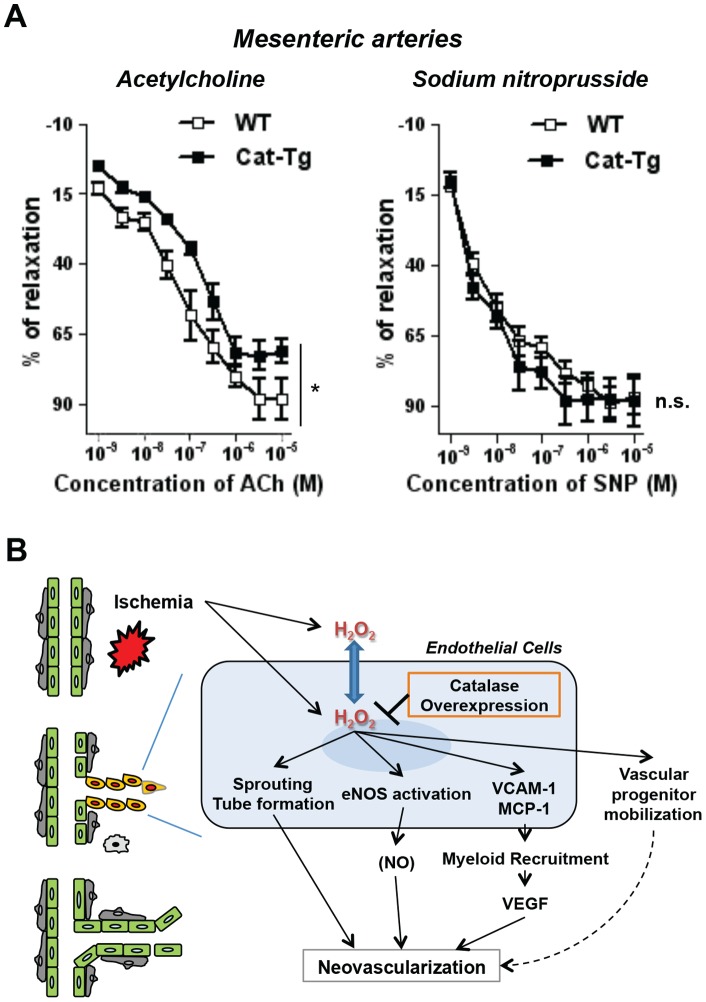
Figure 7. Endothelial catalase overexpression blunts endothelium-dependent relaxation of resistant vessels.
A, the first branches mesenteric arteries were harvested from Wild-type (WT) and Tie2-driven catalase transgenic (Cat-Tg) mice and assessed for endothelium-dependent or – independent relaxation by acetylcholine or sodium nitroprusside, respectively (n = 4 per group and *p<0.05). Data shown are mean+SE. B, a proposed model for the role of endogenous H2O2 in endothelial cells during ischemia-induced neovascularization. Tissue ischemia induces endogenous reactive oxygen species production including hydrogen peroxide (H2O2) intracellularly and extracellularly for endothelial cells. Intracellular H2O2, which can be reduced by Tie2-driven catalase overexpression in this study, promote crucial neovascular signaling regulating endothelial sprouting and tube formation, endothelial nitric oxide synthase (eNOS) activation as well as the expression of vascular adhesion molecule (VCAM)-1 and monocyte chemoattractant protein (MCP)-1. Endothelial H2O2 could be involved in vascular progenitor mobilization. H2O2 is thought to be diffusible across cellular membrane (blue arrow). Myeloid recruitment, vascular endothelial growth factor (VEGF) and potential nitric oxide (NO) production are regulated by endogenous H2O2 in endothelial cells during neovascularization.