Figure 5.
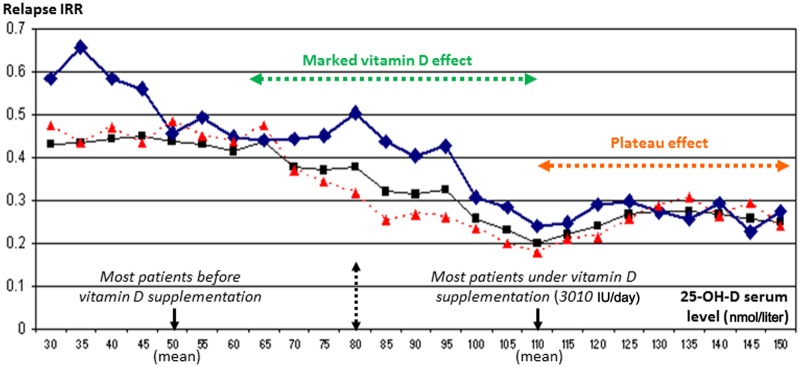
Example of evolution of relapse incidence rate ratio according to the 25-OH-D serum level in patients with MS.
This study was performed before and under vitamin D supplementation (3010 IU/day on average) in a cohort of 156 consecutive patients with relapsing–remitting MS under first-line immunomodulatory therapy and followed for 2.5 years on average (for more details, see Pierrot-Deseilligny and colleagues [Pierrot-Deseilligny et al. 2012]. Note that in a multivariate model adjusted for the patient’s age, disease duration and previous use of an IMT prior to inclusion, a 13.7% decrease in the incidence rate of relapses (95% confidence interval 10.64%–16.64%) was associated with every 10 nmol/liter increase in the 25-OH-D serum level (p < 0.0001). Note also that most patients passed from a stage of vitamin D insufficiency before supplementation [left part of the figure, with for the whole population: mean (black arrow) = 49 nmol/liter; SD = 22] to a stage of relative vitamin D sufficiency under vitamin D supplementation [right part of the figure, with for the whole population: mean (black arrow) = 110 nmol/liter; SD = 26], with a potential vitamin D effect appearing particularly marked on relapses between 60 and 110 nmol/liter (green arrow). Furthermore, a plateau effect (orange arrow) was observed beyond 110 nmol/liter, suggesting that higher 25-OH-D serum concentrations are not required to obtain an optimal beneficial effect on the relapse rate. In black, whole population (n = 156); in blue, group 1 (n = 76, with IMT started prior to vitamin D supplementation); in red, group 2 (n = 80, with IMT started concomitantly with vitamin D supplementation). Adapted with permission from Pierrot-Deseilligny et al. [2012]. IMT, first-line immunomodulatory therapy; IRR, incidence rate ratio; SD, standard deviation.
