2009 were initially enrolled. One therapist was excluded because she was unable to participate in ongoing AIM HI training due to scheduling conflicts.
The final 13 pilot study therapist participants included in the study were primarily female (85%; n = 11), and 46% (n = 6) were Caucasian. The range of years of experience at baseline ranged from less than 1 year to 11 years (M = 3.75 years). Consistent with national samples of therapists in CMH care (e.g., Glisson, Landsverk, Schoenwald, Kelleher, Hoagwood, Mayberg et al., 2008) and larger studies in the same service system (Brookman-Frazee, Garland, Taylor, & Zoffness, 2009b), therapists were primarily master’s level clinicians (77%), with 23% at the Bachelors level (currently in graduate training), and 77% were considered trainees. Therapists came from different mental health disciplines: Marriage and Family Therapy (39%), Psychology (39%), and Social Work (23%). Therapist’s self-reported primary theoretical orientation included: Cognitive-behavioral (31%), Behavioral (15%), Family Systems (15%), Eclectic (15%), and Humanistic/Psychodynamic (8%). Consistent with previous research in these settings, children with ASD represented 24% of therapists’ current caseloads (range: 8–50%).
AIM HI pilot study child/family participants
Pilot study therapist recruitment was linked to family recruitment. Inclusion criteria for pilot study child/family participants were: (a) child aged between five and 13 years at the time of recruitment, (b) had an existing ASD diagnosis on record, (c) met criteria for autism or ASD on the Autism Diagnostic Observation Schedule (ADOS), (c) used phrase speech, (d) spoke English, (e) had received treatment with the participant therapist for less than one year prior to study participation, and (f) caregiver consented to regularly attending therapy sessions with the child (at least one time per month).
The 13 participating pilot study children were aged five to 13 years (M = 10.3, SD = 2.3), 100% were male, and 77% were Caucasian, 15% Latino, and 8% Mixed. These data are generally consistent with the literature on the population of children with ASD seen in mental health settings (Brookman-Frazee et al., 2010b; Joshi et al., 2010). Clinician-reported ASD diagnoses were: 46% Asperger’s Disorder, 39% PDD-NOS, and 15% Autistic Disorder. A majority of children (69%) also had a non-ASD co-occurring psychiatric diagnosis, according to clinician report: 39% ADHD, 23% Anxiety Disorder, 15% Disruptive Behavior Disorder, and 8% Mood Disorder. Mental health care for the majority of families was funded through the school system (85%). The remaining families were funded through government (i.e., Medicaid) sources (15%).
Procedure
Pilot study procedures relevant to the current study are described below. Additional details are provided in Brookman-Frazee and colleagues (2012a).
AIM HI clinical intervention
AIM HI is a package of evidence-based parent-mediated and child focused strategies, based on the principles of applied behavior analysis, designed to reduce challenging behaviors in children with ASD ages five to 13 served in CMH clinics. AIM HI involves a series of 10 steps (8 required, 2 as indicated) and within-session elements aimed at teaching parents of children with ASD to manage challenging behaviors (e.g., aggression, socially inappropriate behaviors) and teach children positive alternative skills (e.g., self-regulation, social skills) using EBPs. The specific AIM HI protocol steps are described in Brookman-Frazee and colleagues (2012a). During treatment, the therapist actively collaborates with the parent(s) and child to identify external functions and patterns of challenging behaviors, develop a treatment plan, and identify/teach functionally-equivalent positive alternative behaviors to the child. Sessions are structured to maximize engagement with parent and child, and active parent and child skill-building. AIM HI was designed to be flexibly implemented in the context of CMH clinics by therapists with limited experience with ASD. A minimum of 13 sessions is required to complete the AIM HI protocol; however, the protocol can be repeated as necessary for a specific child as is clinically indicated.
AIM HI therapist training
The multi-component therapist training approach used during the pilot study included: (a) an interactive introductory workshop, (b) self-study using web-based and printed materials, and (c) ongoing supervisory consultation, practice, and feedback on delivery with an actual family dyad. Specifically, after therapist/family dyads were recruited, therapists received initial training through an introductory workshop and self-study (web-based and printed) materials. AIM HI developers facilitated the one-day (6-hour) workshop. The workshop included didactic lectures, video exemplars, discussion, and interactive practice opportunities. All licensed therapists received continuing education course credit for workshop attendance.
After the initial workshop, participant therapists delivered AIM HI for approximately five months with participating families while receiving consultation twice per month with the AIM HI developers. Therapists started at the treatment planning stage of the intervention, regardless of whether the child was a new client or a client continuing with his or her therapist. During the 10, one-hour consultation meetings, AIM HI steps were reviewed in detail and feedback (based on video-tape review and therapist questions) was provided about therapists’ practice with participating families.
Therapist interviews
At the end of five months, all pilot study therapists participated in a one-time semi-structured individual interview. Interviews were conducted in person and lasted an average of approximately 30 minutes (M = 31.46).
Measures
Semi-structured therapist interview
A trained member of the research team who was not involved in the AIM HI therapist training conducted all semi-structured interviews. Only therapists participating in the AIM HI pilot study were interviewed; therefore, it was not possible for the interviewer to be blinded. Questions were divided into five primary sections. The first section included a set of questions that asked about the most useful and challenging aspects of delivering AIM HI. The second section included a set of questions inquiring about therapists’ perceptions of the most useful and challenging aspects of the AIM HI training model (i.e., the introductory workshop and ongoing consultation meetings). The third section included a set of questions regarding therapists’ perceptions of the impact of AIM HI on their client (e.g., changes in child behavior problems) and client’s parent(s) (e.g., stress, parenting skills). The fourth section included questions inquiring about therapists’ perceptions of the impact of AIM HI on their practice as a therapist (e.g., how delivering AIM HI was different than their usual practice with other children and specifically those with ASD). The final section provided therapists with an opportunity to share any changes they would recommend for the AIM HI training model and clinical intervention to improve its utility.
Data Analysis
These qualitative data were analyzed using a coding, consensus, and comparison methodology (Willms et al., 1990), which followed an iterative approach rooted in grounded theory (Glaser & Strauss, 1967). Specifically, all interviews were first transcribed. Following this, three interviews (23%) were randomly selected and examined independently by two members of the research team to elicit emergent themes (i.e., themes surfacing from the interview text) within the interviews. Emergent themes were identified and assigned a code by considering the frequency of and salience with which (i.e., importance or emphasis) a therapist discussed it. Segments of the texts, ranging from sentences to paragraphs, were assigned specific codes that enabled members of the research team to consolidate interview data into analyzable units. Following this, each interview was independently coded by the same two members of the research team and then collectively reviewed with the principal investigator to identify and reconcile discrepancies. A review of all of the codes for each interview was conducted until members of the research team reached consensus as to which codes should be applied to specific segments of text. After consensus was achieved among coders, interview transcripts were then entered, coded, and analyzed in QSR-NVivo 2.0, a program frequently used in qualitative research (Tappe, 2002).
To further contextualize therapists’ perspectives and understand the utility of the AIM HI training and intervention protocol, themes identified in the current study were compared to themes related to the perspectives of CMH therapists working with children with ASD during a separate mixed-methods needs assessment study, which occurred in the same service setting prior to the development of AIM HI (Brookman-Frazee et al., 2012b) (see Box 1 of Figure 1). As described in Brookman-Frazee et al. (2012b), 100 therapists, serving publicly funded children and adolescents, including youth with ASD, completed questionnaires as part of the mixed-methods needs assessment study. Following collection of questionnaires, therapists were recruited via flier and presentations at staff meetings to participate in subsequent focus groups. A subset of 17 CMH therapists participated in focus groups that discussed the format and content of a training related to serving children with ASD, in preparation for development of AIM HI. For details about the mixed-methods needs assessment study, see Brookman-Frazee et al. (2012b). Despite differences in sample size and data collection methods, CMH therapists in the mixed-methods needs assessment study had similar backgrounds and worked in the same service setting as therapist participants in the AIM HI pilot (and current) study. Additionally, similar methods were used to analyze the qualitative focus group data. Given these methodological similarities, themes from this prior therapist mixed-methods study are considered a representation of therapists’ experience providing routine care in CMH settings for families of children with ASD, and were used as a basis for comparison in the current study. The final themes from the current study are described below.
Results
The following are the primary themes that emerged from the pilot study therapist interviews. Descriptions of themes are accompanied by illustrative quotes from interviews. To further contextualize the themes from the current study, results were compared to those highlighted in a recent mixed-methods study examining therapist perspectives of routine CMH care for ASD described in the Introduction and summarized in Box 1 of Figure 1 (Brookman-Frazee et al., 2012b). Themes are synthesized in Figure 1 and integrated in the Discussion.
Perceptions of Skill Working with ASD
Overall, therapists in the current study reported that the AIM HI training (including the workshop and ongoing consultations) provided during the AIM HI pilot study resulted in meaningful increases in their skills to work with children with ASD in CMH settings. Specific areas of skill development are described below.
Increased knowledge and confidence with ASD
Therapists stated that their knowledge of ASD characteristics and symptoms increased as a direct result of participating in the AIM HI training. As one therapist stated, “I really liked the training because I didn’t know, really, anything about treating kids with ASD before I went into it.” Another stated, “The way [the training] impacted me most is kind of my thinking about …the spectrum, was there’s a lot more to the behaviors…it made me be more open as a therapist and ask more questions.” Therapists also described increased confidence in providing treatment to children with ASD and their families. As one therapist stated, “I feel like it’s given me a very good language to understand and break down what is going on with my patients and to structure things and a way for me to get the family involved and explain to them why they should be involved and, yeah, it’s changed [the] model of how I’m working with the kids.”
Ability to integrate ASD EBPs into current practice, which is perceived as different from routine practice
Therapists reported that the AIM HI training contributed to their ability to integrate ASD EBP approaches (e.g., structured skill-building) into their current practice, which were distinctly different from their practice prior to AIM HI. One therapist explained, “It definitely helped to structure the sessions knowing that I had a specific skill that I was targeting that session. …I feel like with some of my others clients when we have an overall treatment plan it gets kind of jumbled and I end up putting out like little fires instead of looking at the big picture and what’s going to be really helpful overall. …If we don’t have a specific skill that we’re targeting that session, I feel it’s more chaotic rather than structured.”
Facilitators of skill development
Therapists highlighted a number of facilitators to their skill development including the user-friendly materials, individualized performance feedback, and characteristics of the trainers. Specifically, therapists reported that the AIM HI therapist manual and treatment forms (especially the behavior tracking, behavior plan, and session summaries) were useful in learning the intervention protocol. One therapist described the most useful aspects of the intervention: “I think the most useful was actually the whole manual… I like how there were examples to fill out the worksheets… And I think it was really easy to read and pretty friendly language…each form kind of built on the one before it so you have your behavior tracking and then it seemed like everything built on top of that and it all connected.”
Therapists also indicated that the opportunity to receive personalized feedback about their use of AIM HI with their clients during the consultation meetings facilitated their skill development. One therapist explained: “The consultation meetings were great. It was just nice to get feedback about how my patient’s doing, how I’m adopting the model and just to sit with somebody as I’m going along the process…and have somebody with that perspective who knows what they’re doing kind of guiding me through the process.”
Lastly, therapists reported that characteristics of the leaders facilitating the training, such as knowledge about ASD and using EBPs to work with these children, and their accessibility facilitated therapists’ skill development. As one therapist commented, “…everybody was great and very accommodating, really personable and knowledgeable… and they always were prompt in answering questions. If I would email them stuff, they were right on it.”
Perceptions of Treatment Process using AIM HI
Increased focus and systematic approach to address child behaviors
Therapists reported several changes to their treatment process while using AIM HI. In particular, AIM HI pilot study therapists perceived an increased focus and systematic approach to address child behaviors as particularly useful. As one therapist described: “The most useful component was the way that it really forces you to stay on track and target a specific behavior, and so it really allowed me to emphasize when other things came up that kind of gave me an additional permission to really keep the family focused on that one thing in order for them to see the progress and for us to track everything… There was a cohesiveness there that I think was lacking for this particular family and me.”
High parent involvement and collaboration, despite parent stress and other parental characteristics
Therapists reported a high degree of parental involvement and collaboration. Therapists reported that they were able to implement AIM HI despite parental stress and/or, for some parents, parental mental illness and cognitive limitations. While these parental characteristics caused some additional consideration and challenge for some therapists, therapists felt that they were able to implement AIM HI effectively.
Strategies individualized to ASD and child needs
Therapists noted that AIM HI protocol was flexible enough to individualize strategies to meet the unique therapeutic needs of their clients. For example, one therapist indicated that individualizing the amount of time that she spent focusing on teaching a specific skill to her child client was useful. She explained, “…and the other thing I discovered, that it is okay to … repeat and repeat and repeat… Now we’re moving… first we taught him how to do it and mom was prompting him. Then we move on to mom less prompts and more like little reminders. Then we moved to less of all that and him reminding himself. Then we move into him telling himself he did a good job until everything becomes automatic.” Another therapist described how she linked her clinic-based therapy with her client’s school program: “…he’s being funded by the school so a lot of the stuff we’ve got to focus on the school...I observed in the classroom and taught the teacher’s aide how to do some of this stuff, too, the emotion regulation stuff…It seemed like his family and even his teacher both kind of facilitated using the intervention… A lot of it overlapped with, you know, his goals anyway, his IEP goals, so it makes sense to be consistent.”
Preparation time considered challenge
When asked about specific challenges to learning and delivering AIM HI, therapists indicated that it was challenging to carve out time for preparation to deliver AIM HI, given the CMH context and productivity requirements. As one therapist explained, “And then right when it really got into the meat of it was when I had 15 clients and started school back up, and then we had to do [new billing system]…That’s just life.” It is important to note that, although the time was challenging, therapists indicated that they viewed AIM HI favorably.
EBP strategies considered useful for children with and without ASD
Therapists indicated that they perceived AIM HI as useful for children with and without ASD, especially for children with disruptive behavior problems, anxiety, and ADHD. In fact, AIM HI pilot study therapists stated that they will use or had already incorporated concepts and strategies from AIM HI into their therapy approach with other clients presenting with similar symptoms and conditions. As one therapist described, “Well, it’s definitely helped here because I deal with a lot of kids who [have] externalizing behaviors where behavior interventions are really relevant. And so it’s given me a framework…just a place to start, and kind of a progression of interventions that I appreciate.” Another therapist shared how she was applying AIM HI strategies with other clients: “I’ve used the behavior tracking because it just, it makes sense to see the antecedents and the consequences so it just gave me those ideas of how to work with kids who present similar problems, not maybe not the same diagnoses but similar problems.”
Child and Family Outcomes
Reduction in the frequency and/or intensity of child’s challenging behavior
Therapists indicated that AIM HI resulted in a positive impact on child behaviors. Specifically, therapists reported a reduction in the frequency and/or intensity of their client’s challenging behavior over the five months of AIM HI delivery. One therapist explained, “Well, he definitely has improved goal-wise… definitely has decreased his aggressive behaviors at school, he’s more flexible because we worked a lot on flexibility.”
Improved child affect management skills
Therapists also reported an increase in children’s affect management skills as a positive outcome of their use of AIM HI. For example, Therapists reported that their clients were able to better regulate their emotions, which then positively impacted their behavior and relationships. As one therapist commented, “There was a time period where he had to travel. …to hear that he had been so flexible in the change of routine and he kind of just went with the flow and that was so different than what he came in with… targeting [coping, emotion regulation] specifically really helped. I think it had a really good impact on his behavior.”
General improvements in parenting
Therapists described general positive impacts on parents such as, increased patience, supporting child autonomy, and greater parenting self-confidence. One therapist explained that the parent “seems more confident and …more capable to handle him and knows what to do in different situations, whereas before it was kind of like she tried some things but she did not know if it would be effective or not.”
Improved parent management skills
In addition to the general improvements in parenting skills, therapists reported that parents made specific improvements in use of behavior management strategies with their children. For example, some therapists described specific strategies parents were using after receiving AIM HI (e.g., visual schedules, in vivo exposures). One therapist reported, “[The parents] have made a lot of changes. They’ve started using a schedule of events on the weekends, which I think is helpful for the client to know what to expect ahead of time, and that goes into their increased knowledge of the disorder because at first, they were hesitant to buy into that. So they seem to be more… helpful with emotional expression. So they have helped him label it if he can’t verbalize it. They prompt him to use coping skills.”
Discussion
The current study used qualitative methods to examine CMH therapists’ perspectives on the training, delivery and outcomes of AIM HI, a package of EBPs to address challenging behaviors in school-age children with ASD. The current study expands upon the quantitative AIM HI pilot study (Brookman-Frazee et al., 2012a) by examining therapists’ unique perspectives on the skills they gained through the AIM HI training, the treatment process using AIM HI, and child and family outcomes. Therapists participated in both the initial and ongoing AIM HI training, were able to deliver the intervention with fidelity, and perceived the intervention as useful. Additionally, therapists reported increased parental participation in their children’s mental health, and meaningful reductions in children’s problem behaviors (Brookman-Frazee et al., 2012a). These data, in combination with the quantitative data from the parent pilot study, provide initial support for the feasibility and acceptability of the AIM HI intervention protocol and training model for use by therapists in CMH service settings. Furthermore, the current study complements the data collected from parents whose child received AIM HI during the pilot study (Stadnick et al., 2012). Specifically, parents perceived a strong therapeutic alliance with their child’s therapist, perceived a difference from previous therapy once therapists began delivering AIM HI, and reported positive child and parent outcomes as a result of AIM HI. Additionally, these qualitative data provide a comparison, expand, and complement previous research focusing on MH services delivered to children with ASD in CMH settings. The current study provides an approximate comparison to therapists’ perspectives of the care delivered to children with ASD in the same CMH setting prior to the development and implementation of AIM HI (Figure 1) (Brookman-Frazee et al., 2012a).
Community Mental Health Service Setting
As can be seen in Figure 1, the service context in which CMH therapists work was the same for routine care as it was for delivering AIM HI (Brookman-Frazee et al., 2010b, 2011, 2012b). Briefly, children with ASD in this CMH setting presented with complex clinical profiles (e.g., had co-occurring non-ASD psychiatric disorders, such as anxiety disorders), were most frequently categorized as having “high functioning ASD” or PDD-NOS, and were most commonly referred by the school system for behavioral problems. Additionally, the CMH setting itself was complex. Therapists in this setting were generalists in practice – not specializing in the treatment of children with ASD or in specific EBPs.
Therapists Perceptions of Delivering MH Services to Children with ASD
Set within this context, Figure 1 displays an approximate comparison between CMH therapists’ perceptions when delivering routine care (Box 1) versus care when AIM HI was delivered (Box 2). These components are conceptualized as bidirectional, wherein each component influences the others. Differences can be seen between CMH therapists reported perceptions of their skills in working with children with ASD when delivering routine care versus AIM HI. Overall, therapists delivering routine care prior to the development of AIM HI reported negative perceptions of their skill, the routine treatment process, and child and family outcomes (Brookman-Frazee et al., 2012b) (Figure 1, Box 1). Therapists who received AIM HI training and delivered AIM HI reported increased clinical skill in providing ASD EBPs to children with ASD presenting with challenging behaviors, overall positive impressions of the treatment process using AIM HI, and improved child and family outcomes related to the delivery of AIM HI (Figure 1, Box 2).
Specifically, responses from therapists providing routine care to children with ASD indicate that therapists experience a high level of frustration in working with children with ASD, and have a need for additional training in serving children with ASD. In contrast, therapists delivering AIM HI perceived an increase in their knowledge of ASD and confidence in providing treatment to school-age children with ASD and behavior problems related to the AIM HI training and consultation meetings. These perceptions support the quantitative AIM HI pilot study findings wherein AIM HI pilot study therapists reported statistically and clinically significant (Cohen’s d = 1.8) increases in perceived knowledge and confidence related to working with children with ASD from baseline to 5 months of AIM HI training (Brookman-Frazee et al., 2012a). CMH therapists delivering routine care reported lacking an understanding of ASD and the confidence to provide treatment to children with ASD (Brookman-Frazee et al., 2012b). Additionally, CMH therapists who received AIM HI training reported that they were able to integrate ASD EBP strategies into their current practice, which they perceived to be different from their routine practice. This perception was supported by observed fidelity measures included in the AIM HI pilot study (Brookman-Frazee et al., 2012a). Specifically, all 13 AIM HI pilot study therapists reached fidelity in delivering AIM HI. Moreover, therapists delivering AIM HI did not report a need for any additional training related to treating children with ASD in the current study.
Regarding impressions of the therapy process, therapists delivering routine care reported a lack of clear and realistic goals, identified several barriers to implementing EBP strategies and reported other challenges that limited the delivery of EBP strategies. At the conclusion of the AIM HI training and consultation, AIM HI pilot study therapists reported an increase in the focus and intensity of using EBPs. That is, pilot study therapists reported a more focused and systematic approach to treating children with ASD, increased parental involvement and collaboration despite varied parental characteristics, and flexibility to individualize EBPs to meet child needs. While pilot study therapists noted that preparation time was a challenge, data from the larger pilot study of AIM HI indicated that therapists delivered the AIM HI intervention with high intervention fidelity despite perceived time challenges (Brookman-Frazee et al., 2012a). Finally, therapists delivering AIM HI perceived it to be useful for children with and without ASD, particularly children with behavior disorders, anxiety and ADHD. Therapists providing routine care to children with ASD indicated that the characteristics of children with ASD created barriers to implementing strategies that they typically used with other children, resulting in a focus on care coordination during treatment sessions. It is promising that CMH therapists delivering AIM HI reported willingness and ability to generalize the AIM HI intervention to children without ASD. The acceptance of AIM HI for use with children without ASD provides support for the acceptability and feasibility of AIM HI within CMH settings.
Lastly, therapists providing routine care reported generally slow progress and a lack of improvement in the problem behaviors of children with ASD (Brookman-Frazee et al., 2012b). AIM HI pilot study therapists’ perceived child and family outcomes to be improved after delivering AIM HI. Therapists delivering AIM HI reported a reduction in the frequency and/or intensity of children’s challenging behaviors and an increase in adaptive, alternative behaviors such as affect management skills use. Further, therapists were able to provide specific examples of improved child behavior when interviewed. Therapists’ impressions of improved child behavior after delivering AIM HI was supported by clinical outcomes reported in Brookman-Frazee and colleagues (2012a), in which meaningful reductions in child challenging behaviors were observed based on standardized measures. In addition to improved child behavior, therapists perceived parental improvements as well. For example, therapists reported general improvements in parenting skills as well as improved parent behavior management skills.
AIM HI and EBP Delivery Within Community Mental Health Settings
Results of the current qualitative study are consistent with recent studies examining therapists’ perspectives of specific EBP strategies (Brookman-Frazee et al., 2009b; Nakamura, Higa-McMillan, Okamura, & Shimabukuro, 2011), and extend the current literature on therapists’ perspectives on use of EBP strategies in CMH settings, particularly for therapists providing services to children with ASD and their families. While the general literature report negative CMH provider attitudes toward EBPs and manualized approaches (Addis & Krasnow, 2000; Baumann et al., 2006; Essock et al., 2003; Nelson et al., 2006), therapists delivering AIM HI perceived the intervention and training model positively. Given the increased number of children with ASD on CMH therapists’ caseloads (Joshi et al., 2010; Sverd et al., 2003; Brookman-Frazee et al., 2012b), it is important that CMH therapists have an intervention that is perceived to be acceptable, effective and feasible for the service setting.
The AIM HI intervention and training model may have been viewed more positively than other EBP strategies or interventions (or EBPs in general) likely because they met the needs expressed by CMH therapists for a comprehensive training in ASD and effective strategies that can be feasibly delivered within the context of the CMH service setting (Brookman-Frazee et al., 2012a,b). Additionally, the development of the AIM HI intervention and training model were developed with the CMH service setting in mind, which may have increased the acceptability and feasibility of the intervention (Dingfelder & Mandell, 2011). Further, positive perceptions of AIM HI may have resulted from the comprehensive training model that included an introductory workshop with ongoing training through consultation meetings, online materials, feedback and coaching while therapists delivered AIM HI to a training case. These training components have been found in other recent studies involving training CMH therapists in EBPs to increase therapist skill acquisition and mastery, and likely contribute to changes in CMH therapists’ treatment approaches (Herschell, Kolko, Baumann, & Davis, 2010; Herschell, Kogan, Celedonia, Gavin & Stein, 2009; Vismara, Young, Stahmer, Griffith, & Rogers, 2009).
Limitations
Limitations of the current study warrant some caution in interpreting study results. First, a small sample size given the pilot study design precludes obtaining a wider range of CMH therapist perspectives regarding AIM HI. Although the vast majority of therapists reported a positive experience with the training and delivery of AIM HI, therapists reported that preparation time was a challenge. Specifically, some therapists reported that the preparation time needed to participate in the training and additional time needed to prepare for client sessions was difficult to balance with productivity requirements. Despite this, all of the CMH therapists delivering AIM HI perceived the training and delivery of AIM HI as useful, completed the training, and delivered AIM HI with high fidelity (Brookman-Frazee et al., 2012a). A second limitation relates to the sample of CMH therapists participating in AIM HI. In this study, 77% of the therapist participants were trainees. Recruitment occurred as trainees were just beginning to see new clients and, thus, trainee therapists interested in participating may have been more likely than staff therapists to have a child participant meeting the inclusion criteria. Alternatively, trainees have been found to hold more positive views of EBPs than staff in CMH settings (Aarons et al. 2004). This may have played a role in which therapists were interested in participating in the current study. Further, while it was useful to have data on perceptions of CMH therapists working with children with ASD prior to AIM HI implementation in order to draw some approximate comparisons, this study had no simultaneous control group to more rigorously examine therapist perceptions of AIM HI. Future large-scale studies of AIM HI will include a larger sample size and randomized, controlled design to allow for a control group comparison. Finally, it is important to note that AIM HI was delivered within a very specific CMH service setting. It is not known how AIM HI generalizes to various service settings including individual providers, children whose CMH services are privately insured or located in rural areas, among other settings. Additionally, many CMH settings provide services to a broader range of children with ASD, including lower functioning and more severely impaired children with ASD. The current study may not completely represent this broader population of children with ASD who are provided MH services through community settings.
Conclusion
This qualitative study was conducted as part of a broader pilot study to examine CMH therapist perspectives regarding training and delivery of AIM HI in CMH services. Providing attention to the unique perspectives of therapists allowed for specific information on changes in therapist skills and the therapeutic process, and outcomes perceived to be related to the training model and delivery of the AIM HI intervention. Specifically, CMH therapists valued the AIM HI training, perceived an increase of their skills in working with children with ASD and behavior problems, experienced positive changes in their treatment process working with children with ASD, and reported improved child and family outcomes resulting from the delivery of AIM HI. Results provide preliminary support for the acceptability, feasibility, and effectiveness of implementing EBPs for children with ASD and behavior problems and their families in CMH settings. These results also suggest that continued efforts to implement EBPs may be successful in benefitting therapist skills to treating children with ASD and their families, and thus improving care for families of children with ASD. The next steps are to conduct a large, randomized controlled trial to more rigorously examine the effectiveness of the AIM HI intervention and training model.
Acknowledgments
This work was supported by K23MH077584 (LBF). Preparation for this manuscript was also supported by R01MH094317 (LBF) and K01MH093477 (AD). Further, Ms. Stadnick is funded through Dennis Weatherstone Predoctoral Fellowship awarded through Autism Speaks.
References
- Aarons GA. Mental health provider attitudes toward adoption of evidence-based practice: The evidence-based practice attitude scale (EBPAS) Mental Health Services Research. 2004;6:61–74. doi: 10.1023/b:mhsr.0000024351.12294.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aarons GA, Hurlburt M, Horwitz SM. Advancing a conceptual model of evidence-based practice implementation in public service sectors. Administration and Policy in Mental Health and Mental Health Services Research. 2011;38:4–23. doi: 10.1007/s10488-010-0327-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addis ME, Krasnow AD. A national survey of practicing psychologists’ attitudes toward psychotherapy treatment manuals. Journal of Consulting and Clinical Psychology. 2000;68:331–339. doi: 10.1037//0022-006x.68.2.331. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2000. text rev. [Google Scholar]
- Baumann BL, Kolko DJ, Collins K, Herschell AD. Understanding practitioners’ characteristics and perspectives prior to the dissemination of an evidence-based intervention. Child Abuse & Neglect. 2006;30:771–787. doi: 10.1016/j.chiabu.2006.01.002. [DOI] [PubMed] [Google Scholar]
- Brookman-Frazee L, Baker-Ericzen M, Stadnick N, Taylor R. Parent perspectives on community mental health services for children with autism spectrum disorders. Journal of Child and Family Studies. 2011 doi: 10.1007/s10826-011-9506-8. Advanced online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brookman-Frazee L, Baker-Ericzen M, Stahmer A, Mandell D, Haine RA, Hough RL. Involvement of youths with autism spectrum disorders or intellectual disabilities in multiple public service systems. Journal of Mental Health Research in Intellectual Disabilities. 2009a;2:201–219. doi: 10.1080/19315860902741542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brookman-Frazee L, Drahota A. An individualized mental health intervention for children with autism spectrum disorders (AIM HI): A model to address challenging behaviors in children with ASD – A therapist manual. University of California; San Diego: 2010a. [Google Scholar]
- Brookman-Frazee L, Drahota A, Stadnick N. Training community mental health therapists in a package of evidence-base practice strategies for school-age children with autism spectrum disorders: A pilot study. Journal of Autism and Developmental Disorders. 2012a;42:1651–1661. doi: 10.1007/s10803-011-1406-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brookman-Frazee L, Drahota A, Stadnick N, Palinkas LA. Therapist perspectives on community mental health services for children with autism spectrum disorder. Administration and Policy in Mental Health and Mental Health Services Research. 2012b;39:365–373. doi: 10.1007/s10488-011-0355-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brookman-Frazee L, Garland AF, Taylor R, Zoffness R. Therapists’ attitudes toward psychotherapeutic strategies in community-based psychotherapy with children with disruptive behavior problems. Administration and Policy in Mental Health and Mental Health Services Research. 2009b;36:1–12. doi: 10.1007/s10488-008-0195-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brookman-Frazee LI, Taylor R, Garland AF. Characterizing community-based mental health services for children with autism spectrum disorders and disruptive behavior problems. Journal of Autism and Developmental Disorders. 2010b;40:1188–1201. doi: 10.1007/s10803-010-0976-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casper ES. The theory of planned behavior applied to continuing education mental health professionals. Psychiatric Services. 2007;58:1324–1329. doi: 10.1176/ps.2007.58.10.1324. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Prevalence of autism spectrum disorders—Autism and developmental disabilities monitoring network, 14 sites, United States, 2008. Morbidity and Mortality Weekly Report Surveillance Summary. 2012;61:1–19. [PubMed] [Google Scholar]
- Dingfelder HE, Mandell DS. Bridging the research-to- practice gap in autism intervention: An application of diffusion of innovation theory. Journal of Autism and Developmental Disorders. 2010;41:597–609. doi: 10.1007/s10803-010-1081-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Essock SM, Goldman HH, Van Tosh L, Anthony WA, Appell CR, Bond GR, et al. Evidence-based practices: Setting the context and responding to concerns. Psychiatric Clinics of North America. 2003;26:919–938. doi: 10.1016/s0193-953x(03)00069-8. [DOI] [PubMed] [Google Scholar]
- Garland AF, Brookman-Frazee L, Hurlburt MS, Accurso EC, Zoffness RJ, Haine-Schlagel R, et al. Mental health care for children with disruptive behavior problems: A view inside therapists’ offices. Psychiatric Services. 2010;61:788–795. doi: 10.1176/appi.ps.61.8.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland AF, Hurlburt MS, Hawley KM. Examining psychotherapy processes in a services research context. Clinical Psychology: Science and Practice. 2006;13:30–46. [Google Scholar]
- Glaser BG, Strauss AL. The discovery of grounded theory: Strategies for qualitative research. Chicago, IL: Aldine Publishing Company; 1967. [Google Scholar]
- Glisson C, Landsverk J, Schoenwald S, Kelleher K, Hoagwood KE, Mayberg S, et al. Assessing the organizational social context (OSC) of mental health services: Implications for research and practice. Administration and Policy in Mental Health and Mental Health Services. 2008;35:98–113. doi: 10.1007/s10488-007-0148-5. [DOI] [PubMed] [Google Scholar]
- Guest G, Bunce A, Johnson L. How many interviews is enough? An experiment with data saturation and variability. Field Methods. 2006;18:59–82. [Google Scholar]
- Herschell AD, Kogan JN, Celedonia KL, Gavin JG, Stein BD. Understanding community mental health administrators’ perspectives on dialectical behavior therapy implementation. Psychiatric Services. 2009;60:989–992. doi: 10.1176/appi.ps.60.7.989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herschell AD, Kolko DJ, Baumann BL, Davis AC. The role of therapist training in the implementation of psychosocial treatments: A review and critique with recommendations. Clinical Psychology Review. 2010;30:448–466. doi: 10.1016/j.cpr.2010.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joshi G, Petty C, Wozniak J, Henin A, Fried R, Galdo M, et al. The heavy burden of psychiatric comorbidity in youth with autism spectrum disorders: A large comparative study of a psychiatrically referred population. Journal of Autism and Developmental Disorders. 2010;40:1361–1370. doi: 10.1007/s10803-010-0996-9. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Siegel TC, Bass D. Drawing on clinical practice to inform research on child and adolescent psychotherapy: Survey of practitioners. Professional Psychology: Research and Practice. 1990;21:189–198. [Google Scholar]
- Kim JA, Szatmari P, Bryson SE, Streiner DL, Wilson FJ. The prevalence of anxiety and mood problems among children with autism and Asperger syndrome. Autism. 2000;4:117–132. [Google Scholar]
- Lord C, Bishop S. Autism spectrum disorders: Diagnosis, prevalence, and services for children and families. Social Policy Report. 2010;24:3–21. [Google Scholar]
- Mandell DS, Walrath CM, Manteuffel B, Sgro G, Pinto-Martin J. Characteristics of children with autistic spectrum disorders served in comprehensive community-based mental health settings. Journal of Autism and Developmental Disorders. 2005;35:313–321. doi: 10.1007/s10803-005-3296-z. [DOI] [PubMed] [Google Scholar]
- Marshall C, Rossman GB. Designing qualitative research. 4. Thousand Oaks, CA: Sage Publications; 2006. [Google Scholar]
- Matson JL, Mahan S, Hess JA, Fodstad JC, Neal D. Progression of challenging behaviors in children and adolescents with autism spectrum disorders as measured by the Autism Spectrum Disorders-Problem Behaviors for Children (ASD-PBC) Research in Autism Spectrum Disorders. 2010;4:400–404. [Google Scholar]
- Matson J, Wilkins J, Macken J. The relationship of challenging behaviors to severity and symptoms of autism spectrum disorders. Journal of Mental Health Research in Intellectual Disabilities. 2009;2:1931–5864. [Google Scholar]
- Nakamura BJ, Higa-McMillan CK, Okamura KH, Shimabukuro S. Knowledge of and attitudes towards evidence-based practices in community child mental health practitioners. Administration and Policy in Mental Health. 2011;38:287–300. doi: 10.1007/s10488-011-0351-2. [DOI] [PubMed] [Google Scholar]
- National Standards Report. The national standards project—Addressing the need for evidence-based practice guidelines for autism spectrum disorders. Randolph: National Autism Center; 2009. [Google Scholar]
- Nelson TD, Steele RG, Mize JA. Practitioner attitudes toward evidence-based practice: Themes and challenges. Administration and Policy in Mental Health and Mental Health Service Research. 2006;33:398–409. doi: 10.1007/s10488-006-0044-4. [DOI] [PubMed] [Google Scholar]
- Odom SL, Collet-Klingenberg L, Rogers SJ, Hatton DD. Evidence-based practices in interventions for children and youth with autism spectrum disorders. Preventing School Failure. 2010;54:275–282. [Google Scholar]
- Sheehan AK, Walrath CM, Holden EW. Evidence-based practice use, training and implementation in the community-based service setting: A survey of children’s mental health service providers. Journal of Child and Family Studies. 2007;16:169–182. [Google Scholar]
- Stadnick N, Drahota A, Brookman-Frazee L. Parent perspectives of an evidence-based mental health intervention for children with autism spectrum disorders delivered in community mental health clinics. Journal of Child and Family Studies. 2012 doi: 10.1007/s10826-012-9594-0. Advanced online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart RE, Chambless DL. Does psychotherapy research inform treatment decisions in private practice? Journal of Clinical Psychology. 2007;63:267–281. doi: 10.1002/jclp.20347. [DOI] [PubMed] [Google Scholar]
- Sverd J, Dubey DR, Schweitzer R, Ninan R. Pervasive developmental disorders among children and adolescents attending psychiatric day treatment. Psychiatric Services. 2003;54:1519–1525. doi: 10.1176/appi.ps.54.11.1519. [DOI] [PubMed] [Google Scholar]
- Tappe A. Using NVivo in qualitative research. Melbourne: QSR International; 2002. [Google Scholar]
- Vismara LA, Young GS, Stahmer AC, Griffith EM, Rogers SJ. Dissemination of evidence-based practice: Can we train therapists from a distance? Journal of Autism and Developmental Disorders. 2009;39:1636–1651. doi: 10.1007/s10803-009-0796-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willms DG, Best AJ, Taylor DW, Gilbert JR, Wilson DMC, Lindsay EA, et al. A systematic approach for using qualitative methods in primary prevention research. Medical Anthropology Quarterly. 1990;4:391–409. [Google Scholar]
- Wood JJ, Gadow KD. Exploring the nature and function of anxiety in youth with autism spectrum disorders. Clinical Psychology: Science and Practice. 2010;17:281–292. [Google Scholar]