A 43 years old married woman presented to a private clinic with repeated episodes of mouth sores. The clinician diagnosed her with oral candida. Her past medical history was significant only for bronchial asthma since childhood. Her asthma had been poorly controlled in the recent few weeks requiring high doses of oral prednisolone and regular salbutamol inhaler. She had been on this treatment for a month when she presented with these sores. She had neither had a blood transfusion nor experimental HIV vaccine. She had had only one sexual partner in her life. The patient requested an HIV test. . The HIV rapid test came out positive. Her family including the husband and two children tested HIV negative. After some discussion, the clinician recommended that she should start ART. She was started on a combination of d4T, 3TC and nevirapine. .
After one year on therapy, she noticed that her arms, thighs and buttocks were becoming slim and her back and stomach were protruding (see picture).
A diagnosis of lipodystrophy was made, and the patient's treatment was changed to AZT/3TC/NVP. She took this regimen for 2 years (2007). In 2008, she developed anaemia thought to be secondary to AZT. As a result her treatment was changed to TDF/3TC/EFV. . She took this regimen faithfully till May 2011. At this time she had her first CD4 cell count and HIV RNA tests.The CD4 cell count was as >800 cell/mL and the HIV RNA was <400 copies/mL. On personal initiative, the patient visited South Africa and underwent a thorough medical examination in May 2011 including HIV testing. The HIV test using rapid tests was negative and a confirmatory Western blot was also negative. HIV RNA was undetectable.
She was informed of the results and advised to stop HIV treatment and return in 3 months for repeat tests. The repeat tests were unchanged. It was concluded that this lady was never HIV positive.
Discussion
With resources from the Global Fund, the Malawi government has been able to start more than 350000 patients on HAART since 2001. More than 250,000 patients remain in care (ART unit quarterly reports). The Malawi ART programme relies on a public health approach for initiation of ART. A positive HIV test is the only required test for patients to start HAART. A positive rapid HIV test does not require confirmatory by a different test method. The rest of the patients' management is purely clinical (using WHO clinical staging) including monitoring treatment success or failure2. Patients with WHO stage 3 and 4 disease are recommended to start therapy immediately. Those in stages 1 and 2 are asked to come back later. In a few clinics, patients in WHO stages 1 and 2 are offered a CD4 count test. Patients with CD4 cell count < 350 cell/ml are eligible to start therapy following the WHO change in guidelines in 20103.
Advantages of using the public health approach in managing HIV
Proponents of the public health approach to management of HIV point to the large numbers of patients that have been tested and put on treatment4. There is no debate as to the success of this policy in reaching large numbers of people within a short time. However, despite this success, this approach has many challenges if the protocols that govern its use are not rigorously followed. The case of this woman illustrates this point. The challenges can be discussed under the following headings:
Performance of HIV rapid diagnostic tests
Some HIV rapid diagnostic tests have been associated with poor sensitivity and unacceptably high rate of false positive results. A study done in the Rakai District of Uganda revealed critical inaccuracies in rapid testing results. This study was done using the three most commonly used HIV rapid diagnostic tests in Uganda. When the results of the rapid tests were compared with other testing methods (e.g. Western blot) 129 of the 295 people who were diagnosed as HIV-positive were actually HIV-negative5.
In the Democratic Republic of Congo, a study using these tests found that poor performance of HIV rapid diagnostic test two consecutive positive results from two separate rapid tests had a 10.5% chance of producing false-positive results6. In Cameroon, despite using a highly specific second test 2 out of every 100 people who are tested with this algorithm are still receiving false positive results. In Malawi over 1.7 million people were tested for HIV last year. If the national prevalence is 10% , 170,000 of these would have tested HIV positive. Depending on the specificity of the tests used, anything between 2% (3400 people) and 10% (17000 people) would have received a false positive result in Malawi last year.
Human resource issues:
Despite the large numbers of people being tested every year, the number of health professionals available to administer and interpret the test results has not increased proportionately. This has left clinic staff with less training and experience to run testing centres in some areas7. Indeed rapid HIV testing training may not be as demanding as other forms of testing and thus making HIV test feasible in low resource settings8. However underestimating value of training may completely undermine the quality and accuracy of the test results the patients receive. The competence of staff providing counselling is equally critical. In many settings in resource limited countries including Malawi, counsellors providing the service do not have adequate skills. As a result counseling does not take place since testing is being done by a range of professionals who aren't necessarily trained in counseling9. Clinic staff members conducting counseling often lack the skills necessary to provide adequate assistance with crisis intervention and are less effective in terms of helping an HIV-positive individual cope with the results10
Quality Control issues
Many testing sites in Malawi do not have standard operating procedures on how to carry out HIV counseling and testing. The professionals providing testing are also not subject to regular supervision from the laboratories that are supposed to check the validity of test results being given to patients. It is not clear what recourse testing staff have when problems arise during the testing process. The HIV reference laboratory is supposed to provide guidance on HIV testing and redoing the test on a selected percentage of the tests done. The system as it is at present where no samples are stored at the testing site makes this important aspect of quality control impossible to implement. The individuals involved in testing were trained once, it is unclear whether follow up training has occurred in many sites to make sure that the skills are still adequate for those conducting the testing.
Conclusion
It is difficult to pin point where things fell apart in the management of this woman. An analysis of the HIV counseling and testing procedures and HIV treatment in Malawi suggests that there are significant gaps that need to be filled in the HIV programme. It is clear that there are many more people like her that are living positively and on treatment while they may be HIV negative. It is time we adopted rigorous standards in HIV counseling and testing in the Malawi setting. Patients that present with repeated illnesses should be assessed further for other causes of immunosuppression in addition to HIV infection. For this woman, the reason for her oral thrush was very clear. Prolonged use of steroids is a well known cause.
Fig 1.
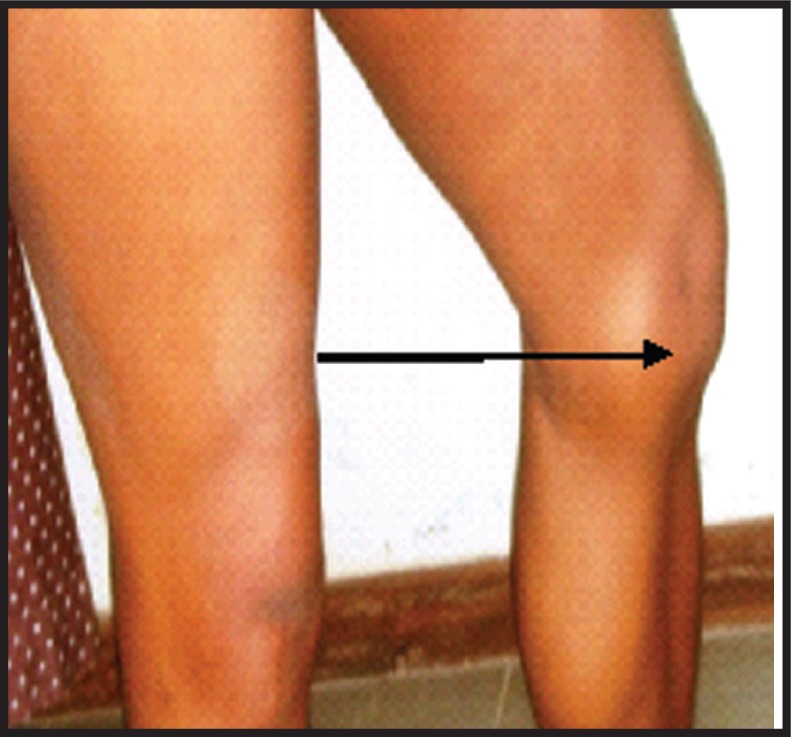
Excess fat on left knee (arrow)
Fig 2.

Excess fat on the back
References
- 1.HIV Program Quarterly reports. Government of Malawi-Ministry of Health; 2011. Apr-Jun. [Google Scholar]
- 2.Clinical management of HIV in adults and children. Malawi: ©2011 Ministry of Health publication; [Google Scholar]
- 3.Prority interventions:HIV/AIDS prevention, treatment and care in the health sector. 2010 [Google Scholar]
- 4.World Health Organization, author. The importance of simple and rapid tests in HIV diagnostics: WHO recommendations. Weekly Epidemiological Record. 1998;73(42):321–328. [Google Scholar]
- 5.Gray R, et al. Limitations of rapid HIV-1 tests during screening for trials in Uganda: diagnostic test accuracy study. BMJ. 2007;335.7612:335. doi: 10.1136/bmj.39210.582801.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Klarkowski D, et al. The Evaluation of Rapid In Situ HIV Confirmation Test in a Programme with a High Failure Rate of the WHO HIV Two-Test Diagnostic Algorithm. PLUS One. 2009;4.2 doi: 10.1371/journal.pone.0004351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grusky O, Roberts K, Swanson A. Failure to return for HIV test results a pilot study of three community testing sites. Journal of the International Association of Physicians in AIDS Care. 2007;6.1 doi: 10.1177/1545109706297530. 47+ [DOI] [PubMed] [Google Scholar]
- 8.Constantine N, Zink H. HIV testing technologies after two decades of evolution. Indian Journal of Medical Research. 2005;121.4:519–538. [PubMed] [Google Scholar]
- 9.Sibbald B. New rapid HIV test opens Pandora's box of ethical concerns. Canadian Medical Association Journal. 2000;162.11:1600. [PMC free article] [PubMed] [Google Scholar]
- 10.Galvin F, Brooks R, Leibowitz A. Rapid HIV Testing: Issues in Implementation. AIDS Patient Care and STDs. 2004;18.1:15–18. doi: 10.1089/108729104322740875. [DOI] [PubMed] [Google Scholar]
- 11.Center for Disease Control and Prevention, author. HIV prevention strategic plan through 2005. 2001. Jan, Available from: URL: http://www.cdc.gov/hiv/pubs/prev-strat-plan.pdf.
- 12.World Health organization, author. Guidelines for use in HIV testing in resource constrained settings. World Health Organization; 2004. [Google Scholar]


