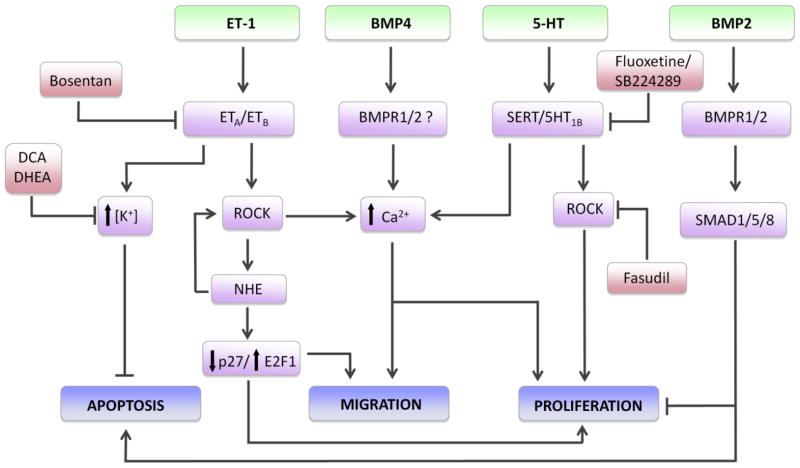
Fig. 1.
Some of the proposed signaling mechanisms in pulmonary arterial smooth muscle cells (PASMCs) leading to vascular remodeling during pulmonary hypertension. Agonists, including endothelin-1 (ET-1), bone morphogenetic proteins 2 and 4 (BMP2 and BMP4, respectively) and serotonin (5-HT) interact with membrane bound receptors or transporters (serotonin transporter, SERT). Activation of ET-1 receptors leads to increased intracellular K+ concentration and inhibition of apoptosis, as well as activation of Rho kinase (ROCK) and downstream signaling through activation of the Na+/H+ exchanger (NHE) and elevation of intracellular Ca2+. NHE increases ROCK activation and promotes migration and proliferation via downregulation of p27 and activation of the transcription factor E2F1. NHE has also been found to increase ROCK, suggesting potential feed-forward regulation. BMP4 and 5-HT both increase intracellular Ca2+, which is required for PASMC migration and proliferation. 5-HT-induced ROCK activity also leads to PASMC proliferation; whether this involves modulation of Ca2+ or Ca2+-independent pathways is unclear. BMP2 binding to type 1 and type 2 receptors (BMPR1 and BMPR2) activates SMAD1/5/8 signaling and represses proliferation and stimulates apoptosis. Pharmacological inhibitors (in red) reduce vascular remodeling by disrupting signaling at various points.