Abstract
Background The etiology, demographics, fracture site in facial injury patients have been reported worldwide. However, few studies have attempted to identify changes in maxillofacial fractures over time periods and between countries. The statistics are vastly different due to variations in social, environmental, and cultural factors.
Methods Data were collected from departmental records between 1996 and 2006 for patients treated at Christchurch Hospital for facial fractures. Variables examined included incidence, demographics, site of fracture, and treatment methods.
Results A total of 2563 patients presented during the study period, 1158 patients in the first half and 1404 patients in the second half. Male-to-female ratio was 4:1 in both periods and males in 16- to 30-year group accounted for about half of all patients. Interpersonal violence was the most common cause of injuries, and there was a decrease in injuries caused by motor vehicle accidents. Approximately half of all patients required hospitalization and surgery, and the most common method of treatment was open reduction and internal fixation.
Conclusion Maxillofacial fracture is a common injury in young males following interpersonal violence in New Zealand. Studies in other countries and over different time periods yield interesting differences in the etiology, demographics, and fractures patterns. These are due to environmental, societal, cultural, and legislative differences.
Keywords: maxillofacial, facial, fracture, epidemiology, trend
Trauma is a major health hazard associated with significant morbidity and mortality. Victims of facial injuries can sustain scars or disfigurements, with their resultant emotional and psychological impact.1 Psychological impairment such as posttraumatic stress syndrome and depression are common after sustaining facial injuries.1,2 Maxillofacial injury is also associated with high socioeconomic cost due to the increasing cost of hospital resource as well as time lost to work.
Epidemiological studies of maxillofacial injuries are numerous in the trauma, surgical, dental, and medical literature globally. Such data are specific to different parts of the world, different countries, and even different regions of the same country due to the environmental, socioeconomic, and cultural and lifestyle differences.3,4 Examples of such differing epidemiology of facial trauma include the higher incidence of sports-related facial injuries in regions with higher participation of heavy contact sports such as rugby5 and the increased proportion of violence-related trauma in the lower socioeconomic areas.3
Trauma epidemiology varies between time periods not only due to population and societal changes but also due to legislative changes. Introduction of compulsory safety belt legislation has led to a significant reduction in motor vehicle accidents (MVA) in past decades.6 The incidence of MVA is further reduced in regions that enforce speed limits. Another example of the impact of legislative change on health is the effect of lowering the legal drinking age and an increase in youth alcohol-related traffic crash trauma.7
Epidemiological studies are a useful tool not only to identify the trauma burden but also to assist health care providers in planning resource allocation. Periodic examination of trauma data is important therefore in planning hospital workload and for government administrators to determine the funding allocations and for the health care providers to plan appropriate education and training of specific skills to deal with particular health problems. It is also important for the treating health care providers to refine treatment algorithms for patients with this type of injuries and for interested organizations to direct education in the prevention of such trauma and improvement in its management.
This study aims to identify the changing trend in the demographics, etiology, distribution, and treatment of maxillofacial injuries in New Zealand over an 11-year period. Comparisons will be drawn between our results and those reported in the English literature.
Materials and Methods
This study reviews patients treated at the Oral and Maxillofacial Surgery unit at Christchurch Hospital in New Zealand between January 1996 and December 2006. Information was collected on variables including demographics, diagnosis, mode of injury, fracture site, and treatment approach. A total of 2581 patients were treated during the study period with radiographically confirmed maxillofacial fractures.
Results
Trend
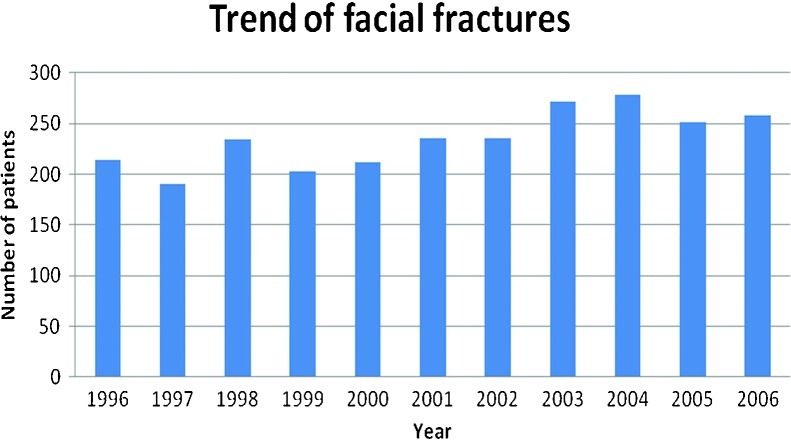
The number of facial fractures per annum over the study period is outlined in Fig. 1. There was an increase in the number of fractures between the two 5.5-year study periods, from 1171 patients in the first period to 1410 in the second, an increase of 20% in number.
Figure 1.
Yearly distribution of fractures.
Demographics
The patients at the time of injury ranged from 1 to 90 years (a mean age of 32 years) in the first half and from 1 to 95 years (a mean age of 27 years) in the second half. A high proportion of patients were males (82.2% in first half and 80.6% in second half; Table 1). The 16- to 30-year age group accounted for 56.6% of all patient in first period and 49.9% in second period (Table 2). the proportion of patients in the 46- to 60-year age group increased from 7.5 to 11.7%.
Table 1. Distribution of Overall Fractures According to Age and Gender.
| Gender | First Half | Second Half |
|---|---|---|
| Male | 962 (82.2) | 1132 (80.6) |
| Female | 208 (17.8) | 273 (19.4) |
| Total | 1170 (100) | 1405 (100) |
Table 2. Distribution of Overall Fractures According to Age and Gender.
| Age (y) | First Half | Second Half |
|---|---|---|
| <16 | 89 (7.9) | 89 (6.4) |
| 16–30 | 634 (56.6) | 696 (49.9) |
| 31–45 | 235 (21.0) | 312 (22.3) |
| 46–60 | 84 (7.5) | 163 (11.7) |
| 61–75 | 79 (7.0) | 135 (9.7) |
| Total | 1121 (100) | 1395 (100) |
Etiology
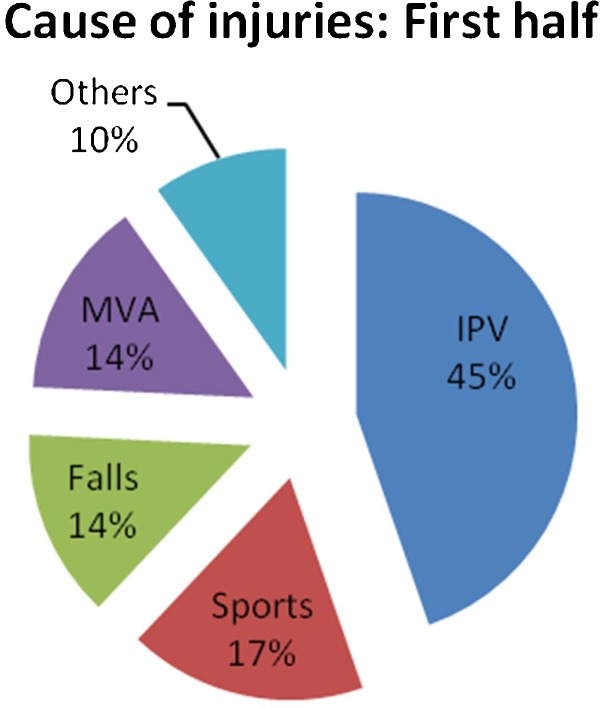
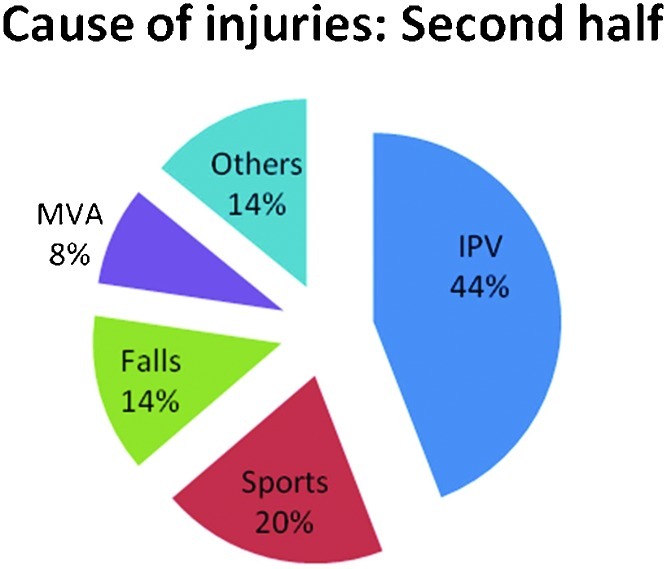
Interpersonal violence (IPV) was the main cause of facial fractures in both periods (Figs. 2 and 3). Although falls and sports accounted for similar proportion of injuries over the study periods, the proportion of patients with MVA-related injuries decreased.
Figure 2.
Causes of injuries: first half. IPV, interpersonal violence; MVA, motor vehicle accident.
Figure 3.
Causes of injuries: second half. IPV, interpersonal violence; MVA, motor vehicle accident.
Site of Fractures
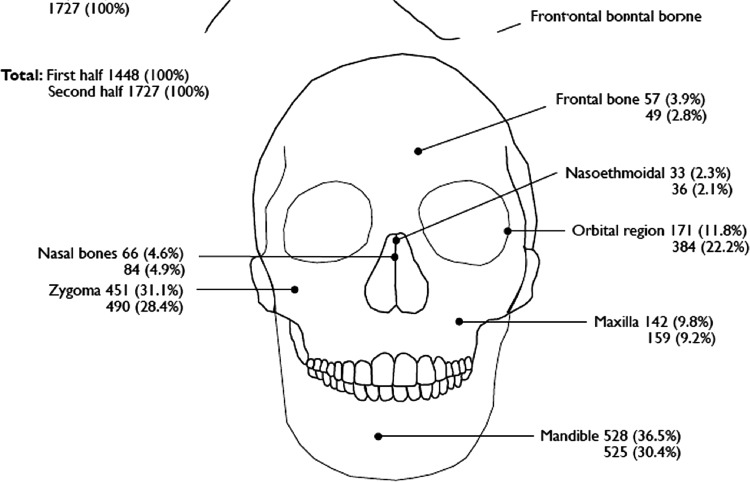
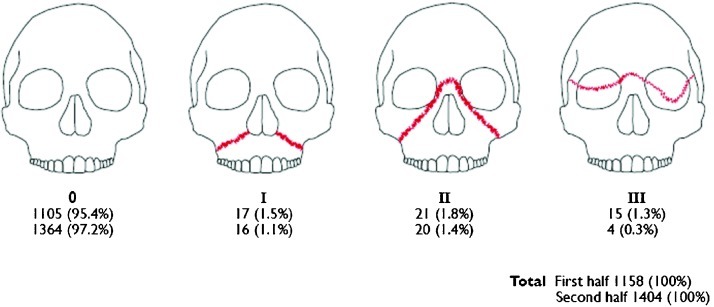
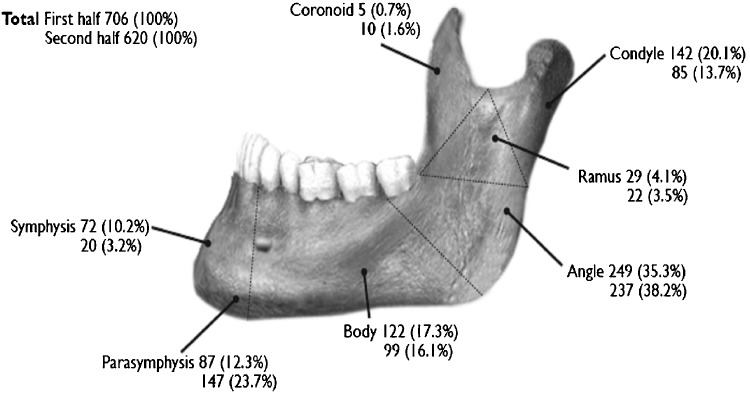
Figure 4 illustrates distribution of fracture at each site in terms of the total number of fractures and proportion of patients with the fractures. The mandible is the most frequently fractured bone in both time periods (36.5% and 30.4%, respectively). Zygoma was the most common midface bone affected (31.1% and 28.4%), followed by the orbital wall (11.8% and 22.2%). LeFort fractures were noted in 4% of patients (Fig. 5). Although the proportion of patients with LeFort I and LeFort II pattern fractures remained similar in both periods, there was a fourfold decrease in the number of patients with LeFort III fractures.
Figure 4.
Facial fracture distribution.
Figure 5.
LeFort fracture distribution.
In the mandible, the angle was the most commonly involved site (35.3% and 38.2%; Fig. 6). The mandibular fracture sites with the greatest change over the time periods were the symphysis (decreased from 10.2 to 3.2%) and the parasymphyseal region (increased from 12.3 to 23.7%).
Figure 6.
Mandibular fracture distribution.
Management
A similar proportion of patients required surgery following their injuries over the two study periods (Table 3). Of the patients who had surgery, approximately a third of all patients had open reduction of the fractures and internal fixation with miniplates and screws in each period (Table 4). There was a decrease in proportion of patients who received closed reduction of fractures (4.4 to 2.7%) and an increase in the need for orbital reconstruction (1.0 to 5.5%).
Table 3. Need for Surgery.
| Surgery | First Half | Second Half |
|---|---|---|
| Yes | 608 (52.7) | 705 (50.8) |
| No | 530 (46.0) | 641 (46.2) |
| Othersa | 15 (1.3) | 42 (3.0) |
| Total | 1153 (100) | 1388 (100) |
Includes nonattenders and no follow-up data.
Table 4. Methods of Treatment.
| Method of Treatment | First Half (%) | Second Half (%) |
|---|---|---|
| Conservative | 530 (46.0) | 641 (46.2) |
| Surgical | ||
| ORIF | 446 (38.7) | 507 (36.5) |
| Open reduction | 99 (8.6) | 85 (6.1) |
| Closed reduction | 51 (4.4) | 37 (2.7) |
| Orbital reconstruction | 12 (1.0) | 76 (5.5) |
| Othersa | 15 (1.3) | 42 (3.0) |
| Total | 1153 (100) | 1388 (100) |
Includes nonattenders and no follow-up data.
Alcohol Involvement
In both time periods, 59% of patients with alcohol involvement were males in the 16- to 30-year-old group (Table 5). Males in the 31- to 45-year-old group also accounted for a high proportion of patients with alcohol involvement (20.2% and 19.3%).
Table 5. Alcohol Involvement.
| First Half | Second Half | |||
|---|---|---|---|---|
| Age (y) | Male, n (%) | Female, n (%) | Male, n (%) | Female, n (%) |
| <16 | 11 (1.8) | 6 (1.0) | 8 (1.3) | 1 (0.2) |
| 16–30 | 359 (59.3) | 40 (6.6) | 370 (59.0) | 35 (5.6) |
| 31–45 | 122 (20.2) | 14 (2.3) | 121 (19.3) | 21 (3.3) |
| 46–60 | 34 (5.6) | 8 (1.3) | 45 (7.2) | 14 (2.2) |
| 61–75 | 10 (1.7) | 1 (0.2) | 8 (1.3) | 4 (0.6) |
| Total | 536 (88.6) | 69 (11.4) | 552 (88.0) | 75 (12.0) |
Discussion
Annual Variation in the Number of Cases
There was a 20% increase in patient number over the two halves of this study, similar to previous New Zealand studies during different study periods.8,9 Studies in other developed countries have found a similar rising trend.10,11,12 Table 6 compares data from past studies.
Table 6. Data from Past Studies.
| Study | Country | Study Period | Common Age (y) | Gender | Etiology (%) | Bone (%) | Treatment |
|---|---|---|---|---|---|---|---|
| Present study | New Zealand | 1996–2006 | 16–30 | 8:2 | IPV 44, sports 18, falls 14 | Mandible 40, zygoma 27, orbital floor 13 | Conservative 45%, ORIF 37% |
| Van Hoof et al 197722 | Netherlands | 1960–1974 | 11–20, 21–30 | 3:1 | RTA 66, falls 13, IPV 8, sports 9 | Md 45, Mid third 44, combo 11 | |
| Van Beek and Merkx 199921 | Denmark | 1960–1974, 1975–1987 | 11–20, 21–30 | 3:1 | Varies | Varies | |
| Afzelius and Rosén 198029 | Sweden | 1969–1976 | 20–29 | 4:1 | RTA 34.8, IPV 27.1, sports 12.8 | ZMC 45, Md 32, Orbit 7, Mx 6 | 12% nonsurgical |
| Zachariades and Papavassiliou 199040 | Greece | 1969–1984 | 21–30 | 3:1 | RTA 57, falls 20, IPV 9, industrial 5, sports 4 | Md 67.1, ZMC 15.6, alveolar 6.3, Mx 6 | |
| Sinclair 197920 | New Zealand | 1974–1978 | 20–29 (39.5%) | 4:1 | IPV 31, RTA 27, sports 20, falls 10, rugby 75 of sports | Md 53, malar 34, Mx 7, combo 6 | |
| Tanaka et al 199411 | Japan | 1977–1989 | 20–29 (30%) | 3.2:1 | RTA 38.4, falls 20, sports 10, IPV 9 | Md 68.6, Mx 6.6, zygoma 4.9, alveolar 10.6, multiple 8.3 | Closed reduction 68.5% |
| Muraoka and Nakai 199812 | Japan | 1978–1992 | 10–29 | 7:3 | Falls 32, RTA 26, IPV 24 | Nasal 50, zygoma 18, Md 8, blowout 10, Mx 2.5 | |
| Kieser et al 20026 | New Zealand | 1979–1998 | 15–19 for F, 20–24 for M | 4:1 (78.9% male) | IPV, sports, RTA | Md 35, nasal 30, malar + mx 26 | |
| Koorey et al 199228 | New Zealand | 1979–1988 | 20–24 | 4:1 | IPV, sports, RTA | ||
| Hammond et al 19918 | New Zealand | 1979–1985 | 20–29 | IPV 32.4, RTA 29.6, sports 19.6, rugby 58.4 | Md 42.8, ZMC 41.6, maxilla 6.2, nasoeth 5.8, orbit 3.5 | ||
| Kontio et al 200510 | Finland | 1981 or 1997 | 31–40 | 3:1 | IPV 42, RTA 26, falls 13, | ||
| Ugboko et al 199844 | Nigeria | 1982–1995 | 21–30 (39.1) | 4.1:1 | RTA 71.9, falls 10.9, IPV 8.4, sports 3.2 | Md 64, Mx 20.8, zygoma 12 | |
| Beck and Blakeslee 198913 | United States | 1983–1987 | 20–30 (65%) | 7.7:1 | IPV35.1, RTA 26.3, sports 12.2, falls 8.8 | Md, zygoma, mx | |
| Timoney et al 199039 | France versus United Kingdom | 1985–1986 | 75% male | ||||
| Oji 199934 | Nigeria | 1985–1995 | 21–30 (35.5) | 3:1 | RTA 83, IPV 7.4, sports and work 4 | Md 53.4, Mid 26.6 | |
| Chan et al 199238 | Hong Kong | 1985–1991 | 20–29 | 76 male | Falls 31, RTA 30, IPV 20, industrial 12, sports 3 | Md 71, Mx 13, zygoma 13 | |
| Bamjee et al 199637 | South Africa | 1989–1992 | 13–18 (70) | 2.3:1 | IPV, RTA | Md 64 | |
| Buchanan et al 20059 | New Zealand | 1989–2000 | 15–24 | 4:1 | IPV 36.2, RTA 24.4, sports 18.3, falls 11.1, | Md 52.6, zygoma 33.4, alveolar 6, maxilla 5.4, orbit 5.1 | |
| Ashar et al 199927 | United Arab Emirates | 1990–1995 | 21–30 (high % young in 16 to 20) | 6.6:1 | RTA 60, falls 11, work 8, sports 7, IPV 6 | Md 45, midface 36 | |
| Bataineh 199833 | Jordan | 1992–1997 | 20–29 (31.8%) | 3:1 | RTA 55.2, fall 19.7, IPV 16.9, sports 6 | Md 74.4, Mx 13.5, ZMC 10.7 | |
| Gassner et al 200341 | Austria | 1991–2000 | 10–37 | 2:1 | Falls and daily life 38, sports 31, IPV 12, RTA 12, work 5 | Midface 71.5, Md 24.3, frontal 4.2 | |
| Olasoji et al 200226 | Nigeria | 1996–1999 | 20–29 | 2:1 | IPV 48, RTA 36, fall 9, sports 4 | Md 66, Mid 27 | |
| Motamedi 200330 | Iran | 1996–2001 | 20–29 | 89% male | RTA 54, falls 20.3, IPV 9.7, sports 6.3 | Md 72.9, Mx 13.9, zygoma 13.5, zygoma + orbit 24 | |
| Deogratius et al 200636 | Tanzania | 1998–2003 | 20–29 | 3:1 | IPV 57.6, falls 19.7, RTA 13.7, sports 8 | Md 70.7 | |
| Al Ahmed et al 200425 | United Arab Emirates | 1999–2000 | 20–29 (39%) | 92% male | RTA 75, falls 12, IPV 8, sports 2.6 | Md 51, Mx 34, zygoma 7, orbit 6 | |
| Brasileiro and Passeri 20063 | Brazil | 1999–2004 | 21–30 | 4:1 | RTA 46.2 male 40.3 female, IPV 23.9 male, falls 34 female | Md 44.2, ZMC 32.5 | |
| Montovani et al 200624 | Brazil | 1991–2004 | 20–29 | 84.9% men | RTA 33, IPV 25, fall 17.2, sports 5.3 | Md 35, zygoma 24, nasal 23 | |
| Hogg et al 200018 (severe only) | Canada | 1992–1997 | 25–34 | 3:1 | MVA 70 | Mx 23, orbit 22, | |
| Alvi et al 200343 (severe only) | United States | 1996–2000 | 87.4% male | IPV 41, MVA 26.5 | Orbit 24.2, Mx 22, nose 19.2, | ||
| Moosa et al 200445 | Tehran | 1999–2000 | 21–30 (81.8) | 4.5:1 | RTA 68.5, fall 20, IPV 9.2 | Md, nose | |
| Kadkhodaie 200631 | Iran | 2001–2004 | 20–29 | 12:1 | RTA 91, falls 5.5, IPV 2.9, sports + other 0.6 | ||
| Malara et al 200617 | Poland | 2001–2005 | 18–25 | 62.6% male | IPV 51.7, RTA 19.3, falls 14.8, sports 8.2 | Md 18.7, ZMC, Mx, Nose, orbit |
IPV, interpersonal violence; RTA, road traffic accidents; MVA, motor vehicle accidents; ORIF, open reduction and internal fixation; ZMC, zygomaticomaxillary complex; Md, mandible; Mx, maxilla; nasoeth, nasoethmoidal complex.
Other studies have found a decrease in the number of fractures over consecutive time periods. This is believed to be due to the significant decrease in road traffic accidents (RTA) over recent times, according to one U.S. study between 1983 and 198713 and a New Zealand study between 1979 and 1998.6 This is supported by other studies that found that severe maxillofacial trauma, which often occurs as a result of RTA, decreased significantly over last three decades.14,15
There is no definite trend in seasonal variation. One would expect more facial fractures arising from an increase in number of RTAs in winter due to hazardous conditions. In contrast, studies in Poland and Brazil reported more facial fractures during spring16,17 due to good driving conditions in spring leading to higher driving speeds. Another study also found high number of injuries in summer.18
Fridays, Saturdays, and Sundays are the most common days for presentation of facial fractures.8,16,18,19 Social activities usually take place during the weekend where alcohol is likely to be involved.9
Age and Sex Distribution
This study found consistently high incidence of injuries in the 16- to 30-year-old age group and an increasing proportion of older patients. A New Zealand study reported a 15% increase in fractures in the 12- to 30-year age group from 1961 to 1979.20 In most Western societies, the 20- to 29-year-old age group seems to have the highest incidence of facial fractures; one Danish study reported an equal incidence in the 11- to 20-year and 20- to 29-year groups,21 and a Dutch study found a similarly high number of young patients, which observed a large number of moped accidents.22
There is also an increase in the average age of patients presenting with maxillofacial injuries; In Finland the most affected age group increased from 31 to 40 years to 41 to 50 years over the 16-year study period.10 This is believed to be due to an increase in life expectancy of people worldwide and a resultant increase in number of older people sustaining maxillofacial injuries.23
Maxillofacial fractures occur more commonly in males and most Western studies report a male-to-female ratio between 3:1 and 4:1. Females are increasingly more involved as observed in studies in the last three decades.12,24
In contrast, in Middle Eastern countries males still account for a significantly higher proportion of facial fracture injuries with ratios ranging from 4.5:1 to 12:1 (25 to 29). In the Middle East, males usually carry out outdoor work and females work mainly as teachers, nurses, and doctors and only a minority drive cars.25 There is a recent trend that more women are involved in outdoor economic activities to earn money due to economic recession, exposing them to various hazards.26
The gender ratio in facial trauma also changes depending on the cause. For example, males account for a higher proportion for assaults (5.5:1), although less for falls (1:1).10 RTA is leading cause of fractures for females.9 Males are more likely to be involved in severe trauma.14,15,18
In the United Arab Emirates, children account for an unusually high percentage of facial fractures (12.1%).25,27 The suggested reason for this is that children are more likely to be unrestrained passengers in MVA.
The incidence of facial fractures is higher in certain ethnic groups. Koorey et al found an overall decrease in incidence of facial fractures over the study period but an increase for indigenous population.28 Buchanan et al found 32% of all facial fractures between 1989 and 2000 occurred in the indigenous Maori group.9 Similarly, Kruger et al reported that the indigenous population accounted for a disproportionately high number of fractures.19
Etiology
It has been noted that the common causes for facial fractures vary from region to region, and less so from time period to time period.12 This study reported that the causes of facial fractures across the two study periods have not differed significantly, with the exception of MVA. Overall causes in maxillofacial injuries did not change from 1981 to 1997 in Finland,10 although MVA decreased from 50 to 20%. Complex fractures caused by RTA decreased from 1969 to 1976 in one study.29 Another study also reported a decrease in RTA from 1960 to 1987, and the incidence of IPV doubled and sports and falls also increased.21
The incidence of RTAs is much higher in developing countries, ranging from 55.2 to 91%.24,27,30,31,32,33,34 This may be due to the fact that in developing countries traffic law enforcement is not as strict, seat belts are not compulsory, vehicles are poorly maintained with minimal safety features, and protective gear such as helmets are less prevalently used.35
In later African studies, IPV overtook RTA as the leading cause of maxillofacial fractures.26,36 IPV is reported to be more common in males whereas RTA more common in females.37 Motorbike and bicycle accidents made up the majority of RTA in Brazil.3,16 In contrast, highly populated regions such as India and Hong Kong have more pedestrian versus car accidents.35,38
Conversely in Western society, there is a downward trend in the incidence of RTA-related facial fractures, and IPV has become the leading cause. In Denmark, there was a decrease in RTA from 1960 to 1987, and the incidence of IPV doubled.21 In Sweden, the number of complex maxillofacial fractures caused by RTA decreased from 1969 to 1976.29 Similar findings have been reported in the United Kingdom and France,39 Finland,10 and New Zealand.8,15,20 Effective drink driving campaigns have helped to decrease the incidence of RTA-related facial injuries but IPV is becoming more predominant. This may be a result of the increasing social acceptance, or overindulgence, of alcohol.9 In Islamic countries where alcohol is forbidden, IPV is less frequently associated with maxillofacial injuries.31 Factors such as the declining economic outlook leading to unemployment can also increase social violence.
Interestingly, in Asian countries the incidence of IPV is lower than that of RTA. This is noted in Hong Kong, a developed country, which has a high number of pedestrian accidents as the majority of the population does no own cars.38 In Japan, falls followed RTA as the main cause and violence-related trauma was not common.11 Accidental falls are the second most common causative factor, which is believe to be due to the living environment including many steep slopes and steps.38 The trend of decreasing RTA and increasing IPV was not observed in Greece.40
Accidental falls occur more commonly in the young and older age groups, and there has been an increase in the number of maxillofacial injuries reported due to falls.9,24 As the population of the world becomes older due to an increase in life expectancy, this trend can be expected to continue.23 Play accidents dominate the first decade of life, and accidental falls become more common in older age groups.9,24,41
Sport is a major part of life in New Zealand culture, and a high proportion of injuries in this study arose from sport. Not surprisingly rugby has always been the main cause8,20 due to the popular and violent nature of the game. The nature of sports injuries depends on geography, for example, skiing in Austria41 and soccer in France.42
Work-related accidents are caused mainly by industrial trades involving mechanical equipment. A high proportion of work-related injuries are due to the construction trade.18 A New Zealand study reported a decrease in industrial work-related facial fractures likely due to increase in safety and automation of machinery.20
Fracture Site
Fracture of the mandible is the most common facial bone fracture reported in the literature. Geographical variations do exist and the mechanism of injury may be responsible for this difference. In general, there is a dominance of angle fractures. A greater number of angle fractures are seen in IPV due to the way the jaw is struck.25 Furthermore, the left side is affected more commonly than the right side due to the way in which right-handed assailants strike the victims.8
Fractures of the mandibular condyles are more commonly reported in some European countries.21,22,29 Condyle fractures occur more frequently in children from falls (result of collision to the chin point) and mandibular body fractures are more commonly observed in IPV-related injuries.30 A Hong Kong study reported a large number of condylar fractures, due to a high incidence of falls-related injuries in this series.38
Several studies from United Arab Emirates, Jordan, Nigeria, and Iran reported a high incidence of fractures of the anterior and body of the mandible.26,31,32,33,34 RTA is the main causative factor in these studies, and the high velocity and impact injury mechanism, particular in the absence of the shock-absorbing effect of airbags, explains the high frequency of anterior and body of mandible fractures.
Midface fractures are common in RTA. Multiple fractures involving the zygoma and orbit occur more often than mandibular fractures alone in severe facial injuries.18,43 There is evidence that a decline in RTA over the last decades has led to a decrease in the number of complex midface injuries.15,21,29 Zygoma fractures were reported to occur more frequently in older patients than mandibles.16
Treatment
Patients with mandibular fractures were predominantly treated with closed reduction in developing countries before the year 2000 (82.3 to 98%).27,32,33 Limitations to open reduction and internal fixation (ORIF) with miniplates and screws include the high cost of internal fixation equipment as well as a lack of training.
However, after 2000 there is a notable move to ORIF, in particular for mandibular fractures.25,30,31 The proportion of patients treated with closed reduction decreased to 67% of all cases and ORIF increased to 49.1% of cases in one study25; another study reported 56.9% of mandibular fractures treated by closed reduction and 54.6% of maxillary fractures treated by closed reduction.30
Recent New Zealand data reported that one-third of fractures were conservatively treated (29% of mandibular, 55% of zygoma, and 59% of nasal fractures).9 This study found almost half of all patients were treated conservatively, which suggest the undisplaced nature of some of these fractures
Alcohol as a Contributing Factor
Excessive consumption of alcohol is found to be strongly associated with facial injuries in previous studies as it can impair judgment and fuel violence.9,43 There has been strong pressure by the New Zealand government through advertisement and television to outlaw drunk drivers and enforce regulation. A law was passed in New Zealand in 1998 to lower the legal age for purchase of alcohol, which has been condemned by some groups as the lowering of age can potentially lead to immature and irresponsible drinking.
A Brazilian study reported that 38% of RTA-related and 58% of IPV-related injuries had alcohol involvement minutes or hours prior to the accident.24 Another study found that 32.4% of major maxillofacial trauma involved alcohol.43 Alcohol is a major factor in facial injuries, and the majority of the injuries involve young men.13,18 Interestingly, alcohol was only involved in 3% of patients in one Hong Kong study, which also reported low incidence of IPV-related injuries.38
In the Middle East, fractures associated with alcohol abuse were rarely reported due to strict laws governing sale and consumption of alcohol and religious beliefs prohibiting consumption of alcohol.25
Postoperative Complication
Incidence of posttreatment complications was not frequently reported in the literature. Infection was the most commonly reported complication, with incidence ranging from 3.7 to 5%.3,30 Less common complications include malunion of fractures, malocclusion, and temporomandibular joint disorder.25,32
Conclusion
Maxillofacial fracture is a common injury presenting to the emergency department. There is a changing trend in the demographics, pattern of fractures, and treatment philosophy in managing these patients over time periods. The variations extend across time and geographic boundaries.
References
- 1.Joy D, Probert R, Bisson J I, Shepherd J P. Posttraumatic stress reactions after injury. J Trauma. 2000;48:490–494. doi: 10.1097/00005373-200003000-00020. [DOI] [PubMed] [Google Scholar]
- 2.Shepherd J. Victims of personal violence: the relevance of Symond's model of psychological response and loss theory. Br J Soc Work. 1990;20:309–332. [Google Scholar]
- 3.Brasileiro B F, Passeri L A. Epidemiological analysis of maxillofacial fractures in Brazil: a 5-year prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:28–34. doi: 10.1016/j.tripleo.2005.07.023. [DOI] [PubMed] [Google Scholar]
- 4.Haug R H, Prather J, Indresano A T. An epidemiologic survey of facial fractures and concomitant injuries. J Oral Maxillofac Surg. 1990;48:926–932. doi: 10.1016/0278-2391(90)90004-l. [DOI] [PubMed] [Google Scholar]
- 5.West P, Reeder A I, Milne B J, Poulton R. Worlds apart: a comparison between physical activities among youth in Glasgow, Scotland and Dunedin, New Zealand. Soc Sci Med. 2002;54:607–619. doi: 10.1016/s0277-9536(01)00055-7. [DOI] [PubMed] [Google Scholar]
- 6.Kieser J, Stephenson S, Liston P N, Tong D C, Langley J D. Serious facial fractures in New Zealand from 1979 to 1998. Int J Oral Maxillofac Surg. 2002;31:206–209. doi: 10.1054/ijom.2002.0208. [DOI] [PubMed] [Google Scholar]
- 7.Kypri K, Voas R B, Langley J D. et al. Minimum purchasing age for alcohol and traffic crash injuries among 15- to 19-year-olds in New Zealand. Am J Public Health. 2006;96:126–131. doi: 10.2105/AJPH.2005.073122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hammond K L, Ferguson J W, Edwards J L. Fractures of the facial bones in the Otago region 1979–1985. N Z Dent J. 1991;87:5–9. [PubMed] [Google Scholar]
- 9.Buchanan J, Colquhoun A, Friedlander L, Evans S, Whitley B, Thomson M. Maxillofacial fractures at Waikato Hospital, New Zealand: 1989 to 2000. N Z Med J. 2005;118:U1529. [PubMed] [Google Scholar]
- 10.Kontio R, Suuronen R, Ponkkonen H, Lindqvist C, Laine P. Have the causes of maxillofacial fractures changed over the last 16 years in Finland? An epidemiological study of 725 fractures. Dent Traumatol. 2005;21:14–19. doi: 10.1111/j.1600-9657.2004.00262.x. [DOI] [PubMed] [Google Scholar]
- 11.Tanaka N, Tomitsuka K, Shionoya K. et al. Aetiology of maxillofacial fracture. Br J Oral Maxillofac Surg. 1994;32:19–23. doi: 10.1016/0266-4356(94)90166-x. [DOI] [PubMed] [Google Scholar]
- 12.Muraoka M, Nakai Y. Twenty years of statistics and observation of facial bone fracture. Acta Otolaryngol Suppl. 1998;538:261–265. doi: 10.1080/00016489850183043. [DOI] [PubMed] [Google Scholar]
- 13.Beck R A, Blakeslee D B. The changing picture of facial fractures. 5-Year review. Arch Otolaryngol Head Neck Surg. 1989;115:826–829. doi: 10.1001/archotol.1989.01860310064024. [DOI] [PubMed] [Google Scholar]
- 14.Down K E, Boot D A, Gorman D F. Maxillofacial and associated injuries in severely traumatized patients: implications of a regional survey. Int J Oral Maxillofac Surg. 1995;24:409–412. doi: 10.1016/s0901-5027(05)80469-2. [DOI] [PubMed] [Google Scholar]
- 15.Adams C D, Januszkiewcz J S, Judson J. Changing patterns of severe craniomaxillofacial trauma in Auckland over eight years. Aust N Z J Surg. 2000;70:401–404. doi: 10.1046/j.1440-1622.2000.01836.x. [DOI] [PubMed] [Google Scholar]
- 16.Chrcanovic B R, Freire-Maia B, Souza L N, Araújo V O, Abreu M H. Facial fractures: a 1-year retrospective study in a hospital in Belo Horizonte. Braz Oral Res. 2004;18:322–328. doi: 10.1590/s1806-83242004000400009. [DOI] [PubMed] [Google Scholar]
- 17.Malara P, Malara B, Drugacz J. Characteristics of maxillofacial injuries resulting from road traffic accidents—a 5 year review of the case records from Department of Maxillofacial Surgery in Katowice, Poland. Head Face Med. 2006;2:27–32. doi: 10.1186/1746-160X-2-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hogg N J, Stewart T C, Armstrong J E, Girotti M J. Epidemiology of maxillofacial injuries at trauma hospitals in Ontario, Canada, between 1992 and 1997. J Trauma. 2000;49:425–432. doi: 10.1097/00005373-200009000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Kruger E, Smith K, Tennant M. Jaw fractures in the indigenous and non-indigenous populations of Western Australia: 1999–2003. Int J Oral Maxillofac Surg. 2006;35:658–662. doi: 10.1016/j.ijom.2006.01.019. [DOI] [PubMed] [Google Scholar]
- 20.Sinclair J H. The changing pattern of maxillo-facial injuries. Ann R Australas Coll Dent Surg. 1979;6:43–49. [PubMed] [Google Scholar]
- 21.Beek G J van, Merkx C A. Changes in the pattern of fractures of the maxillofacial skeleton. Int J Oral Maxillofac Surg. 1999;28:424–428. doi: 10.1034/j.1399-0020.1999.280605.x. [DOI] [PubMed] [Google Scholar]
- 22.Hoof R F van, Merkx C A, Stekelenburg E C. The different patterns of fractures of the facial skeleton in four European countries. Int J Oral Surg. 1977;6:3–11. doi: 10.1016/s0300-9785(77)80066-5. [DOI] [PubMed] [Google Scholar]
- 23.Thomson W M, Stephenson S, Kieser J A, Langley J D. Dental and maxillofacial injuries among older New Zealanders during the 1990s. Int J Oral Maxillofac Surg. 2003;32:201–205. doi: 10.1054/ijom.2002.0373. [DOI] [PubMed] [Google Scholar]
- 24.Montovani J C, de Campos L M, Gomes M A, de Moraes V R, Ferreira F D, Nogueira E A. Etiology and incidence facial fractures in children and adults. Braz J Otorhinolaryngol. 2006;72:235–241. doi: 10.1016/S1808-8694(15)30061-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Al Ahmed H E, Jaber M A, Abu Fanas S H, Karas M. The pattern of maxillofacial fractures in Sharjah, United Arab Emirates: a review of 230 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:166–170. doi: 10.1016/j.tripleo.2004.01.020. [DOI] [PubMed] [Google Scholar]
- 26.Olasoji H O, Tahir A, Arotiba G T. Changing picture of facial fractures in northern Nigeria. Br J Oral Maxillofac Surg. 2002;40:140–143. doi: 10.1054/bjom.2001.0716. [DOI] [PubMed] [Google Scholar]
- 27.Ashar A, Khateery S, Kovacs A. Etiology and patterns of facial fractures in Al-Ain, United Arab Emirates. Saudi Dent J. 1999;11:109–113. [Google Scholar]
- 28.Koorey A J, Marshall S W, Treasure E T, Langley J D. Incidence of facial fractures resulting in hospitalisation in New Zealand from 1979 to 1988. Int J Oral Maxillofac Surg. 1992;21:77–79. doi: 10.1016/s0901-5027(05)80535-1. [DOI] [PubMed] [Google Scholar]
- 29.Afzelius L E, Rosén C. Facial fractures. A review of 368 cases. Int J Oral Surg. 1980;9:25–32. doi: 10.1016/s0300-9785(80)80003-2. [DOI] [PubMed] [Google Scholar]
- 30.Motamedi M H. An assessment of maxillofacial fractures: a 5-year study of 237 patients. J Oral Maxillofac Surg. 2003;61:61–64. doi: 10.1053/joms.2003.50049. [DOI] [PubMed] [Google Scholar]
- 31.Kadkhodaie M H. Three-year review of facial fractures at a teaching hospital in northern Iran. Br J Oral Maxillofac Surg. 2006;44:229–231. doi: 10.1016/j.bjoms.2005.06.016. [DOI] [PubMed] [Google Scholar]
- 32.Ugboko V, Udoye C, Ndukwe K, Amole A, Aregbesola S. Zygomatic complex fractures in a suburban Nigerian population. Dent Traumatol. 2005;21:70–75. doi: 10.1111/j.1600-9657.2004.00275.x. [DOI] [PubMed] [Google Scholar]
- 33.Bataineh A B. Etiology and incidence of maxillofacial fractures in the north of Jordan. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86:31–35. doi: 10.1016/s1079-2104(98)90146-9. [DOI] [PubMed] [Google Scholar]
- 34.Oji C. Jaw fractures in Enugu, Nigeria, 1985–95. Br J Oral Maxillofac Surg. 1999;37:106–109. doi: 10.1054/bjom.1997.0083. [DOI] [PubMed] [Google Scholar]
- 35.Zargar M, Khaji A, Karbakhsh M, Zarei M R. Epidemiology study of facial injuries during a 13 month of trauma registry in Tehran. Indian J Med Sci. 2004;58:109–114. [PubMed] [Google Scholar]
- 36.Deogratius B K, Isaac M M, Farrid S. Epidemiology and management of maxillofacial fractures treated at Muhimbili National Hospital in Dar es Salaam, Tanzania, 1998–2003. Int Dent J. 2006;56:131–134. doi: 10.1111/j.1875-595x.2006.tb00084.x. [DOI] [PubMed] [Google Scholar]
- 37.Bamjee Y, Lownie J F, Cleaton-Jones P E, Lownie M A. Maxillofacial injuries in a group of South Africans under 18 years of age. Br J Oral Maxillofac Surg. 1996;34:298–302. doi: 10.1016/s0266-4356(96)90006-6. [DOI] [PubMed] [Google Scholar]
- 38.Chan S W Yan Y W Tsang C CA Incidence of maxillofacial trauma in the Hong Kong region Hong Kong Dent Assoc Bienn Report. 1992/93
- 39.Timoney N, Saiveau M, Pinsolle J, Shepherd J. A comparative study of maxillo-facial trauma in Bristol and Bordeaux. J Craniomaxillofac Surg. 1990;18:154–157. doi: 10.1016/s1010-5182(05)80510-4. [DOI] [PubMed] [Google Scholar]
- 40.Zachariades N, Papavassiliou D. The pattern and aetiology of maxillofacial injuries in Greece. A retrospective study of 25 years and a comparison with other countries. J Craniomaxillofac Surg. 1990;18:251–254. doi: 10.1016/s1010-5182(05)80425-1. [DOI] [PubMed] [Google Scholar]
- 41.Gassner R, Tuli T, Hachl O, Rudisch A, Ulmer H. Cranio-maxillofacial trauma: a 10 years review of 9,543 cases with 21,067 injuries. J Craniomaxillofac. 2003;31:51–61. doi: 10.1016/s1010-5182(02)00168-3. [DOI] [PubMed] [Google Scholar]
- 42.Maladière E, Bado F, Meningaud J P, Guilbert F, Bertrand J C. Aetiology and incidence of facial fractures sustained during sports: a prospective study of 140 patients. Int J Oral Maxillofac Surg. 2001;30:291–295. doi: 10.1054/ijom.2001.0059. [DOI] [PubMed] [Google Scholar]
- 43.Alvi A, Doherty T, Lewen G. Facial fractures and concomitant injuries in trauma patients. Laryngoscope. 2003;113:102–106. doi: 10.1097/00005537-200301000-00019. [DOI] [PubMed] [Google Scholar]
- 44.Ugboko V I, Odusanya S A, Fagade O O. Maxillofacial fractures in a semi-urban Nigerian teaching hospital. A review of 442 cases. Int J Oral Maxillofac Surg. 1998;27:286–289. doi: 10.1016/s0901-5027(05)80616-2. [DOI] [PubMed] [Google Scholar]
- 45.Zargar M, Khaji A, Karbakhsh M, Zarei M R. Epidemiology study of facial injuries during a 13 month of trauma registry in Tehran. Indian J Med Sci. 2004;58:109–114. [PubMed] [Google Scholar]