Foot infections in individuals with diabetes are a major cause of morbidity, constituting the most common reason for both diabetes-related hospitalization and lower extremity amputations (1,2). Optimal treatment of these diabetic foot infections requires recognizing which foot ulcers are infected and prescribing pathogen-appropriate antibiotic therapy. Most experts concur that diagnosing infection should be based on the presence of primary or secondary clinical signs and symptoms of inflammation (1,2), but the frequent presence of peripheral neuropathy or peripheral arterial disease may confound the diagnosis (3). Thus, some favor using bacterial density in wound cultures to help diagnose infection (4,5). This concept is based on the belief that a high wound “bioburden” leads to “critical colonization,” an intermediary state on the way to overt infection that may be responsible for delayed wound healing and that may respond to antimicrobial therapy (6,7). Certainly, treatment of clinically overt diabetic foot infection requires appropriate systemic antibiotic therapy, which is best guided by identifying the causative pathogens.
Indigenous microorganisms residing on humans were first observed more than 300 years ago (8), and for over 150 years clinicians have relied on the results of cultures to define the causative organisms in bacterial infections. Unfortunately, culture-based techniques select for species that flourish under the typical nutritional and physiological conditions of the diagnostic microbiology laboratory, not necessarily the most abundant or clinically important organisms (9). In the past decade, studies with molecular microbiological techniques have raised doubts about the accuracy of wound culture results (10). Using amplification and sequence analysis of 16S rRNA, a highly conserved gene present in all prokaryotes (bacteria) but not eukaryotes (humans) that contains hypervariable regions allowing bacterial identification, has revealed vastly more complex bacterial communities than those identified by culture, particularly in chronic wounds (11–13).
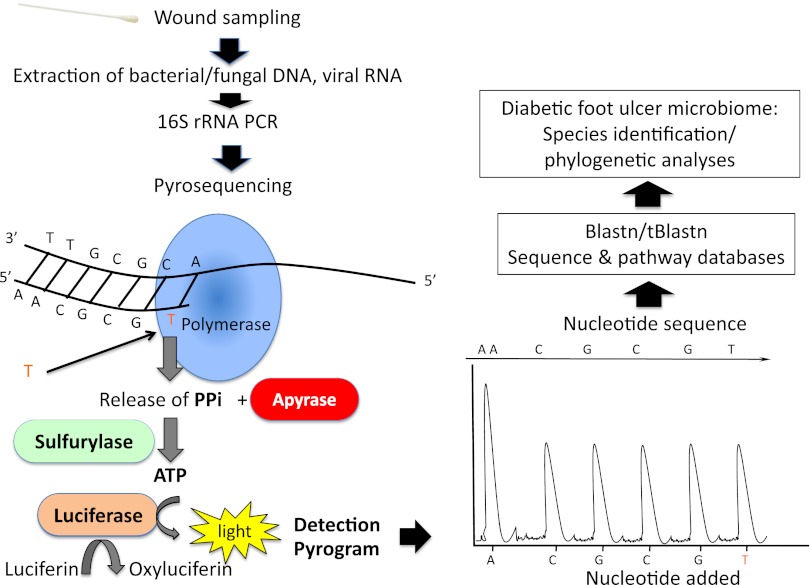
In this issue, Gardner et al. (14) present a study designed to compare the results of standard cultures with gene sequencing in neuropathic diabetic foot ulcers (DFUs) and to ascertain if there are clinical features of these wounds that are related to three key dimensions of wound bioburden. We hope that readers unfamiliar with molecular microbiology will bear with some of the necessary jargon; Fig. 1 illustrates the main techniques used in this study. In brief, their pyrosequencing techniques demonstrated 13 bacterial phyla, but Firmicutes (gram-positives) were the dominant flora, with Staphylococcus species by far the most frequent. In comparison, cultures greatly underestimated the microbial load, overestimated the relative abundance of staphylococci, and underrepresented the prevalence of obligate anaerobes. These findings are not surprising, as staphylococci grow more easily than exigent bacteria such as anaerobes, especially with the short duration of culture and the media typically used in clinical microbiology laboratories. Sequencing demonstrated great heterogeneity in the colonizing flora, but they could generally be divided into three clusters, i.e., those with a high relative abundance of 1) Staphylococcus spp., 2) Streptococcus spp., or 3) anaerobes and Proteobacteria (gram-negatives). This nonrandom distribution pattern of bacteria has been referred to as functionally equivalent pathogroups (11,12), meaning bacterial species considered as nonpathogenic when present alone may coaggregate symbiotically in a pathogenic biofilm and act synergistically to cause a chronic wound infection.
FIG. 1.
Steps for analyzing the microbiome of a DFU (adapted from England R, Pettersson M. Pyro Q-CpG: quantitative analysis of methylation in multiple CpG sites by Pyrosequencing. Nat Methods 2005;2:i–ii). After wound sampling, extraction is performed to obtain bacterial/fungal DNA and/or viral RNA. Specific genetic targets of hypervariable regions within bacterial 16S rRNA genes are amplified by the polymerase chain reaction (PCR) and subjected to DNA pyrosequencing. Sequencing by synthesis occurs by a DNA polymerase–driven generation of inorganic pyrophosphate (PPi) with the formation of ATP and ATP-dependent conversion of luciferin to oxyluciferin. The generation of oxyluciferin causes the emission of light pulses, and the amplitude of each signal is directly related to the presence of one or more nucleosides. The different bacteria can be identified by the effective combination of conserved primer-binding sites and intervening variable sequences that facilitate genus and species identification (software Blastn/tBlastn, http://blast.ncbi.nlm.nih.gov/). The identification of all the bacterial genomes amplified determines the composition of DFU flora (microbiome).
Gardner et al. (14) found that agreement between results on culture and by sequencing was relatively low. Because cultures underrepresented wound flora, the authors used sequencing to analyze the association of the three dimensions of bioburden in the DFU microbiome with six clinical variables. They found that ulcer duration was positively correlated with diversity and Proteobacteria abundance (but negatively associated with Staphylococcus abundance); ulcer depth (and, to a lesser degree, area) was positively associated with abundance of anaerobes (but negatively associated with Staphylococcus abundance); and elevated HbA1c was positively associated with predominant colonization with Staphylococcus or Streptococcus. Strengths of this study include limiting enrollment to a homogeneous group of diabetic patients (those with a clinically uninfected, neuropathic, plantar ulcer), methodically investigating clinical features that are commonly used by clinicians, using optimal molecular techniques, and applying rigorous statistical analysis to their findings. Weaknesses included obtaining specimens for culture by the swab technique; notwithstanding the authors’ belief in the validity of the Levine method (5), most authorities consider tissue specimens more accurate for wound cultures. Also, because those with the common complications of limb ischemia or substantial gangrene were excluded, the results do not apply to such patients.
The study results, while useful and robust, are neither novel nor unexpected. Furthermore, because clinically uninfected wounds should not be treated with antimicrobials (15), and the clinical significance of the extra organisms identified by sequencing but not by culture is unclear, it remains to be demonstrated that this currently scarce technology will be useful in managing patients with a DFU. We regret that the study did not report any follow-up on enrolled patients, as it would have been interesting to know if analysis of the microbiome can predict which uninfected DFUs will become clinically infected. If so, this might challenge two dogmas in the management of DFUs: the lack of usefulness of wound sampling in the absence of clinical evidence of infection and the avoidance of antibiotic treatment for clinically uninfected wounds.
The development of molecular microbiological technologies is a promising tool to better understand the local ecology of chronic wounds, including DFUs (16). It may ultimately help clinicians to more accurately differentiate colonization from infection, to optimize antibiotic therapy against the true wound pathogens, and even to predict ulcer outcome (13). The potential benefits of pyrosequencing must, however, be weighed against the cost in equipment and in technician time, the delay in reporting results, the fact that it amplifies dormant or dead bacteria, and that it fails to demonstrate some bacterial and most nonbacterial microorganisms (17–20). We believe it is likely that molecular techniques, once they become more rapid and affordable, will ultimately replace the increasingly antiquated culture methods now used in clinical microbiology laboratories. But, given their limitations (as outlined above and in the authors’ discussion) and expense, it is not yet clear that this small, albeit important, step forward in defining the microbiome of DFUs provides the long-awaited giant leap in understanding.
ACKNOWLEDGMENTS
No potential conflicts of interest relevant to this article were reported.
Footnotes
See accompanying original article, p. 923.
REFERENCES
- 1.Lipsky BA, Jeffcoate W, Peters EJG, et al. Expert opinion on the management of infections in the diabetic foot. From the International Working Group on the Diabetic Foot. Diabetes Metab Res Rev 2012;28(Suppl. 1):163–178 [DOI] [PubMed] [Google Scholar]
- 2.Lipsky BA, Berendt AR, Cornia PB, et al. 2012 Infectious Diseases Society of America clinical practice guideline for the diagnosis and treatment of diabetic foot infections. Clin Infect Dis 2012;54:e132–e173 [DOI] [PubMed] [Google Scholar]
- 3.Richard JL, Lavigne JP, Sotto A. Diabetes and foot infection: more than double trouble. Diabetes Metab Res Rev 2012;28(Suppl. 1):46–53 [DOI] [PubMed] [Google Scholar]
- 4.Bowler PG, Duerden BI, Armstrong DG. Wound microbiology and associated approaches to wound management. Clin Microbiol Rev 2001;14:244–269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gardner SE, Hills SL, Franz RA. Clinical signs of infection in diabetic foot ulcers with high microbial load. Biol Res Nurs 2009;11:119–128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xu L, McLennan SV, Lo L, et al. Bacterial load predicts healing rate in neuropathic diabetic foot ulcers. Diabetes Care 2007;30:378–380 [DOI] [PubMed] [Google Scholar]
- 7.Woo KY, Sibbald RG. A cross-sectional validation study of using NERDS and STONEES to assess bacterial burden. Ostomy Wound Manage 2009;55:40–48 [PubMed] [Google Scholar]
- 8.Relman DA. Microbiology: Learning about who we are. Nature 2012;486:194–195 [DOI] [PubMed] [Google Scholar]
- 9.Grice EA, Segre JA. The skin microbiome. Nat Rev Microbiol 2011;9:244–253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kong HH, Segre JA. Skin microbiome: looking back to move forward. J Invest Dermatol 2012;132:933–939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dowd SE, Wolcott RD, Sun Y, McKeehan T, Smith E, Rhoads D. Polymicrobial nature of chronic diabetic foot ulcer biofilm infections determined using bacterial tag encoded FLX amplicon pyrosequencing (bTEFAP). PLoS ONE 2008;3:e3326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dowd SE, Sun Y, Secor PR, et al. Survey of bacterial diversity in chronic wounds using pyrosequencing, DGGE, and full ribosome shotgun sequencing. BMC Microbiol 2008;8:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sotto A, Richard JL, Messad N, et al. French Study Group on the Diabetic Foot Distinguishing colonization from infection with Staphylococcus aureus in diabetic foot ulcers with miniaturized oligonucleotide arrays: a French multicenter study. Diabetes Care 2012;35:617–623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gardner SE, Hillis SL, Heilmann K, Segre JA, Grice EA. The neuropathic diabetic foot ulcer microbiome is associated with clinical factors. Diabetes 2013;62:923–930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lipsky BA, Hoey C. Topical antimicrobial therapy for treating chronic wounds. Clin Infect Dis 2009;49:1541–1549 [DOI] [PubMed] [Google Scholar]
- 16.Lipsky BA. Diabetic foot infections: microbiology made modern? Array of hope. Diabetes Care 2007;30:2171–2172 [DOI] [PubMed] [Google Scholar]
- 17.Janda JM, Abbott SL. 16S rRNA gene sequencing for bacterial identification in the diagnostic laboratory: pluses, perils, and pitfalls. J Clin Microbiol 2007;45:2761–2764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ley RE, Bäckhed F, Turnbaugh P, Lozupone CA, Knight RD, Gordon JI. Obesity alters gut microbial ecology. Proc Natl Acad Sci USA 2005;102:11070–11075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wagner M, Horn M. The Planctomycetes, Verrucomicrobia, Chlamydiae and sister phyla comprise a superphylum with biotechnological and medical relevance. Curr Opin Biotechnol 2006;17:241–249 [DOI] [PubMed] [Google Scholar]
- 20.Wolcott RD, Gontcharova V, Sun Y, Dowd SE. Evaluation of the bacterial diversity among and within individual venous leg ulcers using bacterial tag-encoded FLX and titanium amplicon pyrosequencing and metagenomic approaches. BMC Microbiol 2009;9:226. [DOI] [PMC free article] [PubMed] [Google Scholar]