Sir,
Lingual thyroid (LT) is a rare developmental thyroid anomaly affecting 1:100000 individuals, more commonly affecting females. LT is usually located in the midline and in base of the tongue.[1]
LT is usually associated with absence of normal thyroid gland. The majorities of patients are asymptomatic, but may develop dysphagia, dysphonia, pain, bleeding, or fullness in the throat as the LT enlarges. Hypothyroidism may be presenting symptom in the absence of normal thyroid.[2] Hyperthyroidism is an exceptionally rare finding and has been observed only in a few cases.[3]
Although reports of LT complicating airway management have been addressed in the past, but none has addressed the issue from perspective of thyroid storm occurring during attempts to secure airway in an under-optimized hyperthyroid patient.
A 12-year-old boy presented with complaints of abdominal pain and gastrointestinal (GI) bleed. Clinical examination revealed pallor, tachycardia, and a mass in the posterior part of the tongue [Figure 1]. Patient was diagnosed to have a GI bleed due to Meckel's diverticulum with an associated LT [Figure 2]. Thyroid stimulating hormone (TSH) was 0.05 μU/ml (0.35-5.50 μIU/ml); Triiodothyronine (T3) 250 ng/dl (60.00-181.00 ng/dl); Tetraiodothyronine (T4) 23 μg/ml (4.50-12.60 μg/dl), thereby indicating a hyperfuctioning LT.
Figure 1.

Lingual thyroid on the posterior part of the tongue
Figure 2.
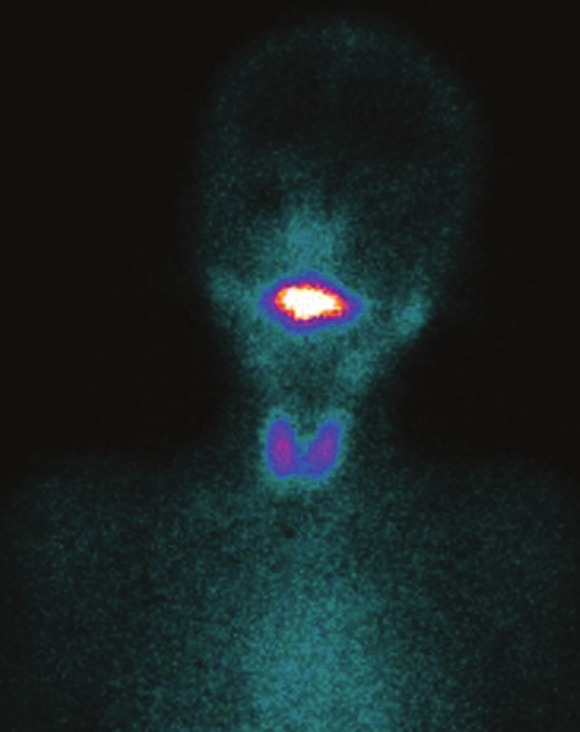
Tc99m pertechnetate planar image of neck and mediastinum showing presence of hyperfunctioning lingual thyroid gland with normal thyroid gland in the neck
Oral propylthiouracil 300 mg QID, iodine 2 drops twice-daily, propanolol 30 mg QID, and hydrocortisone 50 mg TID were prescribed for pre-operative optimization of the thyroid profile. Ongoing GI bleed mandated laparotomy 3 days after the starting of anti-thyroid drugs.
General anesthesia with epidural analgesia was planned. A high-risk consent for emergency surgery was obtained with specific reference to the possibility of an intra-operative thyroid storm.
Standard ASA monitoring was applied. Epidural catheter was inserted at T7-8 level for analgesia. Anesthesia was induced with thiopentone sodium 150 mg, fentanyl 200 mcg, midazolam 1 mg, and vecuronium bromide 4 mg intravenous (IV). Labetolol was kept ready for management of a possible thyroid storm. Nasopharyngeal airway was inserted to facilitate bag and mask ventilation. Tracheal intubation was with a 5.5 mm armored endotracheal tube (ETT) rail-roaded over a 2 mm fiberoptic bronchoscope through the nasal route. Maintenance of anesthesia was with sevoflurane (2%) in an air-oxygen mixture. Surgery proceeded uneventfully. Patient was reversed from anesthesia, and trachea was extubated successfully.
Only a few case report are available suggesting LT as cause of difficult mask ventilation and direct laryngoscopy, but none reports the implications of hyperthyroidism in LT. Maneuvre as simple as insertion of oropharyngeal airway can abrade the LT and produced bleeding in oral cavity, which would have been catastrophic.[4] The LT would have made the conventional DL and mask ventilation difficult,[5] and at the same time, could have produced thyroid storm due to compression of the intraoral mass by the laryngoscope blade. Anesthetist should resort to nasal approach of airway instrumentation in presence of lingual thyroid, and no attempt should be made through the oral route, as doing so may jeopardize the nasal approach as well. We used the nasal route with a small diameter fiberoptic bronchoscope and an undersized ETT.
References
- 1.Ueda D, Yoto Y, Sato T. Ultrasonic assessment of the lingual thyroid gland in children. Pediatr Radiol. 1998;28:126–8. doi: 10.1007/s002470050311. [DOI] [PubMed] [Google Scholar]
- 2.Williams JD, Sclafani AP, Slupchinskij O, Douge C. Evaluation and management of the lingual thyroid gland. Ann Otol Rhinol Laryngol. 1996;105:312–6. doi: 10.1177/000348949610500414. [DOI] [PubMed] [Google Scholar]
- 3.Abdallah-Matta MP, Dubarry PH, Pessey JJ, Caron P. Lingual thyroid and hyperthyroidism: A new case and review of the literature. J Endocrinol Invest. 2002;25:264–7. doi: 10.1007/BF03344002. [DOI] [PubMed] [Google Scholar]
- 4.Buckland RW, Pedley J. Lingual thyroid: A threat to the airway. Anesthesia. 2000;55:1103–5. doi: 10.1046/j.1365-2044.2000.01610.x. [DOI] [PubMed] [Google Scholar]
- 5.Palmer JH, Ball DR. Lingual thyroid: Another potential airway threat. Anesthesia. 2001;56:386. doi: 10.1046/j.1365-2044.2001.01976-25.x. [DOI] [PubMed] [Google Scholar]


