Abstract
Obstructive sleep apnea results from structural compromise of the upper airway and decreased muscle tone during sleep. Central sleep apnea is usually due to instability of the feedback mechanism of the body that controls respiration. While positional changes commonly affect the severity of obstructive sleep apnea, the effect of positional changes on the severity of central sleep apnea is less well known.
Citation:
Zaharna M; Rama A; Chan R; Kushida C. A case of positional central sleep apnea. J Clin Sleep Med 2013;9(3):265-268.
Keywords: Central sleep apnea, sleep position, sleep disordered breathing
Obstructive sleep apnea is characterized by repetitive partial (i.e., hypopnea) or total (i.e., apnea) obstruction of the upper airway with subsequent increased ventilatory effort (e.g., snoring, gasping, choking), resulting in cortical arousals and/or oxygen desaturations. Body position during sleep influences the frequency of apneas and hypopneas in 50% to 60% of individuals with obstructive sleep apnea (OSA).1–5 In such cases, the apnea-hypopnea index (AHI) is increased in the supine posture and reduced in the lateral posture. Positional sleep apnea is said to be present when there is a 50% reduction in the AHI during non-supine sleep.2,5,6
Central sleep apnea (CSA) is characterized by cessation of respiration due to repetitive lapses in ventilatory effort resulting in cortical arousals and/or oxygen desaturations. While positional changes commonly affect the severity of obstructive sleep apnea, the effect of positional changes on the severity of central sleep apnea has not been commonly described in the literature. Cheyne-Stokes Respiration (CSR), a specific form of central sleep apnea characterized by a cyclic crescendo and decrescendo breathing pattern, has been reported to be affected by body position during sleep.8–10 A recent study on patients with heart failure and CSR showed increasing severity of CSR in the supine position, with CSR becoming position-independent as cardiac dysfunction progressed.11
There are few reports in the literature of positional central sleep apnea in patients with no known cardiac history or congestive heart failure.12,13 We present a case of a healthy 29-year-old male with severe idiopathic central sleep apnea isolated to supine sleep that was successfully treated on continuous positive airway pressure (CPAP) therapy.
REPORT OF CASE
A 29-year-old male presented to his primary care doctor with a one-month history of fatigue. The patient is a shift worker and a truck driver, and he found himself tired and yawning while working. He also complained of occasional night time awakenings and snoring. The patient had not previously been seen by his primary care doctor, as he had always been healthy. A full physical examination and basic laboratory testing, including complete blood count, thyroid stimulating hormone, complete metabolic panel, lipid panel, and fasting blood sugar were normal. The patient had a slightly high blood pressure of 130/79 with pulse of 76. He was overweight with a BMI of 29. The patient was not on any medications and denied alcohol or illicit drug use. After a full medical and mental health history was obtained and appeared to be noncontributory, a sleep study was ordered.
The patient presented to our lab for a diagnostic polysomno-gram which showed the results reported in Table 1.
Table 1.
Results of diagnostic polysomnogram testing of patient present to the laboratory
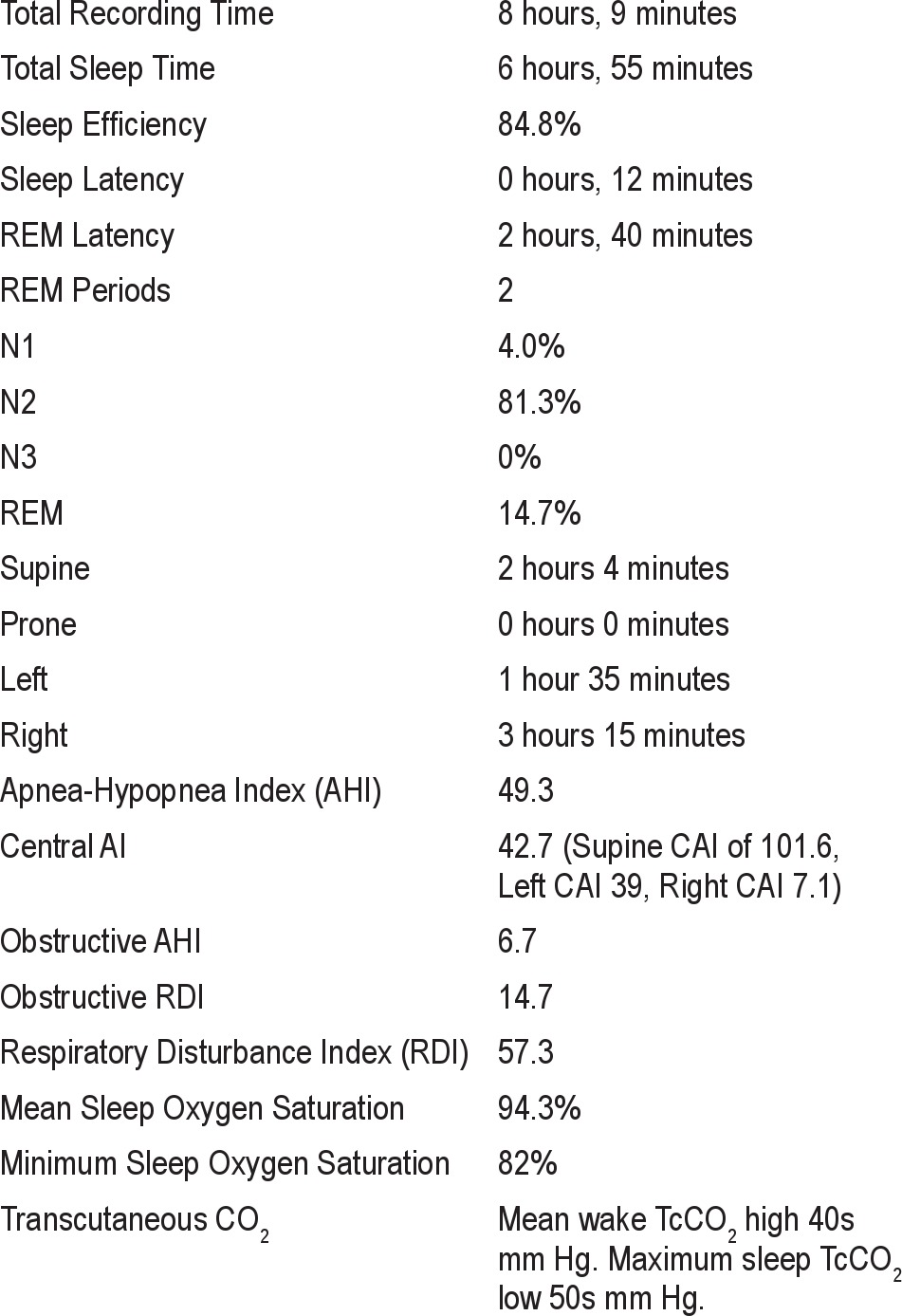
Electrocardiography showed sinus rhythm with one premature ventricular contraction noted. There were no periodic limb movements or unusual behaviors noted, apart from occasional somniloqui. The patient was urged to return for an overnight CPAP and bilevel titration with servoventilation on standby in the event that central apneas were not effectively treated on CPAP or bilevel therapy. A positional pillow to avoid supine sleep was also recommended until positive airway pressure was initiated. (see Figures 1–3)
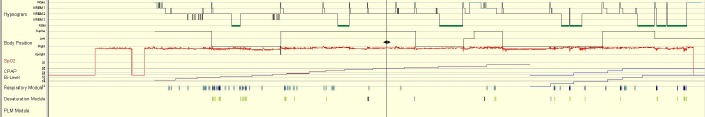
Figure 1.
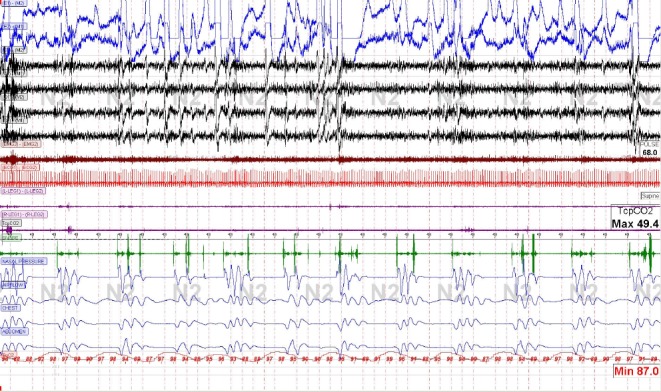
Central apneas in supine sleep on diagnostic polysomnogram.
Figure 2.
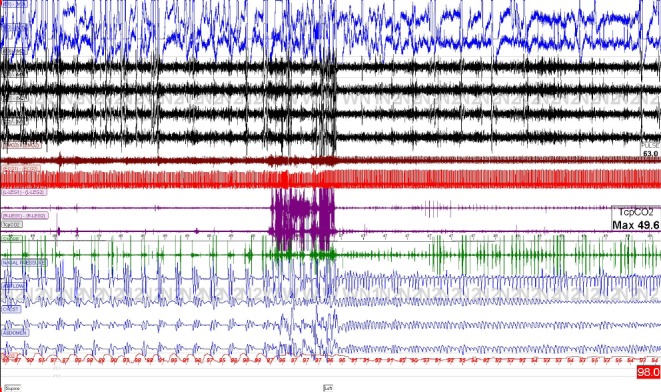
Central apneas in supine sleep on diagnostic polysomnogram which resolved in lateral (left sided) sleep.
Figure 3.
Central apneas in supine sleep on diagnostic polysomnogram which resolved in lateral (left sided) sleep.
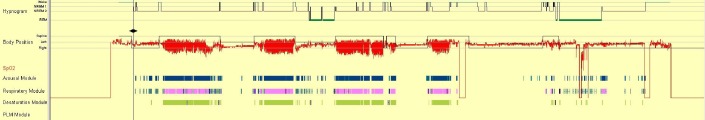
The patient returned for an overnight titration study. CPAP pressures of 5 to 18 cm water were tested. Bilevel pressures of 17/12 to 20/17 cm water were tested. Central sleep apnea dramatically improved on both CPAP and bilevel therapy in the supine and lateral position. A CPAP pressure of 14 cm water was recommended. A mean oxygen saturation of 96%, minimum oxygen saturation of 94%, RDI 2.7, and supine REM was observed at this pressure setting. A positional pillow was not used during the titration study (Figure 4).
Figure 4.
Improvement of positional sleep apnea on CPAP and Bilevel therapy in both lateral and supine sleep.
The patient returned one month later for follow-up after using CPAP. Although he still experienced fatigue, download data showed effective treatment of his sleep apnea. Compliance data showed 100% of days with device usage, with an average of 7.5 h of usage per night. Therapy data showed an average residual AHI of 4.1 on CPAP of 14 cm water. Although download information was satisfactory, the presence of residual fatigue suggests that there may be residual respiratory events that were undetectable by the CPAP device. Although further testing was not pursued, a repeat titration study may have been considered at this point.
The patient was referred back to his primary care physician to evaluate further for possible underlying conditions; however, he denied any symptoms consistent with an underlying cardiac, renal, or neurologic condition. Further diagnostic testing had not been performed at the time of his sleep evaluation. An echo-cardiogram had not been performed, so further information on cardiac systolic and diastolic function, pulmonary artery pressure, and valvular problems was not available.
DISCUSSION
Positional sleep apnea is defined as greater than 50% reduction in the AHI between supine and non-supine positions. Sleeping position commonly affects the severity of obstructive sleep apnea. Specifically, sleeping in the supine position is associated with a worsening of obstructive sleep apnea and is more frequently seen in those patients with less severe OSA and smaller neck circumference. Worsening OSA in supine sleep is thought to be related to relaxation of muscles in the jaw and throat under the influence of gravity that cause narrowing of the airway.
Positional changes in central sleep apnea are less well understood and have mostly been documented in the literature in patients with Cheyne-Stokes respiration associated with congestive heart failure. There are only a few reports in the literature of positional central sleep apnea in patients with no known cardiac history or congestive heart failure. One study did show a change in sleep disordered breathing pattern from obstructive to almost all mixed and central apneas on both diagnostic and CPAP titration studies with change to supine sleeping position in 8 patients who had no cardiac history (one patients had a history of cerebral hemorrhage, and one had cerebral ischemia).12 Another study showed significant supine worsening of sleep apnea in patients with treatment-emergent central sleep apnea or complex sleep apnea both on CPAP therapy and adaptive servoventilation therapy (ASV).13 This case report showed idiopathic central sleep apnea in an otherwise healthy young man that was significantly worse in supine sleep. While CPAP therapy is not always helpful or even the first choice treatment in CSA, significant improvement in AHI was noted in our patient with CPAP pressures as low as 6 cm water during supine sleep. Treatment of central sleep apnea is generally based on the underlying cause. Central sleep apnea may be primary (idiopathic) or due to Cheyne-Stokes breathing (secondary to congestive heart failure, stroke, and possibly renal failure), positive airway pressure (i.e., complex sleep apnea), high altitude (i.e., > 4,000 meters), various medical conditions (e.g., brainstem lesion, cardiac or renal disorders), or drugs (e.g., opioids). In this patient, none of these potential causes were suspected or identified. Additionally, Cheyne-Stokes respiratory pattern and periodic breathing were absent on both the diagnostic and titration studies. Additional treatment options for central sleep apnea include other forms of positive airway pressure (i.e., servoventilation, bilevel PAP), supplemental gases (i.e., oxygen, carbon dioxide), medications (i.e., theophylline, acetazolamide), and correction of the causative etiology.
Sleeping in the supine position reduces cardiac output and increases venous return. Decreased cardiac output delays the transfer of blood gas information from the pulmonary capillary bed to the chemoreceptors and can lead to sustained fluctuations in respiratory output (i.e., central sleep apnea). Atrial pacing has been shown to reduce central sleep apnea in those with low cardiac output due to bradyarrhythmia.14 An increase in venous return could additionally exacerbate both diastolic and systolic dysfunction. This could result in an inability to reduce ventilation with carbon dioxide levels remaining near the central apnea threshold.
In addition to reducing cardiac output and increasing venous return, sleeping in the supine position can result in a reduction of both the functional residual capacity and the metabolic rate, which consequently enhances plant gain. Enhanced plant gain, which is defined as a large change in carbon dioxide levels relative to a small change in ventilation, is another proposed mechanism in the development of central sleep apnea.
The application of positive airway pressure in this patient could conceivably increase cardiac output and reduce venous return, improving arterial circulation time and reduces plant gain, which successfully normalizes ventilation.
The question must be considered whether this could be a mistaken case of obstructive sleep apnea. Given the worsening respiratory pattern in supine sleep, the lack of underlying causative etiology for CSA, absence of esophageal pressure manometry testing, normal wake baseline TcCO2 levels of 40-43 mm Hg, and the positive response to CPAP therapy, the possibility of obstructive sleep apnea cannot be ruled out. Although idiopathic central sleep apnea is usually associated with hypocapnia and this patient's TcCO2 levels were slightly elevated, it is not required. Eupneic patients with congestive heart failure may also have central sleep apnea. More important is the proximity of the central apnea threshold to the carbon dioxide level. Other features of central sleep apnea were evident on the patient's sleep studies, including improvement of respiratory events in REM sleep and clear flattening of the chest and abdominal belts even with an increase in sensitivity.
The present case suggests that positional changes in severity of central sleep apnea may be an important factor to consider. Many patients have difficulty tolerating current treatment options for CSA including CPAP, bilevel PAP, and servoventilation therapy. Positional pillows are often viewed by patients as a more tolerable alternative treatment of sleep apnea. Further research on the prevalence of positional CSA and exploration of positional therapy as a viable treatment option for CSA is needed. Although a positional pillow was recommended to this patient, he did not attempt positional therapy as a treatment option.
DISCLOSURE STATEMENT
This was not an industry supported study. Dr. Kushida receives research support from Philips Respironics and ResMed through Stanford University. The other authors have indicated no financial conflicts of interest.
References
- 1.Oksenberg A, Silverberg DS, Arons E, et al. Positional vs nonpositional obstructive sleep apnea patients: anthropomorphic, nocturnal polysomnographic, and multiple sleep latency test data. Chest. 1997;112:629–39. doi: 10.1378/chest.112.3.629. [DOI] [PubMed] [Google Scholar]
- 2.Cartwright RD. Effect of sleep position on sleep apnea severity. Sleep. 1984;7:110–4. doi: 10.1093/sleep/7.2.110. [DOI] [PubMed] [Google Scholar]
- 3.Akita Y, Kawakatsu K, Hattori C, et al. Posture of patients with sleep apnea during sleep. Acta Otolaryngol. 2003;550(suppl):41–5. [PubMed] [Google Scholar]
- 4.Pevernagie DA, Shephard JW. Relations between sleep stage, posture and effective nasal CPAP levels on OSA. Sleep. 1992;15:162–7. doi: 10.1093/sleep/15.2.162. [DOI] [PubMed] [Google Scholar]
- 5.Cartwright R, Ristanovic R, Diaz F, et al. A comparative study of treatments for positional sleep apnea. Sleep. 1991;14:546–52. doi: 10.1093/sleep/14.6.546. [DOI] [PubMed] [Google Scholar]
- 6.Magalang UJ, Mador MJ. Behavioral and pharmacologic therapy of obstructive sleep apnea. Clin Chest Med. 2003;24:343–53. doi: 10.1016/s0272-5231(03)00022-4. [DOI] [PubMed] [Google Scholar]
- 7.Oksenberg A, Silverberg DS, Arons E, et al. Positional vs. nonpositional obstructive sleep apnea patients: anthropomorphic, nocturnal polysomnographic, and multiple sleep latency test data. Chest. 1997;112:629–39. doi: 10.1378/chest.112.3.629. [DOI] [PubMed] [Google Scholar]
- 8.Oksenberg A, Arons E, Snir D, Radwan H, Soroker N. Cheyne-Stokes respiration during sleep: a possible effect of body position. Med Sci Monit. 2002;8:CS61–5. [PubMed] [Google Scholar]
- 9.Sahlin C, Svanborg E, Stenlund H, et al. Cheyne-Stokes respiration and supine dependency. Eur Respir J. 2005;25:829–33. doi: 10.1183/09031936.05.00107904. [DOI] [PubMed] [Google Scholar]
- 10.Szollosi I, Roebuck T, Thompson B, et al. Lateral sleeping position reduces severity of central sleep apnea/Cheyne-Stokes respiration. Sleep. 2006;29:1045–51. doi: 10.1093/sleep/29.8.1045. [DOI] [PubMed] [Google Scholar]
- 11.Joho S, Oda Y, Hirai T, et al. Impact of sleeping position on central sleep apnea/Cheyne-Stokes respiration in patients with heart failure. Sleep. 2010;11:143–8. doi: 10.1016/j.sleep.2009.05.014. [DOI] [PubMed] [Google Scholar]
- 12.Issa FG, Sullivan CE. Reversal of central sleep apnea using nasal CPAP. Chest. 1986;90:165–71. doi: 10.1378/chest.90.2.165. [DOI] [PubMed] [Google Scholar]
- 13.Allam JS, Olson EJ, Gay PC, et al. Efficacy of adaptive servoventilation in treatment of complex and central sleep apnea syndromes. Chest. 2007;132:1839–46. doi: 10.1378/chest.07-1715. [DOI] [PubMed] [Google Scholar]
- 14.Garrigue S, Bordier P, Jais P, et al. Benefit of atrial pacing in sleep apnea syndrome. N Engl J Med. 2002;346:404–12. doi: 10.1056/NEJMoa011919. [DOI] [PubMed] [Google Scholar]
- 15.Nakao S, Come PC, Miller MJ, et al. Effects of supine and lateral positions on cardiac output and intracardiac pressures: an experimental study. Circulation. 1986;73:579–85. doi: 10.1161/01.cir.73.3.579. [DOI] [PubMed] [Google Scholar]


