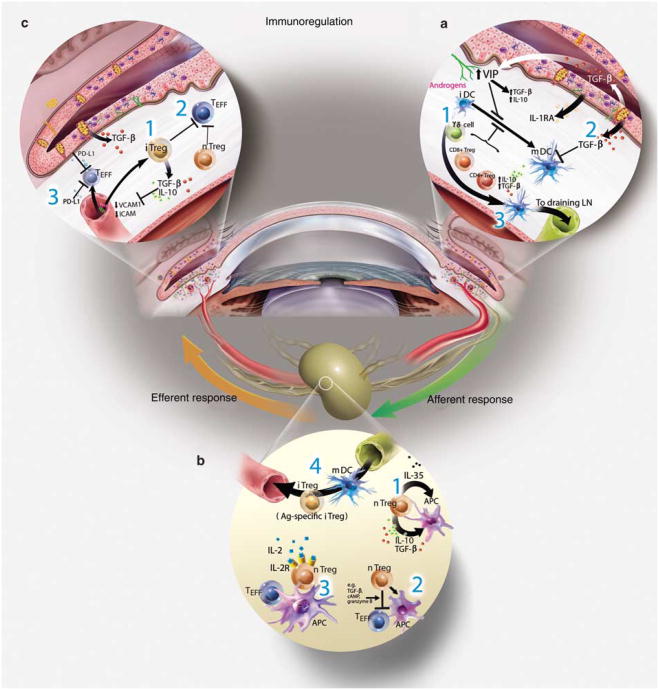
Figure 1.
Immunoregulation on the ocular surface: (a) the ocular surface tissues contain a variety of soluble and cellular factors to reduce inflammation-induced pathology in the lacrimal functional unit. Those implicated in immunoregulation within the ocular surface tissues include: (1) nTregs (e.g., CD4+, CD8+, γδ, and NKT cells), which include many of the conjunctival intraepithelial lymphocytes, are thought to dampen or inhibit the inflammatory/autoimmune response on the ocular surface. (2) The anti-inflammatory cytokine transforming growth factor (TGF)-β is present on the ocular surface, and has profound suppressive affects on resident dendritic cell (DC) maturation in the cornea, autoreactive T-cell proliferation, differentiation, and survival, and Treg differentiation and maintenance. The activity of the potent acute response proinflammatory cytokine interleukin (IL)-1 is modulated by the IL-1 receptor antagonist (IL-1RA), expressed and secreted by corneal and conjunctival epithelial cells. Vasoactive intestinal peptide (VIP) also seems to be protective; VIP secreted by sensory nerve endings in the cornea increases production of TGF-β and IL-10 and inhibits expression of the proinflammatory cytokines/chemokines, IL-1 β, tumor necrosis factor (TNF)-α, interferon (IFN)-γ, and CXCL2. Hormones are also implicated in curbing inflammation and maintaining homeostasis. In addition, the corneal epithelium also expresses vascular endothelium growth factor (VEGF) receptor-1 to sequester VEGF and reduce neovascularization. (3) APCs bearing self-antigen derived at the ocular surface may migrate to the regional lymph nodes to induce antigen-specific Tregs (iTregs). (b) Immunoregulation in the lymphoid organs: nTregs may exert their immunosuppressive function by (1) releasing soluble factors (e.g., TGF-β, IL-10), (2) cell–cell contact, which disables pathogenic effector T cells (Teff) and/or APCs, and/or (3) competing for soluble factors (e.g., IL-2). (4) Inducible Tregs (iTregs) may use similar mechanisms to inhibit cells bearing or responding to autoantigens. It is possible that these Treg-dependent mechanisms may also function within the ocular surface tissues. (c) Other peripheral immunoregulatory mechanisms: additional mechanisms also limit access and effector function of autoreactive T cells within the ocular surface tissues: (1) TGF-β and (2) nTregs and iTregs are suggested to suppress infiltrating autoreactive lymphocytes and (3) low-level expression of integrins in the healthy ocular surface endothelial cells, coupled with expression of the programmed death ligand-1 (PD-L1), negatively regulates activated T cells within the ocular surface tissues.