Abstract
Background:
Stage of Change and Health Belief Models are two the most common models that have been applied in mammography screening behaviors. The purpose of this study was to identify women in different stages of mammography adoption and to examine association between women's beliefs by stage of change among Iranian women.
Methods:
In this population-based study, mammography screening behavior determined using the Rakoweski stage of change scale, and women beliefs were determined by Farsi version of Champion's Health Belief Model scale (CHBMS). The obtained data were analyzed by SPSS (version 16.0) using statistical analysis of variance and Chi-square tests that used to determine relation between socio-demographic variables and HBM scales with stage of mammography. In all of the tests, a significant level α = 0.05 was considered.
Results:
According to stages of change distributions for mammography screening behavior, 36.2% were in pre-contemplation, 21.1% in contemplation, 4.2% in action, 6.2% in maintenance, and 32.3% were in relapse stage. There were significant differences in mammography stage by age, education, married status, family monthly income, husband job, information about breast cancer, and history of breast problems. ANOVA test showed significant differences by stages for all HBM scales, except to perceived severity.
Conclusion:
The findings indicated that women in pre-contemplation, relapse, and contemplation stages are more likely need to educational intervention, which emphasizes the benefits and barriers of mammography, health motivation, and self-efficacy. Furthermore, examining individuals’ beliefs about breast cancer and mammography screening by stage of mammography adoption is especially important in order to development of effectiveness interventions, which targeted to stage of change and promote mammography screening behavior.
Keywords: Breast cancer, Health Belief Model, mammography screening, stage of change, women
INTRODUCTION
Nowadays, cancer is one of the most common causes of death, which affects individuals’ life quality in the world.[1,2] According to WHO reports, about 7.6 million people have died of cancer in 2008 and approximately 12 million deaths will occur worldwide in 2030.[3] In addition, reports of Iran national death registry showed that cancer is the second cause of non-accidental death in our country.[4]
Breast cancer is the top of diagnosed cancer in women, both in developed and developing countries. Incidence rate of this disease cover a wide range in different countries, the highest in North America [Age-Standardized Rate (ASR): 123.6 per 100,000], and the lowest in South Central Asia (ASR: 21.8 per 100,000).[5,6] In Islamic Republic of Iran, although breast cancer incidence rate is lower than developed communities, it is currently ranked as the first among malignancies diagnosed in women; accounting for 25% of all cancers among Iranian females.[7] Based on the literature, the incidence of breast cancer in women increased during recent decade in Iran.[8,9] Emami Razavi et al. study showed that new cases of breast cancer increased from 3250 cases in 2003 to 6456 cases in 2006.[9] It is estimated that the crude incidence rate of breast cancer is about 20 new cases per 1,000,000 women annually, which regards to 30 million female populations, 6000 new cases of breast cancer will occur per year.[10]
It was noted that breast cancer in Iranian women occurs more commonly in younger women, aged between 35 and 44 years.[11] Furthermore, majority of women (82%) diagnosed with advanced-stage breast cancer (18% stage II and 77% stage III).[12] It is well established that delay in diagnosis and prompt treatment of breast cancer decline survival.[13,14] The American Cancer Society (ACS) states that the survival rate for women diagnosed with localized breast cancer is 98%; if cancer has spread to near lymph nodes or distant lymph nodes or organs, the 5 year survival is 84% or 23%, respectively.[15]
The principle cause of breast cancer is uncertain; therefore, its morbidity and mortality decrease depends on secondary prevention.[16,17] Breast cancer screening, especially with mammography recommended by the American Cancer Society (ACS), the American Medical Association (AMA), and also by the American College of Obstetricians and Gynecologist (ACOG) recommended that the women older than 40 years should have annual mammography screening and going on it as long as they are in good health.[15,17,18] According to ACS, mammography will diagnose about 80% to 90% of breast cancers in women without symptoms.[15] Furthermore, annual mammography is introduced as the most effective and valuable method for early detection of breast cancer in the preclinical phase before tumor has metastasized.[17] Iran ministry of health recommendation is that women 40 years and older have a mammogram every year.[19]
Despite effectiveness of mammography screening in decreasing breast cancer mortality, the studies’ findings in Iran[20–22] revealed that compared with developed countries, the mammography rate is low among Iranian women.[23] Therefore, analyzing behavior change is helpful to understand why some women are successful at changing behavior and others are not. According to Stage of Change Model, health behavior change can be occurred on a continuum of stages wherein the individual moves from not thinking about behavior to maintaining adoption of the behavior.[24,25]
The Transtheoretical Model (TTM), also known as Stage of Change Model, was adapted in the early 1980s as a method to understand behavior change. This model proposes that behavior change is a process that occurs in a series of incremental stages. It has been applied widely to survey different health behaviors such as smoking, alcohol and substance abuse, high-fat diet, exercise, breast feeding, anxiety and panic disorders, depression, HIV/AIDS prevention, mammography, and other cancer screening.[26–28] TTM has 4 principle constructs comprising of: (1) Stage of change adoption (readiness to action), (2) Process of change (cognitive, affective, and behavioral activities that facilitate behavior change), (3) Decisional balance (pros and cons of behavior change), and (4) Self-efficacy (confidence to make and continue changes in difficult situation).[26,29]
Stage of change describes the person's current health behavior and its intention regarding to behavior change.[30] Rakowski and collaborators in 1992 adapted this model to predict mammography use. Five stages of mammography adoption defined by Rakowski et al. including :(I) – Pre-contemplation (women who have never had no prior mammogram and are not planning to get a mammogram in the coming year), (II) – Contemplation (women who are planning to get a mammogram in the coming year, but have not yet done), (III) – Action (women who have had a mammogram with age-specific interval and intent to have another one in the coming year), (IV) – Maintenance (women who have two or more mammogram on schedule and intend to have another one in the coming year) and (V) – Relapse (women who have had one or more mammogram in the previous but don’t intend to have another one in the coming year).[31,32]
Decisional balance focuses on the positive and negative aspects of a health behavior, which are similar to Health Belief Model's concepts of perceived benefits and perceived barriers. The decision to move toward action and maintenance is based on the relative weight give to pros and cons of a behavior change.[29,33] Several studies have verified the positive relationship between decisional balance and stage of mammography adoption.[27,28,34] To our knowledge, there are no published studies on the stage of change mammography screening in Iranian women. To investigate this important issue in Iran, we applied the stage of change to examine mammography screening behavior among Iranian women aged 40 years and older. Findings of this primary survey can provide useful evidence for designing effective interventions to promote mammography screening in Iranian women. Furthermore, this research seeks to answer 3 following questions:
How is the distribution of Iranian women in different stages of mammography adoption?
What is the association between the socio-demographic factors and stage of mammography adoption?
Are there differences in HBM scales (perceived susceptibility, perceived severity, perceived benefits, perceived barriers, health motivation, and self-efficacy) by stage of change?
METHODS
Study design and sample
This was a population-based study, in which the factors related to stage of mammography adoption on the basis of the Stage of Change Model was investigated. The sample population of this research was women of 40 years old and older in Isfahan, a city located in central region of Iran. Inclusion criteria for participation in this study included being Isfahanian women aged 40 years and older, no personal history of breast cancer, willingness to participate in the survey, and being able to speak. Therefore, we excluded females with a history of breast cancer and women <40 years old.
Telephone interview were carried out with 384 eligible women randomly selected from the communication center of Isfahan, Iran. At first, 2500 immobile telephone numbers were acquired from Isfahan communication center, which were randomly chosen from all of telephone centers of Isfahan city. Telephone interviews were accomplished over a 14-week period from March 2011 to June 2011. One female PhD student of health education conducted all of the telephone interviews. At first, interviewer briefly explained the purpose of the survey and how their response may help future planning for women's health. Also, these confidences give to each person including its anonymous and voluntary nature of interview. Then, data was collected from those whom verbally consented to participate. A telephone interview lasted between 20-45 minutes. From total of 2500 telephone calls, there was no response from 985 (39.4%) telephone contacts, 82 (3.28%) blocked the telephone number, in 196 (7.8%) contacts, there weren’t women, 648 (25.92%) women were in the unsuitable age group (<40 years old), and 589 (23.56%) contacts contained women in the appropriate age group (>40 years old), of which 205 women were not eligible to interview in the study due to unwillingness to participate, or had personal history of breast cancer. For each telephone number with no response or women who were absent, telephone dialing repeated a total of 3 times at different times of the day with at least one time being scheduled at weekend. As a result, 348 women were interviewed by telephone. The Ethical Committee of Isfahan Medical University approved the study.
Instrument
In this study, socio-demographic variables were measured using information such as age, marriage age, age of first birth, level of education, current marital status, number of child, breastfeeding duration, menopausal status, health insurance coverage, monthly household income, having first-degree relatives with history of breast cancer, and personal history of breast problems.
The history of having mammography screening behavior was assessed using 3 questions. These questions were included (1) “Have you ever had a mammogram (yes/no),” (2) if yes, “number of mammography,” and (3) “The time of last mammography screening.”
In order to assess women's intention to get mammography, we utilized mammography stage of change scale developed by Rakoweski et al.[35] The stage of change had been defined as: Pre-contemplation, contemplation, action, maintenance, and relapse (discussed in the introduction section). This scale comprise of one question with 5 choices, subjects were placed in one of the 5 stage of change described previously.
To assess the women's beliefs toward positive and negative aspects of mammography screening behavior, we used the Farsi version of Champion Health Belief Model Scale (CHBMS), which was adapted by Taymooori and Berry.[36] This section consists of 61 items: Three items assessed the perceived susceptibility, 7 items assessed perceived severity, 7 items assessed health motivation, 6 items assessed benefits of mammography, 10 items assessed the barriers of mammography, and 4 items assessed perceived self-efficacy. Each item has a 5-point likert scale, with possible response ranging from strongly disagree = 1 to strongly agree = 5. Scores of all items in each subscale was calculated separately.
Data analyzes
The obtained data were analyzed by SPSS version 16.0 (SPSS Inc, Chicago, Illinois). Descriptive analyzes were utilized to summarize the subject's variables. Analysis of variance and Chi-square tests were used to determine relation between socio-demographic variables and HBM scales with stage of mammography. In all of the tests, a significant level α = 0.05 was considered.
RESULTS
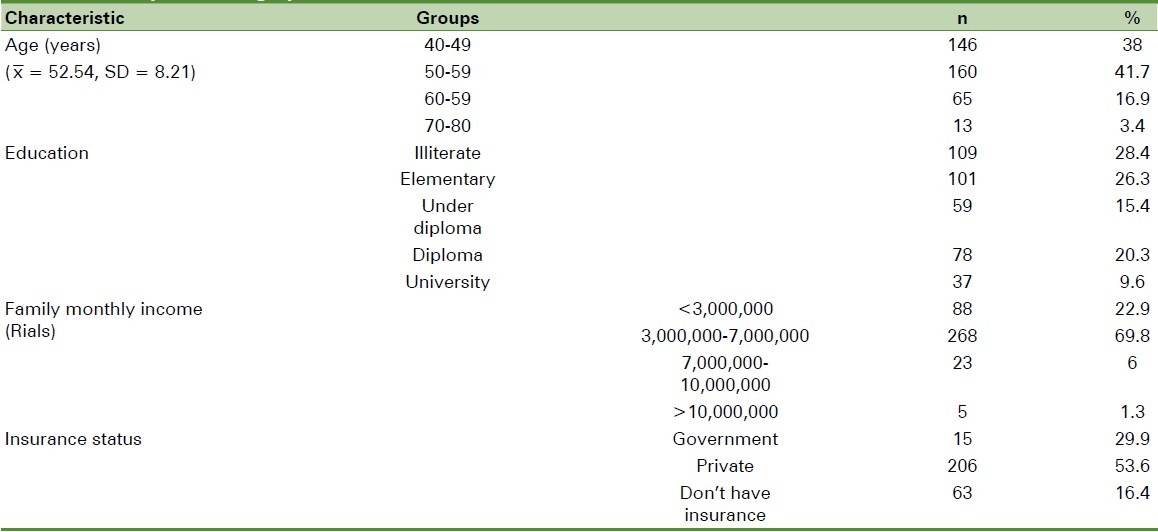
In total, 384 women aged 40 years and older were interviewed by telephone in the current study. The mean age of the participants was 52.24 ± 8.21 years (ranged from 40 to 80 years). The most (78.6%) were housekeeper, 83.9% were married, and 26.3% had elementary education. More than three-forth of the women (83.6%) had health insurance, and 69.8% stated family monthly income between 3-7 million Rials. Fewer than half (44.3%) expressed having had at least one mammography in their lifetime, and the majority of these women (85.6%) reported receiving their most recent mammogram longer than 2 years [Table 1].
Table 1.
Participant demographic characteristics (N = 384)
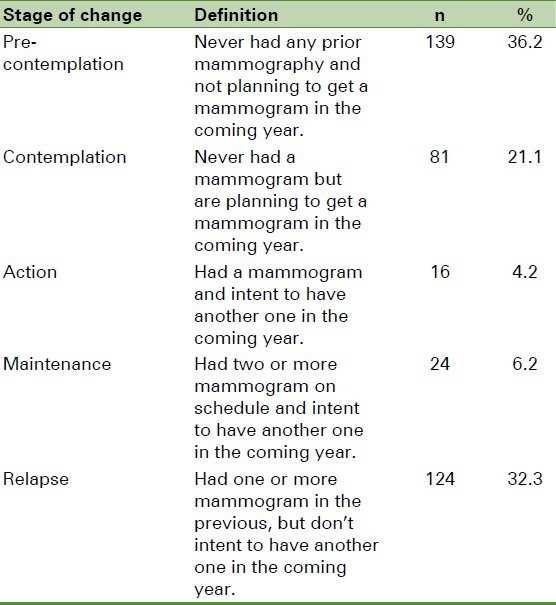
Distribution of mammography adoption stage showed that most of subjects were in the pre-contemplation stage (36.2%) and only 10.6% were in action and maintenance stages [Table 2].
Table 2.
Mammography stage of change
Socio-demographic variables and stage of mammography adoption
Socio-demographic characteristics by stage of mammography adoption are summarized in Table 3. There were significant differences in mammography stage by age (F = 11.18, P = 0/000), education (x2 = 25.7, df = 12, P = 0/01), married status (x2 = 11.13, df = 3, P = 0/01), menopause (x2 = 15.89, df = 3, P = 0/001), hysterectomy (x2 = 9.19, df = 3, P = 0/02), family monthly income (x2 = 16.9, df = 6, P = 0/009), husband's job (x2 = 26.67, df = 12, P = 0/009), information about breast cancer (x2 = 28.07, df = 3, P = 0/000), history of breast problems (x2 = 90.63, df = 3, P = 0/000), and how many years ago got mammogram (x2 = 3.58, df = 6, P = 0/000).
Table 3.
Demographic characteristic by stage of mammography adoption
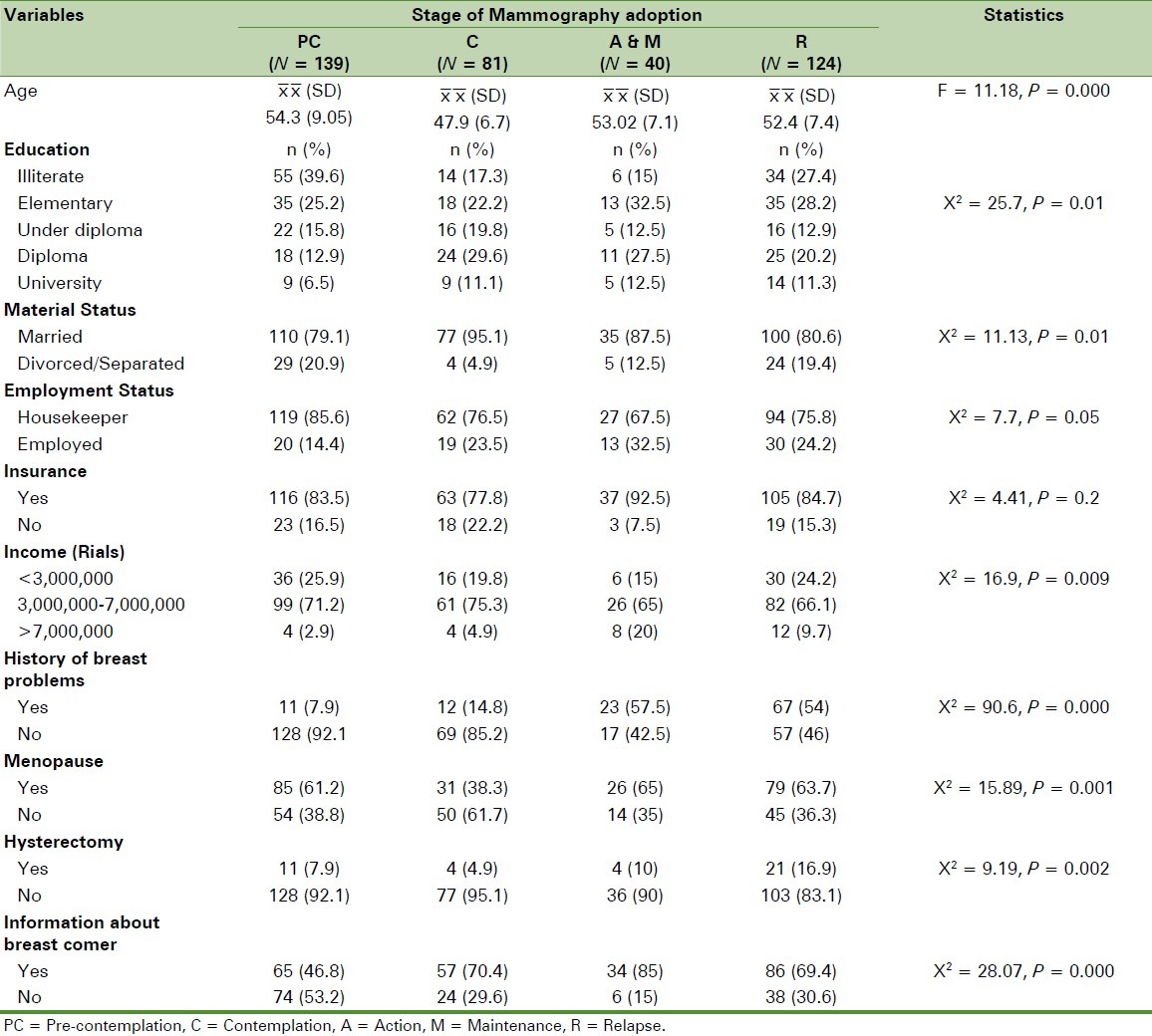
These results revealed that women in the contemplation stage were significantly younger than women in other stages. More women in the pre-contemplation stage were illiterate, and significantly fewer women had information about breast cancer than women in the action and maintenance stages. Significantly, more women in the action and maintenance stages had history of breast problems than women in the pre-contemplation stage. No significant differences observed in employment status and health insurance among stages of mammography adoption.
HBM scales and stage of mammography
One-way analysis of variance (ANOVA) was used to identify associations between HBM scales and stage of mammography adoption. Also, differences between groups were determined by Scheffe's post hoc analysis. There were significant differences by stages for all HBM scales, except to perceived severity [Table 4]. Perceived susceptibility was significantly different by stages (F = 4.82, P = 0.001). Scheffe's post hoc test revealed that the women in the maintenance stage had significantly higher perceived susceptibility about breast cancer in comparison to those in the pre-contemplation, relapse, contemplation, and action stages.
Table 4.
Comparison of CHBM Scales by stage of mammography adoption
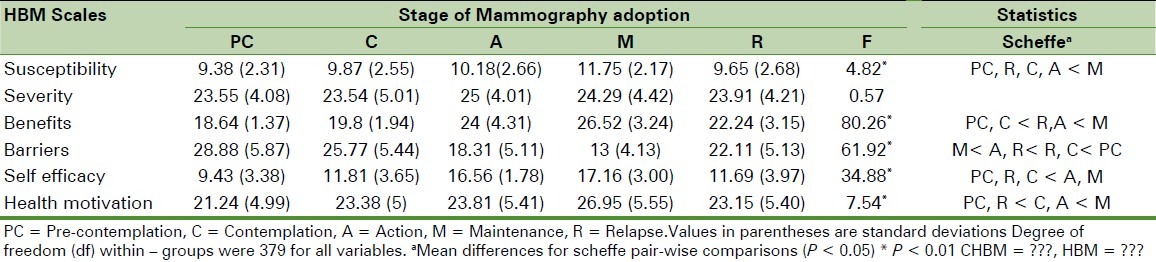
Significantly, perceived benefits were associated by stage (F = 80.26, P = 0.000). Scheffe's post hoc tests revealed that women who currently are in maintenance stage, perceived significantly more benefits than those in action, relapse, contemplation, and pre-contemplation stages. For perceived barriers, women in the pre-contemplation stage had the highest scores followed by the contemplation and relapse stages and those in the maintenance stage had the lowest scores (F = 61.92, P = 0.000).
In addition, we found that women in the maintenance and action stages had more perceived self-efficacy than did women in the contemplation, relapse and pre-contemplation stages (F = 34.88, P = 0.000). Finally, health motivation scale was significantly related to stage (F = 90.69, P = 0.000). Women in the maintenance stage had significantly more health motivation than did women in the action, contemplation, relapse, and pre-contemplation stages. Furthermore, women who regularly received mammography (maintenance stage) had more motivation and self-efficacy for health than women who were not thinking about mammography screening (pre-contemplation stage).
DISCUSSION
This investigation was one of the first studies, which surveyed the stages of mammography adoption among Iranian women. This study also examined association between HBM scales with stage of change in order to developing effective and stage-matched interventions. Our study finding revealed that mammography screening rate was low among Iranian women. Despite more than 40% of participants reported that had at least one mammogram in their lifetime, only 10.4% women were in action and maintenance stages and 33.3% were in the relapse stage. Kim et al. found that 80% of study participants were in the relapse stage and stated “this sporadic mammography use could be partly attributed to obtaining screening mammography by chance.”[37]
In our study, the majority of subjects (36.2%) were in the pre-contemplation stage. Tu et al. also reported pre-contemplation stage as the most percentage among a sample of Cambodian American women.[38] Whereas in Strong et al.[39] and Wu et al.[27,33] studies, the highest proportion of study participants were in the maintenance and action stages. These differences in distribution of mammography stages could be because of difference in beliefs and cultural, social, economical characteristics of studied samples.
Similar to previous studies,[40–46] our study results showed that level of education was significantly associated with the stage of mammography adaption. In this study, more women in pre-contemplation were illiterate. These women usually have lower health literacy and low information about breast cancer and mammography. Furthermore, this suggests more emphasis on educational interventions in less educated women. While prior studies suggested that interventions among women with high education level and more health literacy increase mammography adoption.[46–52]
Consistent with finding from prior studies, marital status was significantly related to mammography stage of adoption.[44,46,53–55] Divorced/separated or unmarried women usually have more problem including lower social support, lower income, and more hopelessness than married women.[44,53,56,57] Unlike to finding of Strong et al., we did not find insurance to be a significant factor related to stage of mammography adoption.[39]
In this study and contrary to Otero-sabogel et al.[28], we found that older women were more in pre-contemplation stage. Dolan et al. and Marwill et al. also found similar finding.[58,59] These results indicated that intervention should emphasize older women because they are at high risk for developing breast cancer.
The present study showed that beliefs about mammography screening were significantly different by stage of change. Perceived susceptibility, benefits, and self-efficacy was lower in pre-contemplation than women in other stages of mammography adoption. This finding is consistent with other studies that found perceived susceptibility, benefits, and self-efficacy to be different by stage.[34,37,60–65] Whereas, Wu et al. study in Asian American women showed that perceived benefits were not significantly different by stage.[27]
Other finding of this study revealed that perceived barriers were significantly higher in pre-contemplators. This finding is similar to reported results in other studies.[27,34,37,60–62,66] In this study, also, health motivation was significantly different by stage. Women in maintenance stage had higher motivation for health, contrary to pre-contemplators as reported by Champion et al.[60]
In conclusion, association between beliefs and stage of mammography adoption demonstrated that women in the maintenance and action stages perceived more benefits and less barriers of mammography screening, had higher motivation for health, and more confidence for having mammography. Based on these findings, women in pre-contemplation, relapse, and contemplation stages are more likely to need an educational intervention, which emphasizes the benefits and barriers of mammography, health motivation, and self-efficacy. Furthermore, examining individuals’ beliefs about breast cancer and mammography screening by stage of mammography adoption is especially important in order to development of effectiveness interventions, which targeted to stage of change and promote mammography screening behavior.
Limitation
This is one of the first studies to examine the mammography-associated beliefs by stage of mammography adoption among Iranian women. As the current study was conducted by telephone interview, it would be possible that some bias may have occurred. It should be noted that these potential biases have been described elsewhere.
This study was limited to women who were living in urban regions of Isfahan. However, since women's beliefs could be different by various regions of the country, for example, in urban and rural location, additional studies should be implemented in other regions of the country. Moreover, this study has been examined stage of mammography adoption and other constructs of TTM only; therefore, decisional balance and process of change have not been investigated. Further studies will be necessary to assess these constructs among Iranian women.
ACKNOWLEDGMENT
This article is part of a PhD dissertation (project number = 389476). The authors would like to thank the Deputy for Research of Isfahan University of Medical Sciences for their financial support and all the women who participated in this study.
Footnotes
Source of Support: Isfahan University of Medical Sciences
Conflict of Interest: None declared
REFERENCES
- 1.Babaei M, Jaafarzadeh H, Sadjadi A, Samadi F, Yazdanbod A, Fallah M, et al. Cancer incidence and mortality in Ardabil: Report of an ongoing population-based cancer registry in Iran, 2004-2006. Iran J Public Health. 2009;38:35–45. [Google Scholar]
- 2.Katapodi M, Lee K, Facione N, Dodd M. Predictors of perceived breast cancer risk and the relation between perceived risk and breast cancer screening: A meta-analytic review. Prev Med. 2004;38:388–402. doi: 10.1016/j.ypmed.2003.11.012. [DOI] [PubMed] [Google Scholar]
- 3.Farmer P, Frenk J, Knaul FM, Shulman LN, Alleyne G, Armstrong L, et al. Expansion of cancer care and control in countries of low and middle income: A call to action. Lancet. 2010;376:1186–93. doi: 10.1016/S0140-6736(10)61152-X. [DOI] [PubMed] [Google Scholar]
- 4.Naghavi M, Jafari N. Research and Development Office. Tehran, Iran: Ministry of Health, Deputy for Health Directory; 2003. Mortality views in 23 Provinces of Iran in 2004; pp. 75–6. [Google Scholar]
- 5.Harirchi I, Kolahdoozan S, Karbakhsh M, Chegini N, Mohseni SM, Montazeri A, et al. Twenty years of breast cancer in Iran: Downstaging without a formal screening program. Ann Oncol. 2011;22:93–7. doi: 10.1093/annonc/mdq303. [DOI] [PubMed] [Google Scholar]
- 6.Yip CH, Smith RA, Anderson BO, Miller AB, Thomas DB, Ang ES, et al. Guideline implementation for breast healthcare in low- and middle-income countries: Early detection resource allocation. Cancer. 2008;113(8 Suppl):2244–56. doi: 10.1002/cncr.23842. [DOI] [PubMed] [Google Scholar]
- 7.Heydari Z, Mahmoudzadeh-Sagheb HR, Sakhavar N. Breast cancer screening knowledge and practice among women in southeast of Iran. Acta Med Iran. 2008;46:321–8. [Google Scholar]
- 8.Moodi M, Balali-Mood M, Sharifirad GR, Shahnazi H, Sharifzadeh G. Evaluation of breast self-examination program using Health Belief Model in female students. J Res Med Sci. 2011;16:316–22. [PMC free article] [PubMed] [Google Scholar]
- 9.Emami Razavi S, Aghajani H, Haghazali M, Nadali F, Ramazani F, Dabiri E, et al. The most common cancers in Iranian women. Iran J Public Health. 2009;38:109–12. [Google Scholar]
- 10.Montazeri A, Ebrahimi M, Mehrdad N, Ansari M, Sajadian A. Delayed presentation in breast cancer: A study in Iranian women. BMC Womens Health. 2003;3:4. doi: 10.1186/1472-6874-3-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Taleghani F, Yekta ZP, Nasrabadi AN. Coping with breast cancer in newly diagnosed Iranian women. J Adv Nurs. 2006;54:265–72. doi: 10.1111/j.1365-2648.2006.03808_1.x. [DOI] [PubMed] [Google Scholar]
- 12.Mousavi SM, Montazeri A, Mohagheghi MA, Jarrahi AM, Harirchi I, Najafi M, et al. Breast cancer in Iran: An epidemiological review. Breast J. 2007;13:383–91. doi: 10.1111/j.1524-4741.2007.00446.x. [DOI] [PubMed] [Google Scholar]
- 13.Yavari P, Pourhoseingholi MA. Socioeconomic factors association with knowledge and practice of breast self-examination among Iranian women. Asian Pac J Cancer Prev. 2007;8:618–22. [PubMed] [Google Scholar]
- 14.Sim HL, Seah M, Tan SM. Breast cancer knowledge and screening practices: A survey of 1,000 Asian women. Singapore Med J. 2009;50:132–8. [PubMed] [Google Scholar]
- 15.Cancer Facts and Figures 2011. Atlanta: American Cancer Society; 2011. American Cancer Society, (ACS) pp. 9–10. [Google Scholar]
- 16.Gøtzsche PC, Nielsen M. Screening for breast cancer with mammography. Cochrane Database Syst Rev. 2009;4:CD001877. doi: 10.1002/14651858.CD001877.pub3. [DOI] [PubMed] [Google Scholar]
- 17.Bulletins ACoP. ACOG Practice Bulletin: Clinical management guidelines for obstetrician gynecologists. Number 122, August 2011: Breast Cancer screening (replaces practice bulletin, number 152, April 2003) Obstet Gynecol. 2011;122:1–11. [Google Scholar]
- 18.Dundar PE, Ozmen D, Ozturk B, Haspolat G, Akyildiz F, Coban S, et al. The knowledge and attitudes of breast self-examination and mammography in a group of women in a rural area in western Turkey. BMC Cancer. 2006;6:43. doi: 10.1186/1471-2407-6-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goya M. Iranian Annual Cancer Registration Report 2005/2006. Ministry of Health and Medical Education, Health Deputy. Center for Disease Control and Prevention. 2007 [Google Scholar]
- 20.Farshbaf Khalili A, Shahnazi M, Ghahveehi A, Torabi Sh. Performance conditions of breast cancer screening methods and its efficient factors among women referring to health centers of Tabriz. Iran J Nurs Res. 2009;4:27–38. [Google Scholar]
- 21.Pormehr S, Karimian NS, Sheykhan Z, Alavi Majd H. Investigation of breast cancer screening tests performance and affecting factors in women referred to Ardebil's health and medical centers. J Ardabil Univ Med Sci Health Serv. 2011;10:310–8. [Google Scholar]
- 22.Banaeian SH, Kazemian A, Kheiri S. Knowledge, attitude and practice about breast cancer screening and related factors among women referred to health care centers in Boroujen in 2005. Shahrekord Univ Med Sci J. 2006;7:28–34. [Google Scholar]
- 23.Rahman S, Price JH, Dignan M, Lindquist PS, Jordan TR. Access to mammography facilities and detection of breast cancer by screening mammography: A GIS approach. Int J Cancer Prev. 2009;2:403–13. [PMC free article] [PubMed] [Google Scholar]
- 24.Prochaska J, Wright J, Velicer W. Evaluating theories of health behavior change: A hierarchy of criteria applied to the transtheoretical model. Appl Psychol. 2008;57:561–88. [Google Scholar]
- 25.Champion V, Springston J, Zollinger T, Saywell R, Jr, Monahan P, Zhao Q, et al. Comparison of three interventions to increase mammography screening in low income African American women. Cancer Detect Prev. 2006;30:535–44. doi: 10.1016/j.cdp.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 26.Glanz K, Rimer BK, Viswanath K. Health behavior and health education: Theory, research, and practice. San Francisco: Jossey-Bass Inc Pub; 2008. pp. 98–117. [Google Scholar]
- 27.Wu TY, Hsieh HF, West BT. Stages of mammography adoption in Asian American women. Health Educ Res. 2009;24:748–59. doi: 10.1093/her/cyp009. [DOI] [PubMed] [Google Scholar]
- 28.Otero-Sabogal R, Stewart S, Shema S, Pasick R. Ethnic differences in decisional balance and stages of mammography adoption. Health Educ Behav. 2007;34:278–96. doi: 10.1177/1090198105277854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hayden J. Introduction to Health Behavior Theory. United States: Jones and Bartlett Learning; 2009. pp. 65–78. [Google Scholar]
- 30.Lin ZC, Effken JA. Effects of a tailored web-based educational intervention on women's perceptions of and intentions to obtain mammography. J Clin Nurs. 2010;19:1261–9. doi: 10.1111/j.1365-2702.2009.03180.x. [DOI] [PubMed] [Google Scholar]
- 31.Rakowski W, Dube C, Goldstein M. Considerations for extending the transtheoretical model of behavior change to screening mammography. Health Educ Res. 1996;11:77–96. [Google Scholar]
- 32.Rakowski W, Andersen MR, Stoddard AM, Urban N, Rimer BK, Lane DS, et al. Confirmatory analysis of opinions regarding the pros and cons of mammography. Health Psychol. 1997;16:433–41. doi: 10.1037//0278-6133.16.5.433. [DOI] [PubMed] [Google Scholar]
- 33.Wu TY, West BT. Mammography stage of adoption and decision balance among Asian Indian and Filipino American women. Cancer Nurs. 2007;30:390–8. doi: 10.1097/01.NCC.0000290812.14571.2c. [DOI] [PubMed] [Google Scholar]
- 34.Champion VL, Skinner CS. Differences in perceptions of risk, benefits, and barriers by stage of mammography adoption. J Womens Health (Larchmt) 2003;12:277–86. doi: 10.1089/154099903321667618. [DOI] [PubMed] [Google Scholar]
- 35.Rakowski W, Ehrich B, Dubé C, Pearlman D, Goldstein M, Peterson K, et al. Screening mammography and constructs from the transtheoretical model: Associations using two definitions of the stages-of-adoption. Ann Behav Med. 1996;18:91–100. doi: 10.1007/BF02909581. [DOI] [PubMed] [Google Scholar]
- 36.Taymoori P, Berry T. The validity and reliability of Champion's Health Belief Model Scale for breast cancer screening behaviors among Iranian women. Cancer Nurs. 2009;32:465–72. doi: 10.1097/NCC.0b013e3181aaf124. [DOI] [PubMed] [Google Scholar]
- 37.Kim JH, Menon U. Pre- and postintervention differences in acculturation, knowledge, beliefs, and stages of readiness for mammograms among Korean American women. Oncol Nurs Forum. 2009;36:E80–92. doi: 10.1188/09.onf.e80-e92. [DOI] [PubMed] [Google Scholar]
- 38.Tu SP, Yasui Y, Kuniyuki A, Schwartz SM, Jackson JC, Taylor VM. Breast cancer screening: Stages of adoption among Cambodian American women. Cancer Detect Prev. 2002;26:33–41. doi: 10.1016/S0361-090X(02)00013-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Strong C, Liang W. Relationships between decisional balance and stage of adopting mammography and Pap testing among Chinese American women. Cancer Epidemiol. 2009;33:374–80. doi: 10.1016/j.canep.2009.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Welsh AL, Sauaia A, Jacobellis J, Min SJ, Byers T. The effect of two church-based interventions on breast cancer screening rates among Medicaid-insured Latinas. Prev Chronic Dis. 2005;2:A07. [PMC free article] [PubMed] [Google Scholar]
- 41.Kreuter MW, Lukwago SN, Bucholtz DC, Clark EM, Sanders-Thompson V. Achieving cultural appropriateness in health promotion programs: Targeted and tailored approaches. Health Educ Behav. 2003;30:133–46. doi: 10.1177/1090198102251021. [DOI] [PubMed] [Google Scholar]
- 42.Husaini BA, Sherkat DE, Levine R, Bragg R, Van CA, Emerson JS, et al. The effect of a church-based breast cancer screening education program on mammography rates among African-American women. J Natl Med Assoc. 2002;94:100–6. [PMC free article] [PubMed] [Google Scholar]
- 43.Husaini BA, Sherkat DE, Bragg R, Levine R, Emerson JS, Mentes CM, et al. Predictors of breast cancer screening in a panel study of African American women. Women Health. 2001;34:35–51. doi: 10.1300/J013v34n03_03. [DOI] [PubMed] [Google Scholar]
- 44.Lubetkin EI, Santana A, Tso A, Jia H. Predictors of cancer screening among low-income primary care patients. J Health Care Poor Underserved. 2008;19:135–48. doi: 10.1353/hpu.2008.0001. [DOI] [PubMed] [Google Scholar]
- 45.Champion V, Menon U. Racial and educational differences in mammography-related perceptions among 1,336 nonadherent women. J Psychosoc Oncol. 2002;20:1–18. [Google Scholar]
- 46.Steele-Moses SK, Russell KM, Kreuter M, Monahan P, Bourff S, Champion VL. Cultural constructs, stage of change, and adherence to mammography among low-income African American women. J Health Care Poor Underserved. 2009;20:257–73. doi: 10.1353/hpu.0.0123. [DOI] [PubMed] [Google Scholar]
- 47.Ward E, Jemal A, Cokkinides V, Singh GK, Cardinez C, Ghafoor A, et al. Cancer disparities by race/ethnicity and socioeconomic status. CA Cancer J Clin. 2004;54:78–93. doi: 10.3322/canjclin.54.2.78. [DOI] [PubMed] [Google Scholar]
- 48.Rauscher GH, Hawley ST, Earp JA. Baseline predictors of initiation vs.maintenance of regular mammography use among rural women. Prev Med. 2005;40:822–30. doi: 10.1016/j.ypmed.2004.09.029. [DOI] [PubMed] [Google Scholar]
- 49.Calvocoressi L, Kasl SV, Lee CH, Stolar M, Claus EB, Jones BA. A prospective study of perceived susceptibility to breast cancer and nonadherence to mammography screening guidelines in African American and White women ages 40 to 79 years. Cancer Epidemiol Biomarkers Prev. 2004;13:2096–105. [PubMed] [Google Scholar]
- 50.Selvin E, Brett KM. Breast and cervical cancer screening: Sociodemographic predictors among White, Black, and Hispanic women. Am J Public Health. 2003;93:618–23. doi: 10.2105/ajph.93.4.618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Greene AL, Torio CM, Klassen AC. Measuring sustained mammography use by urban African-American women. J Community Health. 2005;30:235–51. doi: 10.1007/s10900-005-3703-6. [DOI] [PubMed] [Google Scholar]
- 52.Grindel CG, Brown L, Caplan L, Blumenthal D. The effect of breast cancer screening messages on knowledge, attitudes, perceived risk, and mammography screening of African American women in the rural South 2004. Oncol Nurs Forum. 2004;31:801–8. doi: 10.1188/04.ONF.801-808. [DOI] [PubMed] [Google Scholar]
- 53.Farmer D, Reddick B, D’Agostino R, Jackson SA. Psychosocial correlates of mammography screening in older African American women. Oncol Nurs Forum. 2007;34:117–23. doi: 10.1188/07.ONF.117-123. [DOI] [PubMed] [Google Scholar]
- 54.Taplin SH, Ichikawa L, Yood MU, Manos MM, Geiger AM, Weinmann S, et al. Reason for late-stage breast cancer: Absence of screening or detection, or breakdown in follow-up? J Natl Cancer Inst. 2004;96:1518–27. doi: 10.1093/jnci/djh284. [DOI] [PubMed] [Google Scholar]
- 55.Zhu K, Hunter S, Bernard LJ, Payne-Wilks K, Roland CL, Elam LC, et al. An intervention study on screening for breast cancer among single African-American women aged 65 and older. Prev Med. 2002;34:536–45. doi: 10.1006/pmed.2002.1016. [DOI] [PubMed] [Google Scholar]
- 56.Dailey AB, Kasl SV, Holford TR, Calvocoressi L, Jones BA. Neighborhood-level socioeconomic predictors of nonadherence to mammography screening guidelines. Cancer Epidemiol Biomarkers Prev. 2007;16:2293–303. doi: 10.1158/1055-9965.EPI-06-1076. [DOI] [PubMed] [Google Scholar]
- 57.Fowler BA. The influence of social support relationships on mammography screening in African-American women. J Natl Black Nurses Assoc. 2007;18:21–9. [PubMed] [Google Scholar]
- 58.Dolan NC, Reifler DR, McDermott MM, McGaghie WC. Adherence to screening mammography recommendations in a university general medicine clinic. J Gen Intern Med. 1995;10:299–306. doi: 10.1007/BF02599947. [DOI] [PubMed] [Google Scholar]
- 59.Marwill SL, Freund KM, Barry PP. Patient factors associated with breast cancer screening among older women. J Am Geriatr Soc. 1996;44:1210–4. doi: 10.1111/j.1532-5415.1996.tb01371.x. [DOI] [PubMed] [Google Scholar]
- 60.Champion VL. Beliefs about breast cancer and mammography by behavioral stage. Oncol Nurs Forum. 1994;21:1009–14. [PubMed] [Google Scholar]
- 61.Russell KM, Monahan P, Wagle A, Champion V. Differences in health and cultural beliefs by stage of mammography screening adoption in African American women. Cancer. 2007;109(2 Suppl):386–95. doi: 10.1002/cncr.22359. [DOI] [PubMed] [Google Scholar]
- 62.Menon U, Champion V, Monahan PO, Daggy J, Hui S, Skinner CS. Health belief model variables as predictors of progression in stage of mammography adoption. Am J Health Promot. 2007;21:255–61. doi: 10.4278/0890-1171-21.4.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Brenes GA, Skinner CS. Psychological factors related to stage of mammography adoption. J Womens Health Gend Based Med. 1999;8:1313–21. doi: 10.1089/jwh.1.1999.8.1313. [DOI] [PubMed] [Google Scholar]
- 64.Lauver DR, Henriques JB, Settersten L, Bumann MC. Psychosocial variables, external barriers, and stage of mammography adoption. Health Psychol. 2003;22:649–53. doi: 10.1037/0278-6133.22.6.649. [DOI] [PubMed] [Google Scholar]
- 65.Champion VL, Springston J. Mammography adherence and beliefs in a sample of low-income African American women. Int J Behav Med. 1999;6:228–40. doi: 10.1207/s15327558ijbm0603_2. [DOI] [PubMed] [Google Scholar]
- 66.Skinner CS, Arfken CL, Sykes RK. Knowledge, perceptions, and mammography stage of adoption among older urban women. Am J Prev Med. 1998;14:54–63. doi: 10.1016/s0749-3797(97)00008-1. [DOI] [PubMed] [Google Scholar]


