Abstract
The objective here was to review the effects of polyvinylpyrrolidone (PVP) upon sperm function and embryonic development in humans. PVP has been used successfully in intracytoplasmic sperm injection (ICSI) to facilitate the handling and immobilization of sperm for both domestic animals and humans. In our previous reports, PVP solution exists locally in embryos injected during the early developmental period, and also exerts influence over the developmental capacity of such embryos. In other reports, PVP causes significant damage to sperm membranes that can be detected by transmission electron microscopy, and has been associated with chromosomal abnormalities in pregnancy derived from ICSI embryos. In some Japanese clinics, PVP‐free media has been used for sperm immobilization in order to optimise safety. Consequently, it is strongly suggested that the success rate of fertilization and clinical pregnancy could be improved by using PVP‐free solution for human ICSI. In conclusion, our interpretation of the available data is to perform ICSI without PVP or select a lower concentration of PVP solution in order to reduce safety for pregnancy and children born via ICSI.
Keywords: Sperm capacitation, Embryo development, Polyvinylpyrrolidone (PVP), Clinical utility in vitro embryo production in human
Introduction
Polyvinylpyrrolidone (PVP) is a soluble polymer in water and made from N‐vinylpyrrolidone [1]. In the 1930s, the PVP patent was filed as one of the most attractive chemicals of acetylene chemistry [1]. PVP was first used for a blood plasma substitute and subsequently in a variety of applications in the fields of medicine, pharmacy, cosmetics and industry [1]. Povidone iodine is equally effective and could be preferred due to easy availability and lower cost for the objectives of those fields [2]. On the other hand, we experienced many documented cases of allergic reactions to PVP/povidone, especially for subcutaneous utility and when PVP has been touching autologous serum and mucous membranes [3, 4]. In another case, an allergic reaction to PVP was found in some people [5, 6, 7]. Over recent years, PVP has been used for sperm manipulation in human assisted reproduction (ART), and has been investigated during embryo development [8]. It is thus vital to confirm the safety of PVP application for human ART. Therefore, the objective of this review article is to examine the detrimental effects and potential risk of PVP upon sperm function and early embryo development following human ICSI.
The history of PVP in assisted reproduction for animals
PVP has been used for sperm selection, oocyte culture and cryopreservation for the last 50 years. Initially, PVP, the average molecular weight of which is 10,000 Da, was found to provide the greatest degree of protection to platelets when cryopreserved at −196 °C [9]. Researchers demonstrated the production of piglets following the transfer of vitrified porcine embryos after stepwise dilution of PVP and other cryoprotectants [9]. Next, percoll, consisting of silica particles coated with PVP, have been used for many years for routine sperm preparation for animal reproduction protocols [10, 11, 12]. Motile sperm were highly purified in an inner column of a centrifuge tube via the use of a discontinuous percoll density gradient [10]. In another study, PVP was substituted for protein in media to promote the development of in vitro methods that permit IVM/IVF embryos to mature, fertilize and develop to the blastocyst stage, but in a protein‐free medium without bovine serum albumin [11, 12, 13]. PVP prevents oocytes from adhering to plastic and glass dishes. PVP was also used to establish a culture system to support the growth of immature bovine oocytes enclosed in granulosa cell complexes [14]. When PVP medium was used, the ability of immature oocytes obtained from bovine ovaries to fertilise and develop to the blastocyst stage was increased in vitro [14]. Finally, PVP has been used successfully for intracytoplasmic sperm injection (ICSI) in order to increase the viscosity of sperm solution, thus facilitating the handling and immobilization of individual sperm in both domestic animal and human situations [8, 15, 16, 17, 18, 19]. PVP can be used to help regulate fluid handling in the injection pipette and limit the final volume injected into the oocyte [20]. During ICSI, sperm are first suspended in a medium containing PVP and a single spermatozoon is chosen and injected into the oocyte, unavoidably together with a small amount of medium [21].
Current perspective and potential risk for the application of PVP for intracytoplasmic sperm injection in clinics and hospitals
A summary of the clinical use of PVP is given in Table 1. More than 90 % of published studies used PVP to immobilize sperm motility during ICSI treatment. Fertilization, cleavage and clinical pregnancy rate were 20–80, 40–90 and 10–50 %, respectively. More than ten thousand ICSI children have been born every year since ICSI was introduced for human ART [22]. These data suggest that the embryo can develop to fetal stages and into a healthy child following the co‐injection of sperm and a small volume of PVP into the oocyte during infertility treatment.
Table 1.
The use of PVP in clinical reports for 20 years
| PVP used/not used | PVP brand | Fertilization rate a (%) | Cleavage rate b (%) | Clinical pregnancy rate c (%) | References |
|---|---|---|---|---|---|
| × | – | 80.0 | 80.0 | 0.0 | [59] |
| o | – | 41.7 | 41.7 | 50.0 | [60] |
| × | – | 68.0 | 52.9 | 14.3 | [61] |
| × | – | 69.0 | 13.3 | 44.6 | [62] |
| o | – | 66.7 | 75.0 | 50.0 | [63] |
| o | – | 86.7 | 15.4 | 16.7 | [64] |
| o | – | 73.9 | 22.4 | 40.9 | [65] |
| o | – | – | – | – | [66] |
| o | – | – | – | – | [67] |
| o | – | – | – | – | [68] |
| o | – | – | – | – | [69] |
| × | – | – | – | – | [70] |
| × | – | – | – | – | [71] |
| o | – | – | – | – | [72] |
| o | – | 82.6 | 69.5 | – | [73] |
| o | ICN Biochemicals | – | – | – | [8] |
| o | Scandinavian IVF Science AB | 64.3 | – | 28.4 | [74] |
| o | Scandinavian IVF Science AB | 67.6 | 62.2 | 17.0 | [75] |
| o | SAGE IVF Inc. | 66.7 | 54.4 | 46.8 | [76] |
| o | VitroLife | 58.3 | 95.7 | 37.0 | [77] |
| o | VitroLife | 73.0 | – | 31.3 | [78] |
| o | VitroLife | 71.3 | 92.8 | 40.9 | [79] |
| o | Fertipro | 59.3 | 55.8 | 46.3 | [80] |
| o | Fertipro | 57.0 | 54.0 | 18.1 | [81] |
| o | Sigma | – | – | – | [82] |
| o | Sigma | 19.0 | 14.2 | 50.0 | [83] |
| o | Sigma | 69.4 | 62.9 | 44.4 | [84] |
| o | Sigma | – | 25.0 | 25.0 | [85] |
| o | Sigma | – | – | – | [86] |
| o | Sigma | 80.9 | 88.3 | 26.7 | [87] |
| o | MediCult | 85.8 | – | 20.9 | [88] |
| o | MediCult | 56.3 | – | 37.1 | [89] |
| o | MediCult | 87.1 | – | 21.6 | [90] |
| o | MediCult | 80.9 | 78.9 | 40.6 | [91] |
| o | MediCult | 62.6 | 60.6 | 31.1 | [92] |
| o | MediCult | 67.0 | 51.3 | 28.9 | [93] |
| o | MediCult | 61.9 | – | 57.1 | [94] |
| o | MediCult | 27.0 | 27.0 | 33.3 | [95] |
| o | MediCult | 45.0 | – | – | [96] |
| o | MediCult | 75.6 | 75.6 | 44.1 | [97] |
| o | MediCult | 69.0 | 69.0 | 49.1 | [98] |
| o | Irvine Scientific | 58.6 | 84.1 | – | [99] |
| o | Irvine Scientific | – | – | – | [100] |
| o | Irvine Scientific | 40.0 | 40.0 | 33.3 | [101] |
| o | Irvine Scientific | 43.0 | 39.0 | – | [102] |
| o | Irvine Scientific | 73.9 | 82.7 | 28.6 | [103] |
| o | Irvine Scientific | 67.7 | 50.3 | 25.0 | [104] |
| o | Irvine Scientific | 67.9 | – | 37.5 | [105] |
| o | Irvine Scientific | – | 43.9 | 44.8 | [106] |
| o | Irvine Scientific | – | – | – | [107] |
aFertilized oocytes per injected metaphase II oocyte
bCleavaged oocytes per injected metaphase II oocyte
cThe number of pregnancy per embryo transferred
However, the exposure of sperm to PVP has been found to cause sub‐microscopic changes in sperm structure; damage has been observed in the sperm nucleus, both in terms of shape and in the texture of chromatin, which was frequently decondensed [23]. PVP‐induced nuclear and membrane damage may have been due to the breakdown of sperm membranes [24]. These studies suggest that PVP induces nuclear damage in the sperm leading to subsequent chromosomal aberration. Furthermore, PVP delayed the onset of calcium oscillations and sperm decondensation within the oocyte [25, 26]. Consequently, it is likely that exposure of sperm to PVP may suppress fertilization and embryonic development. Moreover, as the molecular weight of PVP used for ICSI is 360,000 Da, PVP injected during the ICSI procedure remains in the oocytes for a prolonged period of time [27]. Consequently, this means that PVP is likely to impede embryo development and pregnancy.
The numbers of ICSI treatments have been increasing more than conventional IVF treatments in Europe over the last few years [28]. These data suggest that ICSI treatment for male fertility is becoming the most important option for human ART. However, the European pregnancy rates of ICSI embryos are lower compared to IVF embryos [28]. The main differences between ICSI and IVF treatments involve the oocyte membrane being broken by a micropipette, along with the subsequent injection of sperm, PVP solution and external media, or the process of fertilization, especially, non‐sperm‐egg fusion in ICSI, there is delay of onset of sperm decondensation and Ca oscillation [29].
The detrimental effects of PVP upon sperm function
PVP can cause injury to the sperm membrane, acrosome, head and nucleus
We examined the effects of PVP upon sperm capacitation and the acrosome reaction in bovines [30] and found that sperm cultured in PVP demonstrated increased rates of acrosome reaction when compared with bull sperm cultured in a control group (Fig. 1). PVP may thus trigger the acrosome reaction. While numerous events are known to occur during capacitation, it appears that regulation of the intracellular concentration of Ca2+ is one of the most important. During capacitation, the initial influx of Ca2+ into the sperm is used to fill an intracellular Ca2+ store located in the acrosome [31]. One possibility suggested by Spungin and Breitbart [32] was that increased levels of adenylate cyclase activity triggered a further increase in cyclic AMP causing further Ca2+ channels in the acrosome to release Ca2+ from internal stores into the cytoplasm. Binding of capacitated sperm to the zona pellucida triggers the activation of a G protein that, in turn, opens a cation channel in the plasma membrane [33]. Furthermore, the acrosome reaction has been induced artificially following the influx of Ca2+ into the sperm head [34]. In human sperm, PVP has been shown to induce damage to sperm membranes, mitochondrial membranes and to cause deterioration of the axonemal tubules and fibrous sheath [23]. When considered collectively alongside these earlier studies, we infer that the presence of PVP in culture medium induces damage to the sperm plasma membrane and thus initiates the influx of Ca2+ into the sperm cells prematurely, thereby inducing the acrosome reaction.
Figure 1.
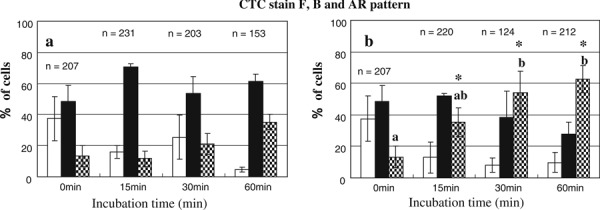
Effect of PVP on capacitation and the acrosome reaction in bovine sperm. Uncapacitated bovine sperm suspension was incubated for 0, 15, 30 and 60 min in the absence (A) or presence (B) of 10 % PVP in modified‐SOF and then analysed using CTC stain. Experiments were repeated six times. Data represent the percentage of cells expressing the F pattern (open bars), B pattern (filled bars), and AR pattern (hatched bars) of CTC fluorescence. Values represent mean ± SEM. Annotation (a, b) indicates p < 0.05 compared to 0 min (ANOVA: F 6,38 = 0.0068). Asterisks indicate p < 0.05 compared to controls. n the number of sperm. Figure from Kato and Nagao [30]
Sperm exposed to PVP incurred damage to the nucleus following ICSI
We also examined the effects of incubating bull sperm in PVP on fertilization [30] and found that sperm cultured in PVP solution exhibited lower fertility rates in vitro compared with sperm cultured in a control media. This finding showed that the use of PVP solution resulted in a significant reduction in the rate of sperm incorporation into oocytes. From this finding, we concluded that PVP caused injury to the ultrastructure of the mitochondria and sperm tail in our experiments. It is well established that sperm cells become motile and travel to oocytes via tail motion. The hyperactive state associated with the acrosome reaction allows sperm to penetrate the cumulus and zona pellucida surrounding the oocyte [35]. Progressive motility is one of the most important criteria for establishing the fertilization potential of sperm [36]. This finding demonstrates that incubation with PVP affects natural gamete interactions and can result in lower fertilization rates.
We also showed the effect of sperm cultured in PVP solution upon fertilization following ICSI. Most sperm cultured in PVP involved the acrosome reaction (Fig. 1), then the sperm were injected into bovine oocytes. These results showed that the injection of sperm without intact acrosomes and cultured in PVP, resulted in enhanced pronuclear formation following ICSI. The reason for this is that if the acrosome is removed from the sperm head, then the sperm nucleus may become pronuclear. Ca oscillations were immediately initiated after injection of acrosome‐less and demembranated mouse spermatozoa [29]. Generally, the factor influencing onset of Ca oscillation in ICSI most is immobilization of sperm [37]. PVP also delayed the onset of calcium oscillations in the oocyte [25, 26]. From these finding, PVP directly and indirectly influence Ca oscillation after sperm injection. Recent studies show that oscillatory patterns of Ca2+ in fertilized mouse eggs influence embryonic gene expression in blastocysts and post‐implantation development to term [38]. Data also suggest that hyper‐stimulation of the calcium oscillation profile exhibited a far greater variability in birth weight and pregnancy/implantation rates following embryo transfer. We infer that PVP‐treated sperm might affect the Ca2+ oscillation profile, resulting in impediment to embryo and fetus development. Therefore, PVP could be potentially dangerous for the sperm nucleus during ICSI treatments. Consequently, when embryologists use PVP solution, it may be better to reduce the length of the treatment period.
PVP may induce defective embryo development
The hazardous effects of PVP injection upon pronuclear oocytes and development to the blastocyst stage
Embryo development was clearly suppressed by PVP injection in bovines [30]. Rates of cleavage and blastocyst formation were significantly reduced in embryos injected with PVP (Table 2). Embryos injected with PVP mostly arrested at the two‐ to 16‐cell stage (data not shown) and only a few developed to the blastocyst stage. The total numbers of cells at the blastocyst stage in control groups were higher than in the PVP group (88.9 ± 6.0, 90.4 ± 4.5, and 48.8 ± 10.7, respectively). There was no difference in the chromosomal integrity of blastocysts when compared between PVP‐injected blastocysts and non‐injected blastocysts (64.3 %:9/14 vs 78.9 %:15/19, p > 0.05). In this particular experiment, the direct injection of PVP into IVF embryos resulted in a reduction in the rate of cleavage and blastocyst formation, along with a reduction in the number of cells in blastocysts when compared with control IVF embryos (Table 2). In the first cleavage, microfilaments play a key role in mitosis and cytokinesis [39], indicating that PVP‐induced deterioration of the axonemal tubules [23], and thus microfilaments, could impart significant detriment upon in vitro development of the embryo, cleavage and blastocyst stage. On the other hand, PVP did not affect chromosomal integrity in this particular study, although other authors [40] have suggested that PVP may affect chromosomes for long periods throughout the blastocyst stage. Moreover, the effects of maintaining mouse sperm in PVP solution upon developmental arrest [41], and the effect of injecting mouse zygotes with small amounts of medium, may serve as key research for human ICSI, while avoiding ethical problems linked with experiments with human oocytes and embryos [42].
Table 2.
In vitro developmental rate of bovine embryos to the blastocyst stage following intracytoplasmic injection with PVP solution (n = 3–9)
| Number of oocytes | Number of embryos cleaved (%) | Number of blastocysts (%) | |
|---|---|---|---|
| Injected product | |||
| None (control) | 129 | 105 (81.4 %)a | 31 (24.0 %)c |
| SOF | 79 | 62 (78.5 %)a | 19 (24.1 %)c |
| PVP | 73 | 38 (52.1 %)b | 5 (6.8 %)d |
| Brand of PVP injected | |||
| Sigma | 90 | 44 (48.9 %)e | 13 (14.4 %)gh |
| Irvine | 115 | 79 (68.7 %)e | 24 (20.9 %)g |
| Fertipro | 110 | 53 (48.2 %)f | 9 (8.2 %)h |
| Injection medium | |||
| 199 | 65 | 41 (63.1 %) | 9 (13.8 %) |
| SOF | 95 | 63 (66.3 %) | 11 (11.5 %) |
| HTF | 61 | 36 (59.0 %) | 6 (9.8 %) |
This table was from Kato and Nagao [30]
n number of replicated experiments, letters within columns indicate significant differences (a–b χ 2 = 10.142, p < 0.001, c–d χ 2 = 10.14, p < 0.01, e–f χ 2 = 12.09, p < 0.01, g–h χ 2 = 7.260, p < 0.05)
Media brand could impede early embryo development while solvents of PVP do not
The differing nature of the various brands of PVP is known to cause differential effects. We infer that the process used to manufacture PVP can cause influence upon embryo development due to differences among various brands and solvent media [30]. The level of PVP purification, and therefore, the potential for contamination, may be critical in the generation of more efficient techniques for performing human ICSI. Van Steirteghem et al. [8] used dialyzed PVP for human ICSI. Thus, there remains the distinct possibility that the level of purification and potential contamination associated with PVP brands A, B and C may exert differential effects upon embryonic development. It is therefore very important for embryo development that different chemical suppliers are investigated in this respect [43]. Clearly, it would be vital to avoid selecting any media that was known to suppress embryo development.
We also investigated the brand of PVP in many clinical reports (Tables 1, 3). The average of fertilization rates were 58.5 % (Irvine), 58.2 % (Fertipro), 56.4 % (Sigma), 67.5 % (Vitrolife) and 65.8 % (Medicalt), respectively (Tables 1, 3 show reference). The average of cleavage rates were 56.7 % (Irvine), 54.9 % (Fertipro), 47.6 % (Sigma), 94.3 % (Vitrolife) and 60.4 % (Medicalt), respectively. The average of clinical pregnancy rates were 33.8 % (Irvine), 32.2 % (Fertipro), 36.5 % (Sigma), 36.4 % (Vitrolife) and 36.4 % (Medicalt), respectively (Tables 1, 3 show reference). There were no differences between the pregnancy rates for Irvine, Fertipro, Sigma, Vitrolife and Medicalt media. From these studies, differences were apparent between different brands in terms of embryo development and development to fetus, at least in the bovine model. However, in clinical reports, these rates were not significantly affected by the solvent used to dilute the PVP (Table 3).
Table 3.
PVP availability reported during the past 20 years
| Use/or not PVP | PVP brand | Fertilization rate a (%) | Cleavage rate b (%) | Pregnancy rate c (%) |
|---|---|---|---|---|
| ○ | Scandinavian IVF Science AB (n = 2) | 66.0 | 62.2 | 22.7 |
| ○ | SAGE IVF Inc. (n = 1) | 66.7 | 54.4 | 46.8 |
| ○ | VitroLife, Kungsbacka, Sweden (n = 3) | 67.5 | 94.3 | 36.4 |
| ○ | Fertipro, Belgium (n = 2) | 58.2 | 54.9 | 32.2 |
| ○ | Sigma, St. Louis, MO, USA (n = 3–4) | 56.4 | 47.6 | 36.5 |
| ○ | MediCult, Jyllinge, Denmark (n = 7–12) | 65.3 | 60.4 | 36.4 |
| ○ | Irvine Scientific, Santa Ana, Ca, USA (n = 5–6) | 58.5 | 56.7 | 33.8 |
aThe average of fertilization rates in the reports (n)
bThe average of cleavage rates in the reports (n)
cThe average of pregnancy rates in the reports (n)
Other factors to consider when addressing the potential utility of PVP are those pertaining to the PVP solvent selected for use. We investigated PVP solvents in several clinical reports. The composition of PVP solvent media are shown in Table 4. There were no differences between the pregnancy rates when different types of solvent were compared (Tables 1, 3, 4). From these studies, it appears that the solvent used for PVP does not affect embryo development and development of the fetus.
Table 4.
Composition of injection media for human intracytoplasmic injection of PVP
| Fertipro | MediCult | SAGE IVF Inc (present; CooperSurgical, Inc.) | Irvine Scientific | VitroLife |
|---|---|---|---|---|
| Water | Water | Water | Water | Water |
| Sodium chloride | – | Sodium chloride | Sodium chloride | Sodium chloride |
| Potassium chloride | – | Potassium chloride | Potassium chloride | Potassium chloride |
| Calcium chloride | – | Calcium chloride | Calcium chloride, anhydrous | Calcium chloride |
| Sodium dihydrogen phosphate | – | – | – | – |
| – | – | Potassium phosphate, anhydrous | Potassium phosphate, monobasic | Potassium di‐hydrogen |
| Magnesium sulfate | – | Magnesium sulfate | Magnesium sulfate, anhydrous | Magnesium sulfate |
| Sodium pyruvate | Sodium pyruvate | Sodium pyruvate | Sodium pyruvate | Sodium pyruvate |
| Glucose monohydrate | Glucose | Glucose | Glucose | Glucose |
| Sodium lactate | – | Sodium lactate | Sodium lactate | Sodium lactate |
| Sodium bicarbonate | Sodium bicarbonate | Sodium bicarbonate | Sodium bicarbonate | Sodium bicarbonate |
| Taurine | ||||
| Alanyl‐glutamine | ||||
| HEPES | Hepes free acid | HEPES | – | – |
| – | Hepes sodium salt | – | – | – |
| – | – | EDTA | – | EDTA |
| Human serum albumin | Human serum albumin | Human serum albumin 5 mg/mL | Human serum albumin 7–10 % | Recombinant human albumin |
| Polyvinylpyrrolidone | Polyvinylpyrrolidone | Polyvinylpyrrolidone | Polyvinylpyrrolidone | Polyvinylpyrrolidone |
| – | Streptomycine sulfate salt | Gentamicin | Gentamicin | – |
| – | Penicillin sodium salt | – | – | – |
| – | Phenol red (not product no. 1090) | Phenol red | – | – |
| – | EBSS | – | – | |
| Synthetic Serum Replacement (SSR®; USA: ART supplement contains recombinant human insulin) | – | – | – |
PVP can localize inside oocyte/embryo and prevent development to the fetal stage
During ICSI, PVP molecules are injected directly into the oocytes and their effect on intracellular membranes or DNA in the developing embryo is unknown. No detrimental effects have been demonstrated in the development of preimplantation bovine embryos in vitro [44]. However, our results showed that the direct injection of PVP into IVF embryos resulted in a reduction in the rates of cleavage and blastocyst formation, along with a reduction in the number of cells in blastocysts, relative to control IVF embryos. The reason for this was the smaller volume used by Motoishi et al. [44] compared to that used by Kato et al. [29]. Motoishi et al. injected only 2–3 pl of PVP into the bovine zygote while Kato et al. injected 24–32 pl of PVP. We conclude that the larger volume reduced development to the blastocyst stage, along with blastocyst cell number.
We demonstrated the precise localization of PVP solution in embryos. An example of a fixed IVF embryo is shown in Fig. 2. There were three patterns of PVP location in fixed IVF embryos. In most embryos, PVP solution dispersed soon after injection (1–3 h) and was not evident in the IVF embryos; similar results were obtained in the control group (Fig. 2a). In some IVF embryos, PVP generally dispersed (59.1 %), although some still remained at the injection site (15.9 %, Fig. 2b). In other embryos, all of the PVP solution remained at the injection site (25.0 %, Fig. 2c). PVP remained in 40.9 % of PVP‐injected IVF embryos.
Figure 2.
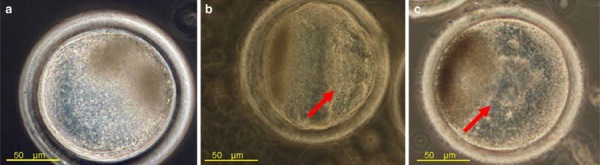
The location of PVP solution in embryos. a PVP was generally not observed in the embryo and appeared similar to the control. b PVP generally dispersed with some PVP remaining at the injection site. c Entire volume of PVP remaining in parts of the oocyte. Arrows show the localization of PVP solution. Figure from Kato and Nagao [30]
Since PVP is a large polymer (molecular weight 360 kDa), it will therefore be difficult to diffuse out of the oocyte or be readily digested by lysosomal enzymes [27]. Cells that are routinely in contact with PVP exhibited increased mucoid secretion as a result of the interaction between this agent and the cell cytoplasm [45]. PVP is likely, therefore, to be present in the inner cell mass and trophectoderm, and be transferred to organs and tissue of the fetus and induce cell death as a result of organelle damage. Previously, our studies showed that PVP injection reduced the cell number of blastocysts [30]. The number of trophectoderm cells is related to pregnancy and implantation in human ART [46]. In clinical reports describing ICSI with or without PVP, the mean averages of clinical pregnancy rates were 47.4 % [47, 48, 49] and 33.1 % (Table 1), respectively. Moreover, the application of PVP conveys potential embryonic toxicity which may result in chromosomal abnormalities [27]. It has been reported that chromosomal abnormalities in ICSI‐derived pregnancies might be related to the inclusion of PVP during the ICSI procedure [39]. These data imply a hazardous risk that PVP impedes blastocyst quality and pregnancy, and might induce the miscarriage of ICSI embryos. On the other hand, spontaneous abortion among 29–39 years olds was approximately 10–25 % [50], and the rate amongst IVF and ICSI cases was 11.5–12.3 and 10.6–12.3 % in the UK between 2002 and 2005, respectively [51, 52, 53, 54]. There were no differences in abortion rates among natural, IVF and ICSI cases. Therefore, we concluded that while spontaneous abortion is not induced by human ART, it is possible that PVP retained within ICSI embryos may induce miscarriage during pregnancy.
The use of immobilization media without PVP for ICSI in clinical treatment
HA is an anionic, nonsulfated glycosaminoglycan distributed widely throughout connective, epithelial, and neural tissues. Hyaluronan contributes significantly to cell proliferation and migration in the extracellular matrix [55]. Polymers of hyaluronan range in size from 5,000 to 20,000,000 Da in vivo. [56]. Hyaluronate is degraded to natural sugar molecules that can be metabolized readily by normal cellular biochemical pathways by lysosomes [57]. Moreover, the selection of normal sperm by hyaluronic acid binding assays might help to reduce early embryonic mortality due to chromosomal aberration [58]. We reviewed the effect of HA and PVP as sperm handling solutions during ICSI treatments (Table 5). There were no differences between the fertilization and pregnancy rate following PVP‐ICSI and HA‐ICSI. These data suggested that hyaluronate could become a direct replacement for PVP, as a natural and readily degradable glycosaminoglycan [58].
Table 5.
The risk of PVP and HA during ICSI treatments
| Report A [109] | Report B [108] | Report C [88] | Report D [90] | |||||
|---|---|---|---|---|---|---|---|---|
| Group HA | Group PVP | Group HA | Group PVP | Group HA | Group PVP | Group HA | Group PVP | |
| Number of cycles | 58 | 65 | 48 | 44 | 125 | 107 | ||
| Fertilization rate a | 72.6 % (525/723) | 74.6 % (484/649) | 72 % (360/499) | 75 % (337/449) | 91.6 % (304/332) | 85.8 % (236/275) | 93.4 % (874/936) | 87.1 % (223/256) |
| Clinical pregnancy rate b | 50 % (29/58) | 38.5 % (25/65) | 41.7 % (20/48 ) | 43.2 % (19/44) | 24.8 % (31/125) | 20.9 % (22/105) | 32.8 % (107/326) | 21.6 % (21/96) |
| Implantation rate c | 18.6 % (41/221) | 14.0 % (35/250) | 18.1 % (27/149) | 19.1 % (27/141) | 12.4 % (35/282) | 10.2 % (23/226) | 17.1 % (133/778) | 10.3 % (22/213) |
aFertilized oocytes per injected metaphase II cumulus–oocytecomplex
bThe number of pregnancy per embryo transferred
cTnumber of gestation sacs per embryo transferred
Sperm immobilization medium that was devoid of PVP has been used to perform ICSI in Kato Ladies’ Clinic and their associated clinical groups. Fertilization and blastocyst rates were more than 80 and 50 %, and clinical pregnancy rates exceeded 40 % [47, 48, 49]. These clinics have helped many infertile couples and resulted in the birth of more 20,000 children. PVP‐free solution would require the high level technique of sperm immobilization and manipulation and improve the technique of human embryologist. These technical improvements could increase the embryo quality and pregnancy rate. The embryologists should select a lower concentration of PVP solution for ICSI treatment, and undergo effective training in order to perform future ICSI cycles without PVP. For direct and indirect reasons, the success rate of fertilization and clinical pregnancy in human ICSI may be improved by using PVP‐free solution during ICSI.
Conclusion
PVP can cause significant damage to sperm membranes and induce the acrosome reaction and reduce fertilization rate. Moreover, PVP remained detectable in IVF embryos, suppressed embryo development, and reduced the number of cells at the blastocyst stage. Clinical pregnancy rates of ICSI using sperm immobilization without PVP exhibited high rates. Miscarriage might be related to the injection of sperm with PVP during human ICSI. On the other hand, the immobilization of sperm in PVP‐free media for ICSI is difficult for junior or trainee embryologists. Sperm immobilization in PVP‐free media could be beneficial for the technical improvements, embryo quality and pregnancy rate in the hands of an experienced embryologist.
Acknowledgments
The authors thank Genetics Hokkaido Co., Ltd for providing frozen semen and Chikusei Meat Center and Nakao Chikusan Co., Ltd. for providing the ovaries used in this study.
Open Access
This article is distributed under the terms of the http://creativecommons.org/licenses/by/3.0/ License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
References
- 1. Sanner AHF, Straub F. Polymers of N‐vinylpyrrolidone: synthesis, characterization and uses. Polym J, 1985, 17, 143–152 10.1295/polymj.17.143 [Google Scholar]
- 2. Das SK, Saha SK, Das A, Halder AK, Banerjee SN, Chakraborty M. A study of comparison of efficacy and safety of talc and povidone iodine for pleurodesis of malignant pleural effusions. J Indian Med Assoc, 2008, 106, 589–590 [PubMed] [Google Scholar]
- 3. Yoshida K, Sakurai Y, Kawahara S, Takeda T, Ishikawa T, Murakami T, Yoshioka A. Anaphylaxis to polyvinylpyrrolidone in povidone‐iodine for impetigo contagiosum in a boy with atopic dermatitis. Int Arch Allergy Immunol, 2008, 146, 169–173 10.1159/000113522 [DOI] [PubMed] [Google Scholar]
- 4. Adachi A, Fukunaga A, Hayashi K, Kunisada M, Horikawa T. Anaphylaxis to polyvinylpyrrolidone after vaginal application of povidone‐iodine. Contact Dermat, 2003, 48, 133–136 10.1034/j.1600‐0536.2003.00050.x [DOI] [PubMed] [Google Scholar]
- 5. Rönnau AC, Wulferink M, Gleichmann E, Unver E, Ruzicka T, Krutmann J, Grewe M. Anaphylaxis to polyvinylpyrrolidone in an analgesic preparation. British J Dermatol, 2000, 143, 1055–1058 10.1046/j.1365‐2133.2000.03843.x [DOI] [PubMed] [Google Scholar]
- 6. Quartier S, Garmyn M, Becart S, Goossens A. Allergic contact dermatitis to copolymers in cosmetics–case report and review of the literature. Contact Dermat, 2006, 55 (5) 257–267 10.1111/j.1600‐0536.2006.00960.x [DOI] [PubMed] [Google Scholar]
- 7. Ketel WG, Berg WH. Sensitization to povidone–iodine. Dermatol Clin, 1990, 8, 107–109 [PubMed] [Google Scholar]
- 8. Steirteghem AC, Nagy Joris H, Liu J, Staessen C, Smitz J, Wisanto A, Devroey P et al. High fertilization and implantation rates after intracytoplasmic sperm injection. Hum Reprod, 1993, 8, 1061–1066 [DOI] [PubMed] [Google Scholar]
- 9. Suzuki T, Saha S, Sumantri C, Takagi M, Boediono A. The influence of polyvinylpyrrolidone on freezing of bovine IVF blastocysts following biopsy. Cryobiology, 1995, 32, 505–510 10.1006/cryo.1995.1051 [DOI] [PubMed] [Google Scholar]
- 10. Kaneko S, Oshio S, Kobanawa K, Kobayashi T, Mohri H, Iizuka R. Purification of human sperm by a discontinuous Percoll density gradient with an innercolumn. Biol Reprod, 1986, 35, 1059–1063 10.1095/biolreprod35.4.1059 [DOI] [PubMed] [Google Scholar]
- 11. Saeki K, Hoshi M, Leibfried‐Rutledge ML, First NL. In vitro fertilization and development of bovine oocytes matured in serum‐free medium. Biol Reprod, 1991, 44, 256–260 10.1095/biolreprod44.2.256 [DOI] [PubMed] [Google Scholar]
- 12. Nagao Y, Ohta Y, Murakami H, Kato Y. The effects of methyl‐β‐cyclodextrin on in vitro fertilization and the subsequent development of bovine oocytes. Zygote, 2010, 18, 323–330 10.1017/S0967199409990396 [DOI] [PubMed] [Google Scholar]
- 13. Haidri AA, Miller IM, Gwatkin RB. Culture of mouse oocytes in vitro, using a system without oil or protein. J Reprod Fertil, 1971, 26, 409–411 10.1530/jrf.0.0260409 [DOI] [PubMed] [Google Scholar]
- 14. Hirao Y, Itoh T, Shimizu M, Iga K, Aoyagi K, Kobayashi M, Kacchi M, Hoshi H, Takenouchi N. In vitro growth and development of bovine oocyte‐granulosa cell complexes on the flat substratum: effects of high polyvinylpyrrolidone concentration in culture medium. Biol Reprod, 2004, 70, 83–91 10.1095/biolreprod.103.021238 [DOI] [PubMed] [Google Scholar]
- 15. Kimura Y, Yanagimachi R. Intracytoplasmic sperm injection in the mouse. Biol Reprod, 1995, 52, 709–720 10.1095/biolreprod52.4.709 [DOI] [PubMed] [Google Scholar]
- 16. Hamano K, Li X, Funauchi K, Furudate M, Minato Y. Gender preselection in cattle with intracytoplasmically injected, flowcytometrically sorted sperm heads. Biol Reprod, 1999, 60, 1194–1197 10.1095/biolreprod60.5.1194 [DOI] [PubMed] [Google Scholar]
- 17. Catt SL, Catt JW, Gomez MC, Maxwell WM, Evans G. Birth of a male lamb derived from an in vitro matured oocyte fertilised by intracytoplasmic injection of a single presumptive male sperm. Vet Rec, 1996, 139, 494–495 10.1136/vr.139.20.494 [DOI] [PubMed] [Google Scholar]
- 18. Cochran R, Meintjes M, Reggio B, Hylan D, Carter J, Pinto C, Paccamonti D, Godke RA. Livefoals produced from sperm‐injected oocytes derived from pregnant mares. J Equine Vet Sci, 1998, 18, 736–740 10.1016/S0737‐0806(98)80504‐2 [Google Scholar]
- 19. Martin MJ. Development of in vivo‐matured porcine oocytes following intracytoplasmic sperm injection. Biol Reprod, 2000, 63, 109–112 10.1095/biolreprod63.1.109 [DOI] [PubMed] [Google Scholar]
- 20. Gianaroli L, Plachot M, Kooij R, Al‐Hasani S, Dawson K, DeVos A, Magli MC, Mandelbaum J, Selva J, van Inzen W. ESHRE guidelines for good practice in IVF laboratories. Committee of the Special Interest Group on Embryology of the European Society of Human Reproduction and Embryology. Hum Reprod, 2000, 15, 2241–2246 10.1093/humrep/15.10.2241 [DOI] [PubMed] [Google Scholar]
- 21. Hlinka D, Herman M, Vesela J, Hredzak R, Horvath S, Pacin J. A modified method of intracytoplasmic sperm injection without the use of polyvinylpyrrolidone. Hum Reprod, 1998, 13, 1922–1927 10.1093/humrep/13.7.1922 [DOI] [PubMed] [Google Scholar]
- 22. Palermo GD, Joris H, Devroey P, Steirteghem AC et al. Pregnancies after intracytoplasmic sperm injection of a single spermatozoon into an oocyte. Lancet, 1992, 340, 17–18 10.1016/0140‐6736(92)92425‐F [DOI] [PubMed] [Google Scholar]
- 23. Strehler E, Baccetti B, Sterzik K, Capitani S, Collodel G, Santo DM, Gambera L, Piomboni P. Detrimental effects of polyvinylpyrrolidone on the ultrastructure of spermatozoa. Hum Reprod, 1998, 13, 120–123 10.1093/humrep/13.1.120 [DOI] [PubMed] [Google Scholar]
- 24. Arcidiacono A, Walt H, Campana A, Balerna M. The use of Percoll gradients for the preparation of subpopulations of human spermatozoa. Int J Androl, 1983, 6, 433–445 10.1111/j.1365‐2605.1983.tb00558.x [DOI] [PubMed] [Google Scholar]
- 25. Dorzortsev D, Sutter P, Rybouchkin A, Dhont M. Sperm plasma membrane damage prior to intracytoplasmic sperm injection: a necessary condition for sperm nucleus. Assit Reprod Rev, 1995, 5, 32–39 [DOI] [PubMed] [Google Scholar]
- 26. Dozortsev D, Rybouchkin A, Sutter P, Dhont M. Sperm plasma membrane damage prior to intracytoplasmic sperm injection: a necessary condition for sperm nucleus decondensation. Hum Reprod, 1995, 10, 2960–2964 [DOI] [PubMed] [Google Scholar]
- 27. Jean M, Mirallié S, Boudineau M, Tatin C, Barrière P. Intracytoplasmic sperm injection with polyvinylpyrrolidone: a potential risk. Fertil Steril, 2001, 76, 419–420 10.1016/S0015‐0282(01)01874‐X [DOI] [PubMed] [Google Scholar]
- 28. de Mouzon J, Goossens V, Bhattacharya S, Castilla JA, Ferraretti AP, Korsak V, Kupka M, Nygren KG, Andersen AN. Assisted reproductive technology in Europe, 2006: results generated from European registers by ESHRE. Hum Reprod, 2010, 25, 1851–1862 10.1093/humrep/deq124 [DOI] [PubMed] [Google Scholar]
- 29. Morozumi K, Shikano T, Miyazaki S, Yanagimachi R. Simultaneous removal of sperm plasma membrane and acrosome before intracytoplasmic sperm injection improves oocyte activation/embryonic development. Proc Natl Acad Sci USA, 2006, 103, 17661–17666 10.1073/pnas.0608183103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kato Y, Nagao Y. Effect of PVP on sperm capacitation status and embryonic development in cattle. Theriogenology, 2009, 72, 624–635 10.1016/j.theriogenology.2009.04.018 [DOI] [PubMed] [Google Scholar]
- 31. Parrish JJ, Susko‐Parrish JL, Graham JK. In vitro capacitation of bovine spermatozoa: role of intracellular calcium. Theriogenology, 1999, 51, 461–472 10.1016/S0093‐691X(98)00240‐4 [DOI] [PubMed] [Google Scholar]
- 32. Spungin B, Breitbart H. Calcium mobilization and influx during sperm exocytosis. J Cell Sci, 1996, 109, 1947–1955 [DOI] [PubMed] [Google Scholar]
- 33. Florman HM, Arnoult C, Kazam IGLC, O'Toole CM. A perspective on the control of mammalian fertilization by egg activated ion channels in sperm: a tale of two channels. Biol Reprod, 1998, 59, 12–16 10.1095/biolreprod59.1.12 [DOI] [PubMed] [Google Scholar]
- 34. Dragileva E, Rubinstein S, Breitbart H. Intracellular Ca(2+)–Mg(2+)‐ATPase regulates calcium influx and acrosomal exocytosis in bull and ram spermatozoa. Biol Reprod, 1999, 61, 1226–1234 10.1095/biolreprod61.5.1226 [DOI] [PubMed] [Google Scholar]
- 35. Suarez SS. Interactions of spermatozoa with the female reproductive tract: inspiration for assisted reproduction. Reprod Fertil Dev, 2007, 19, 103–110 10.1071/RD06101 [DOI] [PubMed] [Google Scholar]
- 36.WHO Health Organization. Organization laboratory manual for the examination of human semen and sperm‐cervical mucus interaction, 4. Cambridge: Cambridge University Press; 1999.
- 37. Yanagida K, Katayose H, Hirata S, Yazawa H, Hayashi S, Sato A. Influence of sperm immobilization on onset of Ca(2+) oscillations after ICSI. Hum Reprod, 2001, 16, 148–152 10.1093/humrep/16.1.148 [DOI] [PubMed] [Google Scholar]
- 38. Ozil JP, Banrezes B, Toth S, Pan H, Schultz RM. Ca2+ oscillatory pattern in fertilized mouse eggs affects gene expression and development to term. Dev Biol, 2006, 300, 534–544 10.1016/j.ydbio.2006.08.041 [DOI] [PubMed] [Google Scholar]
- 39. Tremoleda JL, Stout TA, Lagutina I, Lazzari G, Bevers MM, Colenbrander B, Galli C. Effect of in vitro production on horse embryo morphology, cytoskeletal characteristic, and blastocysts capsule formation. Biol Reprod, 2003, 69, 1895–1906 10.1095/biolreprod.103.018515 [DOI] [PubMed] [Google Scholar]
- 40. Feichtinger W, Obruca A, Brunner M. Sex chromosomal abnormalities and intracytoplasmic sperm injection. Lancet, 1995, 346, 1566 10.1016/S0140‐6736(95)92098‐6 [DOI] [PubMed] [Google Scholar]
- 41. Mizuno K, Hoshi K, Huang T. Fertilization and embryo development in a mouse ICSI model using human and mouse sperm after immobilization in polyvinylpyrrolidone. Hum Reprod, 2002, 17, 2350–2355 10.1093/humrep/17.9.2350 [DOI] [PubMed] [Google Scholar]
- 42. Bras M, Dumoulin JCM, Pieters MHEC, Michaels AHJC, Geraedts JPM, Evers JLH. The use of a mouse zygote quality control system for training purposes and toxicity determination in an ICSI programme. Hum Reprod, 1994, 9, 23–24 [Google Scholar]
- 43. Nagao Y, Saeki K, Hoshi M, Takahashi Y, Kanagawa H. Effects of water quality on in vitro fertilization and development of bovine oocytes in protein‐free medium. Theriogenology, 1995, 44, 433–444 10.1016/0093‐691X(95)00197‐G [DOI] [PubMed] [Google Scholar]
- 44. Motoishi M, Goto K, Tomita K, Ookutsu S, Nakanishi Y. Examination of the safety of intracytoplasmic injection procedures by using bovine zygotes. Hum Reprod, 1996, 11, 618–620 10.1093/HUMREP/11.3.618 [DOI] [PubMed] [Google Scholar]
- 45. Kepes JJ, Chen WY, Jim YF. “Mucoid dissolution” of bones and multiple pathologic fractures in a patient with past history of intravenous administration of polyvinylpyrrolidone (PVP). A case report. Bone Miner, 1993, 22, 33–41 10.1016/S0169‐6009(08)80079‐7 [DOI] [PubMed] [Google Scholar]
- 46. Ahlström A, Westin C, Reismer E, Wikland M, Hardarson T. Trophectoderm morphology: an important parameter for predicting live birth after single blastocyst transfer. Hum Reprod, 2011, 26, 3289–3296 10.1093/humrep/der325 [DOI] [PubMed] [Google Scholar]
- 47. Kuwayama M, Vajta G, Kato O, Leibo SP. Highly efficient vitrification method for cryopreservation of human oocytes. Reprod Biomed Online, 2005, 11, 300–308 10.1016/S1472‐6483(10)60837‐1 [DOI] [PubMed] [Google Scholar]
- 48. Kuwayama M, Vajta G, Ieda S, Kato O. Comparison of open and closed methods for vitrification of human embryos and the elimination of potential contamination. Reprod Biomed Online, 2005, 11, 608–614 10.1016/S1472‐6483(10)61169‐8 [DOI] [PubMed] [Google Scholar]
- 49. Teramoto S, Kato O. Minimal ovarian stimulation with clomiphene citrate: a large‐scale retrospective study. Reprod Biomed Online, 2007, 15, 134–148 10.1016/S1472‐6483(10)60701‐8 [DOI] [PubMed] [Google Scholar]
- 50. Heffner LJ. Advanced maternal age—how old is too old?. N Engl J Med, 2004, 351, 1927–1929 10.1056/NEJMp048087 [DOI] [PubMed] [Google Scholar]
- 51.European IVF‐monitoring programme (EIM) for the European Society of Human Reproduction and Embryology (ESHRE), Andersen AN, Gianaroli L, Felberbaum R, de Mouzon J, Nygren KG. Assisted reproductive technology in Europe, 2002. Results generated from European registers by ESHRE. Hum Reprod. 2006;21:1680–97. [DOI] [PubMed]
- 52. Andersen AN, Goossens V, Gianaroli L, Felberbaum R, Mouzon J, Nygren KG et al. Assisted reproductive technology in Europe, 2003 Results generated from European registers by ESHRE. Hum Reprod, 2006, 2007 (22) 1513–1525 [DOI] [PubMed] [Google Scholar]
- 53. Andersen AN, Goossens V, Ferraretti AP, Bhattacharya S, Felberbaum R, Mouzon J, Nygren KG. European IVF‐monitoring (EIM) Consortium; European Society of Human Reproduction and Embryology (ESHRE). Assisted reproductive technology in Europe, 2004: results generated from European registers by ESHRE. Hum Reprod, 2008, 23, 756–771 10.1093/humrep/den014 [DOI] [PubMed] [Google Scholar]
- 54. Andersen AN, Goossens V, Bhattacharya S, Ferraretti AP, Kupka MS, Mouzon J et al. European IVF‐monitoring (EIM) Consortium, for the European Society of Human Reproduction and Embryology (ESHRE). Assisted reproductive technology and intrauterine inseminations in Europe, 2005: results generated from European registers by ESHRE: ESHRE. The European IVF Monitoring Programme (EIM), for the European Society of Human Reproduction and Embryology (ESHRE). Hum Reprod, 2009, 24, 1267–1287 10.1093/humrep/dep035 [DOI] [PubMed] [Google Scholar]
- 55. Fraser JR, Laurent TC, Laurent UB. Hyaluronan: its nature, distribution, functions and turnover. J Intern Med, 1997, 242, 27–33 10.1046/j.1365‐2796.1997.00170.x [DOI] [PubMed] [Google Scholar]
- 56. Saari H, Konttinen YT, Friman C, Sorsa T. Differential effects of reactive oxygen species on 31 native synovial fluid and purified human umbilical cord hyaluronate. Inflammation, 1993, 17 (498) 403–415 10.1007/BF00916581 [DOI] [PubMed] [Google Scholar]
- 57.Roden L. Structure and metabolism of connective tissue proteoglycan. In: Lennarz WJ, editor. The biochemistry of glycoproteins and proteoglycans. New York: Plenum Press; 1980. p. 254–75.
- 58. Huszar G, Ozenci CC, Cayli S, Zavaczki Z, Hansch E, Vigue L. Hyaluronic acid binding by human sperm indicates cellular maturity, viability, and unreacted acrosomal status. Fertil Steril, 2003, 79 (Suppl 3) 1616–1624 10.1016/S0015‐0282(03)00402‐3 [DOI] [PubMed] [Google Scholar]
- 59. Chia CM, Chan WB, Quah E, Cheng LC. Triploid pregnancy after ICSI of frozen testicular spermatozoa into cryopreserved human oocytes: case report. Hum Reprod, 2000, 15, 1962–1964 10.1093/humrep/15.9.1962 [DOI] [PubMed] [Google Scholar]
- 60. Manno M, Marchesan E, Crovatto M, Martelli P, Tomei F, Adamo V. Preliminary evidence on the safety of ICSI with testicular spermatozoa in HCV‐infected male: a case report. Hum Reprod, 2003, 18, 1666–1668 10.1093/humrep/deg324 [DOI] [PubMed] [Google Scholar]
- 61. Meseguer M, Garrido N, Remohí J, Pellicer A, Simón C, Martínez Jabaloyas JM, Gil‐Salom M et al. Testicular sperm extraction (TESE) and ICSI in patients with permanent azoospermia after chemotherapy. Hum Reprod, 2003, 18, 1281–1285 10.1093/humrep/deg260 [DOI] [PubMed] [Google Scholar]
- 62. Alikani M, Palermo G, Adler A, Bertoli M, Blake M, Cohen J. Intracytoplasmic sperm injection in dysmorphic human oocytes. Zygote, 1995, 3, 283–288 10.1017/S0967199400002707 [DOI] [PubMed] [Google Scholar]
- 63. Murase Y, Araki Y, Mizuno S, Kawaguchi C, Naito M, Yoshizawa M, Araki Y. Pregnancy following chemical activation of oocytes in a couple with repeated failure of fertilization using ICSI: case report. Hum Reprod, 2004, 19, 1604–1607 10.1093/humrep/deh294 [DOI] [PubMed] [Google Scholar]
- 64. Hashimoto S, Murata Y, Kikkawa M, Sonoda M, Oku H, Murata T, Sugihara K, Nagata F, Nakaoka Y, Fukuda A, Morimoto Y. Successful delivery after the transfer of twice‐vitrified embryos derived from in vitro matured oocytes: a case report. Hum Reprod, 2007, 22, 221–223 10.1093/humrep/del354 [DOI] [PubMed] [Google Scholar]
- 65. Vos A, Landuyt L, Ranst H, Vandermonde A, D'Haese V, Sterckx J, Haentjens P, Devroey P, Elst J. Randomized sibling‐oocyte study using recombinant human hyaluronidase versus bovine‐derived Sigma hyaluronidase in ICSI patients. Hum Reprod, 2008, 23, 1815–1819 10.1093/humrep/den212 [DOI] [PubMed] [Google Scholar]
- 66. Taylor TH, Elliott T, Colturato LF, Straub RJ, Mitchell‐Leef D, Nagy ZP. Comparison of bovine‐ and recombinant human‐derived hyaluronidase with regard to fertilization rates and embryo morphology in a sibling oocyte model: a prospective, blinded, randomized study. Fertil Steril, 2006, 85, 1544–1546 10.1016/j.fertnstert.2005.10.053 [DOI] [PubMed] [Google Scholar]
- 67. Vanderzwalmen P, Hiemer A, Rubner P, Bach M, Neyer A, Stecher A, Uher P, Zintz M, Lejeune B, Vanderzwalmen S, Cassuto G, Zech NH. Blastocyst development after sperm selection at high magnification is associated with size and number of nuclear vacuoles. Reprod Biomed Online, 2008, 17, 617–627 10.1016/S1472‐6483(10)60308‐2 [DOI] [PubMed] [Google Scholar]
- 68. Hauser R, Yogev L, Amit A, Yavetz H, Botchan A, Azem F, Lessing JB, Ben‐Yosef D. Severe hypospermatogenesis in cases of nonobstructive azoospermia: should we use fresh or frozen testicular spermatozoa?. J Androl, 2005, 26, 772–778 10.2164/jandrol.05044 [DOI] [PubMed] [Google Scholar]
- 69. Bonduelle M, Wennerholm UB, Loft A, Tarlatzis BC, Peters C, Henriet S, Mau C, Victorin‐Cederquist A, Van Steirteghem A, Balaska A, Emberson JR, Sutcliffe AG et al. A multi‐centre cohort study of the physical health of 5‐year‐old children conceived after intracytoplasmic sperm injection, in vitro fertilization and natural conception. Hum Reprod, 2005, 20, 413–419 10.1093/humrep/deh592 [DOI] [PubMed] [Google Scholar]
- 70. Sbracia M, Colabianchi J, Giallonardo A, Giannini P, Piscitelli C, Morgia F, Montigiani M, Schimberni M. Cetrorelix protocol versus gonadotropin‐releasing hormone analog suppression long protocol for superovulation in intracytoplasmic sperm injection patients older than 40. Fertil Steril, 2009, 91, 1842–1847 10.1016/j.fertnstert.2008.02.165 [DOI] [PubMed] [Google Scholar]
- 71. Verpoest W, Rademaeker M, Sermon K, Rycke M, Seneca S, Papanikolaou E, Spits C, Landuyt L, Elst J, Haentjens P, Devroey P, Liebaers I. Real and expected delivery rates of patients with myotonic dystrophy undergoing intracytoplasmic sperm injection and 561 preimplantation genetic diagnosis. Hum Reprod, 2008, 23, 1654–1660 10.1093/humrep/den105 [DOI] [PubMed] [Google Scholar]
- 72. Ahmady A, Michael E. Successful pregnancy and delivery following intracytoplasmic injection of frozen‐thawed nonviable testicular sperm and oocyte activation with calcium ionophore. J Androl, 2007, 28, 13–14 10.2164/jandrol.106.000174 [DOI] [PubMed] [Google Scholar]
- 73. Miller JE, Smith TT. The effect of intracytoplasmic sperm injection and semen parameters on blastocyst development in vitro. Hum Reprod, 2001, 16, 918–924 10.1093/humrep/16.5.918 [DOI] [PubMed] [Google Scholar]
- 74. Rienzi L, Ubaldi F, Anniballo R, Cerulo G, Greco E. Preincubation of human oocytes may improve fertilization and embryo quality after intracytoplasmic sperm injection. Hum Reprod, 1998, 13, 1014–1019 10.1093/humrep/13.4.1014 [DOI] [PubMed] [Google Scholar]
- 75. Wood S, Sephton V, Searle T, Thomas K, Schnauffer K, Troup S, Kingsland C, Lewis‐Jones I. Effect on clinical outcome of the interval between collection of epididymal and testicular spermatozoa and intracytoplasmic sperm injection in obstructive azoospermia. J Androl, 2003, 24, 67–72 [PubMed] [Google Scholar]
- 76. Yang WJ, Hwu YM, Lee RK, Li SH, Fleming S. Early‐cleavage is a reliable predictor for embryo implantation in the GnRH agonist protocols but not in the GnRH antagonist protocols. Reprod Biol Endocrinol, 2009, 7, 20 10.1186/1477‐7827‐7‐20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Nasr‐Esfahani MH, Razavi S, Javdan Z, Tavalaee M. Artificial oocyte activation in severe teratozoospermia undergoing intracytoplasmic sperm injection. Fertil Steril, 2008, 90, 2231–2237 10.1016/j.fertnstert.2007.10.047 [DOI] [PubMed] [Google Scholar]
- 78. Heindryckx B, Gheselle S, Gerris J, Dhont M, Sutter P. Efficiency of assisted oocyte activation as a solution for failed intracytoplasmic sperm injection. Reprod Biomed Online, 2008, 17, 662–668 10.1016/S1472‐6483(10)60313‐6 [DOI] [PubMed] [Google Scholar]
- 79. Verza S Jr, Esteves SC. Sperm defect severity rather than sperm source is associated with lower fertilization rates after intracytoplasmic sperm injection. Int Braz J Urol, 2008, 34, 49–56 10.1590/S1677‐55382008000100008 [DOI] [PubMed] [Google Scholar]
- 80. Noorashikin M, Ong FB, Omar MH, Zainul‐Rashid MR, Murad AZ, Shamsir A, Norsina MA, Nurshaireen A, Sharifah‐Teh NS, Fazilah AH. Affordable ART for developing countries: a cost benefit comparison of low dose stimulation versus high dose GnRH antagonist protocol. J Assist Reprod Genet, 2008, 25, 297–303 10.1007/s10815‐008‐9239‐9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Rashid MR, Ong FB, Omar MH, Ng SP, Nurshaireen A, Sharifah‐Teh NS, Fazilah AH, Zamzarina MA. GnRH agonist and GnRH antagonist in intracytoplasmic injection cycles. Med J Malaysia, 2008, 63, 113–117 [PubMed] [Google Scholar]
- 82. Yanagida K, Morozumi K, Katayose H, Hayashi S, Sato A. Successful pregnancy after ICSI with strontium oocyte activation in low rates of fertilization. Reprod Biomed Online, 2006, 13, 801–806 10.1016/S1472‐6483(10)61027‐9 [DOI] [PubMed] [Google Scholar]
- 83. Yanagida K, Katayose H, Yazawa H, Kimura Y, Sato A, Yanagimachi H, Yanagimachi R. Successful fertilization and pregnancy following ICSI and electrical oocyte activation. Hum Reprod, 1999, 14, 1307–1311 10.1093/humrep/14.5.1307 [DOI] [PubMed] [Google Scholar]
- 84. Huang CC, Cheng TC, Chang HH, Chang CC, Chen CI, Liu J, Lee MS. Birth after the injection of sperm and the cytoplasm of tripronucleate zygotes into metaphase II oocytes in patients with repeated implantation failure after assisted fertilization procedures. Fertil Steril, 1999, 72, 702–706 10.1016/S0015‐0282(99)00309‐X [DOI] [PubMed] [Google Scholar]
- 85. Lewin A, Weiss DB, Friedler S, Ben‐Shachar I, Porat‐Katz A, Meirow D, Schenker JG, Safran A. Delivery following intracytoplasmic injection of mature sperm cells recovered by testicular fine needle aspiration in a case of hypergonadotropic azoospermia due to maturation arrest. Hum Reprod, 1996, 11, 769–771 10.1093/oxfordjournals.humrep.a019252 [DOI] [PubMed] [Google Scholar]
- 86. Nagy ZP, Verheyen G, Tournaye H, Steirteghem CA et al. Special applications of intracytoplasmic sperm injection: the influence of sperm count, motility, morphology, source and sperm antibody on the outcome of ICSI. Hum Reprod, 1998, 13, 143–154 10.1093/humrep/13.suppl_1.143 [DOI] [PubMed] [Google Scholar]
- 87. Yoshimoto‐Kakoi T, Terada Y, Tachibana M, Murakami T, Yaegashi N, Okamura K. Assessing centrosomal function of infertile males using heterologous ICSI. Syst Biol Reprod Med, 2008, 54, 135–142 10.1080/19396360802043091 [DOI] [PubMed] [Google Scholar]
- 88. Parmegiani L, Cognigni GE, Bernardi S, Troilo E, Ciampaglia W, Filicori M. “Physiologic ICSI”: hyaluronic acid (HA) favors selection of spermatozoa without DNA fragmentation and with normal nucleus, resulting in improvement of embryo quality. Fertil Steril, 2010, 93, 598–604 10.1016/j.fertnstert.2009.03.033 [DOI] [PubMed] [Google Scholar]
- 89. Volpes A, Sammartano F, Coffaro F, Mistretta V, Scaglione P, Allegra A. Number of good quality embryos on day 3 is predictive for both pregnancy and implantation rates in in vitro fertilization/intracytoplasmic sperm injection cycles. Fertil Steril, 2004, 82, 1330–1336 10.1016/j.fertnstert.2004.03.067 [DOI] [PubMed] [Google Scholar]
- 90. Parmegiani L, Cognigni GE, Ciampaglia W, Pocognoli P, Marchi F, Filicori M. Efficiency of hyaluronic acid (HA) sperm selection. J Assist Reprod Genet, 2010, 27, 13–16 10.1007/s10815‐009‐9380‐0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Sousa M, Cremades N, Silva J, Oliveira C, Ferraz L, Teixeira da Silva J, Viana P, Barros A et al. Predictive value of testicular histology in secretory azoospermic subgroups and clinical outcome after microinjection of fresh and frozen‐thawed sperm and spermatids. Hum Reprod, 2002, 17, 1800–1810 10.1093/humrep/17.7.1800 [DOI] [PubMed] [Google Scholar]
- 92. Pinto F, Oliveira C, Cardoso MF, Teixeira‐da‐Silva J, Silva J, Sousa M, Barros A. Impact of GnRH ovarian stimulation protocols on intracytoplasmic sperm injection outcomes. Reprod Biol Endocrinol, 2009, 7, 5 10.1186/1477‐7827‐7‐5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Dumoulin JC, Coonen E, Bras M, Wissen LC, Ignoul‐Vanvuchelen R, Bergers‐Jansen JM, Derhaag JG, Geraedts JP, Evers JL. Comparison of in vitro development of embryos originating from either conventional in vitro fertilization or intracytoplasmic sperm injection. Hum Reprod, 2000, 15, 402–409 10.1093/humrep/15.2.402 [DOI] [PubMed] [Google Scholar]
- 94. Mitchell V, Rives N, Albert M, Peers MC, Selva J, Clavier B, Escudier E, Escalier D. Outcome of ICSI with ejaculated spermatozoa in a series of men with distinct ultrastructural flagellar abnormalities. Hum Reprod, 2006, 21, 2065–2074 10.1093/humrep/del130 [DOI] [PubMed] [Google Scholar]
- 95. Rives N, Sibert L, Clavier B, Delabroye V, Marpeau L, Macé B. Full‐term delivery following intracytoplasmic sperm injection with frozen‐thawed immotile testicular spermatozoa. Hum Reprod, 1998, 13, 3399–3401 10.1093/humrep/13.12.3399 [DOI] [PubMed] [Google Scholar]
- 96. Schmiady H, Tandler‐Schneider A, Kentenich H. Premature chromosome condensation of the sperm nucleus after intracytoplasmic sperm injection. Hum Reprod, 1996, 11, 2239–2245 10.1093/oxfordjournals.humrep.a019083 [DOI] [PubMed] [Google Scholar]
- 97. Allegra A, Marino A, Coffaro F, Lama A, Rizza G, Scaglione P, Sammartano F, Santoro A, Volpes A. Is there a uniform basal endometrial gene expression profile during the implantation window in women who became pregnant in a subsequent ICSI cycle?. Hum Reprod, 2009, 24, 2549–2557 10.1093/humrep/dep222 [DOI] [PubMed] [Google Scholar]
- 98. Nicopoullos JD, Gilling‐Smith C, Almeida PA, Homa S, Nice L, Tempest H, Ramsay JW. The role of sperm aneuploidy as a predictor of the success of intracytoplasmic sperm injection?. Hum Reprod, 2008, 23, 240–250 10.1093/humrep/dem395 [DOI] [PubMed] [Google Scholar]
- 99. Nasr‐Esfahani MH, Razavi S, Mozdarani H, Mardani M, Azvagi H. Relationship between protamine deficiency with fertilization rate and incidence of sperm premature chromosomal condensation post‐ICSI. Andrologia, 2004, 36, 95–100 10.1111/j.1439‐0272.2004.00612.x [DOI] [PubMed] [Google Scholar]
- 100. Alosilla Fonttis A, Napolitano R, Tomás MA. Successful ICSI in a case of severe asthenozoospermia due to 93% non‐specific axonemal alterations and 90% abnormal or absent mitochondrial sheaths. Reprod Biomed Online, 2002, 5, 270–272 10.1016/S1472‐6483(10)61831‐7 [DOI] [PubMed] [Google Scholar]
- 101. Madaschi C, Aoki T, de Almeida Ferreira Braga DP, de Cássia Sávio Figueira R, Semião Francisco L, Iaconelli A Jr, Borges E Jr et al. Zona pellucida birefringence score and meiotic spindle visualization in relation to embryo development and ICSI outcomes. Reprod Biomed Online, 2009, 18, 681–686 10.1016/S1472‐6483(10)60014‐4 [DOI] [PubMed] [Google Scholar]
- 102. Casper RF, Meriano JS, Jarvi KA, Cowan L, Lucato ML. The hypo‐osmotic swelling test for selection of viable sperm for intracytoplasmic sperm injection in men with complete asthenozoospermia. Fertil Steril, 1996, 65, 972–976 [DOI] [PubMed] [Google Scholar]
- 103. Li ZL, Lin H, Zhang XN, Xiao WF. Intracytoplasmic sperm injection in cases with history of in vitro fertilization failure. Asian J Androl, 2003, 5, 69–72 [PubMed] [Google Scholar]
- 104. Ma S, Ho Yuen B. Assessment of maximal fertilization rates with intracytoplasmic sperm injection. J Assist Reprod Genet, 2000, 17, 80–86 10.1023/A:1009410331774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. De Cássia Savio Figueira R, Souza Setti A, Paes De Almeida Ferreira Braga D, Iaconelli A Jr, Borges E Jr et al. Blastomere multinucleation: Contributing factors and effects on embryo development and clinical outcome. Hum Fertil, 2010, 13, 143–150 10.3109/14647273.2010.508505 [DOI] [PubMed] [Google Scholar]
- 106. Rosen MP, Shen S, Rinaudo PF, Huddleston HG, McCulloch CE, Cedars MI. Fertilization rate is an independent predictor of implantation rate. Fertil Steril, 2010, 94, 1328–1333 10.1016/j.fertnstert.2009.05.024 [DOI] [PubMed] [Google Scholar]
- 107. Melamed RM, Bonetti TC, Braga DP, Madaschi C, Iaconelli A, Borges E. Deciding the fate of supernumerary frozen embryos: parents’ choices. Hum Fertil, 2009, 12, 185–190 10.3109/14647270903377186 [DOI] [PubMed] [Google Scholar]
- 108. Balaban B, Lundin K, Morrell JM, Tjellström H, Urman B, Holmes PV. An alternative to PVP for slowing sperm prior to ICSI. Hum Reprod, 2003, 18, 1887–1889 10.1093/humrep/deg385 [DOI] [PubMed] [Google Scholar]
- 109. Barak Y, Menezo Y, Veiga A, Elder K. A physiological replacement for polyvinylpyrrolidone (PVP) in assisted reproductive technology. Hum Fertil (Camb)., 2001, 4, 99–103 10.1080/1464727012000199371 [DOI] [PubMed] [Google Scholar]


